Abstract
Purpose
Shoulder dislocation comprises 60% of all major joint dislocations worldwide and a number of reduction techniques are described in the literature with varying degrees of success. The description of a large number of techniques speaks for itself that no method is effective all the times and one should be acquainted with more than one technique. An ideal method of reduction should be simple, easily reproducible, relatively painless that can be performed unassisted without sedation or anaesthesia with minimal or no further complications. We report our results of using a novel method of anterior shoulder reduction described recently in the literature that claims to fulfil most of the characteristics of an ideal method if not all.
Methods
This prospective study was conducted in a tertiary care centre. All the cases of primary anterior shoulder dislocation presenting within three days of injury without any associated fracture or spine trauma with or without greater tuberosity fracture were included. The reduction was done using a novel method by orthopaedic residents in all cases. The need for a second reduction attempt or anaesthesia was considered a treatment failure. Time taken for reduction, pain felt during reduction and complications if any were noted.
Results
There were 47 (77.04%) males and 14 (22.95%) females with a mean age of (37.04 ± 12.63) years. The new technique was effective in locating a shoulder dislocation on the first attempt in 58 of the 61 dislocated shoulders (95.08%). The remaining three shoulders were reduced on second attempt by the same technique. Sedative, pre-medication or anaesthesia was not used in any case. The average time taken for the shoulder reduction was (130.5 ± 25.8) seconds and confidence interval (95%) 124–137 s. Iatrogenic complications were not seen in any of the patients.
Conclusion
This relatively painless technique of shoulder reduction is easy to acquire and practice in emergency department. The advantages of this manoeuvre and its associated safety may justly lead surgeons to select it as their primary method for reduction of anterior shoulder dislocations.
Keywords: Shoulder dislocation, External rotation manoeuvre, Prakash's manoeuvre
Introduction
Shoulder dislocation is the commonest joint dislocation seen in emergency trauma room worldwide comprising more than half of all dislocations with anterior dislocation being the commonest subvariety.1, 2, 3, 4, 5, 6, 7 A number of reduction techniques are in vogue with varying degree of results and reproducibility; however, most of these techniques require some sort of premedication, sedation or anaesthesia.6, 7, 8, 9 The choice of reduction manoeuvre depends upon the surgeon or treating physicians and the environment or place of work. However, in general a manoeuvre which is relatively painless, does not require sedation or anaesthesia, without the need of an assistant, with no or minimal complications that can be easily reproducible is preferred. We were using Kocher's reduction manoeuvre for reducing anterior shoulder dislocations in our institute in most of the cases and Spaso's manoeuvre in some. However, in June 2016 we came across a novel, relatively simple technique of shoulder reduction that was described and announced through a video on YouTube which was later published in a journal.10 The original author propagated it as a painless (relatively) method of reducing anterior shoulder dislocation which can be performed by a single surgeon without traction and need for sedation or anaesthesia.10 We conducted this prospective study with an intent to evaluate the results of this new method of shoulder reduction (Prakash's manoeuvre) in acute primary anterior dislocations of shoulder in the relatively inexperienced hands of orthopaedic residents.
Methods
This prospective single centre study was conducted in the department of orthopaedics in a tertiary care institute of northern India between January 2017 and June 2018. All the diagnosed patients of anterior shoulder dislocation were initially enrolled in the study. The demographic data including age, sex, laterality, history of previous dislocation, time since dislocation and associated fracture of greater tuberosity were noted in patient case sheet. We excluded the patients with a history of previous dislocation, associated or suspected spine injury, unconscious patients, those presenting later than a week since dislocation, fracture dislocations except for greater tuberosity fractures and hemodynamic unstable patients Consent was taken from all the patients after explaining the new procedure. A total of 87 patients with anterior shoulder dislocation were treated during the study period, out of which 61 patients met the inclusion criteria that constituted the study group. The results were analysed in terms of time to reduction, pain felt during the reduction manoeuvre as noted on visual analog scale and any iatrogenic complication. The reduction manoeuvre was done by orthopaedic residents in all the patients. A single attempt was allowed if more than one attempt or anaesthesia or sedative were needed that was considered as treatment failure.
Technique
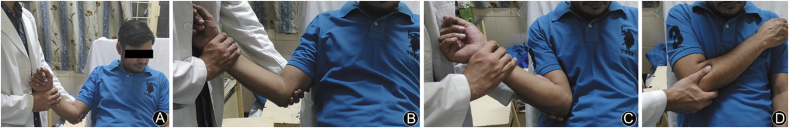
The patients are made to sit on a bed with back rest or on a chair with back rest or stand against a wall to fix the scapula. The surgeon holds the patients elbow with one hand and wrist with the other (Fig. 1A). No attempt is made to adduct or abduct the shoulder. Gradual and gentle external rotation of shoulder is done in the position of deformity until its parallel to coronal plane (Fig. 1B). This step is crucial and external rotation force is sustained for more than a minute and during this step try to engage the patient in some talk to reduce apprehension. After sustained external rotation the arm is gradually adducted until the elbow comes over the body then internally rotate the arm so that the hand touches the opposite shoulder. The shoulder reduces without any clunk or sound (Figs. 1C and 1D).
Fig. 1.
(A) Hold elbow with one hand and forearm with the other in the position of deformity without adducting or abducting. (B) Gently externally rotate the arm until it becomes near parallel to body, this position is maintained for a minute or so. (C) Gradually adduct the limb until the point of elbow comes over the body. (D) The arm is internally rotated so that the hand touches the opposite shoulder which confirms reduction.
Results
There were 47 (77.04%) males and 14 (22.95%) females with a mean age of (37.04 ± 12.63) years. The age varied between 18 and 62 years with a standard error of mean 1.61. The complete demographic profile of patients is presented in Table 1. The greater tuberosity was fractured in four patients and regimental badge sign was positive in two patients at presentation. We had observed a proclivity of right shoulder to dislocate (n = 37) compared with left, yielding a ratio of 1.54:1. The new technique (Prakash's Manoeuvre) was effective in locating a shoulder dislocation on the first attempt in 58 of the 61 dislocated shoulders (95.08%). The remaining three shoulders were reduced on second attempt by the same technique. Although we were able to reduce all shoulders, the patients requiring a second attempt (n = 3) were considered as treatment failures. There were no iatrogenic complications as a result of reduction manoeuvre as confirmed on clinical examination & radiographs (Fig. 2). The fractures of the greater tuberosity (n = 4) were found to be reduced to within acceptable limits post reduction (Fig. 3). The pain experienced during the reduction manoeuvre as noted on VAS scale ranged from 0 to 7 with a mean of 2.22 ± 1.25. Only one patient in our series had a pain score of seven on VAS. None of the patients in our series refused to continue the reduction procedure at any point. Linear regression analysis of time taken for reduction with age did not revealed any correlation. The average time taken for the shoulder reduction was 130.5 s with a range of 90–200 s. The standard deviation was 25.8 s and 95% confidence interval (CI) 124–137 s.
Table 1.
Demographic data of patients with primary anterior shoulder dislocation.
| Parameter | Number (percentage) |
|---|---|
| Gender | |
| Males | 47 (77.04) |
| Females | 14 (22.95) |
| Age (years) | |
| Mean | 37.04 ± 12.63 |
| Range | 18–62 |
| Standard error | 1.61 |
| Laterality | |
| Right | 37 (60.65) |
| Left | 24 (39.34) |
| Presentation | |
| Within 24 h | 56 (91.8) |
| 1–3 days | 05 (8.19) |
| Greater tuberosity fracture | 4 (6.55) |
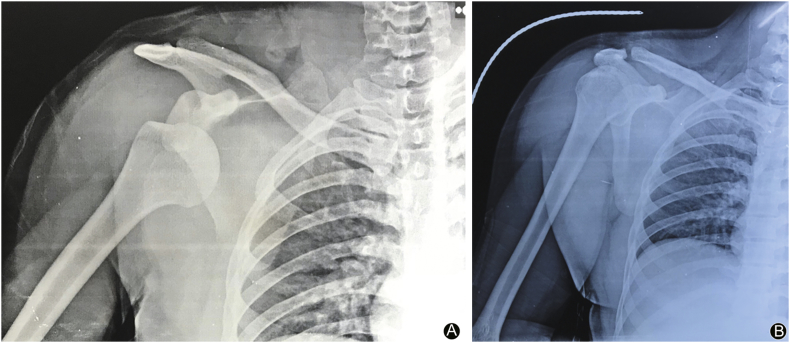
Fig. 2.
Pre-reduction radiograph (A) and post-reduction radiograph (B) of a patient with anterior shoulder dislocation, showing an uncomplicated reduction.
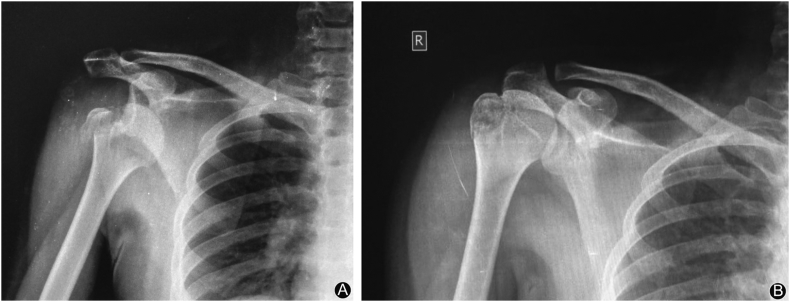
Fig. 3.
Pre-reduction (A) and post-reduction radiograph (B) of anterior shoulder dislocation with greater tuberosity fracture, showing greater tuberosity in acceptable reduction.
Discussion
Anterior shoulder dislocation being the commonest major joint dislocation is frequently seen in emergency trauma room.1, 2, 3, 4, 5, 6, 7, 8, 9, 10 The oldest known method for reduction was described by Hippocrates using traction & counter traction manoeuvres.11 Modern variations of these traction techniques are widely used today and most of these techniques if not all are performed using analgesia and/or sedation and most require an assistant. The complications associated with different traction methods using excessive traction were classified by Calvert et al.12 and included upper extremity dysfunction, amputations, and mortalities. The more severe iatrogenic injuries are rarely seen in clinical practice nowadays; however, neurovascular affliction is a recognized complication of contemporary traction techniques.13 We came across a novel method of shoulder reduction claimed to be painless that can be performed single handedly without sedation or anaesthesia. The original author published the results of 147 shoulder dislocations reduced by this new technique, over a period of eleven years, achieving a success rate of 100%.10 The exact mechanism of reduction is not fully understood. The original author believed shoulder dislocations to be rotational and translational injuries with little role of traction for reduction.10 However, since this manoeuvre is performed in sitting position, how much and what is the role of gravity is still not known. We believe it is a novel method and a broader acceptability will generate more interest in research which will further help in delineating the exact mechanism of reduction. The commonly performed shoulder reduction procedures are Kocher's, Spaso's vertical traction method, external rotation method of Leidlmeyer, Milch Manoeuvre, Eskimo & Stimson's and many more with varied effectiveness among different published series.14, 15, 16, 17, 18, 19, 20 A complete review of all the methods of shoulder reduction is beyond the scope of this research article. The choice of selection of a method depends upon such factors as its simplicity, reproducibility, need for sedation or anaesthesia, number of assistant required and time taken for reduction.8, 21 Irrespective of the technique used the rate of success for a first time anterior shoulder dislocation ranges from 70% to 90%.9, 21 Many a times more than one technique may be required in some cases, whereas 5%–10% of cases cannot be reduced in the emergency room.9, 21 Mirick et al.19 evaluated the external rotation method and reported it to be successful in 69 of 85 (81%) patients. They found traction-countertraction method to be most frequently effective when external rotation failed. In another study evaluating Spaso's technique successful reduction could be achieved in 87.5% of patients.22 Kuhn23 compared the best existing evidence regarding the treatment of patients with a primary anterior shoulder dislocation and reported that little data exist to ascertain the best method and that premedication with intra-articular lidocaine has fewer complications and needs a shorter time in the emergency room than intravenous sedation, with no obvious variances in success rates. The reported success rate of different reduction manoeuvres for anterior shoulder dislocation in the literature ranged from 70% to 100%.8, 17, 22, 24, 25, 26 However, most of these studies represented the results of experienced surgeons or physicians performing the reduction manoeuvre. There is paucity of data on success rate in the relatively inexperienced hands of junior residents. In a study depicting results of scapular manipulation technique, the residents were only able to reduce 63% cases. The success rate of 100% (95.08% on first attempt) in this series was analogous to other series performed by experienced orthopaedic surgeons and emergency physicians. There is a drawback of the procedure as well, since this manoeuvre is performed with the patient sitting or standing, it cannot be performed in unconscious, polytrauma and spine injury patients. The high success rate in this study reflects the simplicity and reproducibility of this procedure. Though the initial results of this technique seem promising, however, there is a need to conduct randomized controlled trial to prove its effectiveness compared with other manoeuvres & whether it can become the primary method of anterior shoulder reduction. The drawbacks of the study include a smaller sample size and no direct comparison with other techniques.
In conclusion, this relatively painless technique of shoulder reduction (Prakash's manoeuvre) is easy to acquire and practice in emergency department. The method is effective in achieving reduction of acute anterior shoulder dislocations (95.08%) on first attempt in the hands of orthopaedic residents. The advantages of this manoeuvre and its concomitant safety may justly lead surgeons to select it as their primary method for reduction of anterior shoulder dislocations. However, more studies are needed to see the results and reproducibility of this technique.
Funding
Nil.
Ethical statement
This study has been approved by the local ethical committee.
Conflicts of interest
No benefits in any form have been received or will be received from a commercial party-related directly or indirectly with regard to this article and there are no competing interests related to this article.
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.Ceroni D., Sadri H., Leuenberger A. Anteroinferior shoulder dislocation: an auto-reduction method without analgesia. J Orthop Trauma. 1997;11:399–404. doi: 10.1097/00005131-199708000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Villarin L.A., Jr., Belk K.E., Freid R. Emergency department evaluation and treatment of elbow and forearm injuries. Emerg Med Clin N Am. 1999;17:843–858. doi: 10.1016/s0733-8627(05)70100-0. [DOI] [PubMed] [Google Scholar]
- 3.Plummer D., Clinton J. The external rotation method for reduction of acute anterior shoulder dislocation. Emerg Med Clin N Am. 1989;7:165–175. [PubMed] [Google Scholar]
- 4.Blake R., Hoffman J. Emergency department evaluation and treatment of the shoulder and humerus. Emerg Med Clin N Am. 1999;17:859–876. doi: 10.1016/s0733-8627(05)70101-2. [DOI] [PubMed] [Google Scholar]
- 5.Hill J.A. Epidemiologic perspective on shoulder injuries. Clin Sports Med. 1983;2:241–247. [PubMed] [Google Scholar]
- 6.Westin C.D., Gill E.A., Noyes M.E. Anterior shoulder dislocation: a simple and rapid method for reduction. Am J Sports Med. 1995;23:369–371. doi: 10.1177/036354659502300322. [DOI] [PubMed] [Google Scholar]
- 7.Wen D.Y. Current concepts in the treatment of anterior shoulder dislocations. Am J Emerg Med. 1999;17:401–407. doi: 10.1016/s0735-6757(99)90097-9. [DOI] [PubMed] [Google Scholar]
- 8.Gleeson A.P. Anterior glenohumeral dislocation: what to do and how to do it. J Accid Emerg Med. 1998;15:7–12. doi: 10.1136/emj.15.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Riebel G.D., McCabe J.B. Anterior shoulder dislocation: a review of reduction techniques. Am J Emerg Med. 1991;9:180–188. doi: 10.1016/0735-6757(91)90187-o. [DOI] [PubMed] [Google Scholar]
- 10.Prakash L. A new method for reduction of shoulder dislocations. Ortho Surg Ortho Care Int J. 2018;1:1–5. [Google Scholar]
- 11.Brockbank W., Griffiths D.L. Orthopaedic surgery in the sixteenth and seventeenth centuries. J Bone Joint Surg Br. 1948;30:365–375. [PubMed] [Google Scholar]
- 12.Calvert J., LeRoy M., Lacroix L. Shoulder dislocations and vascular injuries. J Chir. 1942;58:337–346. [Google Scholar]
- 13.Waldron V.D., Hazel D. Tips of the trade #37. Technique for reduction of shoulder dislocation. Orthop Rev. 1991;10:563–566. [PubMed] [Google Scholar]
- 14.Janecki C.J., Shahcheragh G.H. The forward elevation maneuver for reduction of anterior dislocations of the shoulder. Clin Orthop Relat Res. 1982;164:177–180. [PubMed] [Google Scholar]
- 15.Johnson G., Hulse W., McGowan A. The Milch technique for reduction of anterior shoulder dislocations in an accident and emergency department. Arch Emerg Med. 1992;9:40–43. doi: 10.1136/emj.9.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Russell J.A., Holmes E.M., Keller D.J. Reduction of acute anterior shoulder dislocations using the Milch technique: a study of ski injuries. J Trauma. 1981;21:802–804. doi: 10.1097/00005373-198109000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Beattie T.F., Steedman D.J., McGowan A. A comparison of the Milch and Kocher techniques for acute anterior dislocation of the shoulder. Injury. 1986;17:349–352. doi: 10.1016/0020-1383(86)90161-0. [DOI] [PubMed] [Google Scholar]
- 18.Milch H. Treatment of dislocation of the shoulder. Surgery. 1938;3:732–740. [Google Scholar]
- 19.Mirick M.J., Clinton J.E., Ruiz E. External rotation method of shoulder dislocation reduction. JACEP. 1979;8:528–531. doi: 10.1016/s0361-1124(79)80302-0. [DOI] [PubMed] [Google Scholar]
- 20.Leidelmeyer R. Reduced a shoulder subtly and painlessly. Emerg Med. 1977;9:223–234. [Google Scholar]
- 21.Manes H.R. A new method of shoulder reduction in the elderly. Clin Orthop Relat Res. 1980;147:200–202. [PubMed] [Google Scholar]
- 22.Yuen M.C., Tung W.K. Reducing anterior shoulder dislocation by the Spaso technique. Hong Kong J Emerg Med. 2001;8:96–100. doi: 10.1136/emj.18.5.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kuhn J.E. Treating the initial anterior shoulder dislocation an evidence-based medicine approach. Sports Med Arthrosc Rev. 2006;14:192–198. doi: 10.1097/01.jsa.0000212328.25345.de. [DOI] [PubMed] [Google Scholar]
- 24.Uehara D.T., Rudzinski J.P. Injuries to the shoulder complex and humerus. In: Tintinalli J.E., Kelen D.G., Stapczynski J.S., editors. Emergency Medicine: A Comprehensive Study Guide. fifth ed. Mcgraw-Hill; New York: 2000. pp. 1783–1791. [Google Scholar]
- 25.Connolly . second ed. W.B. Saunders Co; Philadelphia, Pa: 1981. Management of fractures and Dislocations: An Atlas. [Google Scholar]
- 26.Kocher T. A new reduction method for shoulder dislocations. Berlin Klin Wochnschr. 1870;7:101–106. [Google Scholar]