Abstract
Background:
Patient-reported outcome measures are commonly used to measure knee pain and functional impairment. When structural abnormality is identified on examination and imaging, arthroscopic partial meniscectomy and chondroplasty are commonly indicated for treatment in the setting of pain and decreased function.
Purpose:
To evaluate the relationship between patient characteristics, mental health, intraoperative findings, and patient-reported outcome measures at the time of knee arthroscopy.
Study Design:
Cross-sectional study; Level of evidence, 3.
Methods:
Between February 2015 and October 2016, patients aged 40 years and older who were undergoing routine knee arthroscopy for meniscal and cartilage abnormality, without reconstructive or restorative procedures, were prospectively enrolled in this study. Routine demographic information was collected, and the Knee injury and Osteoarthritis Outcome Score (KOOS) Pain, Quality of Life (QoL), and Physical Function Short Form (PS) subscales and the mental and physical component subscales of the Veterans RAND 12-Item Health Survey (VR-12 MCS and VR-12 PCS) were administered preoperatively on the day of surgery. Intraoperative findings were collected in a standardized format. Patient demographics, intraoperative findings, and the VR-12 MCS were used as predictor values, and a multivariate analysis was conducted to assess for relationships with the KOOS and VR-12 as dependent variables.
Results:
Of 661 eligible patients, baseline patient-reported outcomes and surgical data were used for 638 patients (97%). Lower scores on both subscales of the VR-12 were predicted by female sex, positive smoking history, fewer years of education, and higher body mass index (BMI). All KOOS subscales were negatively affected by lower VR-12 MCS scores, female sex, lower education level, and higher BMI in a statistically meaningful way. Positive smoking history was associated with worse scores on the KOOS-PS. Abnormal synovial status was associated with worse KOOS-Pain.
Conclusion:
The demographic factors of sex, smoking status, BMI, and education level had an overwhelming impact on preoperative KOOS and VR-12 scores. Of interest, mental health as assessed by the VR-12 MCS was also a consistent predictor of KOOS scores. The only intraoperative finding with a significant association was abnormal synovial status and its effect on KOOS-Pain scores.
Keywords: knee pain, knee function, patient-reported outcome measures, knee arthroscopy
Outpatient knee arthroscopy is one of the most commonly performed orthopaedic procedures in the United States. Its incidence has increased at rates surpassing the corresponding population growth, with nearly 1 million procedures reported in 2006.18 Preoperative patient-reported outcome measures can influence postoperative outcomes after knee reconstruction and arthroplasty.4,21,29 To study patient outcomes, a comprehensive understanding of factors that influence common patient-reported outcome measures is warranted. Given the aggregate cost associated with knee arthroscopy nationwide, it is important to identify factors that influence preoperative measures to better understand postoperative outcomes.
Because of the widespread application of knee arthroscopy for the treatment of meniscal tears and chondral injuries in the middle-aged population, its use has come under scrutiny, with some studies casting doubt over the efficacy of arthroscopy compared with nonsurgical treatment modalities.14,17,27 Multiple studies have also brought into question the cause of perceived knee symptoms for patients whose pain and level of function are commonly attributed to structural abnormality found on imaging or at the time of surgery. Although some authors have demonstrated that knee abnormality or synovial biomarkers24 can be associated with patients’ pain and function, other authors have found demographic factors to be more predictive.3,5,6,10,12,20,26,30,31 Aside from physical attributes and abnormalities, the mental health of patients with common musculoskeletal conditions can be an important predictor of pain and functional outcomes.1,7,13,34
A recent study by Tornbjerg et al30 in a European population examined the relationship between intraoperative findings at the time of knee arthroscopy and preoperative scores on 3 subscales of the Knee injury and Osteoarthritis Outcome Score (KOOS): Pain (KOOS-Pain), Function in Sport and Recreation (KOOS-Sport/Rec), and Function in Activities of Daily Living (KOOS-ADL). No strong associations between structural abnormality and outcomes were identified. The current cross-sectional study encompasses a larger American cohort and additionally examines the effect of preoperative mental health on overall pain and function. Our hypothesis was that although structural abnormality might not relate to patient-reported outcome measures, patient demographics as well as mental health would have a significant impact on baseline knee pain and function.
Methods
This study was approved by a local institutional review board. Patients age 40 years and older undergoing unilateral knee arthroscopy for partial meniscectomy and/or chondroplasty at our institution were prospectively enrolled between February 2015 and October 2016. Patients were excluded if they had a prior surgery on the ipsilateral or contralateral knee other than a knee arthroscopy for partial meniscectomy and/or chondroplasty, if they had an intraoperative diagnosis of an anterior cruciate ligament injury, or if they were undergoing concomitant procedures including ligamentous repair or reconstruction, osteotomy, removal of hardware, irrigation and debridement, microfracture, autologous chondrocyte implantation, or osteochondral autograft or allograft transfer.
On the day of surgery, patients were asked preoperatively to complete a Veterans RAND 12-Item Health Survey (VR-12), which assesses general health and has both a Physical Component Score (VR-12 PCS) and a Mental Component Score (VR-12 MCS). Patients were also asked to complete several portions of the KOOS, including the KOOS-Pain, Physical Function Short Form (KOOS-PS), and Quality of Life (KOOS-QoL) subscales to assess knee health.11,33 Demographic information, including sex, age, body mass index (BMI), education, and smoking status, was also collected. Data were entered by the patient on an electronic tablet. All information was collected and managed on a secure online Research Electronic Data Capture (REDCap) database managed by our institution.16
At the conclusion of each surgery, a secure email was sent to the primary surgeon with an electronic link to a data entry system. This system, using branching logic, efficiently collects detailed intraoperative findings; it is designed to be completed promptly after surgery on a smartphone or similar device and stores that information in a secure REDCap database.
Groupings were made of similar intraoperative predictor values to decrease the number of independent variables and decrease the chance that meaningful associations would be subject to type II error. Cartilage and meniscal lesions were grouped into distinct categories based on the similarity of the lesions. Cartilage groupings included grade 0 or 1 lesions, grade 2 focal lesions, grade 2 diffuse lesions, grade 3 or 4 focal lesions, and grade 3 or 4 diffuse lesions. Meniscal lesions were categorized as normal, oblique or flap tears, longitudinal or bucket-handle tears, radial tears, root tears, or horizontal or complex tears. Ipsilateral and contralateral knee range of motion in 5° increments and the presence of a flexion contracture were also noted but were not used in the statistical analysis, as most participating surgeons did not measure these parameters with a goniometer and it was believed that the data might not be consistently accurate.
With the KOOS and VR-12 scores used as outcome variables, univariate and multivariate analyses were conducted with patient demographic data and intraoperative findings as predictor variables. The VR-12 MCS doubled as a predictor variable in analysis of the remaining outcome scores to determine the effect of a patient’s mental health on his or her perceived overall and knee-specific function, pain, and quality of life. For the univariate analysis, the categorical predictors and outcome variables were compared by use of the Welch 2-sample t test or 1-way analysis of variance, whereas Pearson correlations were used to measure and test associations between numerical predictors and the outcome variables.
To control for confounders, multivariate analysis was conducted. Outcome variables were modeled by ordinary least squares regression. Predictor variables were selected in a backward-stepwise manner according to P values with a retention threshold of .05. Remaining predictors were added and removed from each model individually to ensure that no important variables were omitted. All analyses were performed with R software (R version 3.3.2), and all testing was 2-sided and considered significant at the 5% level.
Results
A total of 661 patients were identified at our institution according to the inclusion and exclusion criteria. No data for the KOOS and VR-12 scores were available for 13 patients. Ultimately, 648 patients were available for investigation, more than 98% of the initial eligible cohort. In 10 of these patients, the surgeon noted a prior partial excision of the medial or lateral meniscus when describing the meniscal status. These groups were deemed too small to independently analyze by meniscal tear status and type, and from the surgeon-collected data available it was unclear which of the remaining meniscal groups these patients should be categorized under. A decision was made to exclude these patients from analysis, leaving almost 97% (n = 638) of the initially eligible cohort.
The patient data used in the final analysis were contributed by 18 surgeons. Only 4 data points were missing in the entirety of the remaining data: 3 KOOS subscale scores and 1 medial meniscal tear type. Data from these patients were used except for observations directly related to the missing values. Numerical predictors are summarized in Table 1, and categorical predictors are summarized in Table 2. Univariate and multivariate analyses were completed for all outcome variables, and the results are summarized in Table 3.
TABLE 1.
Numerical Variables at Time of Surgerya
| Numerical Variable | Mean ± SD | Q1 | Median | Q3 |
|---|---|---|---|---|
| Age, y | 55.1 ± 8.6 | 48.6 | 54.6 | 60.8 |
| Educationb | 14.7 ± 2.7 | 12 | 14.5 | 16 |
| Body mass index, kg/m2 | 31.3 ± 7.2 | 26 | 30.2 | 34.8 |
| Compartments with diffuse cartilage injury, 0-3 | 0.87 ± 0.89 | 0.0 | 1.0 | 2.0 |
| VR-12 MCS | 55.4 ± 11.5 | 45.8 | 55.8 | 62.3 |
| VR-12 PCS | 32.2 ± 10.2 | 24.8 | 31.1 | 39.2 |
| KOOS-Pain | 47.4 ± 18.5 | 36.1 | 47.2 | 61.1 |
| KOOS-QoL | 29.6 ± 18.1 | 18.8 | 31.2 | 43.8 |
| KOOS-PS | 46 ± 16.8 | 45.6 | 56 | 64.7 |
aN = 638 patients. Q1 and Q3 reflect the first (25%) and third (75%) quartiles, respectively. KOOS, Knee injury and Osteoarthritis Outcome Score; MCS, Mental Component Score; PCS, Physical Component Score; PS, Physical Function Short Form; QoL, Quality of Life; VR-12, Veterans RAND 12-Item Health Survey.
bYears completed starting at first grade.
TABLE 2.
Categorical Variables at Time of Surgerya
| Categorical Variable and Groupings | Result |
|---|---|
| Sex | |
| Male | 52% |
| Female | 47% |
| Smoking | |
| Yes (current and former) | 58% |
| No | 42% |
| Prior arthroscopy | |
| None | 87% |
| Ipsilateral | 4% |
| Contralateral | 8% |
| Bilateral | 1% |
| Ipsilateral effusion | |
| Yes (any) | 18% |
| No | 82% |
| Meniscal status | |
| Normal | 18% M, 71% L |
| Partial tear | 26% M, 11% L |
| Complete tear | 55% M, 19% L |
| Main meniscal tear type | |
| None | 18% M, 71% L |
| Oblique or flap | 8% M, 3% L |
| Longitudinal or bucket handle | 5% M, 3% L |
| Radial | 9% M, 3% L |
| Root | 5% M, 1% L |
| Horizontal or complex | 55% M, 19% L |
| Cartilage injury | |
| Grade 0 or 1 | 35% PF, 33% M, 72% L |
| Grade 2 focal | 11% PF, 7% M, 5% L |
| Grade 2 diffuse | 10% PF, 10% M, 6% L |
| Grade 3 or 4 focal | 21% PF, 20% M, 10% L |
| Grade 3 or 4 diffuse | 24% PF, 31% M, 7% L |
| Synovium | |
| Normal | 91% |
| Abnormal | 9% |
aL, lateral compartment; M, medial compartment; PF, patellofemoral compartment.
TABLE 3.
Results of Univariate and Multivariate Analysesa
| Significant Predictors After Univariate Analysis | Significant Predictors After Multivariate Analysis | ||||
|---|---|---|---|---|---|
| Outcome Variable | Predictor | P | Predictor | P | R 2 |
| VR-12 MCS | Female sex | .019 | Female sex | .049 | 0.0647 |
| Positive smoking history | <.001 | Positive smoking history | <.001 | ||
| Fewer years of education | <.001 | Fewer years of education | .02 | ||
| Higher BMI | <.001 | Higher BMI | <.001 | ||
| VR-12 PCS | Female sex | <.001 | Female sex | <.001 | 0.178 |
| Positive smoking history | <.001 | Positive smoking history | .002 | ||
| Lower VR-12 MCS | .002 | Fewer years of education | <.001 | ||
| Fewer years of education | <.001 | Higher BMI | <.001 | ||
| Higher BMI | <.001 | ||||
| Patellofemoral cartilage lesion type | .031 | ||||
| Lateral compartment cartilage lesion type | .029 | ||||
| Number of diffuse cartilage grades | .024 | ||||
| KOOS-Pain | Female sex | <.001 | Female sex | .003 | 0.224 |
| Positive smoking history | <.001 | Lower VR-12 MCS | <.001 | ||
| Lower VR-12 MCS | <.001 | Fewer years of education | <.001 | ||
| Fewer years of education | <.001 | Higher BMI | <.001 | ||
| Higher BMI | <.001 | Abnormal synovium | .032 | ||
| Patellofemoral cartilage lesion type | .015 | ||||
| Medial compartment cartilage lesion type | .029 | ||||
| Abnormal synovium | .039 | ||||
| Number of diffuse cartilage grades | .001 | ||||
| KOOS-PS | Female sex | .001 | Female sex | .034 | 0.237 |
| Positive smoking history | <.001 | Positive smoking history | .003 | ||
| Lower VR-12 MCS | <.001 | Lower VR-12 MCS | <.001 | ||
| Fewer years of education | <.001 | Fewer years of education | <.001 | ||
| Higher BMI | <.001 | Higher BMI | <.001 | ||
| Number of diffuse cartilage grades | .03 | ||||
| KOOS-QoL | Female sex | <.001 | Female sex | .008 | 0.175 |
| Positive smoking history | .001 | Lower VR-12 MCS | <.001 | ||
| Lower VR-12 MCS | <.001 | Fewer years of education | .001 | ||
| Fewer years of education | <.001 | Higher BMI | <.001 | ||
| Higher BMI | <.001 | ||||
aBMI, body mass index; KOOS, Knee injury and Osteoarthritis Outcome Score; MCS, Mental Component Score; PCS, Physical Component Score; PS, Physical Function Short Form; QoL, Quality of Life; VR-12, Veterans RAND 12-Item Health Survey.
Either a flexion contracture or a difference in knee extension of 5° or more with normal flexion (equal to the nonoperative knee and ≥120°) was noted in 28 patients. Knee flexion less than 120° or any difference in knee flexion of 5° or more with normal extension (no flexion contracture and equal to the nonoperative knee) was noted in 74 patients. Abnormalities in both flexion and extension were noted in 10 patients.
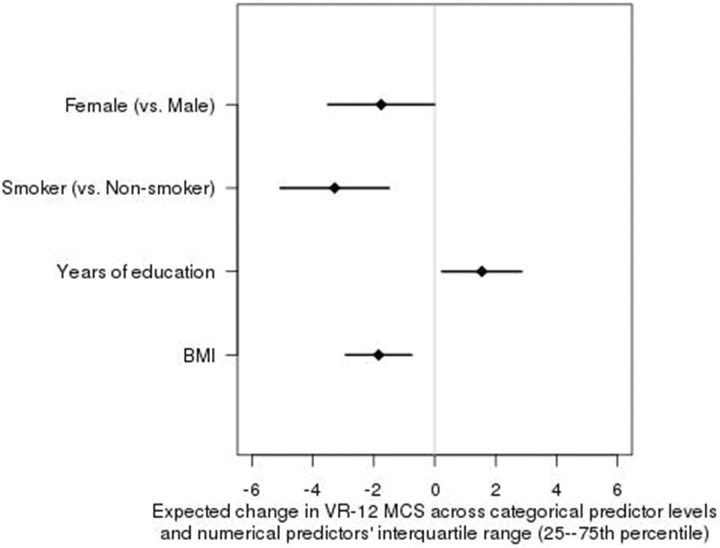
Considering VR-12 MCS as an outcome variable, the multivariate model displayed a low R 2 of 0.0647, meaning that only 6.5% of the variance in VR-12 MCS was explained by the model. The same variables that were associated on the univariate model were all significant on the multivariate model (female sex, P = .049; positive smoking status, P < .001; fewer years of education, P = .02; and higher BMI, P < .001), whereas no new variables emerged. Figure 1 demonstrates the independent effect of each predictor on the VR-12 MCS outcome.
Figure 1.
Effect of each predictor on Veterans RAND 12-Item Health Survey Mental Component Score (VR-12 MCS), with the other predictors held constant. BMI, body mass index.
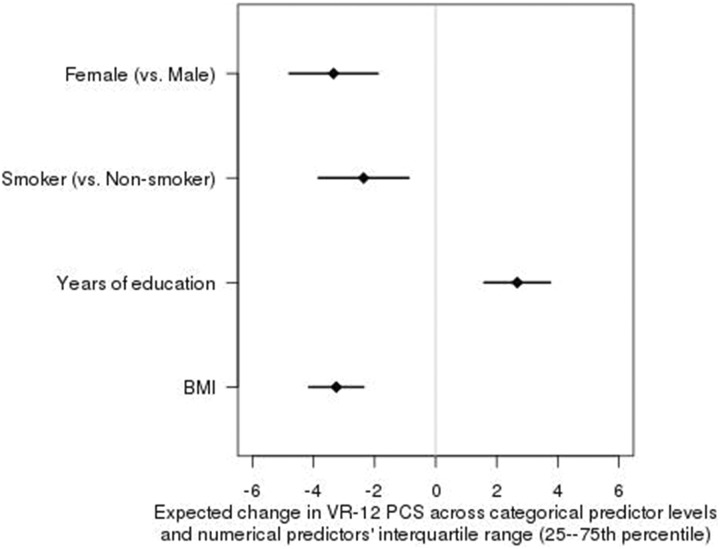
When the VR-12 PCS was analyzed as an outcome variable on multivariate analysis, the R 2 was 0.178. Female sex (P < .001), positive smoking status (P = .002), fewer years of education (P < 001), and higher BMI (P < .001) demonstrated statistically significant relationships with the outcome variable. Although significant on the univariate analysis, patellofemoral and lateral cartilage characteristics as well as the VR-12 MCS and number of diffuse cartilage grades no longer demonstrated an association. Figure 2 demonstrates the independent effect of each predictor on VR-12 PCS.
Figure 2.
Effect of each predictor on Veterans RAND 12-Item Health Survey Physical Component Score (VR-12 PCS), with the other predictors held constant. BMI, body mass index.
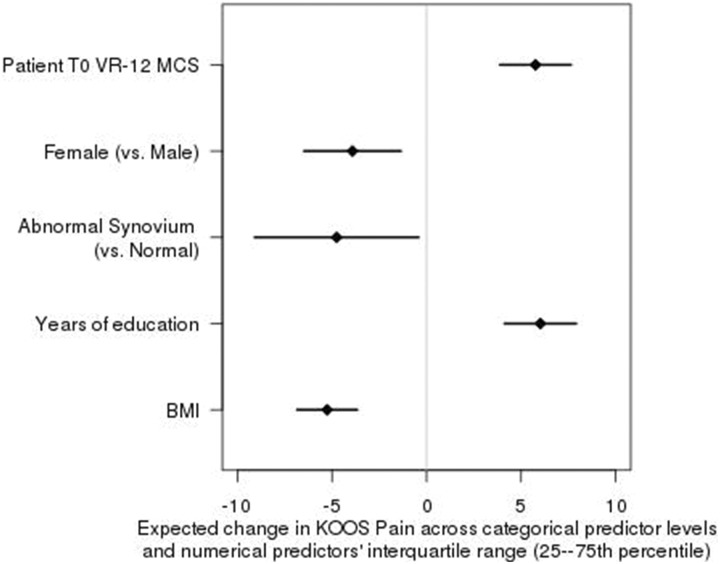
Multivariate analysis of the KOOS-Pain subscale demonstrated an R 2 value of 0.224. VR-12 MCS (P < .001), female sex (P = .003), lower education level (P < .001), higher BMI (P < .001), and abnormal synovial status (P = .032) maintained a significant relationship with the KOOS-Pain outcome variable when controlling for other variables, whereas the remainder of the associations found on the univariate analysis were lost. Figure 3 demonstrates the independent effect of each predictor on KOOS-Pain.
Figure 3.
Effect of each predictor on Knee injury and Osteoarthritis Outcome Score (KOOS) Pain, with the other predictors held constant. BMI, body mass index; VR-12 MCS, Veterans RAND 12-Item Health Survey Mental Component Score.
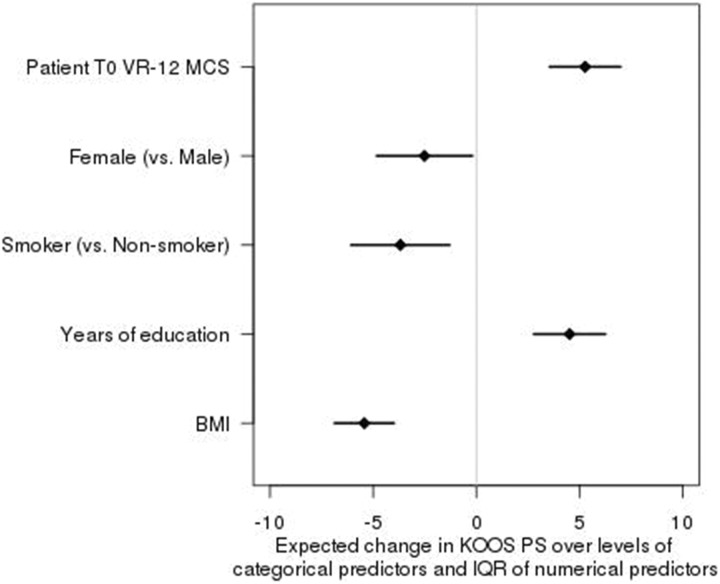
Multivariate analysis of the KOOS-PS subscale demonstrated an R 2 value of 0.237. Significant relationships between KOOS-PS and VR-12 MCS (P < .001), female sex (P = .034), positive smoking status (P = .003), lower education level (P < .001), and higher BMI (P < .001) were confirmed. Figure 4 demonstrates the independent effect of each predictor on KOOS-PS.
Figure 4.
Effect of each predictor on Knee injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), with the other predictors held constant. BMI, body mass index; IQR, interquartile range; VR-12 MCS, Veterans RAND 12-Item Health Survey Mental Component Score.
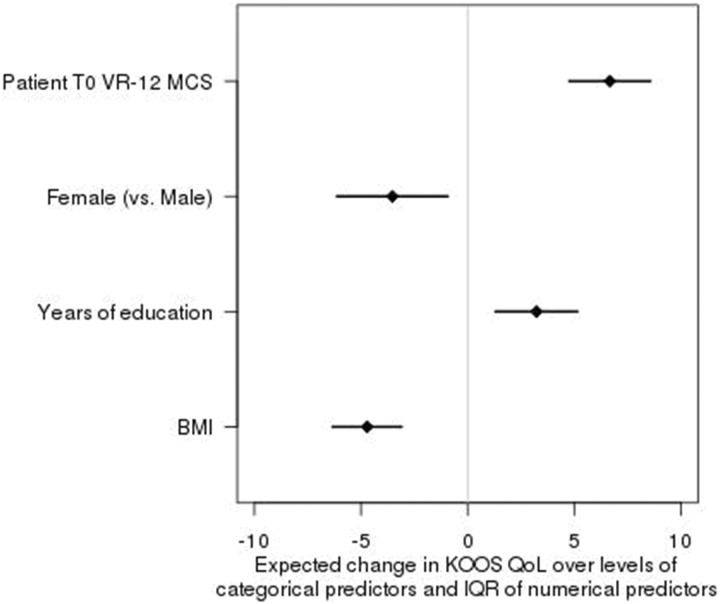
Relationships between the KOOS-QoL and independent predictors on multivariate analysis revealed a significant relationship between lower scores and VR-12 MCS (P < .001), female sex (P = .008), years of education (P = .001), and BMI (P < .001), with an R 2 of 0.175. Figure 5 demonstrates the independent effect of each predictor on KOOS-QoL.
Figure 5.
Effect of each predictor on Knee injury and Osteoarthritis Outcome Score Quality of Life (KOOS-QoL), with the other predictors held constant. BMI, body mass index; IQR, interquartile range; VR-12 MCS, Veterans RAND 12-Item Health Survey Mental Component Score.
Discussion
For all patient-reported outcome measures assessed, there was an overwhelming association with patient factors not related to abnormality in the operative knee, including sex, education level, BMI, and smoking status. When the VR-12 MCS was used as a predictor variable, a statistically significant association was uncovered with all KOOS subscales. Although it was not found to influence the VR-12 PCS, this result would be expected given the orthogonal nature of the 2 distinct subsections of the VR-12. The only intraoperative finding that predicted preoperative pain or function was the influence of an abnormal synovial status (anything other than “normal” noted by the surgeon) on the KOOS-Pain score.
In the multivariate models, all outcomes except VR-12 MCS had R 2 values in the 0.18 to 0.24 range, meaning that about 20% of the variance in each model can be explained by the predictor variables. The VR-12 MCS model explains only 6.5% of the variance, indicating that much of the variance is explained by variables not captured in our data set.
In 2017, Tornbjerg et al30 examined a cohort of 443 Danish patients who were 18 years or older with meniscal abnormality and compared intraoperative findings with KOOS-Pain, KOOS-Sport/Rec, and KOOS-ADL scores just prior to surgery. Age, sex, and body mass were the most consistent predictors of outcomes in their model, although their associations were weak, with R 2 values between 0.10 and 0.12. The only structural abnormality with any association was the presence of synovitis and its effect on the KOOS-Sports/Rec subscale, although the R 2 was only 0.03. Our study showed similar findings regarding the effects of abnormal synovium on patient-reported outcome measures.
Our findings differ from the Tornbjerg et al30 study in that age was not a significant predictor in our cohort. Our minimum age for inclusion was 40 years, which might explain the difference in findings, although overall average ages were similar between the 2 cohorts (49.7 ± 12.8 vs 55.1 ± 8.6 years for the current study). Our study addressed smoking status, which was found to be a significant predictor in 3 of the 5 measured outcome variables. When mental health was assessed with the VR-12 MCS, this was also found to have a significant association with all KOOS subscales.
Other studies have examined the effects of demographics and abnormality on pain and function. Sex-based differences in preoperative pain and function have been identified in patients undergoing total knee arthroplasty. Although this likely includes a more advanced disease process of the cartilage in comparison with our cohort of arthroscopy patients, our results confirm these findings.25 In a 2017 study by Baldwin et al,2 an analysis of KOOS scores in healthy individuals revealed that women and participants with higher BMIs tended to have lower KOOS scores. In another cohort study of patients with Kellgren-Lawrence grade 2 or higher knee osteoarthritis, having fewer than 12 years of education was found to predict lower Western Ontario and McMaster Universities Index of Osteoarthritis (WOMAC) scores.8 Lower education levels predicted lower KOOS scores in our study. Finally, in a cohort of Finnish forestry workers,23 a higher BMI and current or former smoking status were associated with reports of knee pain at the onset of the study. The demographic predictors of pain and poor function identified in our cohort confirm these past findings.
Scanzello et al26 compared preoperative 12-Item Short Form Health Survey, Lysholm, and visual analog scale (VAS) pain scores with intraoperative diagnoses of synovitis in 28 patients undergoing knee arthroscopy. Inflammatory findings were confirmed by pathological analysis and were found, in addition to BMI, to be associated with worse Lysholm scores. Our study, which involved a much larger cohort but no histological analysis, confirms the conclusion that symptoms and synovitis are associated, although different predictive and outcome measures were used. Unlike the findings of Boks et al,6 the presence of knee effusion within our cohort was not found to be associated with more severe symptoms.
A patient’s mental health has been shown to be an important predictor of symptoms and outcomes of musculoskeletal disease.13,15 In their observations in an outpatient spine surgery clinic, Abtahi et al1 found that psychological distress, as measured by the Distress and Risk Assessment Method (DRAM) questionnaire, was significantly associated with the results of a patient satisfaction survey. Wylie et al34 examined a cohort of 169 patients with full-thickness rotator cuff tears. The strongest predictor of VAS pain, VAS function, Simple Shoulder Test (SST), and American Shoulder and Elbow Surgeons (ASES) scores was the 36-Item Short Form Health Survey Mental Component Summary (SF-36 MCS), a validated measure of mental health. Our study found a similar association in a population of patients undergoing knee arthroscopy for nonreconstructive indications.
Whereas our study examined only preoperative patient-reported outcomes, Liebensteiner et al19 searched for factors related to improvement in SF-36 scores after arthroscopic knee surgery. Those investigators found that the degree of cartilage degeneration was significantly associated with the degree of improvement after surgery (patients with milder arthritic changes tended to improve more than patients with severe changes). These findings suggest that although preoperative factors may not be associated with intra-articular abnormality, changes in postoperative outcome measures could be more closely correlated with structural findings and subsequent treatment.
The current study has several limitations. Our study cohort did not represent the general population, as it was a self-selected group of patients presenting with knee pain who consented to undergo arthroscopic surgery. No asymptomatic control group was included, and the results should not be interpreted as indicating that meniscal tears or cartilage abnormality does not cause pain or limit function. Although our predictor variables may be important in predicting pain and function before surgery in this group, similar findings have been identified in populations not seeking treatment for knee pain.2 Our study involved the collection of detailed intraoperative data by multiple surgeons. Among our specific group, no published data are available regarding inter- or intraobserver reliability of the surgeon-generated data, although several studies have shown that the arthroscopic grading of meniscal9 and cartilage22 lesions is reliable and reproducible among multiple surgeons operating at different medical centers.
As a cross-sectional investigation, this study examined only the effects of findings noted by the patient and the surgeon on the day of surgery. No conclusions can be drawn regarding changes in outcomes after surgery and what factors, if any, may modify these results. Previous studies have identified associations between baseline characteristics and outcomes after knee arthroscopy.28 Further research with postoperative outcome data on this cohort would certainly be helpful to identify whether the same predictors of preoperative pain and function have the same overwhelming effect on outcomes after surgery. Many surgeons would find it beneficial to understand what modifiable factors could be identified to predict outcomes after intervention. Although the KOOS is a widely used outcome measure for knee injuries, other measures may have different characteristics that make them more or less appropriate for certain abnormalities.32 Finally, our database does not include any information regarding radiographic or magnetic resonance imaging findings, although these are commonly obtained before the time of knee arthroscopy. Our hope is that the detailed documentation of intraoperative findings would more accurately describe the extent of the disease process.
Conclusion
In a large cohort of North American patients undergoing knee arthroscopy for nonreconstructive purposes, KOOS and VR-12 measures of baseline health were correlated with the patient demographic characteristics of sex, BMI, education level, and smoking status, as well as mental health as measured by the VR-12 MCS. Intraoperative findings did not consistently predict preoperative pain or function, as abnormal synovial status was associated only with worse KOOS-Pain scores. Surgeons should understand that patients’ preoperative pain and function levels may be more closely related to patient demographics and mental health than actual abnormality.
Acknowledgment
The authors thank the Cleveland Clinic orthopaedic patients, staff, and research personnel whose efforts related to regulatory issues, data collection, patient follow-up, data quality control, analyses, and manuscript preparation have made this consortium successful. The authors also thank Drs Thomas Anderson, Timothy Gajewski, Ryan Goodwin, David Gurd, Carlos Higuera, Robert Molloy, Michael Mont, Trevor Murray, Joseph Scarcella, Jonathan Schaffer, and Jim Williams for contributing cases, and William Messner, MA, MS, for statistical analysis. Finally, thanks to Brittany Stojsavljevic, editorial assistant, Cleveland Clinic Foundation, for editorial management.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: Research reported in this publication was partially supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under award No. R01 AR053684 (to K.P.S.) and under award No. K23 AR066133, which supported a portion of M.H.J.’s professional effort. The content is solely the responsibility of the authors and does not necessarily represent official views of the National Institutes of Health. M.C.B. has received educational support from Arthrex and Smith & Nephew and hospitality payments from Arthrex, DePuy Synthes, and Zimmer Biomet. R.W.W. has received educational support from Arthrex and Smith & Nephew and hospitality payments from Arthrex and Medical Device Business Solutions. A.D. has received educational support from Arthrex and Rock Medical and hospitality payments from Amniox, Arthrex, Conventus, Trice Medical, and Wright Medical. L.F. has received consulting fees from Zimmer Biomet and hospitality payments from the Musculoskeletal Transplant Foundation. M.S.H. has received educational support from Arthrex and Smith & Nephew and hospitality payments from Medical Device Business Solutions. A.M. has received consulting fees from Amniox Medical, Arthrosurface, Linvatec, and Stryker; speaking fees from Trice Medical; educational support from Rock Medical; and hospitality payments from Arthrex, DJO, and Smith & Nephew; receives royalties from Arthrosurface, Wolters Kluwer, and Zimmer Biomet; and has stock or stock options in Arthrosurface and Trice Medical. R.P. receives royalties from Zimmer Biomet and has received hospitality payments from the Musculoskeletal Transplant Foundation and Smith & Nephew. J.R. has received educational consulting fees from Smith & Nephew. P.S. has received consulting fees from Arthrex, educational support from Rock Medical, and hospitality payments from DJO, Medical Device Business Solutions, and the Musculoskeletal Transplant Foundation. K.P.S. has received research support from DonJoy and Smith & Nephew and hospitality payments from DePuy; receives royalties or consulting fees from the NFL, Cytori, and Mitek; and receives royalties from nPhase. K.S. has received honoraria from Fidia Pharma, educational support from Arthrex and Biomet, and hospitality payments from Horizon Pharma, MTS, Ramsay Medical, and Stryker. M.H.J. is a member of the Scientific Advisory Board for Samumed. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Cleveland Clinic Institutional Review Board.
References
- 1. Abtahi AM, Brodke DS, Lawrence BD, Zhang C, Spiker WR. Association between patient-reported measures of psychological distress and patient satisfaction scores after spine surgery. J Bone Joint Surg Am. 2015;97(10):824–828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Baldwin JN, McKay MJ, Simic M, et al. Self-reported knee pain and disability among healthy individuals: reference data and factors associated with the Knee injury and Osteoarthritis Outcome Score (KOOS) and KOOS-Child. Osteoarthritis Cartilage. 2017;25(8):1282–1290. [DOI] [PubMed] [Google Scholar]
- 3. Bedson J, Croft PR. The discordance between clinical and radiographic knee osteoarthritis: a systematic search and summary of the literature. BMC Musculoskelet Disord. 2008;9:116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Berliner JL, Brodke DJ, Chan V, SooHoo NF, Bozic KJ. Can preoperative patient-reported outcome measures be used to predict meaningful improvement in function after TKA? Clin Orthop Relat Res. 2017;475(1):149–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bhattacharyya T, Gale D, Dewire P, et al. The clinical importance of meniscal tears demonstrated by magnetic resonance imaging in osteoarthritis of the knee. J Bone Joint Surg Am. 2003;85(1):4–9. [DOI] [PubMed] [Google Scholar]
- 6. Boks SS, Vroegindeweij D, Koes BW, Hunink MM, Bierma-Zeinstra SM. Magnetic resonance imaging abnormalities in symptomatic and contralateral knees: prevalence and associations with traumatic history in general practice. Am J Sports Med. 2006;34(12):1984–1991. [DOI] [PubMed] [Google Scholar]
- 7. Brander VA, Stulberg SD, Adams AD, et al. Predicting total knee replacement pain: a prospective, observational study. Clin Orthop Relat Res. 2003;416:27–36. [DOI] [PubMed] [Google Scholar]
- 8. Cleveland RJ, Luong ML, Knight JB, et al. Independent associations of socioeconomic factors with disability and pain in adults with knee osteoarthritis. BMC Musculoskelet Disord. 2013;14:297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dunn WR, Wolf BR, Amendola A, et al. Multirater agreement of arthroscopic meniscal lesions. Am J Sports Med. 2004;32(8):1937–1940. [DOI] [PubMed] [Google Scholar]
- 10. Elson DW, Jones S, Caplan N, St Clair Gibson A, Stewart S, Kader DF. Clinically insignificant association between anterior knee pain and patellofemoral lesions which are found incidentally. Knee. 2013;20(6):471–475. [DOI] [PubMed] [Google Scholar]
- 11. Engelhart L, Nelson L, Lewis S, et al. Validation of the Knee injury and Osteoarthritis Outcome Score subscales for patients with articular cartilage lesions of the knee. Am J Sports Med. 2012;40(10):2264–2272. [DOI] [PubMed] [Google Scholar]
- 12. Englund M, Guermazi A, Gale D, et al. Incidental meniscal findings on knee MRI in middle-aged and elderly persons. N Engl J Med. 2008;359(11):1108–1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gatchel RJ, Polatin PB, Mayer TG. The dominant role of psychosocial risk factors in the development of chronic low back pain disability. Spine (Phila Pa 1976). 1995;20(24):2702–2709. [DOI] [PubMed] [Google Scholar]
- 14. Gauffin H, Tagesson S, Meunier A, Magnusson H, Kvist J. Knee arthroscopic surgery is beneficial to middle-aged patients with meniscal symptoms: a prospective, randomised, single-blinded study. Osteoarthritis Cartilage. 2014;22(11):1808–1816. [DOI] [PubMed] [Google Scholar]
- 15. Giesinger JM, Kuster MS, Behrend H, Giesinger K. Association of psychological status and patient-reported physical outcome measures in joint arthroplasty: a lack of divergent validity. Health Qual Life Outcomes. 2013;11:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Katz JN, Brophy RH, Chaisson CE, et al. Surgery versus physical therapy for a meniscal tear and osteoarthritis. N Engl J Med. 2013;368(18):1675–1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kim S, Bosque J, Meehan JP, Jamali A, Marder R. Increase in outpatient knee arthroscopy in the United States: a comparison of National Surveys of Ambulatory Surgery, 1996 and 2006. J Bone Joint Surg Am. 2011;93(11):994–1000. [DOI] [PubMed] [Google Scholar]
- 19. Liebensteiner MC, Nogler M, Giesinger JM, Lechner R, Lenze F, Thaler M. Cartilage degeneration and not age influences the health-related quality of life outcome after partial meniscectomy. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):26–31. [DOI] [PubMed] [Google Scholar]
- 20. Lo GH, McAlindon TE, Niu J, et al. Bone marrow lesions and joint effusion are strongly and independently associated with weight-bearing pain in knee osteoarthritis: data from the osteoarthritis initiative. Osteoarthritis Cartilage. 2009;17(12):1562–1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mansson O, Kartus J, Sernert N. Pre-operative factors predicting good outcome in terms of health-related quality of life after ACL reconstruction. Scand J Med Sci Sports. 2013;23(1):15–22. [DOI] [PubMed] [Google Scholar]
- 22. Marx RG, Connor J, Lyman S, et al. Multirater agreement of arthroscopic grading of knee articular cartilage. Am J Sports Med. 2005;33(11):1654–1657. [DOI] [PubMed] [Google Scholar]
- 23. Miranda H, Viikari-Juntura E, Martikainen R, Riihimaki H. A prospective study on knee pain and its risk factors. Osteoarthritis Cartilage. 2002;10(8):623–630. [DOI] [PubMed] [Google Scholar]
- 24. Nair A, Gan J, Bush-Joseph C, et al. Synovial chemokine expression and relationship with knee symptoms in patients with meniscal tears. Osteoarthritis Cartilage. 2015;23(7):1158–1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. O’Connor MI. Implant survival, knee function, and pain relief after TKA: are there differences between men and women? Clin Orthop Relat Res. 2011;469(7):1846–1851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Scanzello CR, McKeon B, Swaim BH, et al. Synovial inflammation in patients undergoing arthroscopic meniscectomy: molecular characterization and relationship to symptoms. Arthritis Rheum. 2011;63(2):391–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sihvonen R, Paavola M, Malmivaara A, et al. Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med. 2013;369(26):2515–2524. [DOI] [PubMed] [Google Scholar]
- 28. Spahn G, Muckley T, Kahl E, Hofmann GO. Factors affecting the outcome of arthroscopy in medial-compartment osteoarthritis of the knee. Arthroscopy. 2006;22(11):1233–1240. [DOI] [PubMed] [Google Scholar]
- 29. Thomee P, Wahrborg P, Borjesson M, Thomee R, Eriksson BI, Karlsson J. Self-efficacy of knee function as a pre-operative predictor of outcome 1 year after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2008;16(2):118–127. [DOI] [PubMed] [Google Scholar]
- 30. Tornbjerg SM, Nissen N, Englund M, et al. Structural pathology is not related to patient-reported pain and function in patients undergoing meniscal surgery. Br J Sports Med. 2017;51(6):525–530. [DOI] [PubMed] [Google Scholar]
- 31. Torres L, Dunlop DD, Peterfy C, et al. The relationship between specific tissue lesions and pain severity in persons with knee osteoarthritis. Osteoarthritis Cartilage. 2006;14(10):1033–1040. [DOI] [PubMed] [Google Scholar]
- 32. van de Graaf VA, Wolterbeek N, Scholtes VA, Mutsaerts EL, Poolman RW. Reliability and validity of the IKDC, KOOS, and WOMAC for patients with meniscal injuries. Am J Sports Med. 2014;42(6):1408–1416. [DOI] [PubMed] [Google Scholar]
- 33. Wang D, Jones MH, Khair MM, Miniaci A. Patient-reported outcome measures for the knee. J Knee Surg. 2010;23(3):137–151. [DOI] [PubMed] [Google Scholar]
- 34. Wylie JD, Suter T, Potter MQ, Granger EK, Tashjian RZ. Mental health has a stronger association with patient-reported shoulder pain and function than tear size in patients with full-thickness rotator cuff tears. J Bone Joint Surg Am. 2016;98(4):251–256. [DOI] [PubMed] [Google Scholar]