Abstract
This study examined the level of acceptance of Health Information Technology (HIT) as tools for diabetes care and management, in six selected tertiary hospitals in southwestern zone of Nigeria. Using both quantitative and qualitative methods, this study was conducted amongst selected healthcare stakeholders namely Nurses, Doctors, Laboratory Scientists, Pharmacists, ICT unit Professionals, Medical Record Officers, and Type-2 diabetes out-patients available in the designated hospitals. Adapting Technology Acceptance and Chronic Care Models, the level of HIT acceptance by the respondents in the study area was measured in terms of Perceived Ease-of-Use, Perceived Usefulness, and the Perceived Unintended Consequences relating to HIT, while also considering the roles of the government, community and healthcare organizations. One hundred and fifty (150) respondents were examined, each for both Staff and Patients, and the factor variables studied on a 5-point Likert rating scale of measurement from 1 (Strongly Disagree) to 5 (Strongly Agree). The results revealed strong perception of Staff and Patients about HIT implementation and acceptance and showed that in some cases, the perception of Staff and patients about HIT acceptance are the same, while different in some. The study concluded that for acceptability of HIT, hospitals have to embark on ‘continuous’ training for the HIT users, so that users would familiarize themselves with the system, and it will be fully incorporated into their workflow. Based on the findings, a conceptual Health Information Technology Acceptance Framework for Chronic diseases' management, especially for diabetes mellitus was developed.
Keywords: Health profession, Information science
1. Introduction
Scientific evidences from around the world have discovered that the usage of Information and Communications Technology (ICT) and acceptance of modern-day technology are critical in improving healthcare services quality, particularly in the management of chronic diseases. Diabetes as a chronic disease, is characterized by relative or absolute deficiency in insulin action or secretion, hyperglycaemia, which may result to short or long term multi-organ and/or multi-system complications (James et al., 2010; Barnett et al., 2014; Bauer et al., 2014; Lazo et al., 2017; Punthakee et al., 2018). It is a lasting disorder that ensues when there is a rise in the level of glucose (i.e. sugar) present in the blood, as a result of failure of the body pancreas to produce insulin, which is a hormone that aids the circulation of glucose, starting from blood stream to all other body parts. Thus, the common opinion in the literature about diabetes is that, “it is a metabolic disorder triggered by various factors, characterized by prolonged rise in the levels of blood sugar, with disturbances in fat, carbohydrate and protein metabolism, caused by insulin defects in action, secretion, or both”. This is because all sugary foods are broken down into glucose in the blood, which insulin helps to get into the cells (Brereton et al., 2014; Chiarello-Ebner, 2016; Miller, 2016). Therefore, there is a need for diabetes to be managed by health information technology (HIT), which is because HIT can provide information about guidelines and safety, patient conditions, treatments and other relevant characteristics, and also send alerts and reminders to physicians at the point-of-care (Benson et al., 2018), so as to reduce the number of cardio-vascular complications and deaths caused by the disease. Health systems are only as effective as the services they provide and enhancing service delivery quality is a main strategy to attain Millennium Development Goals (WHO, 2008).
Healthcare quality has been defined from various perspectives and by several scholars. For example, Tabrizi et al. (2011) simply defined healthcare quality as doing the correct thing, at a correct time, in a correct way, while also in the correct place, for the correct patient, and having a correct outcome. Moreover, WHO (2008) stated that diverse terms such as acceptability, affordability and availability are frequently used to show whether people are getting the quality services they want. Acceptability of services primarily as a socio-psychological aspect, such that in healthcare services, the experience of the patient plays a crucial role in rating and assessing acceptability of services. Also, Affordability has to do with the capability of the client or patient to pay for the needed services. Furthermore, Availability connotes the reachability of services which meet the minimum standard. It includes requirements in terms of the basics of service delivery, comprising such as drugs and commodities, basic equipment and health workforce (availability and training), having the needed guidelines for treatment. In view of all these, patient-centered web-based HIT is being developed to encourage patients to manage and understand their disease, especially the involved complications, so as not to be poorly controlled (Davoody et al., 2016; Krist et al., 2016; Gray and Gilbert, 2018). Moreover, diabetes has been referred to by many researchers as a “patient-managing disease”, because of the roles a patient plays in managing his disease for optimal care (Unger, 2013; Hoffman, 2015; Benson et al., 2018). Hence, there is a need to devise a method for diabetes management that will empower the patients in managing their disease.
Consequently, HIT has been known to be a vital component of patient-centred resource in managing diabetes (Nutting et al., 2011; Barello et al., 2012). However, in Nigeria, studies have shown that much has not been done in the area of HIT applications in the health sector. Thus, several studies have revealed that care quality provided for diabetes patients in many Nigerian hospitals is not adequate, because most hospitals still use paper record keeping in managing diabetes (Pradeepa et al., 2011). This is because as the diabetes population is increasing, there is a need to discover ways of improving efficiency and quality of diabetes management, which paper records management might not be able to handle. For instance, paper record system does not allow having a database of diabetes cases in the country, while also making urgent medical referral cases difficult, among others. Therefore, the treatment and management of diabetes are not adequate in Nigeria (Ogbera and Ekpebegh, 2014), because there is low adoption of this Health Information System in the Nigerian health sector. This sub-optimal management has forced many Nigerians to go abroad for their disease management, and the people that cannot afford to go abroad seek other methods for their disease management, which include religious way of management.
Religion-based medicine has been in existence in several communities in Nigeria, as a result of the reaction to people health needs (Ezuruike and Prieto, 2014). Therefore, unlike in the developed countries, where diabetes care is mostly sought in hospitals, a rather different, mixed approach is prevailing in Nigeria, because many Nigerians often complement hospital care with treatment from churches and mosques, but mainly from traditional doctors. In this context, Traditional medicine refers to “practices and approaches that apply separately, or in combination, plant, animal, and mineral-based medicines, spiritual therapies, manual techniques and exercises to diagnose, prevent, and treat diabetes, and generally to maintain or enhance well-being” (Fokunang et al., 2011). These people (traditional healers) are usually consulted for diagnosis, treatment and/or management of diabetes. This is because of the ability of these traditionalists in dealing with the unseen, and the supernatural, thus, they are usually highly respected in the community (Agbor and Naidoo, 2011). However, despite all these diabetes management techniques in use in Nigeria, desired care outcomes are still not acceptable and due to this, the satisfaction of patient is not adequate, therefore leading to different diabetes complications for both diagnosed and undiagnosed patients (Ogbera and Ekpebegh, 2014).
A study by Idowu et al. (2008) noted that one of the reasons for Nigerian health sector to be lagging behind in the application of Health Information Technology is its inability to sustain the HIT tools that have come into being since the inception of Information and Communications Technology, ICT. In other words, many ICT tools that have been used in the Nigerian health sector could not be sustained, and thus failed, despite the huge investment on them, majorly due to the reason that they were not adequately accepted by the users. Therefore, there is fear of sustainability for the emerging ones, because their level of acceptance is not known. Thus, in this study, we assessed the acceptance for sustainability of HIT so as to encourage optimal management of diabetes mellitus (simply called diabetes); evaluates how HIT can be used for the management of diabetes in Nigerian health sector; and then develop a model including the role of government, community and healthcare organizations in delivering optimal health services for diabetes management.
This study is significant in that most of the studies on Technology acceptance only focus on the constructs used by Technology Acceptance Model (TAM), which are Perceived ease-of-use, Perceived Usefulness, Behavioural Intention to use the system and finally, Attitude towards usage. However, this study seeks to introduce a new concept of Perceived Unintended Consequences of Technology, and its impact on Technology Acceptance was evaluated. Though, for this study, a particular chronic disease (diabetes mellitus), and a specific geo-political zone (Southwest), out of the six Nigerian geopolitical zones, are taken so as to have in-depth knowledge and studies about how the disease is thoroughly managed in the zone. So, a further study could look into some other chronic diseases, and likewise some other geopolitical zones. Moreover, the study was only conducted among Nurses, Doctors, Laboratory scientists, Pharmacists, ICT unit professionals, Medical Record officers, and adult Type-2 diabetes out-patients available in the designated hospitals, other health stakeholders could also be considered in the future.
2. Theory
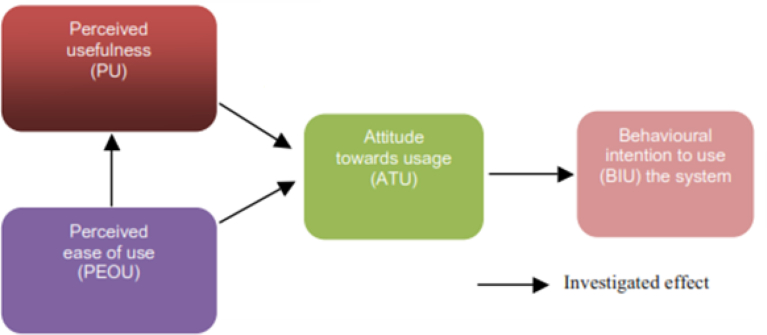
There are various frameworks that discussed the acceptability of any technology in any sector, but one of the foundational models, on which other researchers are building on, was established by Davis et al. (1989), called the Technology Acceptance Model. This has been utilized by some researchers to explore and interpret physicians' acceptance of information technology (For example, Liu and Cheng (2015)). Therefore, the conceptual frameworks, adapted from Davis et al. (1989) Technology Acceptance Model; and Wagner (1998) Chronic Care Management Model (CCM) were adapted for this study. TAM is used to describe computer-usage behaviour and the factors related to technology acceptance (Fig. 1). According to this model, any technology's acceptance and usage (health information technology inclusive) is predominantly explained by behavioural intention to use the system (BIU). This behavioural intention is formed as a result of the attitude towards the usage of system (ATU). This attitude towards the usage of the system, in turn, is controlled by two factors: Perceived ease of use (PEOU) and Perceived usefulness (PU). By manipulating these two, system developers will be able to have better control of users' beliefs (perception) of the system, and consequently, over their attitude towards usage and behavioural intention to use the system.
Fig. 1.
Technology acceptance model (Modified after Davis et al., 1989).
Therefore, the important keywords for this TA model are: Perceived ease-of-use, Perceived Usefulness, Attitude towards system usage and lastly, Behavioural Intention to use a system. Perceived Usefulness is defined according to (Davis, 1989) as the level that a technology user trusts that using the technology would improve his job performance. Similarly, Perceived ease of use refers to the level to which a technology user has confidence that using the technology will be effort free (Davis, 1989). Although Health Information Technology (for example in the forms of Decision Support-incorporated Electronic Medical Record System and mobile technologies) have been proven to enhance quality diabetes management. However, the perception of respondents regarding the technology is very important and still needs to be evaluated. Thus, Perceived ease of use and Perceived usefulness can be considered to be cognitive factors.
On the other hand, Attitude towards usage can be defined also as the level to which a technology user can associate and evaluate a target system with his job (Davis, 1993). Whereas, Attitude towards usage is known to be a factor that guides future behaviour, or what finally leads to a certain behavior (Dinev et al., 2016). In Technology Acceptance Model, attitude towards usage is also considered to be the assessed effect of negative or positive individuals' feelings in having a certain behaviour, which is controlled by perceived usefulness and perceived ease of use. Likewise, Behavioural Intention is the cognitive user's readiness to have a specific behaviour, which is considered to be the direct antecedent of behavior (Thoolen et al., 2009; Dinev et al., 2016; Tommasetti et al., 2018). It is largely determined by perceived usefulness and attitude.
However, several researches have revealed many undesired and unanticipated consequences of HIT implementation (Koppel and Chen, 2016; Taneja, 2018; Tubaishat, 2019). Therefore, there is another concept introduced and developed from this study to complement the findings and model of Davis et al. (1989). The concept is known to be the “Perceived Unintended Consequences of technology”, and it simply refers to the unintended consequences of Health Information Technology in this case. These undesirable and unanticipated consequences, usually called unintended consequences (Tubaishat, 2019), are what frequently affect patient safety practices and also sometimes harm them (Virginio Jr and Ricarte, 2015; Taneja, 2018), just like any other technology, that there is risk associated to it, thus no perfect technology.
The lack of adoption and acceptability of Health Information Technology in the Nigerian health sector could be attributed to the reality and users' awareness of some of these unintended consequences that HIT might bring after implementation. Thus, this measure of acceptability using this model is very important for both the Information Technology (IT) vendor who would like to know whether demand will rise or fall; and the information system manager who would like to evaluate the acceptability of these vendor products among its subordinates. In this study, to asses the acceptance level of HIT tools for the management of diabetes mellitus, the Perceived Ease-of-use, Perceived Usefulness and Perceived Unintended Consequences of HIT were measured and modified. The variables measured for each parameter are presented in Table 1, measured on a Likert rating scale of 1 through 5, from Strongly Disagree to Strongly Agree, with six items under each.
Table 1.
Measurement variables for acceptability of HIT.
| S/N | Perceived Usefulness |
Perceived Ease-of-use |
Perceived Unintended Consequences of HIT |
|---|---|---|---|
| i. | Using HIT would allow me to complete tasks more quickly | Learning to use HIT will not be difficult for me | Implementation of HIT could lead to job loss |
| ii. | Using HIT would improve my job performance | I will find it easy to use HIT for what I want it to do | HIT will even create more errors than expected |
| iii. | Using HIT would increase my job productivity | My interaction with HIT will be understandable and clear | HIT will be a third party between me and my patient, thus will be a distraction |
| iv. | HIT would enhance my job effectiveness | I would find HIT flexible to interact with | HIT would be taking more of my time in typing and recording |
| v. | Using HIT will make it easier to do my job | It will be easy for me to be skilful at using HIT | HIT would introduce more patient data security breaches |
| vi. | Generally, I will find HIT useful in my job | Generally, I will find HIT easy to use | HIT would negatively affect the way I express my thoughts in clinical notes and how I communicate with my colleagues |
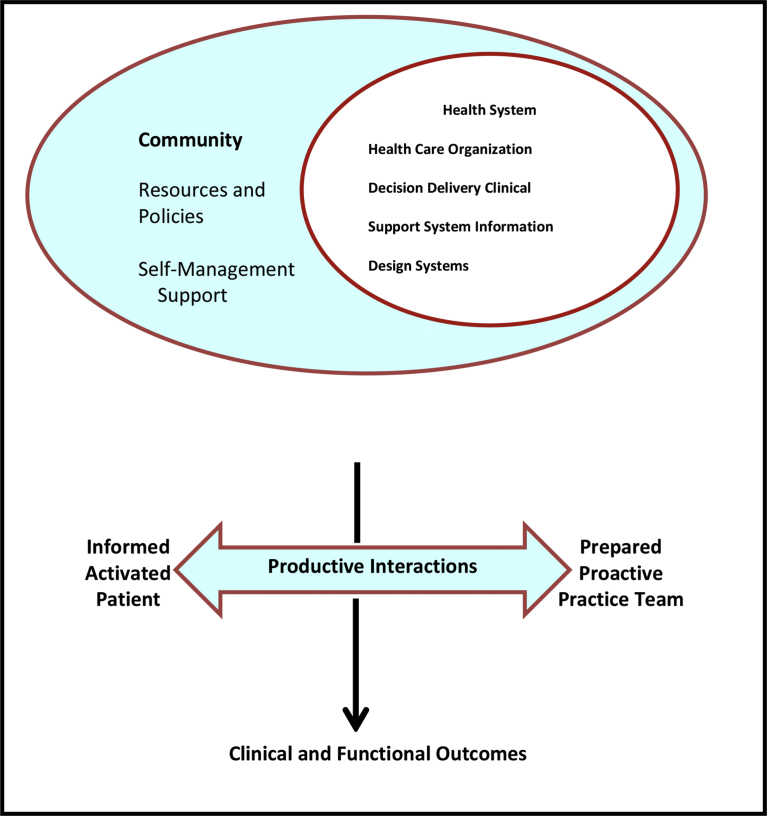
Although Health information technology (HIT) has been reported by several researchers, to be a way of improving the healthcare quality, reducing cost and enhancing patient safety (Menachemi et al., 2015). However, while important, HIT alone is not sufficient for the management of chronic diseases like diabetes, it has to be supported by some proven components according to the Chronic Care Model developed by (Wagner, 1998), which is another framework used in this study, as illustrated in Fig. 2.
Fig. 2.
The Chronic Care Model, CCM (Wagner, 1998).
The Chronic Care Model (CCM) has been serving as a theoretical framework that positively transforms healthcare services for chronic disease populations (Zgibor et al., 2017). Historically, CCM was developed to review the health interventions given to chronic disease patients, to bring about optimal care for them. Broadly, according to Wagner (1998), there are four categories of multicomponent changes that form the basis of CCM, so as to bring improved care: Enhancing the skills of health practitioners; empowering patients by supporting and educating them; Making healthcare services be more planned and team-based; and Making better use of Health information Technology.
A study by Group Health Research Institute (GHRI, 2015), made the first category explicit that the skills of health practitioners is observed when the treatment decisions is based on clear and established guidelines, buttressed by clinical research. These guidelines must also be deliberated with the involved patients, so that they can comprehend the principles involved in their care. Therefore, the skills of the health practitioners that make treatment decisions are enhanced by ongoing training, so as to be up-to-date on the latest guidelines and principles of medical education.
The second category is ‘empowering patients by supporting and educating them’. Here, all the patients with chronic illness decide to have behaviours that have implications on their health (self-management). Thus, the chronic disease management depends to a substantial level, on the efficacy of self-management. Effective self-management support therefore connotes more than giving patients information on what to do, but also means patients admitting a central role in their care, a one that nurtures a sense of accountability for their health management. Also, it comprises the use of established programs that give basic information, strategies and passionate support for people with chronic disease. Thus, using a collective approach, patients and healthcare providers work together to state the problems, institute goals, set priorities, form management plans and then resolve problems together (Dent and Pahor, 2015; Renedo et al., 2015).
Making healthcare services to be more planned and team-based is the third category. Managing the health of people living with chronic diseases requires a strategy that is basically reactive, which means responding mostly when a patient is sick - to the one that is proactive, and focuses on keeping individuals all the times as healthy as possible. This necessitates only not deciding what care is needed, but also spelling out responsibilities to ensure that the patient gets the right care by using structured and planned interactions. Moreover, it requires following up the management plans by the health practitioners, so patients are not left alone immediately they leave the hospitals' premises. Furthermore, complex patients might need more thorough management, say for a period of time, so as to enhance clinic care and self-management. Thus, health literacy and cultural sensitivity are two important emergent themes in health care. Healthcare providers are progressively thus being called to respond commendably to the different cultural and linguistic needs of patients.
The last category is making better use of HIT. Optimal chronic illness management is not possible practically without HIT that assures timely access to important data of individual patients (Desmedt et al., 2017; Braunstein, 2018). An all-inclusive clinical information system, also known as HIT, can augment patients' care, by giving reminders for the needed services on time, while also summarizing data that will help in tracking and planning care. Also, at the practice population level, HIT can detect groups of patients that need further care to enable performance monitoring and quality enhancement programs. Therefore, CCM is currently and widely used in chronic disease management, as it is being applied for diabetes management in this study. It helps governments in their decisions in formulating policies, which will capture the aforementioned four aspects, in order to bring about optimal chronic disease management (Zwar et al., 2017).
3. Materials and methods
3.1. Data acquisition
To obtain primary data for this study, a mixed method of quantitative and qualitative data collection using multi method-qualitative data was used. Therefore, three research methods were used in the study: Questionnaire, observation and structured interviews. The survey, which was cross-sectional, cut across some healthcare stakeholders including the Nurses, Doctors, Laboratory scientists, Pharmacists, ICT unit professionals, Medical Record officers, and Type-2 diabetes out-patients of the hospital organization. Due to its large population, Nigeria is grouped into six geopolitical zones namely: North-central, Northeastern, Northwestern, Southeastern, Southsouth and Southwestern. Out of these, Southwestern zone was studied. A particular single geopolitical zone (southwestern zone) was taken for detailed study and analysis, and the zone comprises six states: Ogun, Osun, Lagos, Ekiti, Oyo and Ondo States. This region lies to the south and to the west of the River Niger in Nigeria. As afore-mentioned, this study was conducted among Nurses, Doctors, Laboratory scientists, Pharmacists, ICT unit professionals, Medical Record officers, and adult Type-2 diabetes out-patients of six selected tertiary hospitals in the geopolitical zone (Southwestern zone). These selected tertiary hospitals in these mentioned states were visited to have detailed study and analysis, while the research participants were the healthcare stakeholders aforementioned. Based on the background knowledge about the number of Staff (e.g. Doctors and Nurses) and patients available for a diabetes clinic on a particular day in each of the selected hospitals, the minimum number of samples was then taken across all the hospitals, unlike in the totality of the whole hospitals.
For questionnaire administration, a random sampling was used in a situation whereby the number available is more than the number of respondents needed for the survey. For instance, where there are more than 25 patients in the clinic, or the number of nurses/doctors in a particular clinic are more than the three needed and so on, random sampling was used to select the respondents. Three hundred (300) copies of questionnaire were distributed amongst 18 Doctors, 18 Nurses, 30 Laboratory Scientists, 30 Pharmacists, 30 ICT Unit Professionals, 18 Medical Record Officers, and 150 Patients, with 300 respondents altogether. The response rate was 100%, due to the ethical clearances already had from the management of each of the hospitals. These clearances were understood to be approval granted before any research, relating to human subjects, is carried out in the various departments.
Observation method was also employed to confirm the findings obtained from other research instruments used for the study. For example among others, observation method was used to confirm the questionnaire findings on the aspect(s) of HIT in use in the hospitals (e.g. EMR, Electronic prescription etc). Therefore and most importantly, the observation method served as a facility assessment of the HIT options in use, using a checklist. In order to explore the research questions further, semi structured interviews were used to confirm the results from the questionnaire and observation methods of data collection. This is because semi-structured questions give the respondents opportunity to demonstrate their understanding of the research themes, for there is no strict following of the set structured questions.
To have valid and reliable data from questionnaire, Sekaran and Bougie (2016) suggested that the design of a questionnaire in terms of its wordings and type of questions asked can determine its validity and reliability. So when the questionnaires were being designed, it was made sure that the chosen words were not clumsy or ambiguous, and different types of questions (Likert rating scale, open questions etc.) were formed so that the respondents would not be bored while answering the questions. The questionnaire included demographic questions and itemized questions on the acceptability and sustainability of Health Information Technology. This is based on the technology acceptance model of Davis et al. (1989) using Perceived Usefulness and Perceived ease-of-use of the technology along with Perceived unintended consequences that the HIT might introduce. Moreover, information on the effects of government policy interventions on acceptability and sustainability of Health Information Technology was also gathered from the questionnaire.
3.2. Data analysis
In analyzing the qualitative data from the semi-structured interviews, the interviews were transcribed verbatim using Nvivo software Version 11.0. The transcription were then organized and categorized into themes/concepts. To achieve this, three major steps were taken: Verbatim transcripts were first of all independently coded. This aided identification of key themes and concepts that were used during the interview discussions. The second step was to create a coding schema based on the emergent themes and subthemes that came up during the interview, and thirdly, to compare the results of these independent coding with the data from other methods used for the study.
The Cronbach's alpha analysis was run on all the variables and the result generated is presented in Table 2 with Staff and Patients differentiated to indicate the varying questions asked. This is necessary to measure the internal consistency and reliability of the entire scale. For instance, Pallant (2013) suggested a reliability score of 70% or more to be acceptable. From the Table 2, all the items had Cronbach's alphas of .70 or more, thus making the scales to be suitable for the survey.
Table 2.
Cronbach's alpha reliability analysis for the studied variables.
| Research Objective | No of Items Considered | Cronbach's Alpha |
|
|---|---|---|---|
| Staff | Patients | ||
| Level of HIT Acceptance | 37 | 0.825 | 0.710 |
4. Results and discussion
4.1. Level of HIT acceptance by respondents in the study area
The variables used in this study to measure HIT acceptance differ from Staff to patients. To measure the Perceived Usefulness, the respondents were categorised as Staff and Patients. The Staff in this context comprises of the Medical Record officers, Pharmacists, Laboratory Scientists, ICT Unit Professionals, Nurses and Doctors under study in the selected hospitals. Six (6) factors were examined under the Perceived Usefulness parameter for each of them. The mean ranking, in descending order, of the variables measured among staff are presented in Table 3. There were one hundred and fifty (150) respondents (N) examined (each for both Staff and Patients) on a 5-point Likert rating scale of measurement ranging from 1 (Strongly Disagree) to 5 (Strongly Agree). It is obvious that Staff agreed on Job easiness with 4.60 mean, Job Performance Improvement (Mean 4.59), Quick Task Accomplishment (Mean 4.41) and General Job Usefulness with 4.03 mean (Table 3). It could be concluded from the selected variables that the Staff perceive HIT to be the one that will make their job easy, improve their job performance, make them accomplish their daily task quickly and be useful generally in performing their daily tasks, which is in agreement with the studies of Meeks et al. (2014) and Palojoki et al. (2017). Therefore, if Staff is to accept the HIT technology, all these have to be put into consideration.
Table 3.
Perceived usefulness of HIT among the staff.
| S/N | Perceived Usefulness | N | Min | Max | Mean |
|---|---|---|---|---|---|
| 1. | Job Easiness | 150 | 1 | 5 | *4.60 |
| 2. | Job Performance Improvement | 150 | 1 | 5 | *4.59 |
| 3. | Quick Task Accomplishment | 150 | 1 | 5 | *4.41 |
| 4. | General Job Usefulness | 150 | 1 | 5 | *4.03 |
| 5. | Job Effectiveness Enhancement | 150 | 1 | 5 | 3.97 |
| 6. | Job Productivity Increment | 150 | 1 | 5 | 3.91 |
5.0: Strongly Agreed, 4.0–4.99: Slightly Agreed, 3.0–3.99: Neither Agreed nor Disagreed, 2.0–2.99: Slightly Disagreed and 1.0–1.99: Strongly Disagreed.
Mean for Agreed items.
The values for patients agreed mostly on Disease Management Plans Improvement and Easy Disease Management Plans, which have the same mean of 4.81 (Table 4). This result might be due to the importance the patients place on their disease management plans, to be easy and improved. This result is in conformity with what Free et al. (2013) suggested that for patients to see a technology as being useful, it has to enhance their disease management plans. Following these two is ‘Seeing Healthcare Provider quickly’, which has a mean value of 4.77. This might be so because seeing healthcare quickly might be an important dictator of having interest to come to the clinic for treatment, because it will determine if coming to the clinic would be time-consuming and stressful to the patients.
Table 4.
Perceived usefulness of HIT among the patients.
| S/N | Perceived Usefulness | N | Min | Max | Mean |
|---|---|---|---|---|---|
| 1. | Disease Management Plans Improvement | 150 | 1 | 5 | *4.81 |
| 2. | Easy Disease Management Plans | 150 | 1 | 5 | *4.81 |
| 3. | Seeing Healthcare Provider Quickly | 150 | 1 | 5 | *4.77 |
| 4. | Disease Management Plans Enhancement | 150 | 1 | 5 | 1.19 |
| 5. | Useful in Disease Management Plans | 150 | 1 | 4 | 1.17 |
| 6. | Disease Management Plans Effectiveness | 150 | 1 | 5 | 1.16 |
5.0: Strongly Agreed, 4.0–4.99: Slightly Agreed, 3.0–3.99: Neither Agreed nor Disagreed, 2.0–2.99: Slightly Disagreed and 1.0–1.99: Strongly Disagreed.
Mean for Agreed items.
For measuring the Perceived Ease-of-Use, the respondents were also categorised as Staff and Patients. Six factors were also examined under the Perceived Usefulness parameter for each of them. The mean ranking, in descending order, of the factor variables measured among Staff are presented in Table 5. There were also one hundred and fifty (150) respondents (N) examined (each for both Staff and Patients) on a 5-point Likert rating scale of measurement ranging from 1 to5; Strongly Disagree to Strongly Agree. From Table 5, it is clear that Understandable and Clear Interaction (Mean of 4.67), Flexible Interaction (Mean 4.60), Easy Usage (Mean 4.56), General Easiness (Mean 4.07) and Easy Learning (Mean 4.03) were paramount ease-of-use parameters among Staff in the selected hospitals. Thus, it could be concluded from the selected options of the Staff that they perceive HIT to be interactive, flexible and even educative. These are in line with what Idowu et al. (2008)suggested that one of the reasons why all the HIT that were introduced into the health sector since the inception of ICT, were not accepted was because they were not interactive and flexible.
Table 5.
Perceived ease-of-use of HIT among the staff.
| S/N | Perceived Ease-of-Use | N | Min | Max | Mean |
|---|---|---|---|---|---|
| 1. | Understandable and Clear Interaction | 150 | 1 | 5 | *4.67 |
| 2. | Flexible Interaction | 150 | 1 | 5 | *4.60 |
| 3. | Easy Usage | 150 | 1 | 5 | *4.56 |
| 4. | General Easiness | 150 | 1 | 5 | *4.07 |
| 5. | Easy Learning | 150 | 1 | 5 | *4.03 |
| 6. | Skills Enhancement | 150 | 1 | 5 | 3.95 |
5.0: Strongly Agreed, 4.0–4.99: Slightly Agreed, 3.0–3.99: Neither Agreed nor Disagreed, 2.0–2.99: Slightly Disagreed and 1.0–1.99: Strongly Disagreed.
Mean for Agreed items.
Similarly, Table 6 shows the items under Perceived Ease-of-Use that the patients under study selected based on their mean rankings. Similar to the selection of Staff, the patients also agreed that ‘Understandable and Clear Interaction’ and ‘Flexible Interaction’ of the same mean 4.77 to be their priorities, followed by Easy Usage (mean 4.59), as similarly confirmed by Idowu et al. (2008) that technology interactivity and flexibility are important criteria for HIT acceptance.
Table 6.
Perceived ease-of-use of HIT among the patients.
| Perceived Ease-of-Use | N | Min | Max | Mean |
|---|---|---|---|---|
| Understandable and Clear Interaction | 150 | 1 | 5 | ∗4.77 |
| Flexible Interaction | 150 | 1 | 5 | ∗4.77 |
| Easy Usage | 150 | 1 | 5 | ∗4.59 |
| Skills Enhancement | 150 | 1 | 5 | 1.47 |
| General Easiness | 150 | 1 | 5 | 1.43 |
| Easy Learning | 150 | 1 | 5 | 1.20 |
5.0: Strongly Agreed, 4.0–4.99: Slightly Agreed, 3.0–3.99: Neither Agreed nor Disagreed, 2.0–2.99: Slightly Disagreed and 1.0–1.99: Strongly Disagreed.
Mean for Agreed items.
Likewise, the respondents were also categorised as Staff and Patients to measure the Perceived Unintended Consequences of HIT; and six factors were examined for Staff and only five for patients. The mean ranking, in descending order, of the factor variables for Staff are presented in Table 7. So from the Table 7, Data Insecurity and Job loss (of the same mean 4.60) are the major fear of Staff when HIT is implemented. According to Terry et al. (2012), this might be because with implementation of HIT, the private health data of patients can be leaked out just at the click of a mouse, if proper security measures are not in place. Moreover, Staff may be fearful about them losing their job, especially jobs that are not ICT-related when HIT is implemented, emphasizing the fact that manual jobs involving people may eventually be taken over by computerization, thus resulting in fewer employment opportunities.
Table 7.
Perceived unintended consequences of HIT among the staff.
| S/N | Perceived Unintended Consequence | N | Min | Max | Mean |
|---|---|---|---|---|---|
| 1. | Data Insecurity | 150 | 1 | 5 | ∗4.60 |
| 2. | Job Loss | 150 | 1 | 5 | ∗4.60 |
| 3. | Time Consuming | 150 | 1 | 5 | ∗4.59 |
| 4. | Lack of Thought Expression and Communication | 150 | 1 | 5 | 2.97 |
| 5. | Error Creation | 150 | 1 | 5 | 2.93 |
| 6. | Third Party | 150 | 1 | 5 | 2.28 |
5.0: Strongly Agreed, 4.0–4.99: Slightly Agreed, 3.0–3.99: Neither Agreed nor Disagreed, 2.0–2.99: Slightly Disagreed and 1.0–1.99: Strongly Disagreed.
Mean for Agreed items.
However, Staff could go on ICT training or reshuffle their posts to avoid job loss after HIT implementation. Moreover, the Staff also had the fear of HIT consuming more time after implementation. This might be due to the fact that patient data will need to be keyed in one by one, and it would be slower for Staff that is not fast in typing, because of the huge amount of time involved in data entry by the physicians, which is obviously far more than what they had (Greiver et al., 2011). However, they further suggested creating a data-typing post that the person would be dedicated to keying in of patient data, as one of the solutions.
Table 8 illustrates the main fear of patients after HIT implementation, which is firstly ‘Data security breaches’, as similar to the Staff. This might be according to what Beck et al. (2016) explained that health data to patients are very crucial, and that they might cause some embarrassment, ruin or damage, for example, to the patient's career, discharge from work etc, if disclosed unlawfully. ‘Third Party’ is followed with a mean of 4.49 as an unintended consequence. This might be so in that in the countries that HIT is already implemented, patients see the HIT implementation as a third party, because instead of the physician to be looking at them during visit and be observing them, he continues to gaze at the computer screen, keying in the patient data (Abelson, 2010; Drapcho, 2016). The ‘Error creation’ variable chosen (mean 4.02) might arise for example, from erroneous copying/cutting and pasting, if care is not taken (Lowry et al., 2017).
Table 8.
Perceived unintended consequences of HIT among the patients.
| S/N | Perceived Unintended Consequences |
N | Min | Max | Mean |
|---|---|---|---|---|---|
| 1. | Data Security Breaches | 150 | 1 | 5 | ∗4.56 |
| 2. | Third Party | 150 | 1 | 5 | ∗4.49 |
| 3. | Error Creation | 150 | 1 | 5 | ∗4.02 |
| 4. | Lack of Healthcare Provider Relationship | 150 | 1 | 5 | 1.71 |
| 5. | Time Consuming | 150 | 1 | 5 | 1.46 |
5.0: Strongly Agreed, 4.0–4.99: Slightly Agreed, 3.0–3.99: Neither Agreed nor Disagreed, 2.0–2.99: Slightly Disagreed and 1.0–1.99: Strongly Disagreed.
Mean for Agreed items.
Thus in overall, the perception of Staff and Patients about HIT implementation are summarised in Tables 9 and 10, respectively so that the order of importance of each factor is reflected. Hence, from Staff perception table (Table 9), it is obvious that it is the ease-of-use (Understandable and Clear Interaction) that is paramount to Staff. That is, no matter be the usefulness of the technology, if it is not easy to understand and easy to interact with, then its usefulness is useless as confirmed by Meeks et al. (2014), as this will determine the HIT acceptance and sustainability among staff. Whereas for patients as in Table 10, ‘Disease Management Plans Improvement’ and ‘Easy Disease Management Plans’ (both with mean 4.81) emerged as the most crucial, which are both perceived usefulness parameters. This is an indication that it is the disease management that is crucial to patients, because it will determine their longevity in life. Thus, they are ready to accept any system that will enhance their survival because the disease is lifelong.
Table 9.
Overall perception of staff about HIT implementation.
| S/N | Perception | N | Min | Max | Mean |
|---|---|---|---|---|---|
| 1. | Understandable And Clear Interaction | 150 | 1 | 5 | ∗4.67 |
| 2. | Flexible Interaction | 150 | 1 | 5 | 4.60 |
| 3. | Data Insecurity | 150 | 1 | 5 | 4.60 |
| 4. | Job Loss | 150 | 1 | 5 | 4.60 |
| 5. | Job Easiness | 150 | 1 | 5 | 4.60 |
| 6. | Time Consuming | 150 | 1 | 5 | 4.59 |
| 7. | Job Performance Improvement | 150 | 1 | 5 | 4.59 |
| 8. | Easy Usage | 150 | 1 | 5 | 4.56 |
| 9. | Quick Task Accomplishment | 150 | 1 | 5 | 4.41 |
| 10. | General Easiness | 150 | 1 | 5 | 4.07 |
| 11. | Easy Learning | 150 | 1 | 5 | 4.03 |
| 12. | General Job Usefulness | 150 | 1 | 5 | 4.03 |
| 13. | Job Effectiveness Enhancement | 150 | 1 | 5 | 3.97 |
| 14. | Skills Enhancement | 150 | 1 | 5 | 3.95 |
| 15. | Job Productivity Increment | 150 | 1 | 5 | 3.91 |
| 16. | Thought Expression and Communication | 150 | 1 | 5 | 2.97 |
| 17. | Error Creation | 150 | 1 | 5 | 2.93 |
| 18. | Third Party | 150 | 1 | 5 | 2.28 |
5.0: Strongly Agreed, 4.0–4.99: Slightly Agreed, 3.0–3.99: Neither Agreed nor Disagreed, 2.0–2.99: Slightly Disagreed and 1.0–1.99: Strongly Disagreed.
Highest Mean for Agreed items.
Table 10.
Overall perception of patients about HIT implementation.
| S/N | Perception | N | Min | Max | Mean |
|---|---|---|---|---|---|
| 1. | Disease Management Plans Improvement | 150 | 1 | 5 | ∗4.81 |
| 2. | Easy Disease Management Plans | 150 | 1 | 5 | ∗4.81 |
| 3. | Understandable and Clear Interaction | 150 | 1 | 5 | 4.77 |
| 4. | Seeing Healthcare Provider Quickly | 150 | 1 | 5 | 4.77 |
| 5. | Flexible Interaction | 150 | 1 | 5 | 4.77 |
| 6. | Easy Usage | 150 | 1 | 5 | 4.59 |
| 7. | Data Security Breaches | 150 | 1 | 5 | 4.56 |
| 8. | Third Party | 150 | 1 | 5 | 4.49 |
| 9. | Error Creation | 150 | 1 | 5 | 4.02 |
| 10. | Healthcare Provider Relationship | 150 | 1 | 5 | 1.71 |
| 11. | Skills Enhancement | 150 | 1 | 5 | 1.47 |
| 12. | Time Consuming | 150 | 1 | 5 | 1.46 |
| 13. | General Easiness | 150 | 1 | 5 | 1.43 |
| 14. | Easy Learning | 150 | 1 | 5 | 1.20 |
| 15. | Disease Management Plans Enhancement | 150 | 1 | 5 | 1.19 |
| 16. | Useful in Disease Management Plans | 150 | 1 | 4 | 1.17 |
| 17. | Disease Management Plans Effectiveness | 150 | 1 | 5 | 1.16 |
5.0: Strongly Agreed, 4.0–4.99: Slightly Agreed, 3.0–3.99: Neither Agreed nor Disagreed, 2.0–2.99: Slightly Disagreed and 1.0–1.99: Strongly Disagreed.
Highest Mean for Agreed items.
To assess the level of HIT acceptance of the users, the interviews findings suggested that the Staff are ready to accept the HIT because of their perception that it would be useful to them (based on the good news they have heard about the HIT from other countries that use the technology). This is paramount in the findings of the questionnaire that Staff perceive HIT to be the one that will make their job easy, improve their job performance, make them accomplish their daily task quickly and be useful generally in performing their daily tasks.
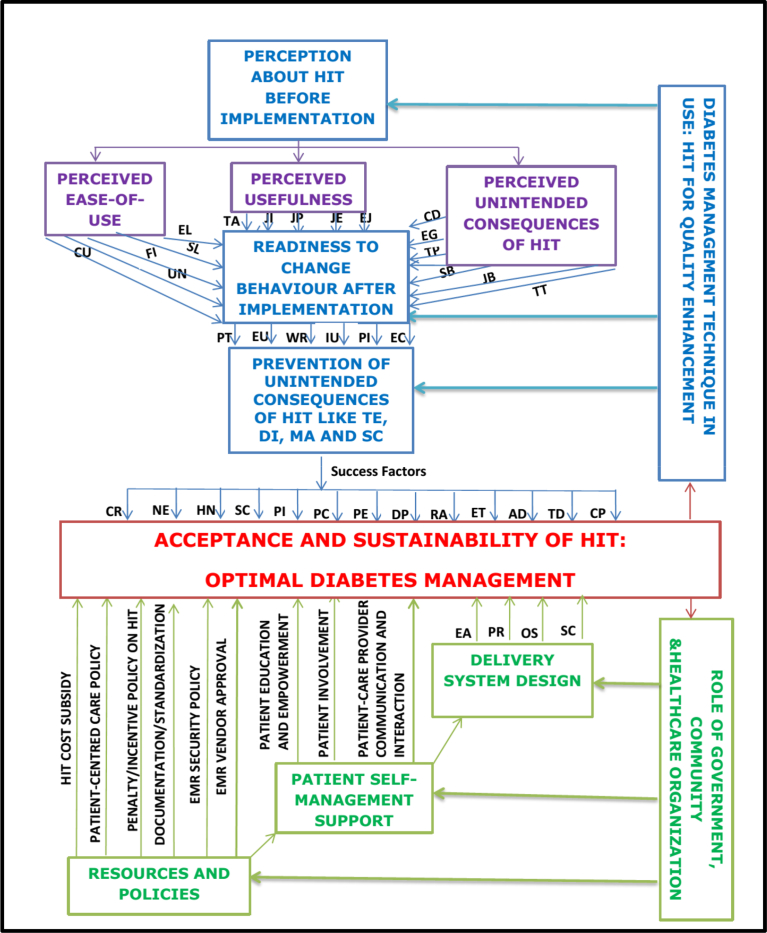
From all the above findings and from the study conceptual frameworks (Technology Acceptance and Chronic Care Models), a Health Information Technology Acceptance Framework for Chronic diseases' management (especially for diabetes) was developed as shown in Fig. 3. As obviously seen in the Figure, the acceptance and sustainability of HIT for optimal management of diabetes mellitus (simply called diabetes) are twofold: The diabetes management technique in use; and the role of government, community and healthcare organizations in delivering optimal health services for diabetes management.
Fig. 3.
Health Information Technology Acceptance Framework for Chronic diseases' management, especially diabetes (Adapted from Davis et al, 1989 and Wagner, 1998). KEY/LEGEND; Perceived Ease-of-Use: CU – Clear Use, UN – Understandable Navigation, FI – Flexible Interaction, SL – Skill Learning, EL – Easy to Learn; Perceived Usefulness: TA – Task Accomplishment, JI – Job Improvement, JP – Job Productivity, JE – Job Effectiveness, EJ – Easiness of Job; Perceived Unintended Consequences of HIT: CD – Communication Disruption, EG – Error Generation, TP – Third Party, TT – Time Taken, SB – Security Breaches, JB – Job Loss; Readiness to Change Behaviour after Implementation: PT – Poor Typing, EU – EMR-features Usage, WR – Workflow Readjustment, IU – Internet Usage, PI – Patient Involvement, EC – Erroneous Copying; Prevention of Unintended Consequences of HIT: TE – Thought Expression, DI – Doctor-patient Interaction, MA – Medical Accuracy, SC – Security and Confidentiality; Success Factors of HIT: CR – Complete Records, NE – Needed Expertise, HN – Hospitals' Network, SC – Security and Confidentiality, PI – Patient Involvement, PC – Patient-Doctor Communication, PE – Patient Education, DP – Delivery Process, RA – Records Accessibility, ET – Effective Treatment, AD – Accurate Decision, TD – True Diagnosis, CP- Clear Prescription; Delivery System Design: EA – Expertise Availability, PR – Staff-Patient Ratio, OS – Organisational Structure, SC – Security Consciousness.
4.2. Health Information Technology Acceptance Framework for Chronic diseases' management
Based on the previous findings, a conceptual framework illustrating health information technology acceptance for chronic diseases like diabetes is shown in Fig. 3 below. Adapting technology acceptance model, apart from perceived ease of use, perceived usefulness and perceived unintended consequences of HIT, the new concept introduced in the framework is ‘Readiness to change behaviour’. This is defined as the willingness of the users of a technology to adjust their actions/behaviours to the technology-promoting ones. Thus, this conceptual framework was based on the postulation that the perception of users before the implementation of HIT (in terms of perceived ease of use, perceived usefulness and perceived unintended consequences of HIT) will determine their readiness to change behaviour to promote the success, acceptance and sustainability of the technology. The changed behavior could be in terms of improving poor typing skills, using all available EMR features, workflow readjustment and so on. The level at which a technology user is ready to change behavior to these technology-promoting ones in turn will determine the rate at which the unintended consequences of technology will be prevented, reduced or avoided. Prevention or reduction of these unintended consequences will form the success factors (such as complete records and needed expertise) of the technology, so as to be accepted by the users and also sustained for optimal chronic disease management like diabetes.
Furthermore, as explained earlier using Chronic Care model, the role of government, community and healthcare organizations in the acceptance of health information technology cannot be over-emphasized. This could be in terms of resources and policies (e.g. HIT cost subsidy etc), patient self-management support (e.g. patient education and empowerment etc.) and delivery system redesign (e.g. expertise availability). The variables for each parameter are illustrated in the figure (Fig. 3).
4.3. Health information technology and diseases' management
What is obvious from this study is that, though there are various diabetes management techniques, out of these techniques, a technique involving the use of HIT (which Wagner, 1998 called Clinical Information System), has been proven by many researchers to be highly effective in attaining optimal diabetes management, and thus enhancing quality of diabetes care and management. Therefore, for HIT to achieve its desired outcomes, the following points are important (modified after the Technology Acceptance Model in Davis et al., 1989). The first point is the perception about HIT before implementation. There is no entirely new system that the users will not have had background knowledge or information about, either from the same/other states or country, even before the technology comes into being. This perception before implementation was broadly grouped into three for this study: Perceived ease-of-use; Perceived usefulness and Perceived unintended consequences of HIT. The variables measured under each parameter have been fully presented in the results section. Above all, these variables determine the acceptance and sustainability of the HIT, which finally brings about the optimal diabetes management.
Likewise as adapted from CCM, the implementation of a good Health Information Technology depends on the roles of the stakeholders in making the technology work and achieve its intended outcomes. For example, the roles of the government, community and the healthcare organizations cannot be overemphasized. Their roles, modified after Wagner's Chronic Care Model (Wagner, 1998), may be grouped into three: Provision of Patient self-management support; adequate policies and resources; and Delivery system redesign. Provision of adequate resources and policies, for example, is in terms of subsidising HIT costs; initiating and implementing patient-centred policy; having incentives for hospitals/staff that promote HIT, and penalties for those ones doing otherwise; implementing documentation/standardization policy nationally and internationally as their jurisdiction is; having data security and confidentiality policies on ground for EMR; and vendor (internal/external to the organization) obtaining government license before commencing on any EMR project to ensure standardization. Patient self-management support involves putting all the aforementioned resources and policies in place, which will lead to patients having self-management support for his illness in terms of patient education and empowerment (through mobile technology and/or internet technology). This is an indication that the patient is being carried along in his disease management (patient involvement) and then enhancing patient-healthcare provider communication and interaction. Furthermore, delivery system redesigns involves providing adequate resources and policies and also patient self-management support thus leading to the delivery system being redesigned in a way that will bring effectiveness, efficiency and cost reduction to diabetes management. This redesign might involve a restructuring of the healthcare organization to enhance the acceptability and sustainability of the new technology. This could be in the forms of making expertise available by constant and continuous training, employing adequate number of staff to increase staff-patient ratio and also being data security conscious because healthcare information is very sensitive, for it contains every detail about the patient care and health (Nilsson et al., 2010; Bexci and Subramani, 2014; Melchiorre et al., 2018).
4.4. Interview results and discussions
The interview method was used to determine the level of acceptance of Health Information Technology (HIT) for the management of diabetes. NVivo software was used to generate the themes/keywords in the two interviews conducted. It was found out from the interviews that the presence and awareness of unintended consequences of HIT was a discouragement for health information technology acceptance. Though, this is due to the low level of awareness of the respondents, that some of these unintended consequences have dos and don'ts that if followed strictly, would eliminate/reduce the negative effects of these unintended consequences. For example in entering patient data details, a dedicated post (a data specialist) could be created, that would be in charge of these entering of data so as to relief the work of the physicians, and to reduce the probability of having erroneous data. However, the interviews findings found out that the Staff are ready to accept the HIT because of their perception that it would be useful to them (based on the good news they have heard about the HIT from other countries that use the technology), which is paramount in the findings of the questionnaire that Staff perceive HIT to be the one that will make their job easy, improve their job performance, make them accomplish their daily task quickly and be useful generally in performing their daily tasks.
5. Conclusion
The study examined the level of Health Information Technology acceptance for the management of chronic diseases, and especially, a model was developed for sustainable management of diabetes mellitus. Adapting Technology Acceptance Model, the level of HIT acceptance by the respondents in the study area was measured in terms of Perceived Ease-of-Use, Perceived Usefulness, and Perceived Unintended Consequences of HIT. The collected data conducted among some healthcare stakeholders (Nurses, Doctors, Laboratory scientists, Pharmacists, ICT unit professionals, Medical Record officers, and Patients), were grouped under Staff and Patients. Using mean ranking and taking all the factor variables together, Staff perceive HIT to be the one that will make their job easy, improve their job performance, make them accomplish their daily task quickly and be useful generally in performing their daily tasks, and all these will determine their acceptability of the technology. Whereas, patients see a technology as being useful when it enhances their disease management plans. Furthermore, Staff perceive HIT to be interactive, flexible and even educative, lack of which might be one of the reasons why all the HIT that were introduced into the health sector since the inception of ICT, were not accepted. These are also confirmed by patients that technology interactivity and flexibility are important criteria for their own HIT acceptance. Data Insecurity and Job loss are the major fear of Staff when HIT is implemented, so also is data security breaches the patients' fear. This is because health data to patients are very crucial, and that they might cause some embarrassment, ruin or damage, for example, to the patient's career, discharge from work etc, if disclosed unlawfully.
Under Chronic care model, the role of government, community and healthcare organizations cannot be overemphasized. Therefore, the government is encouraged to find a way to subsidize the cost of Health Information Technology in tertiary hospitals, so that hospitals will be able to afford it. Thus, adequate budgetary allocation must be provided by the government for the purchase of appropriate HIT hardware and software and other accessories; costs of installation, support and maintenance for better healthcare in the country. Also for acceptability of HIT, hospitals have to embark on ‘continuous’ training for the HIT users, so that users would be able to familiarize themselves with the technology, so as for the HIT to be fully incorporated into their workflow.
Declarations
Author contribution statement
O.S. Ayanlade: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
T.O. Oyebisi: Performed the experiments; Contributed reagents, materials, analysis tools or data; Wrote the paper.
B.A. Kolawole: Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
This research is partly funded by a grant from Obafemi Awolowo University PostGraduate School, Nigeria.
References
- Abelson T.I. The electronic medical record: learning to swim. Clevel. Clin. J. Med. 2010;77:415–419. doi: 10.3949/ccjm.77a.10035. [DOI] [PubMed] [Google Scholar]
- Agbor A.M., Naidoo S. Knowledge and practice of traditional healers in oral health in the Bui Division, Cameroon. J. Ethnobiol. Ethnomed. 2011;7:6. doi: 10.1186/1746-4269-7-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barello S., Graffigna G., Vegni E. Patient engagement as an emerging challenge for healthcare services: mapping the literature. Nurs. Res. Prac. 2012;2012 doi: 10.1155/2012/905934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett A.H., Mithal A., Manassie J., Jones R., Rattunde H., Woerle H.J., Broedl U.C., investigators E-RRt. Efficacy and safety of empagliflozin added to existing antidiabetes treatment in patients with type 2 diabetes and chronic kidney disease: a randomised, double-blind, placebo-controlled trial. Lancet Diab. Endocrinol. 2014;2:369–384. doi: 10.1016/S2213-8587(13)70208-0. [DOI] [PubMed] [Google Scholar]
- Bauer U.E., Briss P.A., Goodman R.A., Bowman B.A. Prevention of chronic disease in the 21st century: elimination of the leading preventable causes of premature death and disability in the USA. Lancet. 2014;384:45–52. doi: 10.1016/S0140-6736(14)60648-6. [DOI] [PubMed] [Google Scholar]
- Beck E.J., Gill W., De Lay P.R. Protecting the confidentiality and security of personal health information in low-and middle-income countries in the era of SDGs and Big Data. Glob. Health Action. 2016;9:32089. doi: 10.3402/gha.v9.32089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benson J., Sediqzad A., Wheeler J. 2018. The Impact of Technology. Leading and Managing in Nursing-E-Book; p. 274. [Google Scholar]
- Bexci M., Subramani R. Health communicationin Non-fatal illness care using ICT: a five-layer model. Indian J. Med. Healthc. 2014;3:350–356. [Google Scholar]
- Braunstein M.L. Health Informatics on FHIR: How HL7's New API is Transforming Healthcare. Springer; 2018. Health informatics in the real world. [Google Scholar]
- Brereton M.F., Iberl M., Shimomura K., Zhang Q., Adriaenssens A.E., Proks P., Spiliotis, Dace W., Mattis K.K., Ramracheya R. Reversible changes in pancreatic islet structure and function produced by elevated blood glucose. Nat. Commun. 2014;5:4639. doi: 10.1038/ncomms5639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiarello-Ebner K. Target: blood Sugar Health Natural support for healthy blood sugar levels. Blood. 2016:1874. [Google Scholar]
- Davis F.D. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. 1989:319–340. [Google Scholar]
- Davis F.D. User acceptance of information technology: system characteristics, user perceptions and behavioral impacts. Int. J. Man Mach. Stud. 1993;38:475–487. [Google Scholar]
- Davis F.D., Bagozzi R.P., Warshaw P.R. User acceptance of computer technology: a comparison of two theoretical models. Manag. Sci. 1989;35:982–1003. [Google Scholar]
- Davoody N., Koch S., Krakau I., Hägglund M. Post-discharge stroke patients’ information needs as input to proposing patient-centred eHealth services. BMC Med. Inf. Decis. Mak. 2016;16:66. doi: 10.1186/s12911-016-0307-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dent M., Pahor M. Patient involvement in Europe–a comparative framework. J. Health Organ. Manag. 2015;29:546–555. doi: 10.1108/JHOM-05-2015-0078. [DOI] [PubMed] [Google Scholar]
- Desmedt M., Pless S., Dessers E., Vandijck D. Integrating and safeguarding care: the potential role of health information technologies. Int. J. Care Coord. 2017;20:112–118. [Google Scholar]
- Dinev T., Albano V., Xu H., D’Atri A., Hart P. Advances in Healthcare informatics and Analytics. Springer; 2016. Individuals’ attitudes towards electronic health records: a privacy calculus perspective. [Google Scholar]
- Drapcho C. 2016. The Effects of Electronic Medical Records on Patient-Physician Relationships and Interactions. [Google Scholar]
- Ezuruike U.F., Prieto J.M. The use of plants in the traditional management of diabetes in Nigeria: pharmacological and toxicological considerations. J. Ethnopharmacol. 2014;155:857–924. doi: 10.1016/j.jep.2014.05.055. [DOI] [PubMed] [Google Scholar]
- Fokunang C., Ndikum V., Tabi O., Jiofack R., Ngameni B., Guedje N., Tembe-Fokunang E., Tomkins P., Barkwan S., Kechia F. Traditional medicine: past, present and future research and development prospects and integration in the National Health System of Cameroon. Afr. J. Tradit. Complement. Altern. Med. 2011;8 doi: 10.4314/ajtcam.v8i3.65276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Free C., Phillips G., Galli L., Watson L., Felix L., Edwards P., Patel V., Haines A. The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: a systematic review. PLoS Med. 2013;10 doi: 10.1371/journal.pmed.1001362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GHRI . 2015. The Chronic Care Model. [Google Scholar]
- Gray K., Gilbert C. Advances in Biomedical Informatics. Springer; 2018. Digital health research methods and tools: suggestions and selected resources for researchers. [Google Scholar]
- Greiver M., Barnsley J., Glazier R.H., Moineddin R., Harvey B.J. Implementation of electronic medical records: effect on the provision of preventive services in a pay-for-performance environment. Can. Fam. Phys. 2011;57:e381–e389. [PMC free article] [PubMed] [Google Scholar]
- Hoffman T.K. Arizona State University; 2015. Exploring Communal Coping: Witnessing the Process of Empowerment Unfold during Shared Medical Appointments. [Google Scholar]
- Idowu P., Cornford D., Bastin L. Health informatics deployment in Nigeria. J. Health Inf. Dev. Ctries. 2008;2 [Google Scholar]
- James B.O., Morakinyo O., Eze G.O., Lawani A.O., Omoaregba J.O. Depression and subjective quality of life among outpatients with diabetes mellitus at a teaching hospital in Nigeria. Ment. Health Fam. Med. 2010;7:179. [PMC free article] [PubMed] [Google Scholar]
- Koppel R., Chen Y. Unintended consequences: new problems, new solutions. Yearb. Med. Inf. 2016;25:87–92. doi: 10.15265/IY-2016-048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krist A.H., Nease D.E., Kreps G.L., Overholser L., McKenzie M. Oncology informatics. Elsevier; 2016. Engaging patients in primary and specialty care. [Google Scholar]
- Lazo M., Nwankwo C., Daya N.R., Thomas D.L., Mehta S.H., Juraschek S., Willis K., Selvin E. Confluence of epidemics of hepatitis C, diabetes, obesity, and chronic kidney disease in the United States population. Clin. Gastroenterol. Hepatol. 2017 doi: 10.1016/j.cgh.2017.04.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C.-F., Cheng T.-J. Exploring critical factors influencing physicians’ acceptance of mobile electronic medical records based on the dual-factor model: a validation in Taiwan. BMC Med. Inf. Decis. Mak. 2015;15:4. doi: 10.1186/s12911-014-0125-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowry S.Z., Ramaiah M., Prettyman S.S., Simmons D., Brick D., Deutsch E., Possanza L., Gray O.B., Levine B.A. US Department of Commerce, National Institute of Standards and Technology; 2017. Examining the Copy and Paste Function in the Use of Electronic Health Records. [Google Scholar]
- Meeks D.W., Smith M.W., Taylor L., Sittig D.F., Scott J.M., Singh H. An analysis of electronic health record-related patient safety concerns. J. Am. Med. Inform. Assoc. 2014;21:1053–1059. doi: 10.1136/amiajnl-2013-002578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melchiorre M.G., Papa R., Rijken M., van Ginneken E., Hujala A., Barbabella F. eHealth in integrated care programs for people with multimorbidity in Europe: insights from the ICARE4EU project. Health Policy. 2018;122:53–63. doi: 10.1016/j.healthpol.2017.08.006. [DOI] [PubMed] [Google Scholar]
- Menachemi N., Rahurkar S., Tarver W.L. 15. HIT to enhance patient care and organizational performance. Handb. Healthc. Manag. 2015:351. [Google Scholar]
- Miller B. Oak Publication Sdn Bhd; 2016. Diabesity: the Twin Threats of Diabetes & Obesity that Is Making You Fat & Sick. [Google Scholar]
- Nilsson C., Skär L., Söderberg S. Swedish District Nurses’ experiences on the use of information and communication technology for supporting people with serious chronic illness living at home–a case study. Scand. J. Caring Sci. 2010;24:259–265. doi: 10.1111/j.1471-6712.2009.00715.x. [DOI] [PubMed] [Google Scholar]
- Nutting P.A., Crabtree B.F., Miller W.L., Stange K.C., Stewart E., Jaén C. Transforming physician practices to patient-centered medical homes: lessons from the national demonstration project. Health Aff. 2011;30:439–445. doi: 10.1377/hlthaff.2010.0159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogbera A.O., Ekpebegh C. Diabetes mellitus in Nigeria: the past, present and future. World J. Diabetes. 2014;5:905. doi: 10.4239/wjd.v5.i6.905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pallant J. McGraw-Hill Education; (UK): 2013. SPSS Survival Manual. [Google Scholar]
- Palojoki S., Mäkelä M., Lehtonen L., Saranto K. An analysis of electronic health record–related patient safety incidents. Health Inf. J. 2017;23:134–145. doi: 10.1177/1460458216631072. [DOI] [PubMed] [Google Scholar]
- Pradeepa R., Prabu A.V., Jebarani S., Subhashini S., Mohan V. SAGE Publications; 2011. Use of a Large Diabetes Electronic Medical Record System in India: Clinical and Research Applications. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Punthakee Z., Goldenberg R., Katz P., Committee DCCPGE Definition, classification and diagnosis of diabetes, prediabetes and metabolic syndrome. Can. J. Diabetes. 2018;42:S10–S15. doi: 10.1016/j.jcjd.2017.10.003. [DOI] [PubMed] [Google Scholar]
- Renedo A., Marston C.A., Spyridonidis D., Barlow J. Patient and public involvement in healthcare quality improvement: how organizations can help patients and professionals to collaborate. Publ. Manag. Rev. 2015;17:17–34. [Google Scholar]
- Sekaran U., Bougie R. John Wiley & Sons; 2016. Research Methods for Business: A Skill Building Approach. [Google Scholar]
- Tabrizi J.S., Wilson A.J., O’Rourke P.K. Customer quality and type 2 diabetes from the patients’ perspective: a cross-sectional study. J. Res. Health Sci. 2011;10:69–76. [PubMed] [Google Scholar]
- Taneja V.C. The George Washington University; 2018. The Unintended Negative Consequences of Electronic Health Records (EHR) in the Healthcare Enterprise. [Google Scholar]
- Terry A.L., Brown J.B., Denomme L.B., Thind A., Stewart M. Perspectives on electronic medical record implementation after two years of use in primary health care practice. J. Am. Board Fam. Med. 2012;25:522–527. doi: 10.3122/jabfm.2012.04.110089. [DOI] [PubMed] [Google Scholar]
- Thoolen B.J., Ridder Dd, Bensing J., Gorter K., Rutten G. Beyond good intentions: the role of proactive coping in achieving sustained behavioural change in the context of diabetes management. Psychol. Health. 2009;24:237–254. doi: 10.1080/08870440701864504. [DOI] [PubMed] [Google Scholar]
- Tommasetti A., Singer P., Troisi O., Maione G. Extended theory of planned behavior (ETPB): investigating customers’ perception of restaurants’ sustainability by testing a structural equation model. Sustainability. 2018;10:2580. [Google Scholar]
- Tubaishat A. The effect of electronic health records on patient safety: a qualitative exploratory study. Inf. Health Soc. Care. 2019;44:79–91. doi: 10.1080/17538157.2017.1398753. [DOI] [PubMed] [Google Scholar]
- Unger J. Lippincott Williams & Wilkins; 2013. Diabetes Management in Primary Care. [Google Scholar]
- Virginio L.A., Jr., Ricarte I.L.M. Proc MedInfo. 2015. Identification of patient safety risks associated with electronic health records: a software quality perspective. [PubMed] [Google Scholar]
- Wagner E.H. Chronic disease management: what will it take to improve care for chronic illness? Effect Clin. Pract. ECP. 1998;1:2–4. [PubMed] [Google Scholar]
- WHO . 2008. SERVICE DELIVERY: Toolkit on Monitoring Health Systems Strengthening. [Google Scholar]
- Zgibor J.C., Solano F.X., Siminerio L. Integrated Diabetes Care. Springer; 2017. A primary health-care system Approach to improving quality of care and outcomes in people with diabetes: the University of Pittsburgh medical center experience. [Google Scholar]
- Zwar N., Harris M., Griffiths R., Roland M., Dennis S., Powell Davies G., Hasan I. 2017. A Systematic Review of Chronic Disease Management. [Google Scholar]