Abstract
Cases of coronary artery spasm secondary to contrast agent use are rarely reported. Herein, we report the case of a 53-year-old woman who developed chest pain, dyspnea, and bradycardia and quickly become unresponsive after magnetic resonance imaging of the brain. A heart monitor showed ST elevation, and an electrocardiogram showed ST elevations in leads II, III, aVF, V3, and V4 and ST segment depression in lead I. Urgent left heart catheterization revealed no evidence of obstructive coronary artery disease or pulmonary embolism. A few days later, she was discharged from the hospital with no symptoms. A type I variant of Kounis syndrome was diagnosed.
Keywords: Acute coronary syndrome, allergy, contrast medium–induced coronary vasospasm, coronary hypersensitivity disorder, Kounis syndrome
Hypersensitivity to a contrast agent can provoke acute coronary syndromes. Kounis syndrome (KS), first described in 1991 by Kounis and Zavras,1 is also known as “allergic angina syndrome” or “allergic myocardial infarction.” It is not rare but is infrequently diagnosed, and its type I variant manifests as a nonthrombogenic cause of angina that can progress to myocardial infarction triggered by the release of inflammatory mediators following an allergic or anaphylactic reaction.2 All contrast agents have the potential to cause KS.
CASE PRESENTATION
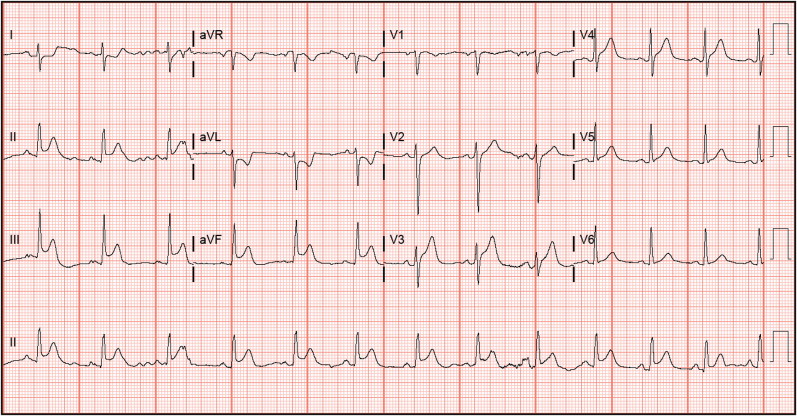
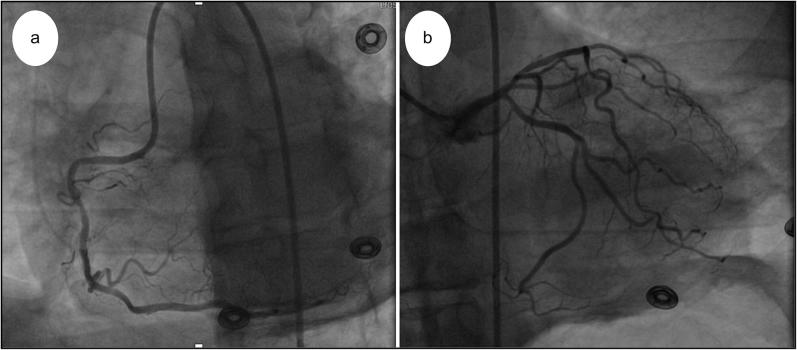
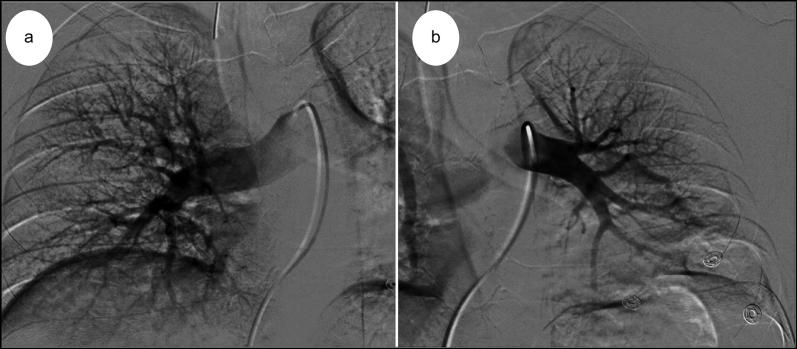
A 53-year-old woman with a history of renal cell carcinoma and recent right nephrectomy was found to have a metastatic lesion of the left lower lobe lung and was scheduled for magnetic resonance (MR) imaging of the brain for headaches. She had no coronary risk factors or family history of premature coronary artery disease. After the patient underwent brain MR imaging without contrast and experienced no adverse effects, no abnormalities were found, and further imaging with gadolinium contrast was ordered. Several minutes after contrast administration, she developed chest pain and shortness of breath. She quickly became unresponsive and was transferred to a nearby hospital. In the emergency room, her oxygen saturation was 50% and her heart rate was 40 beats/min. Subsequently, she was given 0.5 mg of atropine, which increased her heart rate to 100 beats/min. She was still edematous and unconscious. Intubation was made difficult by swelling of the tongue and glottis. Her heart monitor began to show signs of ST elevation. An electrocardiogram showed ST elevations in leads II, III, aVF, V3, and V4 and ST segment depression in lead I (Figure 1). Her troponin level increased from 0.015 to 1.12 ng/mL. Emergent left heart catheterization revealed no evidence of obstructive coronary artery disease or pulmonary embolism (Figures 2 and 3).
Figure 1.
Electrocardiogram showing ST elevations in leads II, III, aVF, V3, and V4 and ST segment depression in lead I.
Figure 2.
Coronary angiogram showing (a) mild disease in the middle right coronary artery and (b) patent coronary arteries with no evidence of stenosis.
Figure 3.
(a) Right and (b) left coronary pulmonary angiography showing no evidence of pulmonary embolism.
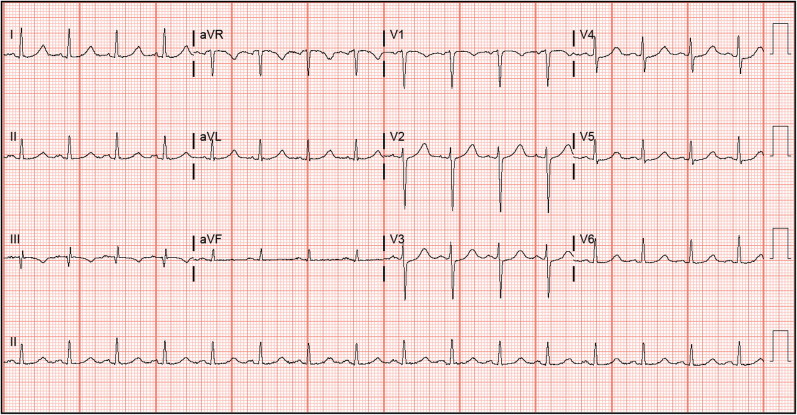
After ruling out acute coronary syndrome, other possibilities for the patient’s sudden deterioration were considered. A hypersensitivity reaction to gadolinium was believed to be the probable cause, especially in the absence of any major cardiovascular risk factors. After gadolinium administration was stopped, her ST elevations returned toward baseline (Figure 4) and her cardiac biomarker levels dropped. The patient was treated with dexamethasone in the intensive care unit. She was extubated after 3 days, transferred to the floor, and discharged home a few days later. In a follow-up appointment a week after discharge, she was pain free and had a normal clinical status.
Figure 4.
Electrocardiogram demonstrating resolution of ST elevations.
DISCUSSION
The association of an acute coronary incident with an allergic reaction following medication administration was first reported with penicillin in 1950.3 In 1991, Kounis and Zavras described allergic coronary syndrome.1 KS is defined as the occurrence of chest pain and hypersensitivity reactions accompanied by clinical and laboratory findings of classic angina pectoris, presumably due to the inflammatory mediators released during the allergic insult.4 The actual incidence of KS is undetermined. In a retrospective study, the annual incidence of severe life-threatening anaphylaxis with circulatory symptoms ranged from 7.9 to 9.6 cases per 100,000 persons per year.5 More than 300 cases of KS have been described following exposure to various substances, including drugs (antibiotics, anesthetics, analgesics, corticosteroids, contrast agents, acetylsalicylic acid), insect venom, food, and drug-eluting stents.6
The pathophysiology of KS is thought to be caused by coronary artery vasospasm due to the release of vasoactive mediators secondary to mast cell degranulation. During mast cell degranulation, several vasoactive compounds and collagen-degrading compounds are released, resulting in a powerful vasoconstriction of the coronary arteries. These mediators may act locally or systemically. Among the mediators released, the most significant are histamine, serotonin, and leukotrienes.4,7 Histamine has also been implicated in the activation of platelets and in triggering thrombosis. The mast cells in the heart tissue participate in anaphylaxis and trigger tachycardia, alter ventricular contractility, and block atrioventricular conduction—all leading to heart blocks of varying degrees. Renin is also released during episodes of anaphylaxis and can lead to heart dysfunction.8 In the case of immediate hypersensitivity reactions to MR contrast media, the pathophysiological mechanism is largely unknown. However, an experimental report suggests that contrast media can induce mast cell degranulation in vitro.9 Examination of coronary arteries from patients who died of acute myocardial infarction revealed that mast cell degranulation was 200 times higher in areas of plaque rupture or erosion than in adjacent areas.2
Three variants of KS have been described. The type I variant occurs in patients with normal or near-normal coronary arteries without predisposing factors for coronary artery disease; the acute release of inflammatory mediators can induce either coronary artery spasm or coronary artery rupture. The type II variant is seen in patients with preexisting atheromatous disease, and the mediator release can induce either coronary artery spasm or coronary artery spasm together with plaque erosion or rupture. Finally, the type III variant is diagnosed in patients with stent implantation who die suddenly, with histological examination of coronary intima, media, or adventitia adjacent to the stent demonstrating infiltration by eosinophils and/or mast cells. The type III variant represents either thrombosis in drug-eluting coronary stents or coronary stent restenosis.10,11
The diagnosis of KS is centered on clinical symptoms and signs, as well as on laboratory, electrocardiographic, echocardiographic, and angiographic evidence.9 The therapeutic management of KS is challenging because it requires addressing both the allergic reaction and the subsequent acute coronary syndrome. Treatment of KS requires thoughtful use of several frequently used medications. Morphine should be avoided because it may stimulate histamine release and exacerbate the pathologic cascade in KS. Beta-blockers also may potentiate coronary vasospasm if used in an acute exacerbation of KS due to unopposed alpha-adrenergic action. Epinephrine, which is used routinely for the treatment of anaphylaxis, should also be cautiously used, because it may potentially worsen coronary vasospasm and aggravate coronary ischemia in KS.12
References
- 1.Kounis NG, Zavras GM. Histamine-induced coronary artery spasm: the concept of allergic angina. Br J Clin Pract. 1991;45:121–128. [PubMed] [Google Scholar]
- 2.Scherbak D, Lazkani M, Sparacino N, Loli A. Kounis syndrome: a stinging case of ST-elevation myocardial infarction. Heart Lung Circ. 2015;24:e48–e50. doi: 10.1016/j.hlc.2014.11.026. [DOI] [PubMed] [Google Scholar]
- 3.Pfister CW, Plice SG. Acute myocardial infarction during a prolonged allergic reaction to penicillin. Am Heart J. 1950;40:945–947. [DOI] [PubMed] [Google Scholar]
- 4.Gázquez V, Dalmau G, Gaig P, Gómez C, Navarro S, Mercé J. Kounis syndrome: report of 5 cases. J Investig Allergol Clin Immunol, 2010;20:162–165. [PubMed] [Google Scholar]
- 5.Helbling A, Hurni T, Mueller UR, Pichler WJ. Incidence of anaphylaxis with circulatory symptoms: a study over a 3-year period comprising 940,000 inhabitants of the Swiss Canton Bern. Clin Exp Allergy. 2004;34:285–290. doi: 10.1111/j.1365-2222.2004.01882.x. [DOI] [PubMed] [Google Scholar]
- 6.Li J, Zheng J, Zhou Y, Liu X, Peng W. Acute coronary syndrome secondary to allergic coronary vasospasm (Kounis syndrome): a case series, follow-up and literature review. BMC Cardiovasc Disord. 2018;18:42.doi: 10.1186/s12872-018-0781-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kounis NG, Grapsas ND, Goudevenos JA. Unstable angina, allergic angina, and allergic myocardial infarction. Circulation. 1999;100:e156–e156. doi: 10.1161/01.CIR.100.25.e156. [DOI] [PubMed] [Google Scholar]
- 8.Triggiani M, Patella V, Staiano R I, Granata F, Marone G. Allergy and the cardiovascular system. Clin. Exp. Immunol. 2008;153(Suppl 1):7–11. [DOI] [PMC free article] [PubMed]
- 9.Tanaka H, Urushima M, Hirano S, Takenaga M. An acute adverse reaction with ST elevation induced by magnetic resonance contrast media: Kounis syndrome. Intern Med. 2019;58:243–245. doi: 10.2169/internalmedicine.0802-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Anandan PK, Hanumanthappa NB, Bhatt P, Cholenahally MN. Allergic angina following wasp sting: Kounis syndrome. Oxf Med Case Rep. 2015;2015:306–308. doi: 10.1093/omcr/omv044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Itoh T, Nakajima Y, Morino Y. Proposed classification for a variant of Kounis syndrome. Clin Chem Lab Med. 2017;55:e107–e107. doi: 10.1515/cclm-2016-0934. [DOI] [PubMed] [Google Scholar]
- 12.Memon S, Chhabra L, Masrur S, Parker MW. Allergic acute coronary syndrome (Kounis syndrome). Proc (Bayl Univ Med Cent). 2015;28:358–362. doi: 10.1080/08998280.2015.11929274. [DOI] [PMC free article] [PubMed] [Google Scholar]