Abstract
Objective
Recent technological advancements have led to the utilization of robotic-assisted knee arthroplasty (raKA) in the operating room.
Methods
All patients who underwent knee arthroplasty from 2009 to 2013 in NYS SPARCS were reviewed. raKAs and non-raKAs were compared for utilization and institutional trends.
Results
Robotic-assistance increased by 500%. 80% of raKAs were performed in teaching hospitals. The trend increase was greater in teaching hospitals. Blood transfusion rates differed between raKA and non-raKA (6.6% vs. 10.9%, p < 0.001).
Conclusion
raKA utilization increased in NYS, moreso within teaching hospitals. raKA transfusion rates were lower but higher in teaching hospitals, potentially related to learning curve.
Keywords: Robotic surgery, Robotic-assisted surgery, Total knee arthroplasty, Unicompartmental knee arthroplasty, Utilization trends
Abbreviations: Statewide Planning and Research Cooperative System (SPARCS), New York State (NYS)
1. Introduction
Osteoarthritis (OA) is an insidious disease process caused resulting in the deterioration of osseous and cartilaginous structures and ultimately results in stiffness, pain, and reduced functional ability of the joint.1, 2, 3 Both total (TKA) and unicompartmental knee (UKA) arthroplasty can effectively relieve pain and improve joint function. In the properly selected patient, UKA is a viable intervention that offers a less invasive procedure, fewer bone cuts and thus less blood loss, and cruciate ligament retention compared to TKA.4,5 Despite advancements in implant design, surgical technique, and outcome made in the last several decades, implant failure remains a concern.6,7 Knee arthroplasty failures are most commonly caused by malposition of the component in the coronal or axial plane.8 Additionally, in UKAs, malalignment and malposition can also lead to progression of OA to the adjacent joint compartment of the knee.4,9,10 However, these complications can be remedied by computer navigated and robot-assisted knee arthroplasty, which assists in bone preparation and with postoperative limb alignment.11
These newer modalities were developed in order to improve the outcomes of knee arthroplasty. Computer-navigated knee arthroplasties utilize preoperative computerized tomography (CT), magnetic resonance imaging (MRI), or infrared studies to register intraoperative landmarks and create a 3-dimensional operation model. A computer then uses these data to guide surgical instruments and adjust orientation and alignment.12 Robotic-assisted surgery combines these visual navigation benefits with a robotic arm that guides the femoral and tibial cuts, allowing for more precise implant placement.13,14 While literature on the efficacy of robotic-assisted knee arthroplasty exists, these studies often focus on specific physical parameters of the procedure.15, 16, 17 There remains a paucity of literature addressing the general trends of robotic-assisted knee arthroplasty procedures.
Therefore, the purpose of this study was to report on the current trends of robotic-assisted knee arthroplasties. Specifically, this study aimed to: 1) identify trends in the utilization of robotic assistance in knee arthroplasty; 2) compare the utilization of robotic-assisted knee arthroplasties in teaching and non-teaching hospitals; and 3) compare blood transfusion rates in robotic and non-robotic knee arthroplasties among teaching and non-teaching hospitals.
2. Methods
2.1. Data source
A retrospective analysis of the Statewide Planning and Research Cooperative System (SPARCS) database was performed using data from January 1, 2009 to December 31, 2013. The SPARCS data are the product of industry and governmental collaboration to create an accessible source for patient level discharge information, and is available through the New York State (NYS) Department of Health's Bureau of Health Informatics.18 All Article 28 licensed hospitals in NYS are required to submit inpatient and outpatient data to the SPARCS database. Article 28 licensed hospital extension clinics and diagnostic and treatment centers, certified to provide ambulatory surgery services, are also required to submit outpatient data to SPARCS. The database consists of the most robust, complete all-payer data available for the state of New York, which also assigns a unique tracking ID to each patient. Since this database is de-identified, the study was deemed exempt by our institutional review board.
2.2. Patient population
Patients who underwent a knee arthroplasty between January 1, 2009 and December 31, 2013 were identified based on the International Classification of Diseases, ninth revision (ICD-9) procedure code for knee arthroplasty (81.54); the code 81.54 was used to code both TKA and UKA. Additionally, robotic-assisted arthroplasties were identified using secondary ICD-9 procedure codes (17.41 and 17.49). The operation rates per year were identified along with the number of academic institutions, and blood transfusion rates.
2.3. Statistical analysis
All statistical analyses were performed with SPSS version 24 (IBM Corporation, Armonk, New York). A p-value of less than 0.05 was used as the threshold for statistical significance. Chi-Square test were utilized to analyze the proportion of robotic-assisted knee arthroplasty versus non-robotic knee arthroplasty procedures, the utilization of robotic-assistance for knee arthroplasty procedures in teaching versus non-teaching hospitals, and the rate of blood transfusion in robotic and non-robotic assisted knee arthroplasty procedures.
3. Results
3.1. Trends in robotic-assisted knee arthroplasty
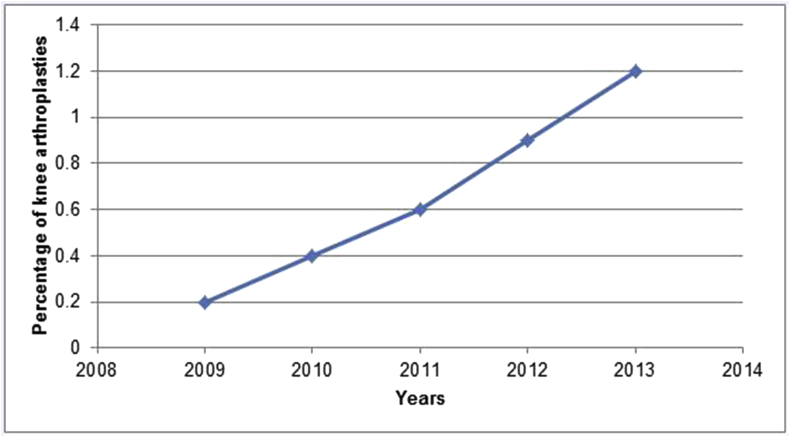
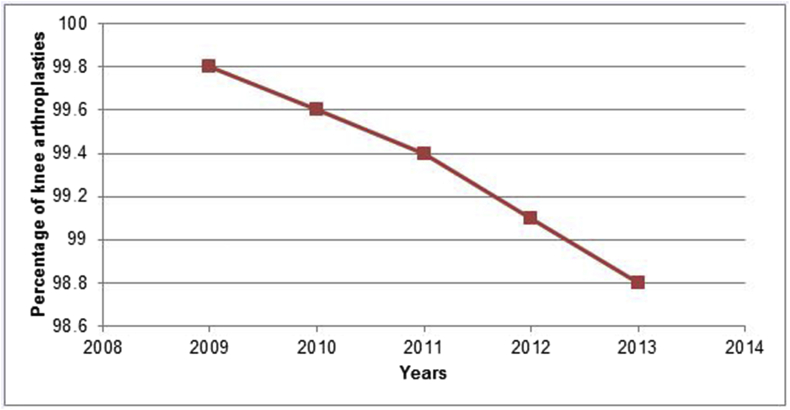
Over the course of the study period, a total of 151,147 knee arthroplasties were performed. Of these, 1002 (0.6%) knee arthroplasties were performed with robotic assistance. Additionally, a 500% increase was seen in the utilization of robotic assistance during the study period (0.2% in 2009 to 1.2% in 2013) of all arthroplasties (Fig. 1a, Fig. 1ba and b).
Fig. 1a.
Trends of robotic-assisted knee arthroplasty: 2009–2013.
Fig. 1b.
Trends of conventional knee arthroplasty: 2009–2013.
3.2. Utilization of robotic-assisted knee arthroplasty by institution type
When stratified by institution type, 80% of robotic-assisted knee arthroplasties were performed in teaching hospitals and 20% were performed in non-teaching hospitals. Overall, 1.4% of robotic-assisted knee arthroplasties were performed in teaching hospitals and 0.2% were performed in non-teaching hospitals (p < 0.001). An increased trend in the utilization of robotic assistance in knee arthroplasty was observed in both teaching and non-teaching hospitals over the 5-year period, but this trend was greater in teaching hospitals.
3.3. Comparison of blood transfusion rates
The blood transfusion rate in robotic-assisted knee arthroplasties was found to be significantly lower than the transfusion rate in non-robotic knee arthroplasties (6.6 vs. 10.9%, p < 0.001). Moreover, the blood transfusion rate was also found to be significantly higher in the procedures that were performed in teaching hospitals compared to those that were performed in non-teaching hospitals (13.9 vs. 9.2%, p < 0.001).
4. Discussion
As the number of annually performed knee arthroplasty procedures increases,19 there has been an increase in the utilization of all robotic-assisted arthroplasties. While these procedures represent only a small portion of knee arthroplasties performed, this study noted a substantial rise in robotic assistance in both teaching and non-teaching hospitals. Additionally, these findings were bolstered by a decreased transfusion rate noted with these procedures. The present study was an overview of the trends and benefits of robotic-assisted knee arthroplasties, and may be beneficial to the medical community in terms of knowledge of this emerging surgical procedure.
There were several limitations to the present study. This was a retrospective database study that was dependent on ICD-9 billing codes, which could be subject to coding errors. Also, the SPARCS database was unable to follow patients that sought continued care outside of the state of New York. Additionally, due to limitations of the database, specific surgical information such as surgical approach, implant type, and component position were not able to be reported. One further limitation is the inability to differentiate between robotic-assisted UKA from TKA. However, as many robotic TKA systems were not commercially available for use until approximately 2016–2017, it is likely that the majority of this reported increase was primarily from UKA. Nevertheless, the results of this study provide helpful information that could be beneficial for the treatment of knee OA.
The results of this study are consistent with previous studies that demonstrated the sparse use of robotic-assistance in knee arthroplasty Picard et al.20 stated that less than 3% of orthopaedic surgeons in the United States and England reported the use of computer-assisted technology in TKA, with similarly sporadic use of such technologies reported in Brazil, France, and Asia. Friederich and Verdonk21 utilized a 24-question online survey to assess the attitudes of orthopaedic surgeons towards computer-assisted TKAs, and was completed by 389 physicians who practiced in the United States, United Kingdom, Switzerland, Belgium, Germany, and the Netherlands. Of the 389 respondents, 202 (51.9%) stated that their workplaces were equipped with a navigation system, 61.4% of which utilized these systems for TKAs. Moreover, 66.8% of the surgeons, were considered “low proportion” users (fewer than 50% of procedures), while 22% reported that they had not used navigation equipment. The minimal utilization of such technologies, even when available to surgeons, was reported to be due to a perceived lack of efficacy of such surgical techniques. Interestingly, 37.4% of the surveyed surgeons stated they had an interest in acquiring navigation systems, and 48% of respondents who already had a navigation system available to them, plan on using it more frequently in the future. These trends appeared in line with those found in the present study regarding an increased use and interest in robotic assistance in knee arthroplasty, despite the slow spread of this technology and its utilization within the field. Unlike the data found in these previous studies, Deep et al.22 noted an increased use of computer-assisted technology had been reported in Australia (28.6%) and Germany (30%). If the trends reported in the present study continue in a similar or increased fashion, this widespread use of computer assisted orthopaedic surgery may soon be seen in the United States.
The present study found that a majority of robotic-assisted knee arthroplasties in the study population were performed at teaching compared to non-teaching hospitals (80% vs. 20%). Several studies focused on the costs and benefits of the introduction and use of robotic and computer-assisted surgical techniques.23,24 Slover et al.23 performed a cost analysis on robotic-assisted treatment of joint disease, and found that the cost of robotic-assisted TKA decreased as the volume of procedures increased, and the costs of surgical complications and revisions decreased. The authors noted that a facility that performs 250 TKAs per year, computer assistance would be cost effective if the annual revision rate of these surgeries is reduced by 2% over a 20-year period. At a facility that performs 150 TKAs per year, cost effectiveness of robotic assistance is achieved by reducing annual revisions by 2.5% over 20 years. In facilities that perform 25 TKAs per year the value of annual revision decrease necessary for cost effectiveness is 13%.23 Conditt et al.24 included additional factors in calculating the value of robotic-assisted arthroplasty, such as increased operation times and higher costs of medical equipment, which although they are usually fixed up-front costs, they may decrease the financial value of such procedures. Additionally, the authors predicted an increase in the utilization of robotic assisted technology in parallel with the increasing utilization of partial knee arthroplasty.24
Randell et al.,25 in a review of the experiences of surgical teams that utilized robotic techniques, also noted the potential complications of increased operative times in robotic surgeries, as well as communication problems that can arise between members of robotic surgery team. The study found a significant difference in the training received by surgical teams. Specific focus in assembling surgical teams as well as increased effort in communications training for these teams might remedy these complications and increase the efficacy and utilization of robotic assisted surgery.
The results of this study regarding blood loss and transfusion rates were similar to those found in previous studies. Kalairajah et al.26 performed a prospective randomized trial to assess blood loss in computer assisted (n = 30) and conventional (n = 30) TKAs, and found that those who underwent computer-assisted TKA had a lower mean postoperative blood drainage than the conventional TKA group (1351 vs. 1747 mL, p = 0.001) Also, there was a lower calculated hemoglobin loss, which was determined by subtracting the postoperative day 2 hemoglobin from the preoperative hemoglobin levels, in the computer-assisted compared to the conventional TKA cohorts (36.5 vs. 52.6 g/dL, p < 0.00001). Millar et al.27 evaluated the blood loss following computer navigated and conventional TKAs in obese and non-obese patients. A cohort of morbidly obese patients (BMI > 40 kg/m2) who underwent computer navigated TKA (n = 30) or conventional TKA (n = 30) were compared to a matched cohort of patients who had a BMI < 30 kg/m2 who underwent computer navigated TKA (n = 31) or conventional TKA (n = 31). They found that across all BMIs, the mean intraoperative blood loss was significantly lower in computer navigated versus the conventional TKAs (1014 vs. 1287 mL, p < 0.001).
5. Conclusions
The utilization of robotic-assisted knee arthroplasty has increased in New York State, and early adaptation was found to be greater among teaching hospitals. This may demonstrate a potential increased early exposure to robotic-assisted knee arthroplasties for residents and fellows during their graduate medical education training. The blood transfusion rate was found to be lower with the robotic-assisted procedures, but was overall higher in teaching hospitals. This may be due the learning curve of this new technique or the academic/teaching nature of the hospital. As the popularity of robotic-assisted knee arthroplasties increases, more studies should be conducted to further elucidate the potential benefits of robotic-assisted knee arthroplasties, in order to provide healthcare providers and patients more effective and appropriate surgical options when indicated.
Funding
No sources of funding were solicited or utilized in the completion of any aspect of this study.
Conflicts of interest
There are no relationships or conflicts of interest directly related to this paper or that could influence or bias this work. The following authors have no disclosures to report: Naziri, Burekhovich, Mixa, Pivec, Newman, and Shah. The author Sastry reports consultant fees from the following: Stryker, Medtronic. The author Sastry reports research support from the following: Stryker. The author Patel reports consultant fees from the following: Stryker.
Author contributions
Qais Naziri, MD, MBA: Study conception and design, manuscript writing, manuscript editing.
Steven A. Burekhovich, BA: Data analysis, manuscript writing, manuscript editing.
Patrick J. Mixa, MD: Data analysis, manuscript writing, manuscript editing.
Robert Pivec, MD: Study conception, data analysis, manuscript writing.
Jared M. Newman, MD: Data analysis, manuscript writing, manuscript editing.
Neil V. Shah, MD, MS: Data analysis, manuscript writing, manuscript editing.
Preetesh D. Patel, MD: Study conception, data validation from orthopaedic surgery standpoint, manuscript editing.
Akhilesh Sastry, MD: Study conception, data validation from orthopaedic surgery standpoint, manuscript editing.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jor.2019.04.020.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Lane N.E., Brandt K., Hawker G. OARSI-FDA initiative: defining the disease state of osteoarthritis. Osteoarthritis Cartilage. 2011;19(5):478–482. doi: 10.1016/j.joca.2010.09.013. [DOI] [PubMed] [Google Scholar]; Lane NE, Brandt K, Hawker G, et al. OARSI-FDA initiative: Defining the disease state of osteoarthritis. Osteoarthr Cartil. 2011;19(5):478-482. doi:10.1016/j.joca.2010.09.013. [DOI] [PubMed]
- 2.Eckstein F., Burstein D., Link T.M. Quantitative MRI of cartilage and bone: degenerative changes in osteoarthritis. NMR Biomed. 2006;19(7):822–854. doi: 10.1002/nbm.1063. [DOI] [PubMed] [Google Scholar]; Eckstein F, Burstein D, Link TM. Quantitative MRI of cartilage and bone: degenerative changes in osteoarthritis. NMR Biomed. 2006;19(7):822-854. doi:10.1002/nbm.1063. [DOI] [PubMed]
- 3.Link T.M., Steinbach L.S., Ghosh S. Osteoarthritis: MR imaging findings in different stages of disease and correlation with clinical findings. Radiology. 2003;226(2):373–381. doi: 10.1148/radiol.2262012190. [DOI] [PubMed] [Google Scholar]; Link TM, Steinbach LS, Ghosh S, et al. Osteoarthritis: MR imaging findings in different stages of disease and correlation with clinical findings. Radiology. 2003;226(2):373-381. doi:10.1148/radiol.2262012190. [DOI] [PubMed]
- 4.Gladnick B.P., Nam D., Khamaisy S., Paul S., Pearle A.D. Onlay tibial implants appear to provide superior clinical results in robotic unicompartmental knee arthroplasty. HSS J. 2015;11(1):43–49. doi: 10.1007/s11420-014-9421-9. [DOI] [PMC free article] [PubMed] [Google Scholar]; Gladnick BP, Nam D, Khamaisy S, Paul S, Pearle AD. Onlay Tibial Implants Appear to Provide Superior Clinical Results in Robotic Unicompartmental Knee Arthroplasty. HSS J. 2015;11(1):43-49. doi:10.1007/s11420-014-9421-9. [DOI] [PMC free article] [PubMed]
- 5.Walker T., Gotterbarm T., Bruckner T., Merle C., Streit M.R. Return to sports, recreational activity and patient-reported outcomes after lateral unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2014;23(11):3281–3287. doi: 10.1007/s00167-014-3111-5. [DOI] [PubMed] [Google Scholar]; Walker T, Gotterbarm T, Bruckner T, Merle C, Streit MR. Return to sports, recreational activity and patient-reported outcomes after lateral unicompartmental knee arthroplasty. Knee Surgery, Sport Traumatol Arthrosc. 2014;23(11):3281-3287. doi:10.1007/s00167-014-3111-5. [DOI] [PubMed]
- 6.Keblish P.A., Briard J.L. Mobile-bearing unicompartmental knee arthroplasty: a 2-center study with an 11-year (mean) follow-up. J Arthroplast. 2004;19(7 SUPPL):87–94. doi: 10.1016/j.arth.2004.07.009. [DOI] [PubMed] [Google Scholar]; Keblish PA, Briard JL. Mobile-bearing unicompartmental knee arthroplasty: A 2-center study with an 11-year (mean) follow-up. J Arthroplasty. 2004;19(7 SUPPL.):87-94. doi:10.1016/j.arth.2004.07.009. [DOI] [PubMed]
- 7.Zuiderbaan H.A., van der List J.P., Chawla H., Khamaisy S., Thein R., Pearle A.D. Predictors of subjective outcome after medial unicompartmental knee arthroplasty. J Arthroplast. 2016;31(7):1453–1458. doi: 10.1016/j.arth.2015.12.038. [DOI] [PubMed] [Google Scholar]; Zuiderbaan HA, van der List JP, Chawla H, Khamaisy S, Thein R, Pearle AD. Predictors of Subjective Outcome After Medial Unicompartmental Knee Arthroplasty. J Arthroplasty. 2016;31(7):1453-1458. doi:10.1016/j.arth.2015.12.038. [DOI] [PubMed]
- 8.Manzotti A., Confalonieri N., Pullen C. Unicompartmental versus computer-assisted total knee replacement for medial compartment knee arthritis: a matched paired study. Int Orthop. 2007;31(3):315–319. doi: 10.1007/s00264-006-0184-x. [DOI] [PMC free article] [PubMed] [Google Scholar]; Manzotti A, Confalonieri N, Pullen C. Unicompartmental versus computer-assisted total knee replacement for medial compartment knee arthritis: A matched paired study. Int Orthop. 2007;31(3):315-319. doi:10.1007/s00264-006-0184-x. [DOI] [PMC free article] [PubMed]
- 9.Jeer P.J.S., Keene G.C.R., Gill P. Unicompartmental knee arthroplasty: an intermediate report of survivorship after the introduction of a new system with analysis of failures. Knee. 2004;11(5):369–374. doi: 10.1016/j.knee.2004.06.001. [DOI] [PubMed] [Google Scholar]; Jeer PJS, Keene GCR, Gill P. Unicompartmental knee arthroplasty: An intermediate report of survivorship after the introduction of a new system with analysis of failures. Knee. 2004;11(5):369-374. doi:10.1016/j.knee.2004.06.001. [DOI] [PubMed]
- 10.Khamaisy S., Zuiderbaan H.A., van der List J.P., Nam D., Pearle A.D. Medial unicompartmental knee arthroplasty improves congruence and restores joint space width of the lateral compartment. Knee. 2016;23(3):501–505. doi: 10.1016/j.knee.2016.02.012. [DOI] [PubMed] [Google Scholar]; Khamaisy S, Zuiderbaan HA, van der List JP, Nam D, Pearle AD. Medial unicompartmental knee arthroplasty improves congruence and restores joint space width of the lateral compartment. Knee. 2016;23(3):501-505. doi:10.1016/j.knee.2016.02.012. [DOI] [PubMed]
- 11.Tamam C., Plate J.F., Augart M., Poehling G.G., Jinnah R.H. Retrospective clinical and radiological outcomes after robotic assisted bicompartmental knee arthroplasty. Adv Orthop. 2015;2015 doi: 10.1155/2015/747309. [DOI] [PMC free article] [PubMed] [Google Scholar]; Tamam C, Plate JF, Augart M, Poehling GG, Jinnah RH. Retrospective Clinical and Radiological Outcomes after Robotic Assisted Bicompartmental Knee Arthroplasty. Adv Orthop. 2015;2015. doi:10.1155/2015/747309. [DOI] [PMC free article] [PubMed]
- 12.Buza J.A., Wasterlain A.S., Thakkar S.C., Meere P., Vigdorchik J. Navigation and robotics in knee arthroplasty. JBJS Rev. 2017;5(2) doi: 10.2106/JBJS.RVW.16.00047. [DOI] [PubMed] [Google Scholar]; Buza JA, Wasterlain AS, Thakkar SC, Meere P, Vigdorchik J. Navigation and Robotics in Knee Arthroplasty. JBJS Rev. 2017;5(2). doi:10.2106/JBJS.RVW.16.00047. [DOI] [PubMed]
- 13.Dunbar N.J., Roche M.W., Park B.H., Branch S.H., Conditt M.A., Banks S.A. Accuracy of dynamic tactile-guided unicompartmental knee arthroplasty. J Arthroplast. 2012;27(5):803–808. doi: 10.1016/j.arth.2011.09.021. e1. [DOI] [PubMed] [Google Scholar]; Dunbar NJ, Roche MW, Park BH, Branch SH, Conditt MA, Banks SA. Accuracy of Dynamic Tactile-Guided Unicompartmental Knee Arthroplasty. J Arthroplasty. 2012;27(5):803-808.e1. doi:10.1016/j.arth.2011.09.021. [DOI] [PubMed]
- 14.Jacofsky D.J., Allen M. Robotics in arthroplasty: a comprehensive review. J Arthroplast. 2016;31(10):2353–2363. doi: 10.1016/j.arth.2016.05.026. [DOI] [PubMed] [Google Scholar]; Jacofsky DJ, Allen M. Robotics in Arthroplasty: A Comprehensive Review. J Arthroplasty. 2016;31(10):2353-2363. doi:10.1016/j.arth.2016.05.026. [DOI] [PubMed]
- 15.Zhang Z., Zhu W., Zhu L., Du Y. Superior alignment but no difference in clinical outcome after minimally invasive computer-assisted unicompartmental knee arthroplasty (MICA-UKA) Knee Surg Sports Traumatol Arthrosc. 2016;24(11):3419–3424. doi: 10.1007/s00167-014-3456-9. [DOI] [PubMed] [Google Scholar]; Zhang Z, Zhu W, Zhu L, Du Y. Superior alignment but no difference in clinical outcome after minimally invasive computer-assisted unicompartmental knee arthroplasty (MICA-UKA). Knee Surg Sports Traumatol Arthrosc. 2016;24(11):3419-3424. doi:10.1007/s00167-014-3456-9. [DOI] [PubMed]
- 16.Cossey A.J., Spriggins A.J. The use of computer-assisted surgical navigation to prevent malalignment in unicompartmental knee arthroplasty. J Arthroplast. 2005;20(1):29–34. doi: 10.1016/j.arth.2004.10.012. [DOI] [PubMed] [Google Scholar]; Cossey AJ, Spriggins AJ. The use of computer-assisted surgical navigation to prevent malalignment in unicompartmental knee arthroplasty. J Arthroplasty. 2005;20(1):29-34. doi:10.1016/j.arth.2004.10.012. [DOI] [PubMed]
- 17.Chowdhry M., Khakha R.S., Norris M., Kheiran A., Chauhan S.K. Improved survival of computer-assisted unicompartmental knee arthroplasty: 252 cases with a minimum follow-up of 5 years. J Arthroplast. 2016:1–5. doi: 10.1016/j.arth.2016.11.027. [DOI] [PubMed] [Google Scholar]; Chowdhry M, Khakha RS, Norris M, Kheiran A, Chauhan SK. Improved Survival of Computer-Assisted Unicompartmental Knee Arthroplasty: 252 Cases With a Minimum Follow-Up of 5 Years. J Arthroplasty. 2016:1-5. doi:10.1016/j.arth.2016.11.027. [DOI] [PubMed]
- 18.Bureau of Health Informatics Office of Quality and Health Safety. Statewide Planning and Research Cooperative System (SPARCS). New York State Department of Health.
- 19.Kurtz S., Ong K., Lau E., Mowat F., Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]; Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780-785. doi:10.2106/JBJS.F.00222. [DOI] [PubMed]
- 20.Frederic Picard Kamal Deep J.C., Gregori A. Computer assisted knee replacement surgery: is the movement mainstream? Orthop Muscular Syst Curr Res. 2014;3(2) [Google Scholar]; Frederic Picard Kamal Deep JC, Gregori A. Computer Assisted Knee Replacement Surgery: Is the Movement Mainstream? Orthop Muscular Syst Curr Res. 2014;3(2). doi:10.4172/2161-0533.1000153.
- 21.Friederich N., Verdonk R. The use of computer-assisted orthopedic surgery for total knee replacement in daily practice: a survey among ESSKA/SGO-SSO members. Knee Surg Sports Traumatol Arthrosc. 2008;16(6):536–543. doi: 10.1007/s00167-008-0518-x. [DOI] [PubMed] [Google Scholar]; Friederich N, Verdonk R. The use of computer-assisted orthopedic surgery for total knee replacement in daily practice: A survey among ESSKA/SGO-SSO members. Knee Surgery, Sport Traumatol Arthrosc. 2008;16(6):536-543. doi:10.1007/s00167-008-0518-x. [DOI] [PubMed]
- 22.Deep K., Shankar S., Mahendra A. Computer assisted navigation in total knee and hip arthroplasty. SICOT-J. 2017;3:50. doi: 10.1051/sicotj/2017034. [DOI] [PMC free article] [PubMed] [Google Scholar]; Deep K, Shankar S, Mahendra A. Computer assisted navigation in total knee and hip arthroplasty. SICOT-J. 2017;3:50. doi:10.1051/sicotj/2017034. [DOI] [PMC free article] [PubMed]
- 23.Slover J.D., Tosteson AN a, Bozic K.J., Rubash H.E., Malchau H. Impact of hospital volume on the economic value of computer navigation for total knee replacement. J Bone Joint Surg Am. 2008;90(7):1492–1500. doi: 10.2106/JBJS.G.00888. [DOI] [PMC free article] [PubMed] [Google Scholar]; Slover JD, Tosteson AN a, Bozic KJ, Rubash HE, Malchau H. Impact of hospital volume on the economic value of computer navigation for total knee replacement. J Bone Joint Surg Am. 2008;90(7):1492-1500. doi:10.2106/JBJS.G.00888. [DOI] [PMC free article] [PubMed]
- 24.Conditt M.A., Bargar W.L., Cobb J.P., Dorr L.D., Lonner J.H. Current concepts in robotics for the treatment of joint disease. Adv Orthop. 2013;2013 doi: 10.1155/2013/948360. 948360. [DOI] [PMC free article] [PubMed] [Google Scholar]; Conditt MA, Bargar WL, Cobb JP, Dorr LD, Lonner JH. Current concepts in robotics for the treatment of joint disease. Adv Orthop. 2013;2013:948360. doi:10.1155/2013/948360. [DOI] [PMC free article] [PubMed]
- 25.Randell R., Honey S., Alvarado N. Embedding robotic surgery into routine practice and impacts on communication and decision making: a review of the experience of surgical teams. Cognit Technol Work. 2016;18(2):423–437. [Google Scholar]; Randell R, Honey S, Alvarado N, et al. Embedding robotic surgery into routine practice and impacts on communication and decision making: a review of the experience of surgical teams. Cogn Technol Work. 2016;18(2):423-437. doi:10.1007/s10111-016-0368-0.
- 26.Kalairajah Y., Simpson D., Cossey A.J., Verrall G.M., Spriggins A.J. Blood loss after total knee replacement: effects of computer-assisted surgery. J Bone Joint Surg Br. 2005;87(11):1480–1482. doi: 10.1302/0301-620X.87B11.16474. [DOI] [PubMed] [Google Scholar]; Kalairajah Y, Simpson D, Cossey AJ, Verrall GM, Spriggins AJ. Blood loss after total knee replacement: effects of computer-assisted surgery. J Bone Joint Surg Br. 2005;87(11):1480-1482. doi:10.1302/0301-620X.87B11.16474. [DOI] [PubMed]
- 27.Millar N.L., Deakin A.H., Millar L.L., Kinnimonth A.W.G., Picard F. Blood loss following total knee replacement in the morbidly obese: effects of computer navigation. Knee. 2011;18(2):108–112. doi: 10.1016/j.knee.2010.03.002. [DOI] [PubMed] [Google Scholar]; Millar NL, Deakin AH, Millar LL, Kinnimonth AWG, Picard F. Blood loss following total knee replacement in the morbidly obese: Effects of computer navigation. Knee. 2011;18(2):108-112. doi:10.1016/j.knee.2010.03.002. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.