Abstract
Venous aneurysms are rarely reported in the literature since they are usually asymptomatic and incidentally detected due to complications such as thrombosis and pulmonary embolism. Often an inferior vena cava (IVC) aneurysm is detected by imaging studies performed for other causes. We report a case of large Type II IVC aneurysm associated with severe pectus excavatum in an asymptomatic man detected on routine 2D echocardiography. Focal narrowing of the IVC at the level of xiphisternum detected in multi-slice computed tomography might be the possible etiology for IVC aneurysm.
<Learning objective: Even though inferior vena cava aneurysms are rare, they can easily be diagnosed non-invasively by 2D echocardiography, ultrasound, and multi-slice computed tomography. The proximal obstruction of inferior vena cava by the xiphisternum as a complication of a severe form of pectus excavatum resulting in inferior vena cava aneurysm is probably a rare and possibly the only reported case in the literature.>
Keywords: Inferior vena cava, Aneurysm, Computed tomography, 2D echocardiography
Introduction
Inferior vena cava (IVC) aneurysms are rare vascular anomalies. Since the first case was reported by Oh et al. [1] in 1973, a review by Montero-Baker et al. [2] in 2015 suggested that a total of 53 such cases have been reported in the literature, including their own. Here, we present one such rare case of an IVC aneurysm with an emphasis on echocardiographic and multi-slice computed tomography (MSCT) findings.
Case report
A 35-year-old asymptomatic man presented to the cardiology department with severe pectus excavatum. His chief complaint was chest deformity. He had no chest pain, dyspnea, or palpitation. Clinically no abnormalities other than significant pectus excavatum like a saucer shape were noted (Fig. 1A). There were no clinical findings of heart failure or hepatic failure. Clinical examination revealed no heart murmur or an extra heart sound and no abdominal mass was palpable. Jugular venous pressure as well as pulse was normal. Blood pressure was 110/72 mmHg.
Fig. 1.
Anteroposterior view of the patient showing pectus excavatum.
His liver function tests, as well as renal function tests, were essentially normal. Chest X-ray posteroanterior view showed vertical anterior ribs (heart-shaped), horizontal posterior ribs, displacement of heart toward the left and blurring of right heart border (Fig. 2A). Electrocardiogram was normal with a heart rate of 85 beats/min (Fig. 2B). The 2D-echocardiography showed normal cardiac study. However, the infra hepatic part of the IVC was dilated and aneurysmal (Fig. 3A). Ultrasound of the abdomen also showed the same findings (Fig. 3B and C). A 64-detector MSCT showed pectus excavatum with a significant incursion of the sternum into the mediastinum with Haller index (maximum transverse diameter/narrowest anteroposterior length of the chest) of 9.4 (>3.5 is significant). There was a focal narrowing of the IVC at the level of xiphisternum (anteroposterior diameter: 9 mm and cross-sectional area: 0.9 cm2) (Fig. 4A). Aneurysmal dilatation of infra-hepatic IVC measuring 6.6 × 4.7 cm extending to a length of 12.6 cm was noted with associated dilatation of its tributaries and multiple venous collaterals (Fig. 4B–E). There was no evidence of thrombosis.
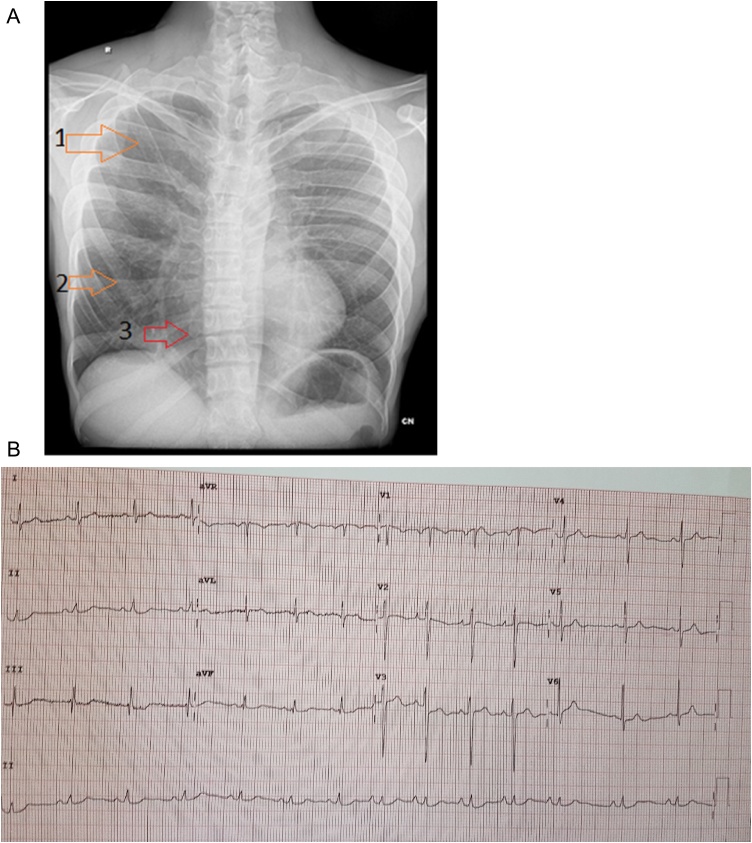
Fig. 2.
(A) Chest X-ray posteroanterior view showed (arrows) 1. Vertical anterior ribs (heart-shaped), 2. Horizontal posterior ribs 3. Displacement of heart towards the left and blurring of right heart border. (B) Electrocardiogram was normal with a heart rate of 85 beats/min.
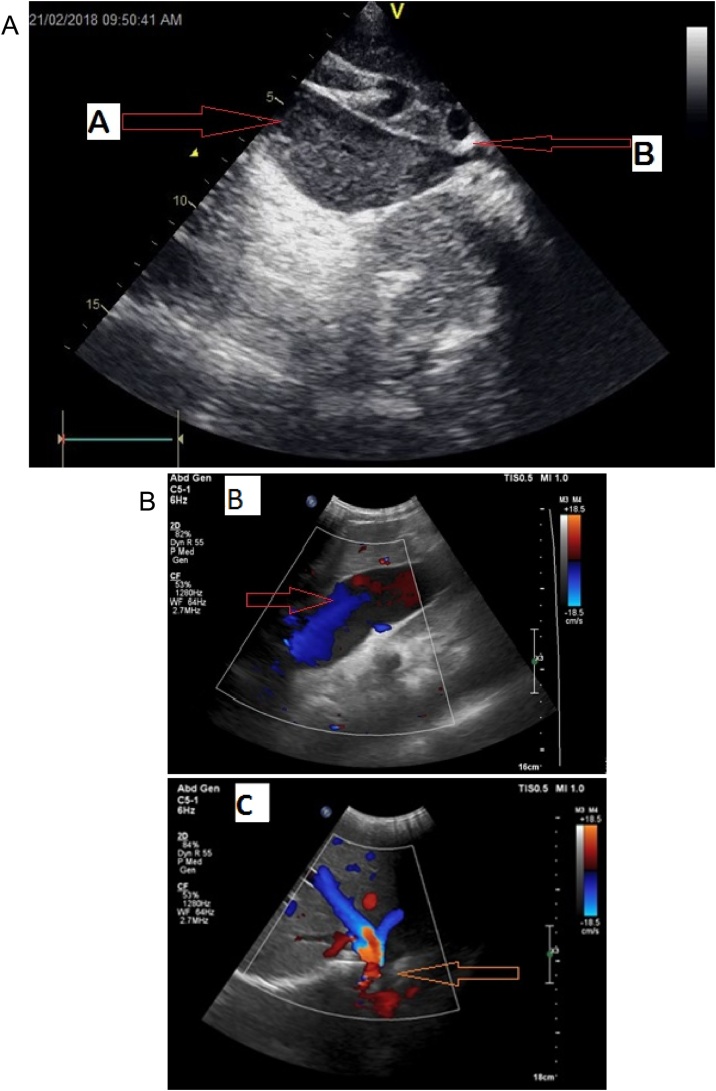
Fig. 3.
(A) Gray-scale images in 2D echocardiogram showing aneurysmal dilatation of inferior vena cava (arrow A) and proximal obstruction to the inferior vena cava (arrow B). Color Doppler ultrasonography images showing (B) aneurysmal dilatation of the inferior vena cava and (C) dilated mid and left hepatic vein (arrow).
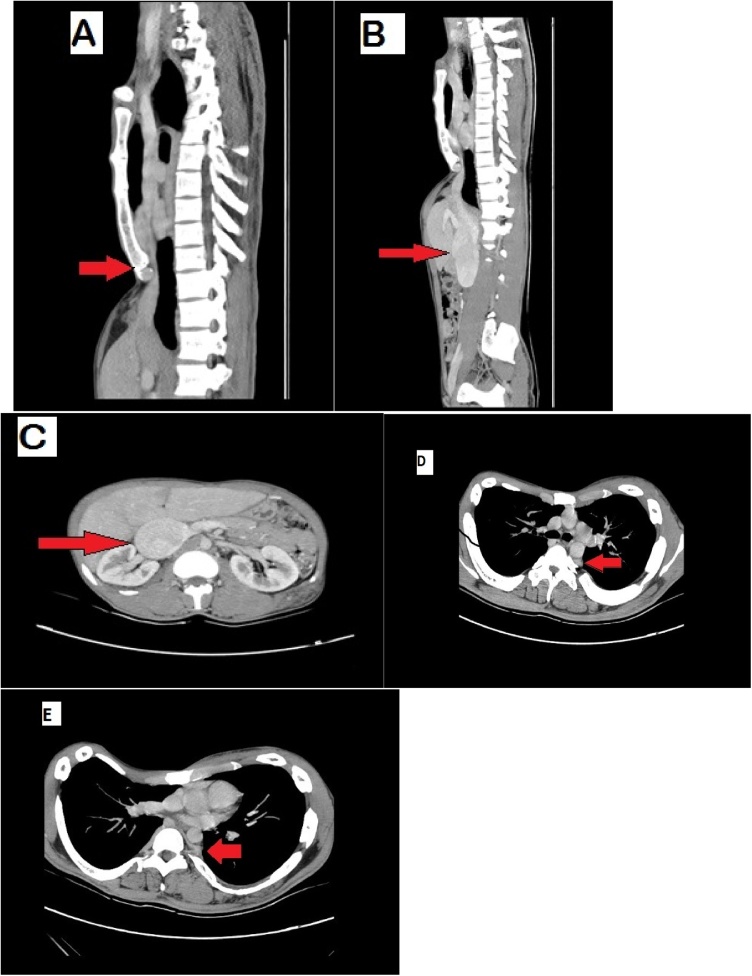
Fig. 4.
Coronal section of post-contrast phase computed tomography showing (A) proximal focal narrowing at the level of the xiphisternum (anteroposterior diameter: 9 mm and cross-sectional area: 0.9 cm2) (B) fusiform aneurysmal dilatation of the infra-hepatic segment of inferior vena cava measuring 6.6 × 4.7 cm extending to a length of 12.6 cm with associated dilatation of its tributaries and multiple venous collaterals (C) fusiform aneurysmal dilatation of the infra-hepatic segment of inferior vena cava in the axial section. (D) and (E) Axial sections showing one dilated venous collateral and collateral draining to azygos vein.
As per the literature review, the correct treatment is a surgical correction of both IVC aneurysm as well as pectus excavatum deformity. However, the patient opted for conservative management. He was treated with antiplatelets and oral anticoagulation and advised close follow-up.
Discussion
Venous aneurysms are rare and are characterized as persistent isolated venous dilatation at least twice the normal diameter (normal range: 1.5–3.7 cm) [3]. The true incidence of IVC aneurysms is yet to be determined. Literature suggests that IVC aneurysms rarely occur along with other congenital anomalies. Clinically, IVC aneurysms are important entities because of the frequent complications of thrombosis, rupture, and pulmonary embolism. In addition, most of the patients with IVC aneurysm remain clinically asymptomatic and diagnosis is made only by chance [4].
There have been rare reports of dynamic compression of IVC in patients with pectus excavatum and reduced exercise tolerance [5] and even syncope in an individual [6]. There is also a case report that describes lower extremity edema in a child due to IVC compression by pectus excavatum [7]. However, there are no reports of pectus excavatum being associated with IVC aneurysm. We postulate that the proximal obstruction by the pectus excavatum of the IVC as the most likely etiology in our case.
Based on the etiology, Thompson and Lindenauer [8] have classified IVC aneurysms in three groups as congenital, acquired, and arteriovenous fistula-dependent. It is suggested that congenital IVC anomalies, trauma, proximal stenosis or obstruction of IVC, prolonged right heart failure, or immune disorders creating injury to the venous wall may lead to the development of acquired aneurysms. Based on the anatomic and embryological properties, Gradman and Steinberg [9] classified IVC aneurysms into 4 groups:
Type I: suprahepatic IVC aneurysm without venous obstruction.
Type II: aneurysms with concurrent IVC interruption below or above the level of hepatic veins.
Type III: aneurysms confined to infrarenal IVC without any concurrent venous anomaly.
Type IV: mixed lesions.
Drugs are prescribed either for the symptomatic relief or to prevent further progression and complications [3]. An extensive review of published cases recommends surgical treatment such as ligation, resection with end to end anastomosis, and resection plus interposition graft for all types of IVC aneurysms except type I, which can be managed conservatively [2], [3]. The review also suggests that the mean age at the time diagnosis of IVC aneurysm was 41 years and 62.5% of those cases were males [2]. Moreover, vascular abnormalities with ileo-caval thrombosis were reported in 20% of these patients [2], [3]. In our case, a 35-year-old asymptomatic man had presented with a severe form of pectus excavatum. He was diagnosed with Type II acquired IVC aneurysm with no evidence of thrombosis.
We emphasize the role of gray-scale 2D-echocardiography, ultrasound of the abdomen, and MSCT imaging in the diagnosis of IVC aneurysms. In particular, MSCT has an important role in making early diagnosis and therapeutic decisions in such patients. MSCT examination can help in the differential diagnosis of IVC aneurysms by its ability to define the origin of aneurysm and relationship with other structures. It can also evaluate vascular structures and adjacent organ parenchyma simultaneously by its virtue of rapid scanning and can allow imaging of many successive systems by its rapid data acquisition properties [4].
Acknowledgment
None.
Acknowledgments
Conflict of interest
The authors declare that there is no conflict of interest.
References
- 1.Oh K.S., Dorst J.P., Haroutunian L.M. Inferior vena caval varix. Radiology. 1973;109:161–162. doi: 10.1148/109.1.161. [DOI] [PubMed] [Google Scholar]
- 2.Montero-Baker M.F., Branco B.C., Leon L.L., Jr., Labropoulos N., Echeverria A., Mills J.L., Sr. Management of inferior vena cava aneurysm. J Cardiovasc Surg (Torino) 2015;56:769–774. [PubMed] [Google Scholar]
- 3.Gusani R., Shukla R., Kothari S., Bhatt R., Patel J. Inferior vena cava aneurysm presenting as deep vein thrombosis — a case report. Int J Surg Case Rep. 2016;29:123–125. doi: 10.1016/j.ijscr.2016.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Atalar M.H. Aneurysm of the inferior vena cava: imaging findings. Austin J Radiol. 2016;3:1053. [Google Scholar]
- 5.Yalamanchili K., Summer W., Valentine V. Pectus excavatum with inspiratory inferior vena cava compression: a new presentation of pulses paradoxus. Am J Med Sci. 2005;329:45–47. doi: 10.1097/00000441-200501000-00008. [DOI] [PubMed] [Google Scholar]
- 6.White J.A., Fine N.M., Shargall Y. Images in cardiovascular medicine. Pectus excavatum with compression of the inferior vena cava: a rare cause of recurrent syncope. Circulation. 2009;120:1722–1724. doi: 10.1161/CIRCULATIONAHA.109.866400. [DOI] [PubMed] [Google Scholar]
- 7.Iannucci G.J., Slesnick T.C., Kogon B., Samai C. Lower extremity edema in a child due to pectus excavatum. Ann Thorac Surg. 2015;99:e29–e30. doi: 10.1016/j.athoracsur.2014.11.051. [DOI] [PubMed] [Google Scholar]
- 8.Thompson N.W., Lindenauer S.M. Central venous aneurysms and arteriovenous fistulas. Ann Surg. 1969;170:852–856. doi: 10.1097/00000658-196911000-00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gradman W.S., Steinberg F. Aneurysm of the inferior vena cava: case report and review of the literature. Ann Vasc Surg. 1993;7:347–353. doi: 10.1007/BF02002888. [DOI] [PubMed] [Google Scholar]