Abstract
Background
Multimorbidity is a complex issue in modern medicine and a more nuanced understanding of how this phenomenon occurs over time is needed.
Aim
To determine the prevalence, characteristics, and patterns of patients living with multimorbidity, specifically the unique combinations (unordered patterns) and unique permutations (ordered patterns) of multimorbidity in primary care.
Design and setting
A retrospective cohort analysis of the prospectively collected data from 1990 to 2013 from the Canadian Primary Care Sentinel Surveillance Network electronic medical record database.
Method
Adult primary care patients who were aged ≥18 years at their first recorded encounter were followed over time. A list of 20 chronic condition categories was used to detect multimorbidity. Computational analyses were conducted using the Multimorbidity Cluster Analysis Tool to identify all combinations and permutations.
Results
Multimorbidity, defined as two or more and three or more chronic conditions, was prevalent among adult primary care patients and most of these patients were aged <65 years. Among female patients with two or more chronic conditions, 6075 combinations and 14 891 permutations were detected. Among male patients with three or more chronic conditions, 4296 combinations and 9716 permutations were detected. While specific patterns were identified, combinations and permutations became increasingly rare as the total number of chronic conditions and patient age increased.
Conclusion
This research confirms that multimorbidity is common in primary care and provides empirical evidence that clinical management requires a tailored, patient-centred approach. While the prevalence of multimorbidity was found to increase with increasing patient age, the largest proportion of patients with multimorbidity in this study were aged <65 years.
Keywords: electronic medical records, epidemiology, longitudinal study, multimorbidity, multiple chronic conditions, primary care
INTRODUCTION
The coexistence of multiple chronic conditions within an individual, also known as multimorbidity, is deemed the ‘norm rather than the exception’ in primary care and represents one of the most complex issues in modern medicine, yet it requires a more nuanced knowledge base and effective clinical practice.1–6 Multimorbidity has been linked with many adverse health outcomes including more frequent and longer hospitalisations,7–10 reduced functional status,11–14 potentially harmful polypharmacy,15–20 compromised patient safety,9,13,21–22 reduced quality of life or increased treatment burden,6,8,23–25 higher healthcare costs,13,26–28 and higher mortality.9,29–30 Creating a more informative profile of the accumulation of multiple chronic conditions over time is necessary and could provide much needed insight for a learning health system and a clinical approach that encourages both management and prevention.
More robust research that examines how multimorbidity develops over time and that uncovers the mechanisms through which these multiple chronic condition diagnoses accumulate will enhance the understanding of this increasing phenomenon.1,6,26,31–33 This requires more than calculating the crude and adjusted prevalence estimates of multimorbidity, and rather, describing the longitudinal patterns and progression of increasingly complex clinical profiles. Because of difficulties in computation, research has tended to examine categories of co-occurring conditions or the most common pairs or triplets.1,34–36 However, the conclusions that can be made from these studies are limited because the complexity of multimorbidity cannot be simplified into broad patterns or simple dyads and triads. Research is needed to determine all unique clusters that exist, in what sequence these multiple chronic conditions are diagnosed, and whether there are key predictors of this natural progression towards multimorbidity over time. This information can increase knowledge from somewhat redundant prevalence calculations, to articulating the dimensions of multimorbidity and then identifying individuals who would benefit from timely and tailored interventions for primary or secondary prevention.
The aim of this study was to determine the prevalence and characteristics of patients living with multimorbidity, as well as to describe the unique combinations (same chronic conditions without a specific sequence) and unique permutations (same chronic conditions with a specific sequence) of multimorbidity in primary care.
How this fits in
| There is a need to examine how multimorbidity develops over time to create a more nuanced understanding of this phenomenon. This study found that the largest proportion of patients with multimorbidity were aged <65 years, giving further support to the argument that multimorbidity is no longer just an issue for older patients and it must also be appropriately managed among younger patients. The study also found that the patterns of multimorbidity represented increasingly unique combinations and permutations, particularly as patient age and total number of chronic diseases increased, which builds from the international literature using a more in-depth analysis and describing a profile of multimorbidity using longitudinal clinical data. This research may lead to new approaches for improving the delivery of care for complex patients with multimorbidity, refocusing biomedical research on co-occurring chronic diseases, and informing more effective interventions for multimorbidity management and prevention. |
METHOD
Study design and participants
Data were derived from the Canadian Primary Care Sentinel Surveillance Network (CPCSSN) electronic medical record (EMR) database, which is a national database of longitudinal clinical data for primary care patients across Canada.37–40 This study was a retrospective cohort analysis of the prospectively collected data from 1990 to 2013. The methodological protocol for this study has been published elsewhere.41 Eligible patients were those receiving care from practices or providers who had consented to participating in the CPCSSN database. The representativeness of patient and provider characteristics has been compared with the broader Canadian population and it was identified that CPCSSN patients were slightly older than the age reported by the 2011 Canadian Census (mean age of CPCSSN patients was 3.5 years older), but followed the same patterns of sex distribution and residential location.38 Adult patients were included in the analyses if they had at least one in-office encounter recorded in their EMR and if they were aged ≥18 years as of their first encounter date. Those patients who did not have a detectable in-office encounter recorded, who were under the age of 18 years at their first encounter date, or who opted out of contributing their data to the CPCSSN database, were excluded from analyses.
Identifying chronic conditions and multimorbidity
Diagnostic codes were recorded using the International Classification of Diseases, ninth revision (ICD-9) system, which was used to detect individual chronic condition diagnoses. To identify adult primary care patients with multimorbidity, a list of 20 chronic condition categories and corresponding ICD-9 codes were used. This was based on work conducted by a national research project called ‘Patient-centred innovations for persons with multimorbidity’,42 which created a validated list based on previous multimorbidity literature and relevance to the primary care population.43 These 20 chronic condition categories, and corresponding ICD-9 codes, have been published elsewhere.41,43 The two common definitions of multimorbidity in the literature were used for this study: at least two and at least three chronic conditions.
Data collection and analysis
To form the CPCSSN database, EMR data are collected and de-identified from regional networks across eight Canadian provinces on a quarterly basis by data managers. Descriptive analyses were conducted using Stata software (version 14.1). The prevalence estimates and corresponding 95% confidence intervals (95% CI) were calculated using the total number of patients with at least two chronic conditions (MM2+) and the total number of patients with at least three chronic conditions (MM3+) as of the date of data extraction (30 September 2013). For both calculations, the denominator consisted of all adult patients in the final sample. To describe the characteristics of patients living with multimorbidity, mean and standard deviation (SD) were calculated for continuous variables, and distributions were explored among categorical variables.
To identify the number and type of unique combinations (unordered patterns) and unique permutations (ordered patterns) of multimorbidity, a computational analysis was conducted using a customised Java program called the Multimorbidity Cluster Analysis Tool.44 An example of a combination is those patients diagnosed with the same three chronic conditions (for example, cancer, obesity, and hypertension), regardless of sequence. For example, some patients may have been diagnosed first with obesity, then hypertension, and later develop cancer. Other patients may have been diagnosed with obesity, then cancer, and then hypertension. Both sets of patients are clustered into the same combination. An example of a permutation is those patients diagnosed with the same three chronic conditions (for example, cancer, obesity, and hypertension), in the same sequence. That is, all patients who are diagnosed with cancer, then with obesity, and then with hypertension are clustered within the same permutation. In comparison, those patients diagnosed with obesity, then with cancer, and then with hypertension, are clustered within a different permutation. To identify the unique combinations, all diagnoses recorded in a patient’s EMR, including those diagnosed on the same date, were included in the analysis. To identify the unique permutations, those chronic condition diagnoses recorded on the same date were removed.
RESULTS
Prevalence and characteristics of multimorbidity
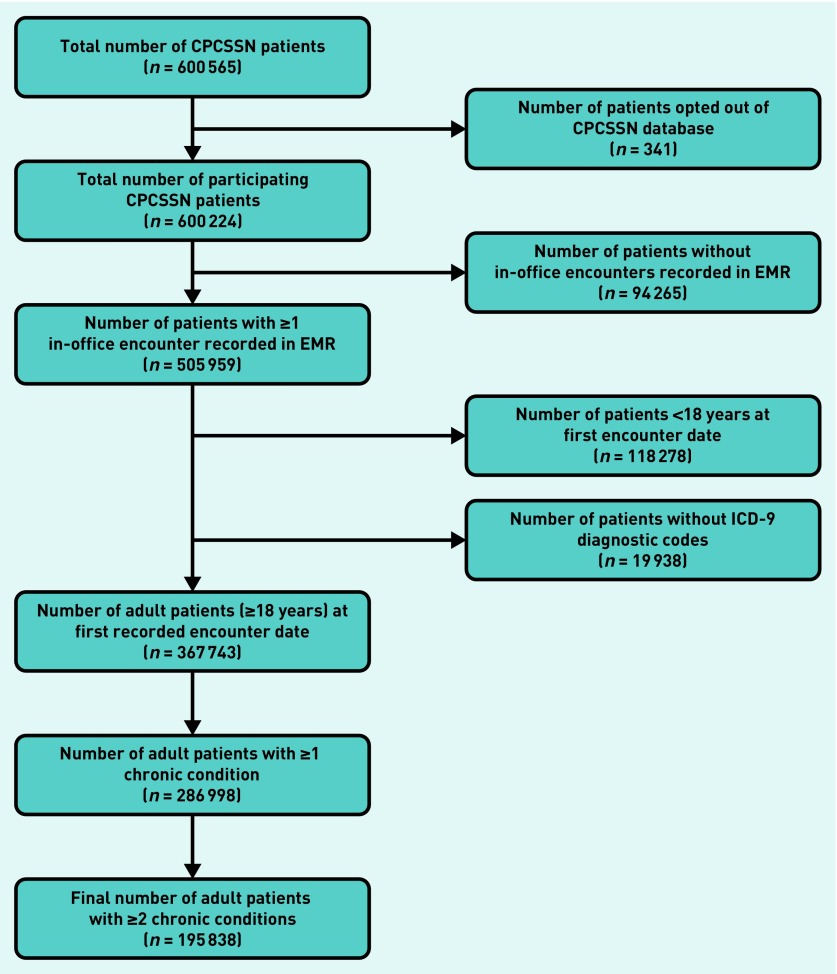
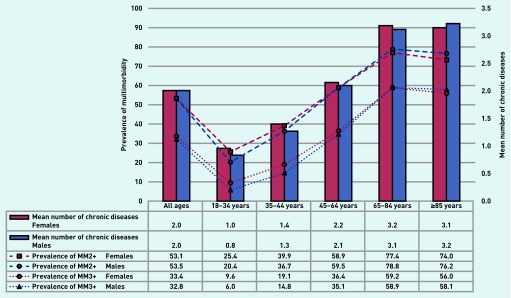
A total of 367 743 adult primary care patients were included in the final sample (Figure 1). As seen in Table 1, there were 195 838 (53.3%) adult primary care patients living with MM2+ and 121 864 (33.1%) adult primary care patients living with MM3+. The sex- and age group-stratified prevalence rates of multimorbidity (MM2+ and MM3+) are shown in Figure 2. This prevalence was observed among those patients who were already seeking care from their primary care provider. For both definitions of multimorbidity, there was an increase in prevalence across the age groups (until the age group of ≥85 years) for female and male patients. The characteristics of all adult patients, as well as those with multimorbidity, are presented in Table 1. Patients living with MM2+ had a mean age of 59.0 years (SD = 17.0) and patients living with MM3+ had a mean age of 62.7 years (SD = 15.9). For both definitions, the largest proportion of patients were between the ages of 45 and 64 years (MM2+ = 40.6%; MM3+ = 39.6%) and 61.7% of patients with MM2+ were <65 years.
Figure 1.
Inclusion flowchart for final sample of adult primary care patients with at least one in-office encounter recorded during the data extraction period. CPCSSN = Canadian Primary Care Sentinel Surveillance Network. EMR = electronic medical record. ICD-9 = International Classification of Diseases, ninth revision.
Table 1.
Characteristics of all adult primary care patients and those primary care patients with multimorbidity, defined as at least two chronic conditions (MM2+) or at least three chronic conditions (MM3+)
| Patient-level variable | All adult patients (n = 367 743) | Patients with MM2+ (n = 195 838) | Patients with MM3+ (n = 121 864) |
|---|---|---|---|
| Age in years | |||
| Mean (SD) | 52.3 (18.3) | 59.0 (17.0) | 62.7 (15.9) |
| Range | 18–114 | 18–114 | 18–114 |
|
| |||
| Age category, years, n (%) | |||
| 18–34 | 74 539 (20.3) | 17 466 (8.9) | 6119 (5.0) |
| 35–44 | 61 783 (16.8) | 23 855 (12.2) | 10 719 (8.8) |
| 45–64 | 134 550 (36.6) | 79 571 (40.6) | 48 254 (39.6) |
| 65–84 | 77 816 (21.2) | 60 696 (31.0) | 45 961 (37.7) |
| ≥85 | 19 055 (5.2) | 14 250 (7.3) | 10 811 (8.9) |
|
| |||
| Sex, n (%) | |||
| Female | 213 402a (58.0) | 113 209 (57.8) | 71 319 (58.5) |
| Male | 154 311a (42.0) | 82 629 (42.2) | 50 545 (41.5) |
|
| |||
| Residential location, n (%) | |||
| Rural | 59 740 (16.3) | 32 607 (16.7) | 22 274 (18.3) |
| Urban | 207 192 (56.3) | 102 151 (52.2) | 65 026 (53.4) |
| Missing | 100 811 (27.4) | 61 080 (31.2) | 34 564 (28.4) |
|
| |||
| Median household income (Canadian dollars) | |||
| Median (IQR) | 60 130 (12 497) | 60 952 (12 497) | 61 175 (12 497) |
| Range | 22 457–181 454 | 22 457–181 454 | 22 457–181 454 |
| Missing, n (%) | 100 811 (27.4) | 61 263 (31.3) | 34 662 (28.4) |
|
| |||
| Total number of chronic conditions | |||
| Mean (SD) | 2.0 (1.8) | 3.3 (1.5) | 4.2 (1.4) |
| Range | 0–14 | 2–14 | 3–14 |
There were missing data for sex for 30 patients (0.0%), but there was no missing data for sex for patients with MM2+ and patients with MM3+. IQR = Interquartile range.
Figure 2.
Mean number of chronic conditions and prevalence estimates of multimorbidity among adult primary care patients, stratified by age group and by sex.
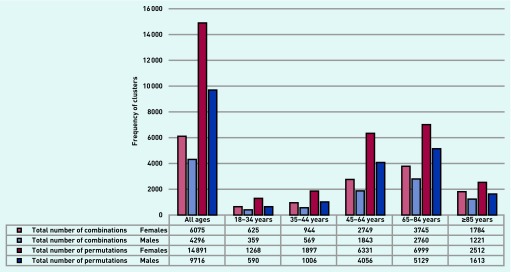
Total number of combinations and permutations
Following the computational analysis, the total number of unique combinations and unique permutations were calculated among each age group and for female and male patients (Figure 3). The total number of combinations in patients of all ages with MM2+ was 6075 for females and 4296 for males. After stratifying by age category, the largest number of unique combinations was detected among female and male patients aged 65–84 years, even though this was not the largest age group for patients with multimorbidity.
Figure 3.
Total number of unique combinations and unique permutations among patients with MM2+, stratified by age group and by sex.
The total number of permutations detected among female and male patients of all ages with multimorbidity was 14 891 and 9716, respectively. After stratifying by age category, the largest number of unique permutations was again detected among female and male patients aged 65–84 years. This indicates the complexity of those aged 65–84 years living with multimorbidity. Indeed, there were a large number of permutations that presented in a very low frequency of patients (13 858 permutations [4981 combinations] for less than five female patients and 8999 permutations [3565 combinations] for less than five male patients) (further information available from authors on request), signalling the distinct challenges of multimorbidity when specific patterns are considered.
Combinations and permutations of multimorbidity
The most frequent combinations and permutations, stratified by patient age, sex, and total number of chronic conditions, are presented in Table 2 and Table 3. Among female patients of all ages with MM2+, the most common combination was anxiety or depression and obesity (n = 3991; 3.5%) and the most common permutation was anxiety or depression followed by obesity (n = 1160; 2.4%). In comparison, among male patients of all ages with MM2+, the most common combination was hypertension and obesity (n = 3866; 4.7%) and the most common permutation was musculoskeletal problem followed by obesity (n = 1051; 3.5%).
Table 2.
Most frequent unique combination clusters for patients with MM2+, stratified by total number of chronic diseases and by sex
| Age group/Rankb | At least two chronic conditionsa | At least three chronic conditionsa | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Female | Male | Female | Male | |||||
|
|
|
|||||||
| Combinationc | n (%)d | Combinationc | n (%)d | Combinationc | n (%)d | Combinationc | n (%)d | |
| All ages, female: 113 209, male: 82 629 | ||||||||
| 1 | AD — OB | 3991 (3.5) | HT — OB | 3866 (4.7) | AD — MP — OB | 1621 (1.4) | HL — HT — OB | 1389 (1.7) |
| 2 | MP — OB | 3837 (3.4) | MP — OB | 3580 (4.3) | HT — MP — OB | 1019 (0.9) | DB — HT — OB | 1226 (1.5) |
| 3 | HT — OB | 3491 (3.1) | AD — OB | 2431 (2.9) | DB — HT — OB | 869 (0.8) | HT — MP — OB | 1061 (1.3) |
|
| ||||||||
| 18–34 years; female: 11 507, male: 5959 | ||||||||
| 1 | AD — OB | 1197 (10.4) | AD — OB | 713 (12.0) | AD — MP — OB | 373 (3.2) | AD — MP — OB | 171 (2.9) |
| 2 | MP — OB | 817 (7.1) | MP — OB | 648 (10.9) | AD — CA — OB | 205 (1.8) | CA — MP — OB | 67 (1.1) |
| 3 | AD — MP | 608 (5.3) | AD — MP | 422 (7.1) | AD — COPDA — OB | 131 (1.1) | AD — CA — OB | 60 (1.0) |
|
| ||||||||
| 35–44 years; female: 14 756, male: 9098 | ||||||||
| 1 | AD — OB | 1140 (7.7) | MP — OB | 932 (10.2) | AD — MP — OB | 483 (3.3) | AD — MP — OB | 241 (2.6) |
| 2 | MP — OB | 1034 (7.0) | AD — OB | 653 (7.2) | AD — CA — OB | 234 (1.6) | HT — MP — OB | 127 (1.4) |
| 3 | CA — OB | 654 (4.4) | HT — OB | 479 (5.3) | CA — MP — OB | 170 (1.2) | CA — MP — OB | 122 (1.3) |
|
| ||||||||
| 45–64 years; female: 44 712, male: 34 856 | ||||||||
| 1 | MP — OB | 1693 (3.8) | HT — OB | 1999 (5.7) | AD — MP — OB | 680 (1.5) | HL — HT — OB | 785 (2.3) |
| 2 | HT — OB | 472 (1.1) | MP — OB | 1725 (4.9) | HT — MP — OB | 551 (1.2) | HT — MP — OB | 605 (1.7) |
| 3 | AD — OB | 404 (0.9.) | HL — OB | 1310 (3.8) | CA — MP — OB | 426 (1.0) | DB — HT — OB | 559 (1.6) |
|
| ||||||||
| 65–84 years; female: 33 264, male: 27 430 | ||||||||
| 1 | HT — OB | 1181 (3.6) | HT — OB | 1092 (4.0) | DB — HT — OB | 427 (1.3) | DB — HT — OB | 536 (2.0) |
| 2 | DB — OB | 146 (0.4) | DB — OB | 678 (2.5) | HL — HT — OB | 386 (1.2) | HL — HT — OB | 468 (1.7) |
| 3 | CA — OB | 343 (1.0) | CA — OB | 377 (1.4) | HT — MP — OB | 292 (0.9) | CA — HT — OB | 262 (1.0) |
|
| ||||||||
| ≥85 years; female: 8970, male: 5279 | ||||||||
| 1 | HT — OB | 212 (2.4) | CA — HT | 42 (0.8) | DB — HT — OB | 59 (0.7) | DB — HT — OB | 53 (1.0) |
| 2 | DE — HT | 151 (1.7) | HT — OB | 41 (0.8) | HT — OB — ORA | 54 (0.6) | CD — HT — OB | 38 (0.7) |
| 3 | CD — HT | 126 (1.4) | CD — HT | 36 (0.7) | CA — HT — OB | 53 (0.6) | CA — HT — OB | 29 (0.5) |
Including data points where the time elapsing between chronic condition diagnoses was 0 days.
Rank indicates that the combinations are listed in order of frequency (starting with most frequent).
Combinations presented in alphabetical order.
Proportion of age group. AD = Anxiety or Depression. CA = Cancer. CD = Cardiovascular Disease. COPDA = Chronic Obstructive Pulmonary Disease or Asthma. DB = Diabetes. DE = Dementia. HL = Hyperlipidemia. HT = Hypertension. MP = Musculoskeletal Problem. OB = Obesity. ORA = Osteoarthritis or Rheumatoid Arthritis. The hyphens between conditions are used to identify combinations (unordered patterns).
Table 3.
Most frequent unique permutation clusters for patients with MM2+, stratified by total number of chronic conditions and by sex
| Age group/Rankb | At least two chronic conditionsa | At least three chronic conditionsa | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Female | Male | Female | Male | |||||
|
|
|
|||||||
| Permutation c | n (%)d | Permutationc | n (%)d | Permutationc | n (%)d | Permutationc | n (%)d | |
| All ages; female: 47 381, male: 30 478 | ||||||||
| 1 | AD ➔ OB | 1160 (2.4) | MP ➔ OB | 1051 (3.5) | AD ➔ OB ➔ MP | 177 (0.4) | HT ➔ OB ➔ HL | 675 (2.2) |
| 2 | MP ➔ OB | 1094 (2.3) | HT ➔ OB | 1179 (3.9) | MP ➔ OB ➔ AD | 176 (0.4) | HT ➔ OB ➔ MP | 374 (1.2) |
| 3 | AD ➔ MP | 909 (1.9) | AD ➔ OB | 1132 (3..8) | AD ➔ MP ➔ OB | 161 (0.3) | DB ➔ OB ➔ HT | 365 (1.2) |
|
| ||||||||
| 18–34 years; female: 5565, male: 2624 | ||||||||
| 1 | AD ➔ OB | 388 (7.0) | MP ➔ OB | 443 (16.9) | MP ➔ OB ➔ AD | 41 (0.7) | AD ➔ OB ➔ MP | 157 (6.0) |
| 2 | AD ➔ MP | 249 (4.5) | AD ➔ OB | 397 (15.1) | AD ➔ OB ➔ MP | 41 (0.7) | AD ➔ MP ➔ OB | 67 (3.0) |
| 3 | MP ➔ OB | 245 (4.4) | AD ➔ MP | 253 (9.7) | MP ➔ AD ➔ OB | 37 (0.7) | MP ➔ AD ➔ OB | 61 (2.3) |
|
| ||||||||
| 35–44 years; female: 6747, male: 3583 | ||||||||
| 1 | AD ➔ OB | 327 (4.8) | MP ➔ OB | 497 (14..0) | AD ➔ MP ➔ OB | 57 (0.8) | AD ➔ OB ➔ MP | 203 (5.7) |
| 2 | MP ➔ OB | 318 (4.7) | AD ➔ OB | 333 (9.2) | AD ➔ OB ➔ MP | 51 (0.8) | MP ➔ OB ➔ AD | 115 (3.2) |
| 3 | AD ➔ MP | 256 (3.8) | MP ➔ AD | 330 (9.2) | MP ➔ OB ➔ AD | 48 (0.7) | MP ➔ AD ➔ OB | 76 (2.1) |
|
| ||||||||
| 45–64 years; female: 18 426, male: 12 372 | ||||||||
| 1 | MP ➔ OB | 456 (2.5) | MP ➔ OB | 674 (5.4) | HT ➔ OB ➔ MP | 87 (0.5) | HT ➔ OB ➔ HL | 291 (2.4) |
| 2 | AD ➔ OB | 400 (2.2) | HT ➔ OB | 472 (3.8) | AD ➔ OB ➔ MP | 80 (0.4) | MP ➔ OB ➔ HL | 205 (1.7) |
| 3 | AD ➔ MP | 365 (2.0) | AD ➔ OB | 404 (3.3) | MP ➔ OB ➔ AD | 78 (0.4) | MP ➔ OB ➔ HT | 162 (1.3) |
|
| ||||||||
| 65–84 years: female: 12 819, male: 9652 | ||||||||
| 1 | HT ➔ OB | 322 (2.5) | HT ➔ OB | 323 (3.3) | HT ➔ OB ➔ HL | 48 (0.4) | DB ➔ OB ➔ HT | 129 (1.3) |
| 2 | HT ➔ MP | 102 (0.8) | DB ➔ OB | 158 (1.7) | HT ➔ OB ➔ MP | 46 (0.4) | HT ➔ OB ➔ MP | 100 (1.0) |
| 3 | HT ➔ HL | 98 (0.8) | HT ➔ HL | 147 (1.6) | DB ➔ OB ➔ HT | 42 (0.3) | HT ➔ OB ➔ HL | 97 (1.0) |
|
| ||||||||
| ≥85 years: female: 3824, male: 2247 | ||||||||
| 1 | HT ➔ OB | 62 (1.6) | HT ➔ OB | 76 (3.4) | HT ➔ OB ➔ ORA | 15 (0.4) | DB ➔ OB ➔ HT | 31 (1.4) |
| 2 | HT ➔ DE | 53 (1.4) | HT ➔ CA | 69 (3.1) | HT ➔ OB ➔ CA | 14 (0.4) | HT ➔ OB ➔ MP | 26 (1.2) |
| 3 | HT ➔ CD | 44 (1.2) | HT ➔ CD | 63 (2.9) | HT ➔ OB ➔ MP | 12 (0.3) | HT ➔ OB ➔ CA | 21 (1.0) |
Excluding data points where the time elapsing between chronic condition diagnoses was zero days.
Rank indicates that the permutations are listed in order of frequency (starting with most frequent).
Permutations presented in temporal order.
Proportion of age group and results representing <5 patients within age group supressed. AD = Anxiety or Depression. CA = Cancer. CD = Cardiovascular Disease. DB = Diabetes. DE = Dementia. HL = Hyperlipidemia. HT = Hypertension. MP = Musculoskeletal Problem. OB = Obesity. ORA = Osteoarthritis or Rheumatoid Arthritis. The arrows between conditions are used to identify permutations (ordered patterns).
As seen in Table 2, the most prevalent combination among the youngest age groups was anxiety or depression and obesity, identified among those aged 18–34 years (10.4% and 12.0% among female and male patients, respectively) and 35–44 years (7.7%) among female patients. The most prevalent combination among male patients aged 35–44 years was musculoskeletal problem and obesity (10.2%).
As seen in Table 3, there was a clear distinction between patients aged 18–64 years whose most prevalent first diagnosis was anxiety or depression, as compared with patients aged ≥65 years whose most prevalent first diagnosis was hypertension. (Among patients aged 45–64 years, musculoskeletal problem was detected as a prevalent first diagnosis, potentially due to the diagnosis of ongoing back pain [and other chronic pain] among patients [both females and males] in this age group.) The type of combinations and permutations that were detected became increasingly rare as two characteristics increased: patient age and the total number of chronic conditions.
As a result of these small clusters, results were suppressed where less than five patients were included in an ordered sequence. Data for patients with at least four chronic conditions are available from the authors on request.
Prevalence of individual chronic conditions and frequency of occurrence in patterns
The prevalence estimates of the individual chronic condition categories among all adult patients, as well as patients with multimorbidity, are available from the authors on request. The most prevalent chronic condition diagnoses were obesity, hypertension, musculoskeletal problem, and anxiety or depression. The least prevalent chronic condition diagnoses among both groups were stroke or transient ischaemic attack, liver disease, and kidney disease or failure.
Each of these chronic conditions had a prevalence of <1% for female and male patients. The frequency with which individual chronic conditions appeared in combinations, permutations, and as the first chronic condition within permutations are available from the authors on request. Hypertension, obesity, and musculoskeletal problem were present in approximately 50% of combinations and 50% of permutations for females and males.
Hypertension was the only chronic condition that presented as the first chronic condition in >20% of permutations among patients.
DISCUSSION
Summary
To the authors’ knowledge, this is the first study to investigate the combinations and permutations of multimorbidity in a national EMR database using a longitudinal and computational approach. This study found that among the sample of adult primary care patients, approximately one in two and one in three patients were living with MM2+ and MM3+, respectively. For both definitions, the largest proportion of patients with multimorbidity was aged <65 years. The current study also found that the patterns of multimorbidity represented increasingly unique combinations and permutations, demonstrating that multimorbidity should be explored at a more in-depth level than identifying pairs or triplets of chronic conditions. Some of the patterns that were detected were logical clinically (for example, co-occurrences of obesity, musculoskeletal problem, and anxiety or depression), but there were thousands of combinations and permutations that included fewer than five patients. There were 4981 combinations and 13 858 permutations with fewer than five female patients and 3565 combinations and 8999 permutations with fewer than five male patients.
Strengths and limitations
A strength of this study was the longitudinal EMR data that allowed for the study of multimorbidity over time and the identification of frequent and rare clinical profiles. In addition, the computational analysis used can be applied to longitudinal datasets in other settings. Limitations include the fact that the CPCSSN database does not capture variables that can be particularly important in the progression of multimorbidity, such as condition severity or self-management; the measure of multimorbidity did not distinguish between transient or controlled chronic conditions; and the estimate of multimorbidity was determined among those patients who were already seeking care from their primary care provider, which may have produced artificially high rates.
Finally, the use of EMR data may have introduced the potential for misclassification of chronic condition occurrence because diagnostic information may not have been recorded or extracted properly from the EMR systems and into the EMR database. This is an important consideration when using EMR data for epidemiological research because these data are collected for clinical, not research, purposes.45–47
Comparison with existing literature
The prevalence estimates of multimorbidity in this study are comparable with many international estimates to date. More specifically, the findings were most comparable with prevalence estimates from the UK at 58.0%,26 the US at 45.2%,48 and Australia at 47.4%.49 The findings that adult primary care patients with multimorbidity tended to be older and female has been corroborated in the existing literature.50–55 While the prevalence of multimorbidity increased as patient age increased, the largest proportion of patients in the current study was aged <65 years. This is consistent with previous literature highlighting the growing burden of multimorbidity among younger cohorts. For example, a study conducted by Ryan et al 56 examined rates of multimorbidity in the province of Ontario and concluded that the ‘common rhetoric’ around the ‘grey tsunami’ is incorrect because the volume of multimorbidity is beginning in younger individuals. It is clear that multimorbidity is no longer an issue of older patients and it must be appropriately managed among younger patients.26,51,56,57
A study conducted by van den Bussche et al 58 examined multimorbidity clusters in primary care data in Germany, which found similar trends for the most prevalent individual chronic conditions (such as hypertension, chronic low back pain, diabetes, and joint arthrosis) and a very large number of unique combinations of multimorbidity. In these data, 10 426 combinations (from a list of 45 chronic conditions) were detected.58 This work is comparable with the current study, which used less than half the number of chronic conditions and found about half the number of combinations in the primary care data.
Implications for research
These in-depth analyses contribute to the global research on multimorbidity,1,59 and identify distinct ‘types’ of multimorbidity in specific age groups of patients, and support the need for care delivery that accounts for the evolution of multimorbidity over time.60– 63 While beyond the scope of the current research, the findings reported in this article could be used to re-examine the potential for effective case management through a more tailored approach to multimorbidity and a more integrated set of health services. Indeed, this research provides empirical evidence of the nuanced complexity of patients living with multimorbidity and the corresponding need for individualised and patient-centred delivery of clinical care.
Acknowledgments
The authors would like to thank the primary care providers and patients who contribute valuable data to the CPCSSN database.
Funding
During the completion of this study, Kathryn Nicholson was supported by the Schulich School of Medicine and Dentistry, the Ontario Graduate Scholarship, and the Canadian Institute for Health Research Strategic Training Program: Transdisciplinary Understanding and Training on Research in Primary Health Care. Martin Fortin was supported by an Applied Chair in Health Services and Policy Research on Chronic Diseases in Primary Care. Amardeep Thind was supported by a Canada Research Chair in Health Services Research.
Ethical approval
The use of the data was approved by the CPCSSN Surveillance and Research Standing Committee and ethical approval was obtained from the Research Ethics Board at Western University, London, Ontario, Canada (reference number is #104705).
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Xu X, Mishra GD, Jones M. Mapping the global research landscape and knowledge gaps on multimorbidity: a bibliometric study. J Glob Health. 2017;7(1):010414. doi: 10.7189/jogh.07.010414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vetrano DL, Calderón-Larrañaga A, Marengoni A, et al. An international perspective on chronic multimorbidity: approaching the elephant in the room. J Gerontol A Biol Sci Med Sci. 2018;73(10):1350–1356. doi: 10.1093/gerona/glx178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ramond-Roquin A, Fortin M. Towards increased visibility of multimorbidity research. J Comorb. 2016;6(2):42–45. doi: 10.15256/joc.2016.6.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moffat K, Mercer SW. Challenges of managing people with multimorbidity in today’s healthcare systems. BMC Fam Pract. 2015;16:129–132. doi: 10.1186/s12875-015-0344-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mercer SW, Salisbury C, Fortin M, editors. ABC of Multimorbidity. Oxford: John Wiley & Sons; 2014. [Google Scholar]
- 6.Boyd CM, Fortin M. Future of multimorbidity research: how should understanding of multimorbidity inform health system design? Public Health Rev. 2010;32(2):451–474. [Google Scholar]
- 7.Gruneir A, Bronskill SE, Maxwell CJ, et al. The association between multimorbidity and hospitalization is modified by individual demographics and physician continuity of care: a retrospective cohort study. BMC Health Serv Res. 2016;16:154–163. doi: 10.1186/s12913-016-1415-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Agborsangaya CB, Lau D, Lahtinen M, et al. Health-related quality of life and healthcare utilization in multimorbidity: results of a cross-sectional survey. Qual Life Res. 2013;22(4):791–799. doi: 10.1007/s11136-012-0214-7. [DOI] [PubMed] [Google Scholar]
- 9.Gijsen R, Hoeymans N, Schellevis FG, et al. Causes and consequences of comorbidity: a review. J Clin Epidemiol. 2001;54(7):661–674. doi: 10.1016/s0895-4356(00)00363-2. [DOI] [PubMed] [Google Scholar]
- 10.Librero J, Peiró S, Ordiñana R. Chronic comorbidity and outcomes of hospital care: length of stay, mortality, and readmission at 30 and 365 days. J Clin Epidemiol. 1999;52(3):171–179. doi: 10.1016/s0895-4356(98)00160-7. [DOI] [PubMed] [Google Scholar]
- 11.Griffith LE, Gruneir A, Fisher K, et al. Patterns of health service use in community living older adults with dementia and comorbid conditions: a population-based retrospective cohort study in Ontario, Canada. BMC Geriatr. 2016;16(1):177–187. doi: 10.1186/s12877-016-0351-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ryan A, Wallace E, O’Hara P, Smith SM. Multimorbidity and functional decline in community-dwelling adults: a systematic review. Health Qual Life Outcomes. 2015;13:168–181. doi: 10.1186/s12955-015-0355-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vogeli C, Shields AE, Lee TA, et al. Multiple chronic conditions: prevalence, health consequences, and implications for quality, care management, and costs. J Gen Intern Med. 2007;22(suppl 3):391–395. doi: 10.1007/s11606-007-0322-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bayliss EA, Bayliss MS, Ware JE, Jr, Steiner JF. Predicting declines in physical function in persons with multiple chronic medical conditions: what we can learn from the medical problem list. Health Qual Life Outcomes. 2004;2:47–55. doi: 10.1186/1477-7525-2-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mangin D, Heath I. Multimorbidity and quaternary prevention (P4) Brazilian Journal of Family and Community Medicine. 2015;10(35):1–5. [Google Scholar]
- 16.Lorgunpai SJ, Grammas M, Lee DS, et al. Potential therapeutic competition in community-living older adults in the U.S.: use of medications that may adversely affect a coexisting condition. PLoS One. 2014;9(2):e89447. doi: 10.1371/journal.pone.0089447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Calderón-Larrañaga A, Poblador-Plou B, González-Rubio F, et al. Multimorbidity, polypharmacy, referrals, and adverse drug events: are we doing things well? Br J Gen Pract. :2012. doi: 10.3399/bjgp12X659295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith SM, O’Dowd T. Chronic diseases: what happens when they come in multiples? Br J Gen Pract. 2007;57:268–270. [PMC free article] [PubMed] [Google Scholar]
- 19.Boyd CM, Darer J, Boult C, et al. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance. JAMA. 2005;294(6):716–724. doi: 10.1001/jama.294.6.716. [DOI] [PubMed] [Google Scholar]
- 20.Tinetti ME, Bogardus ST, Jr, Agostini JV. Potential pitfalls of disease-specific guidelines for patients with multiple conditions. N Engl J Med. 2004;351(27):2870–2874. doi: 10.1056/NEJMsb042458. [DOI] [PubMed] [Google Scholar]
- 21.Panagioti M, Stokes J, Esmail A, et al. Multimorbidity and patient safety incidents in primary care: a systematic review and meta-analysis. PLoS One. 2015;10(8):e0135947. doi: 10.1371/journal.pone.0135947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zulman DM, Asch SM, Martins SB, et al. Quality of care for patients with multiple chronic conditions: the role of comorbidity interrelatedness. J Gen Intern Med. 2014;29(3):529–537. doi: 10.1007/s11606-013-2616-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rosbach M, Andersen JS. Patient-experienced burden of treatment in patients with multimorbidity: a systematic review of qualitative data. PLoS One. 2017;12(6):e0179916. doi: 10.1371/journal.pone.0179916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gill A, Kuluski K, Jaakkimainen L, et al. “Where do we go from here?” Health system frustrations expressed by patients with multimorbidity, their caregivers and family physicians. Healthc Policy. 2014;9(4):73–89. [PMC free article] [PubMed] [Google Scholar]
- 25.Fortin M, Dubois MF, Hudon C, et al. Multimorbidity and quality of life: a closer look. Health Qual Life Outcomes. 2007;5:52. doi: 10.1186/1477-7525-5-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Salisbury C, Johnson L, Purdy S, et al. Epidemiology and impact of multimorbidity in primary care: a retrospective cohort study. Br J Gen Pract. :2011. doi: 10.3399/bjgp11X548929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hartmann J, Hehner S, Hemmrich K, et al. Providing better care at lower cost for multimorbid patients. Health International. 2011;11:38–47. [Google Scholar]
- 28.Rapoport J, Jacobs P, Bell NR, Klarenbach S. Refining the measurement of the economic burden of chronic diseases in Canada. Chronic Dis Can. 2004;25(1):13–21. [PubMed] [Google Scholar]
- 29.Nunes BP, Flores TR, Mielke GI, et al. Multimorbidity and mortality in older adults: a systematic review and meta-analysis. Arch Gerontol Geriatr. 2016;67:130–138. doi: 10.1016/j.archger.2016.07.008. [DOI] [PubMed] [Google Scholar]
- 30.St John PD, Tyas SL, Menec V, Tate R. Multimorbidity, disability, and mortality in community-dwelling older adults. Can Fam Physician. 2014;60(5):e272–e280. [PMC free article] [PubMed] [Google Scholar]
- 31.Strauss VY, Jones PW, Kadam UT, Jordan KP. Distinct trajectories of multimorbidity in primary care were identified using latent class growth analysis. J Clin Epidemiol. 2014;67(10):1163–1171. doi: 10.1016/j.jclinepi.2014.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.France EF, Wyke S, Gunn JM, et al. Multimorbidity in primary care: a systematic review of prospective cohort studies. Br J Gen Pract. :2012. doi: 10.3399/bjgp12X636146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mercer SW, Gunn J, Wyke S. Improving the health of people with multimorbidity: the need for prospective cohort studies. J Comorb. 2011;1:4–7. doi: 10.15256/joc.2011.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Garin N, Koyanagi A, Chatterji S, et al. Global multimorbidity patterns: a cross-sectional, population-based, multi-country study. J Gerontol A Biol Sci Med Sci. 2016;71(2):205–214. doi: 10.1093/gerona/glv128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Violan C, Foguet-Boreu Q, Flores-Mateo G, et al. Prevalence, determinants and patterns of multimorbidity in primary care: a systematic review of observational studies. PLoS One. 2014;9(7):e102149. doi: 10.1371/journal.pone.0102149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Prados-Torres A, Calderón-Larrañaga A, Hancco-Saavedra J, et al. Multimorbidity patterns: a systematic review. J Clin Epidemiol. 2014;67(3):254–266. doi: 10.1016/j.jclinepi.2013.09.021. [DOI] [PubMed] [Google Scholar]
- 37.Garies S, Birtwhistle R, Drummond N, et al. Data Resource Profile: National electronic medical record data from the Canadian Primary Care Sentinel Surveillance Network (CPCSSN) Int J Epidemiol. 2017;46(4):1091f–1092f. doi: 10.1093/ije/dyw248. [DOI] [PubMed] [Google Scholar]
- 38.Queenan JA, Williamson T, Khan S, et al. Representativeness of patients and providers in the Canadian Primary Care Sentinel Surveillance Network: a cross-sectional study. CMAJ Open. 2016;4(1):E28–E32. doi: 10.9778/cmajo.20140128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.CPCSSN . Canadian Primary Care Sentinel Surveillance Network. Kingston ON: CPCSSN; 2016. http://cpcssn.ca/ (accessed 21 May 2019) [Google Scholar]
- 40.Birtwhistle RV. Canadian Primary Care Sentinel Surveillance Network: a developing resource for family medicine and public health. Can Fam Physician. 2011;57(10):1219–1220. [PMC free article] [PubMed] [Google Scholar]
- 41.Nicholson K, Terry AL, Fortin M, et al. Examining the prevalence and patterns of multimorbidity in Canadian primary healthcare: a methodologic protocol using a national electronic medical record database. J Comorb. 2015;5:150–161. doi: 10.15256/joc.2015.5.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stewart M, Fortin M. Patient-centred innovations for persons with multimorbidity: funded evaluation protocol. CMAJ Open. 2017;5(2):E365–E372. doi: 10.9778/cmajo.20160097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fortin M, Almirall J, Nicholson K. Development of a research tool to document self-reported chronic conditions in primary care. J Comorb. 2017;7(1):117–123. doi: 10.15256/joc.2017.7.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nicholson K, Bauer M, Terry A, et al. The Multimorbidity Cluster Analysis Tool: identifying combinations and permutations of multiple chronic diseases using a record-level computational analysis. J Innov Health Inform. 2017;24(4):962. doi: 10.14236/jhi.v24i4.962. [DOI] [PubMed] [Google Scholar]
- 45.Terry AL, Stewart M, Fortin M, et al. Gaps in primary healthcare electronic medical record research and knowledge: findings of a pan-Canadian study. Healthc Policy. 2014;10(1):46–59. [PMC free article] [PubMed] [Google Scholar]
- 46.Häyrinen K, Saranto K, Nykänen P. Definition, structure, content, use and impacts of electronic health records: a review of the research literature. Int J Med Inform. 2008;77(5):291–304. doi: 10.1016/j.ijmedinf.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 47.Thiru K, Hassey A, Sullivan F. Systematic review of scope and quality of electronic patient record data in primary care. BMJ. 2003;326:1070. doi: 10.1136/bmj.326.7398.1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ornstein SM, Nietert PJ, Jenkins RG, Litvin CB. The prevalence of chronic diseases and multimorbidity in primary care practice: a PPRNet report. J Am Board Fam Med. 2013;26(5):518–524. doi: 10.3122/jabfm.2013.05.130012. [DOI] [PubMed] [Google Scholar]
- 49.Harrison C, Britt H, Miller G, Henderson J. Examining different measures of multimorbidity, using a large prospective cross-sectional study in Australian general practice. BMJ Open. 2014;4:e004694. doi: 10.1136/bmjopen-2013-004694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Harrison C, Britt H, Miller G, Henderson J. Prevalence of chronic conditions in Australia. PLoS One. 2013;8(7):e67494. doi: 10.1371/journal.pone.0067494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Barnett K, Mercer SW, Norbury M, et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380(9836):37–43. doi: 10.1016/S0140-6736(12)60240-2. [DOI] [PubMed] [Google Scholar]
- 52.Britt HC, Harrison CM, Miller GC, Knox SA. Prevalence and patterns of multimorbidity in Australia. Med J Aust. 2008;189(2):72–77. doi: 10.5694/j.1326-5377.2008.tb01919.x. [DOI] [PubMed] [Google Scholar]
- 53.Uijen AA, van de Lisdonk EH. Multimorbidity in primary care: prevalence and trend over the last 20 years. Eur J Gen Pract. 2008;14(suppl 1):28–32. doi: 10.1080/13814780802436093. [DOI] [PubMed] [Google Scholar]
- 54.Fortin M, Hudon C, Dubois MF, et al. Comparative assessment of three different indices of multimorbidity for studies on health-related quality of life. Health Qual Life Outcomes. 2005;3:74. doi: 10.1186/1477-7525-3-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.van den Akker M, Buntinx F, Metsemakers JF, et al. Multimorbidity in general practice: prevalence, incidence and determinants of co-occurring chronic and recurrent diseases. J Clin Epidemiol. 1998;51(5):367–375. doi: 10.1016/s0895-4356(97)00306-5. [DOI] [PubMed] [Google Scholar]
- 56.Ryan BL, Bray Jenkyn K, Shariff SZ, et al. Beyond the grey tsunami: a cross-sectional population-based study of multimorbidity in Ontario. Can J Public Health. 2018;109(5–6):845–854. doi: 10.17269/s41997-018-0103-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Taylor AW, Price K, Gill TK, et al. Multimorbidity: not just an older person’s issue. Results from an Australian biomedical study. BMC Public Health. 2010;10:718. doi: 10.1186/1471-2458-10-718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.van den Bussche H, Schäfer I, Wiese B, et al. A comparative study demonstrated that prevalence figures on multimorbidity require cautious interpretation when drawn from a single database. J Clin Epidemiol. 2013;66(2):209–217. doi: 10.1016/j.jclinepi.2012.07.019. [DOI] [PubMed] [Google Scholar]
- 59.Catalá-López F, Alonso-Arroyo A, Page MJ, et al. Mapping of global scientific research in comorbidity and multimorbidity: a cross-sectional analysis. PLoS One. 2018;13(1):e0189091. doi: 10.1371/journal.pone.0189091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tetzlaff J, Epping J, Sperlich S, et al. Widening inequalities in multimorbidity? Time trends among the working population between 2005 and 2015 based on German health insurance data. Int J Equity Health. 2018;17(1):103. doi: 10.1186/s12939-018-0815-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tetzlaff J, Junius-Walker U, Muschik D, et al. Identifying time trends in multimorbidity: defining multimorbidity in times of changing diagnostic practices. Journal of Public Health. 2017;25(2):215–222. [Google Scholar]
- 62.van Oostrom SH, Gijsen R, Stirbu I, et al. Time trends in prevalence of chronic diseases and multimorbidity not only due to aging: data from general practices and health surveys. PLoS One. 2016;11(8):e0160264. doi: 10.1371/journal.pone.0160264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mounce LTA, Campbell JL, Henley WE, et al. Predicting incident multimorbidity. Ann Fam Med. 2018;16(4):322–329. doi: 10.1370/afm.2271. [DOI] [PMC free article] [PubMed] [Google Scholar]