Short abstract
Although internal jugular vein stenosis (IJVS) is not uncommon, a lack of clinical attention will lead to misdiagnosis and missed diagnosis. This study describes two 61-year-old women with bilateral IJVS induced by tortuous internal carotid artery compression and reviews current reports on this condition, including its clinical characteristics and treatment strategies, to provide a reference for clinicians.
Keywords: Internal jugular vein stenosis, internal carotid artery tortuosity, extrinsic compression, jugular vein outflow disturbance, neuroimaging, case report
Introduction
Internal jugular vein stenosis (IJVS) is characterized by a series of nonspecific clinical manifestations associated with blood flow obstruction of the internal jugular vein (IJV), including headache, head noise, tinnitus, high-frequency hearing impairment, neck discomfort, stiffness, diplopia, blurred vision, visual field defect, insomnia, and even transient global amnesia.1–5 Because these manifestations are nonspecific and similar to the symptoms of some other diseases, such as mental and emotional disorders and ocular or ear diseases, IJVS is at risk of misdiagnosis and missed diagnosis. This study describes the clinical manifestations and diagnosis of bilateral IJVS induced by tortuous internal carotid artery (ICA) compression in two 61-year-old women. Additionally, current reports on this condition are reviewed and the clinical characteristics and treatment strategy of IJVS of this etiology are summarized to provide a reference for clinicians.
Case presentation
Case 1
A 61-year-old woman presented with an 11-year history of dryness and a feeling of high pressure in both eyes accompanied by headache. She reported that her headache had worsened approximately 2 weeks previously, especially in the right temporal region, with neck discomfort and insomnia. Her medical history included appendectomy in 1977, cholelithiasis in 2007, and retinal hemorrhage and cataract surgery in 2014. On presentation, her body temperature was 36°C, blood pressure was 130/80 mmHg, heart rate was 70 beats/minute, and respiratory rate was 15 breaths/minute. Neurological examination revealed no abnormalities.
Magnetic resonance imaging (MRI) of the brain revealed demyelination in the bilateral centrum semiovale and perivascular space in the right basal ganglia. Transcranial Doppler (TCD) examination showed no abnormalities. Carotid ultrasound revealed moderate intima–media thickening with multiple plaques in the bilateral carotid arteries, mild stenosis of the left subclavian artery, and a plaque in the wall of the right subclavian artery. However, jugular vein ultrasound showed severe stenosis in the J2 segment of the bilateral IJV (Table 1). Contrast-enhanced magnetic resonance venography (MRV) of the brain showed no abnormalities (Figure 1(a) and (b)). Contrast-enhanced MRV of the neck showed segmental stenosis in the bilateral IJVs due to compression of the adjacent ICAs. The bilateral vertebral venous plexuses were mildly dilated (Figure 1(c) and (d)). Computed tomography venography (CTV) also showed that the bilateral IJVs were compressed by the adjacent ICAs (Figure 1(e) and (f)). Lumbar puncture was not performed to evaluate the intracranial pressure because the patient declined.
Table 1.
Parameters of jugular ultrasound in Case 1.
| Side | Flow rate (cm/s) | Flow volume (mL/minute) | |
|---|---|---|---|
| Case 1 | Left IJV-J2 segment | 14 | 110 |
| Right IJV-J2 segment | 32 | 210 |
IJV, internal jugular vein.
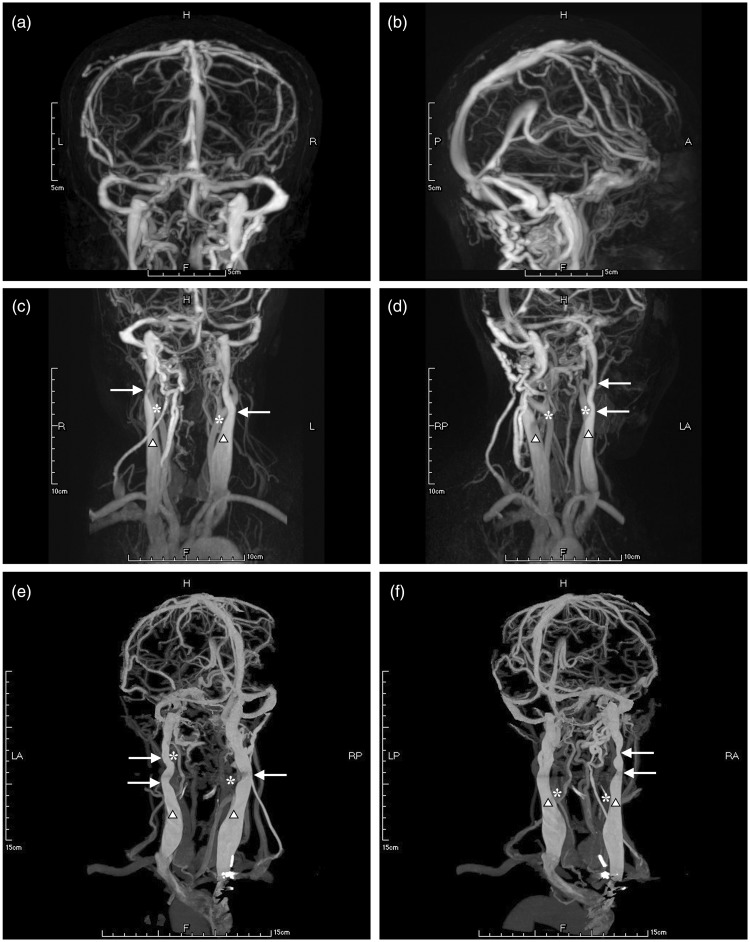
Figure 1.
Magnetic resonance venography images of the (a, b) head and (c, d) neck and (e, f) computed tomography venography images in Case 1. The white asterisk indicates the internal carotid artery, the black-edged white triangle indicates the internal jugular vein, and the white arrow indicates the focal stenosis.
The patient was treated with intravenous panax notoginseng saponin injection (Xueshuantong) at 450 mg/day, oral aspirin at 100 mg/day, oral atorvastatin at 20 mg/day (taken at night), oral probucol at 0.5 g twice a day, and oral 50% glycerol saline at 60 mL twice a day. Her symptoms attenuated after beginning this treatment.
Case 2
A 61-year-old woman presented with a 10-year history of intermittent headache, especially in the left temporal region, and bilateral high-frequency tinnitus. Four months before presentation, these symptoms had worsened and become accompanied by insomnia. She had no history of medications. On presentation, her body temperature was 36°C, blood pressure was 122/77 mmHg, heart rate was 64 beats/minute, and respiratory rate was 20 breaths/minute. Neurological examination revealed no abnormalities except for hearing decline in both ears.
Brain MRI revealed demyelination in the bilateral centrum semiovale and perivascular space in the bilateral basal ganglia. Fundus photography, optical coherence tomography, and TCD showed no abnormalities. Carotid ultrasound revealed a single plaque in the left carotid artery. Jugular vein ultrasound showed bilateral IJVS in the J2 segment (Table 2). Contrast-enhanced MRV of the brain showed no abnormalities (Figure 2(a) and (b)). Contrast-enhanced MRV of the neck showed focal stenosis in the J2–J3 segment of the bilateral IJV due to compression of the adjacent ICAs (Figure 2(c) and (d)). CTV also showed that the bilateral IJVs were compressed by the adjacent ICAs (Figure 2(e) and (f)). Catheter measurement of the trans-stenotic pressure was 5.2 cmH2O on the left side and 4.9 cmH2O on the right side.
Table 2.
Parameters of jugular ultrasound in Case 2.
| Side | Flow rate (cm/s) | Flow volume (mL/minute) | |
|---|---|---|---|
| Case 2 | Left IJV-J2 segment | 34 | 110 |
| Right IJV-J2 segment | 74 | 380 |
IJV, internal jugular vein.
Figure 2.
Magnetic resonance venography images of the (a, b) head and (c, d) neck and (e, f) computed tomography venography images in Case 2. The white asterisk indicates the internal carotid artery, the black-edged white triangle indicates the internal jugular vein, and the white arrow indicates the focal stenosis.
The patient was treated with intravenous ginaton at 70 mg/day, oral betahistine at 6 mg/day, and oral estazolam at 1 mg/day (taken at night). Her symptoms were partially resolved.
This case report was approved by the Ethics Board of Capital Medical University Xuanwu Hospital ([2019]006). Both patients reported in this case series signed a letter of consent for participation and publication.
Discussion
The reported etiologies of IJVS include congenital abnormalities (IJV aplasia or hypoplasia), thrombosis, autoimmune disorders, and extrinsic compression.1,6–9 IJV thrombosis can occur spontaneously or as a complication of surgery, central venous catheterization, head and neck infection, local malignancy, polycythemia, hyperhomocysteinemia, intravenous drug abuse, or neck massage.10 Cerebral venous outflow obstruction induced by IJVS can also predispose to cerebral venous sinus thrombosis.3,8 Autoimmune disorders, such as multiple sclerosis, are also involved in the pathogenesis of some cases of IJVS, and a series of studies reported structural abnormalities of the IJV in patients with multiple sclerosis.7,11–13
Some cases of IJVS might be attributed to extrinsic compression induced by the styloid process, digastric muscle, arteries, lymph nodes, sternocleidomastoid muscle, and thoracic outlet syndrome.6,9 Although IJVS caused by ICA compression was mentioned in one report,9 no detailed description of this condition has been reported until now. We have herein described two patients with bilateral IJVS caused by compression from the adjacent abnormal ICA.
Although the elevated trans-stenosis pressure gradients in the bilateral IJVS in Case 2 did not meet the criteria for stenting,2 the findings in this case highly suggest that the patient’s symptoms were correlated with IJVS. Headache may be correlated with IJVS-induced intravenous hypertension at the proximal end of the stenosis. Because the ophthalmic vein drains venous blood from the eyes into the cavernous sinus, the presence of IJVS aggravates the venous reflux from the eyes, thus explaining the feeling of high pressure in the eyes and the history of retinal hemorrhage in Case 1.14,15 The tinnitus and hearing decline in Case 2 were also considered to be correlated with intravenous hypertension. Endolymph is collected by the IJV through the inferior petrosal sinus. IJVS reportedly may lead to tinnitus, hearing loss, and disequilibrium due to disturbances of endolymph reflux.16–18 Moreover, the insomnia in both patients of the present study was correlated with their headache and tinnitus.
In both cases, the bilateral IJV were compressed by tortuous ICAs. Anatomically, arterial tortuosity is divided into tortuosity, coiling, and kinking.19 These abnormalities may occur congenitally, as in patients with ICA dysplasia and fibromuscular dysplasia.19,20 However, morphological changes of the ICA also increase with age, and arterial tortuosity occurs under pathogenic conditions. All types of hypertension, aneurysm, ectasia, and atherosclerosis may contribute to the tortuosity of the ICA.21–23
IJVS is diagnosed by neuroimaging. Although digital subtraction angiography is the gold standard for evaluating vascular stenosis,24 stronger evidence regarding the extrinsic compression in cases of IJVS would be provided by contrast-enhanced MRV in combination with three-dimensional CT of the neck. MRV may be preferable to CTV because of its high accuracy and low radiation.9 CTV can directly identify extrinsic osseous compression.9 Jugular vein ultrasound should also be performed because Laukontaus et al.25 reported that ultrasound is more sensitive than MRI in screening for IJVS. A reduced flow volume has also been identified in IJVS.26
According to previous studies, stenting seems to be a promising therapeutic option for focal stenosis of the dominant jugular vein. IJVS can be corrected by stenting when the trans-stenotic pressure gradient is ≥5.44 cmH2O.2 The first-line therapies for acute thrombotic-based IJVS are anticoagulation, thrombolysis, and endovascular treatment.27,28 However, the application of anticoagulation for acute suppurated infection-mediated thrombotic IJVS of the head and neck remains controversial; instead, antibiotics and surgical drainage of purulent collections are recommend for this condition.29,30 Thrombolysis and stenting are recommended for patients with IJV thrombosis secondary to IJVS.8 Because extrinsic compression accounts for a large proportion of IJVS, styloidectomy has reportedly been successfully applied in treating IJVS caused by compression from the styloid process.9 Furthermore, a novel method of IJV-to-innominate vein bypass has been reported to relieve symptoms.31 However, these findings require further study.
In the present study, the trans-stenotic pressure gradients in the bilateral IJVS in Case 2 did not meet the criteria for stenting2; therefore, the patient underwent medical therapy instead of stenting. Because no guideline is available for pharmacological treatment of IJVS, the medical treatment in this patient was based on our understanding of IJVS. Glycerol saline may help to reduce the intracranial pressure and intravenous hypertension, and reducing the compression of the IJV by the ICA may help to promote venous outflow and attenuate the symptoms. ginaton, Xueshuantong, aspirin, and statins may help to reduce the blood viscosity and inhibit arteriosclerosis aggravation. Betahistine and estazolam were symptomatic treatments. Stenting was not performed because of the concern that stenting at the stenotic segment of the IJV may lead to compression of the carotid bulb, which would further decrease the heart rate and blood pressure.
Conclusion
Compression by the tortuous ICA is one etiology of extrinsic compression-induced IJVS. Medications may be helpful in attenuating the symptoms.
Author contributions
Dr. Min Li contributed to the study design and drafting of the manuscript.
Dr. Chaoyang Su contributed to the analysis and interpretation of the data.
Dr. Chong Ching Chan contributed to the analysis and interpretation of the data.
Dr. Chunqiu Fan contributed to the acquisition of the data.
Dr. Ran Meng contributed to the acquisition of study funding, the study design, the analysis and interpretation of the data, and critical revision of the manuscript.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This study was partially supported by the National Key R&D Program (2017YFC1308401), the National Natural Science Foundation (81371289), and the Project of Beijing Municipal Top Talent of Healthy Work (2014-2-015) of China. The funding agencies had no role in the design and conduct of the study; in the collection, analysis, and interpretation of the data; or in the preparation, review, or approval of the manuscript.
References
- 1.Brinjikji W, Graffeo CS, Perry A. Moving target: transient rotational stenosis precipitating jugular bow hunter's syndrome. J Neurointerv Surg 2017; 9: e28. [DOI] [PubMed] [Google Scholar]
- 2.Zhou D, Meng R, Zhang X. Intracranial hypertension induced by internal jugular vein stenosis can be resolved by stenting. Eur J Neurol 2018; 25: 365–e13. [DOI] [PubMed] [Google Scholar]
- 3.Saponaro SA, Flanders AE, Friedman DP. Superior sagittal sinus thrombosis in the presence of idiopathic bilateral internal jugular vein stenosis. J Neuroimaging 1994; 4: 48–50. [DOI] [PubMed] [Google Scholar]
- 4.Saha MK, Hamieh T, Larkin B. Cerebral hemorrhage due to internal jugular vein stenosis in a hemodialysis patient. Clin Exp Nephrol 2012; 16: 345–349. [DOI] [PubMed] [Google Scholar]
- 5.Han K, Chao AC, Chang FC. Obstruction of venous drainage linked to transient global amnesia. PLoS One 2015; 10: e0132893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ahn SS, Miller TJ, Chen SW. Internal jugular vein stenosis is common in patients presenting with neurogenic thoracic outlet syndrome. Ann Vasc Surg 2014; 28: 946–950. [DOI] [PubMed] [Google Scholar]
- 7.Sethi SK, Daugherty AM, Gadda G. Jugular anomalies in multiple sclerosis are associated with increased collateral venous flow. AJNR Am J Neuroradiol 2017; 38: 1617–1622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huang P, Yang YH, Lin WC. Successful treatment of cerebral venous thrombosis associated with bilateral internal jugular vein stenosis using direct thrombolysis and stenting: a case report. Kaohsiung J Med Sci 2005; 21: 527–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jayaraman MV, Boxerman JL, Davis LM. Incidence of extrinsic compression of the internal jugular vein in unselected patients undergoing CT angiography. AJNR Am J Neuroradiol 2012; 33: 1247–1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leci-Tahiri L, Zherka-Saracini H, Tahiri A. Bilateral internal jugular vein thrombosis due to malignant tumor. J Med Case Rep 2018; 12: 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Al-Omari MH, Rousan LA. Internal jugular vein morphology and hemodynamics in patients with multiple sclerosis. Int Angiol 2010; 29: 115–120. [PubMed] [Google Scholar]
- 12.Radak D, Kolar J, Tanaskovic S. Morphological and haemodynamic abnormalities in the jugular veins of patients with multiple sclerosis. Phlebology 2012; 27: 168–172. [DOI] [PubMed] [Google Scholar]
- 13.Sethi SK, Utriainen DT, Daugherty AM. Jugular venous flow abnormalities in multiple sclerosis patients compared to normal controls. J Neuroimaging 2015; 25: 600–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bisaria KK. Anatomic variations of venous sinuses in the region of the torcular Herophili. J Neurosurg 1985; 62: 90–95. [DOI] [PubMed] [Google Scholar]
- 15.Smith KR., Jr. Idiopathic bilateral sigmoid sinus occlusion in a child: case report. J Neurosurg 1968; 29: 427–430. [DOI] [PubMed] [Google Scholar]
- 16.Ciccone MM, Scicchitano P, Gesualdo M. Idiopathic sudden sensorineural hearing loss and meniere syndrome: the role of cerebral venous drainage. Clin Otolaryngol 2018; 43: 230–239. [DOI] [PubMed] [Google Scholar]
- 17.Filipo R, Ciciarello F, Attanasio G. Chronic cerebrospinal venous insufficiency in patients with Meniere's disease. Eur Arch Otorhinolaryngol 2015; 272: 77–82. [DOI] [PubMed] [Google Scholar]
- 18.Chandler JR. Diagnosis and cure of venous hum tinnitus. The Laryngoscope 1983; 93: 892–895. [DOI] [PubMed] [Google Scholar]
- 19.Weibel J, Fields WS. Tortuosity, coiling, and kinking of the internal carotid artery. II. Relationship of morphological variation to cerebrovascular insufficiency. Neurology 1965; 15: 462–468. [DOI] [PubMed] [Google Scholar]
- 20.Sethi SS, Lau JF, Godbold J. The S curve: a novel morphological finding in the internal carotid artery in patients with fibromuscular dysplasia. Vasc Med 2014; 19: 356–362. [DOI] [PubMed] [Google Scholar]
- 21.Pancera P, Ribul M, Presciuttini B. Prevalence of carotid artery kinking in 590 consecutive subjects evaluated by Echocolordoppler. Is there a correlation with arterial hypertension? J Intern Med 2000; 248: 7–12. [DOI] [PubMed] [Google Scholar]
- 22.La Barbera G, La Marca G, Martino A. Kinking, coiling, and tortuosity of extracranial internal carotid artery: is it the effect of a metaplasia? Surg Radiol Anat 2006; 28: 573–580. [DOI] [PubMed] [Google Scholar]
- 23.Del Corso L, Moruzzo D, Conte B. Tortuosity, kinking, and coiling of the carotid artery: expression of atherosclerosis or aging? Angiology 1998; 49: 361–371. [DOI] [PubMed] [Google Scholar]
- 24.Jung SC, Kang DW, Turan TN. Vessel and vessel wall imaging. Front Neurol Neurosci 2016; 40: 109–123. [DOI] [PubMed] [Google Scholar]
- 25.Laukontaus SJ, Pekkola J, Numminen J. Magnetic resonance imaging of internal jugular veins in multiple sclerosis: interobserver agreement and comparison with doppler ultrasound examination. Ann Vasc Surg 2017; 42: 84–92. [DOI] [PubMed] [Google Scholar]
- 26.Ozen O, Unal O, Avcu S. Flow volumes of internal jugular veins are significantly reduced in patients with cerebral venous sinus thrombosis. Current neurovascular research 2014; 11: 75–82. [DOI] [PubMed] [Google Scholar]
- 27.Tajima H, Murata S, Kumazaki T. Successful interventional treatment of acute internal jugular vein thrombosis. AJR Am J Roentgenol 2004; 182: 467–469. [DOI] [PubMed] [Google Scholar]
- 28.Thomas RV, Reid W, Perry DJ. Internal jugular vein thrombosis following in-vitro fertilization in a woman with protein S deficiency and heterozygosity for the prothrombin 3' UTR mutation, despite anticoagulation with heparin. Blood Coagul Fibrinolysis 2001; 12: 487–489. [DOI] [PubMed] [Google Scholar]
- 29.Phua CK, Chadachan VM, Acharya R. Lemierre syndrome-should we anticoagulate? A case report and review of the literature. Int J Angiol 2013; 22: 137–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rebelo J, Nayan S, Choong K. To anticoagulate? Controversy in the management of thrombotic complications of head & neck infections. Int J Pediatr Otorhinolaryngol 2016; 88: 129–135. [DOI] [PubMed] [Google Scholar]
- 31.Ahmed A, Gloviczki P, Canton LG. Treatment of chronic headaches with internal jugular vein-to-innominate vein bypass. J Vasc Surg Venous Lymphat Disord 2017; 5: 878–879. [DOI] [PubMed] [Google Scholar]