Abstract
Introduction
The aim of this study was to investigate the urodynamic effects of intravesical administration of bovine adrenal medulla 8-22 (BAM8-22), a selective rat sensory neuron-specific receptor 1 agonist, on the micturition reflex in normal rats and rats with cyclophosphamide-induced bladder overactivity.
Material and methods
Continuous cystometrograms (0.04 ml/min) were performed in urethane-anesthetized rats. After stable micturition cycles were established, vehicle (saline) or BAM8-22 was instilled intravesically and changes in bladder activity were monitored. The experiments using BAM8-22 were also performed in capsaicin-pretreated rats. In another experiment, vehicle (saline) or BAM8-22 was instilled intravesically and changes in bladder activity were monitored in cyclophosphamide-treated rats. Continuous cystometrograms were performed 48 hours after cyclophosphamide injection. Cystometric parameters were recorded and compared before and after intravesical drug administration.
Results
Intravesical administration of BAM8-22 significantly increased the intercontraction interval and threshold pressure in urethane-anesthetized rats, but did not affect the basal pressure or maximum pressure at any doses tested. The inhibitory effects of intravesical administration of BAM8-22 were not inhibited by capsaicin pretreatment. Intravesical administration of BAM8-22 also significantly increased intercontraction interval in the cyclophosphamide-treated rats.
Conclusions
The current results indicate that intravesical administration of a selective rat sensory neuron-specific receptor 1 agonist can inhibit the micturition reflex and can ameliorate cyclophosphamide-induced bladder overactivity in rats.
Keywords: cyclophosphamide, cystometry, rats, sensory neuron-specific receptor
INTRODUCTION
Afferent pathways innervating the urinary bladder arise in the lumbosacral dorsal root ganglia and are carried in two sets of nerves; pelvic and hypogastric nerves [1]. Afferent fibers passing in the pelvic nerve and via L6 and S1 dorsal root ganglia to the spinal cord are responsible for initiating the micturition reflex [2]. Afferent pathways innervating the bladder consist of myelinated Aδ- and unmyelinated C-fibers [1]. In normal rats, conscious voiding is dependent on Aδ-fiber bladder afferents even though both Aδ-fiber and C-fiber bladder afferents are mechanoceptive; whereas C-fiber afferents are responsible for bladder nociceptive responses [3]. Previous studies have suggested that the hyperexcitability of C-fiber bladder afferents, which are silent under normal conditions, is involved in the emergence of overactive bladder and bladder pain in various pathological conditions, such as spinal cord injury, bladder outlet obstruction, or interstitial cystitis [4]. Thus, it has been postulated that targeting afferent hyperexcitability could be effective for treating detrusor overactivity and pain symptoms [4].
A family of G-protein-coupled receptors has been identified in the rat dorsal root ganglia (DRG) and named as sensory neuron-specific receptors (SNSRs) [5]. These receptors are expressed exclusively in a subset of small-diameter sensory neurons in the DRG and trigeminal ganglia. Based on several analyses, this family of receptors is comprised of four to six members in the human (MrgX1-4 or SNSR1-6) and 32 receptors in mouse are classified into three major subfamilies Mrg A, B, and C [5−8]. Initially, only one SNSR gene was identified in the rat [5]. Recently, it has been demonstrated that more than one rat SNSR/Mrg subtype exists [9]. These receptors have been subclassified in a similar scheme as described for human and mouse, rat Mrg A, B, C, and D. For the sake of simplicity, we refer to rat SNSR/rat MrgC as rat SNSR1 in this study, which corresponds to the first gene described in small DRG neurons [5]. It appears that rat SNSR1 is pronociceptive as intrathecal (i.t.) and intradermal administration of its agonists, bovine adrenal medulla 8-22 (BAM8-22) and (Tyr6)-γ2-MSH-6-12, enhance acute nociception [10]. In contrast, it was reported that the activation of rat SNSR1 produces analgesia in the persistent pain model [11].
Recent studies demonstrated that activation of SNSRs can inhibit the micturition reflex via suppression of bladder afferent pathways in urethane-anesthetized normal rats [12]. However, it is unknown whether SNSR1 receptor activation in the bladder can locally affect the micturition reflex in normal rats and rats with various pathological conditions in the lower urinary tract, such as overactive bladder or interstitial cystitis/bladder pain syndrome. Therefore, this study was performed to elucidate the urodynamic effects of intravesical administration of a SNSR1 agonist on the micturition reflex in urethane-anesthetized rats and rats with cyclophosphamide (CYP)-induced bladder overactivity.
MATERIAL AND METHODS
Animals
Adult female Sprague-Dawley rats weighing 230 to 250 g were used. The rats were maintained under standard laboratory conditions with a 12-h light/12-h dark cycle and free access to food pellets and tap water. All animal care and experimental procedures were conducted in accordance with the institutional guide for the care and use of laboratory animals, and the protocols were approved by the Institutional Animal Care and Use Committee. Every effort was made to minimize animal suffering and pain.
Drugs
A selective rat SNSR1 agonist, BAM8-22 (Tocris Bioscience, Ellisville, MO), was used. For intravesical administration BAM8-22 was dissolved in saline (0.9% NaCl).
Intravesical administration of BAM8-22 in normal rats
Rats were anesthetized with 2% isoflurane followed by urethane (1.2 g/kg subcutaneously) (Sigma Chemical Co., St. Louis, MO). A midline abdominal incision was made, and a transvesical catheter (Clay-Adams, Parsippany, New Jersey, PE-60) with a fire-flared tip was inserted into the dome of the bladder and secured with silk thread for bladder filling and pressure recording. A 3-way stopcock was connected to the transvesical catheter to monitor the bladder pressure. After transvesical catheter insertion, saline at a room temperature was continuously infused into the bladder for 2 hours at a rate of 0.04 ml per minute to record cystometrograms during a control period. The PowerLab (ADInstruments Pty, Ltd., Castle Hill, New South Wales, Australia) was used for data acquisition and manipulation. After baseline cystometry, vehicle (saline) or BAM8-22 (100, 300, and 1000 nM, n = 6 per dose) was instilled intravesically and changes in the bladder activity were monitored. The experiments using BAM8-22 (1000 nM) were also performed in rats pretreated with systemic capsaicin (Sigma Chemical Co., St. Louis, Missouri) (n = 6) to determine whether the effect of BAM8-22 was mediated by capsaicin sensitive C-fiber afferent pathways. Capsaicin was administered to rats in a solution (20 mg/ml) given subcutaneously in divided doses on 2 consecutive days: 25 and 50 mg/kg on the first day and 50 mg/kg on the second day. Four days after the first administration of capsaicin, cystometry was performed. To evaluate the effectiveness of capsaicin pretreatment, an eye wipe test was performed. The intercontraction interval (ICI), maximum pressure (MP), threshold pressure (TP), basal pressure (BP) were measured before and after drug administration.
Intravesical administration of BAM8-22 in CYP-treated rats
Rats were anesthetized with isoflurane (2%) and received intraperitoneal injections of CYP (Sigma Chemical Co., St. Louis, MO) to produce urinary bladder inflammation. Experimental and control rats were injected with CYP (200 mg/kg, intraperitoneally) or a corresponding volume of saline, respectively. Continuous cystometrograms were performed 48 hours after CYP or saline injection. CYP-treated and control rats were anesthetized with isoflurane followed by urethane (1.2 g/kg subcutaneously). Thereafter, the abdomen was opened through a midline incision, and a transvesical catheter (PE-60 polyethylene catheter) with a fire-flared tip was inserted into the dome of the bladder and secured with silk thread for bladder filling and pressure recording. A 3-way stopcock was connected to the transvesical catheter to monitor the bladder pressure. After transvesical catheter insertion, saline at a room temperature was continuously infused into the bladder for 2 hours at a rate of 0.04 ml per minute to record cystometrograms during a control period. After baseline cystometry, vehicle (saline) or BAM8-22 (300, 1000, and 3000 nM, n = 6 per dose) was instilled intravesically and changes in bladder activity were monitored. ICI, MP, TP and BP were measured before and after drug administration.
Statistical analysis
All data values are expressed as the mean ±standard deviation. In experiments with intravesical administration of BAM8-22, ICI, MP, TP, BP values during 30 minutes before and after drug administration were averaged in each rat and then the averages in a group of animals were combined. A one-way ANOVA followed by Dunnett's multiple comparison test was used for the statistical analysis between the vehicle and drug-treated groups. Student's paired t-test was used to compare cystometric variables before and after treatment. Student's unpaired t-test was used to evaluate differences in cystometric variables between normal and CYP-treated rats. Statistical analyses were conducted by using SPSS 13.0 (SPSS Inc., Chicago, IL) and GraphPad Prism software (GraphPad Software, Inc., San Diego, CA). For all statistical tests, p <0.05 was considered significant.
RESULTS
Intravesical administration of BAM8-22 in normal rats
As shown in Figure 1A, intravesical administration of BAM8-22 inhibited the micturition reflex as evidenced by increases in ICI and TP. Intravesical administration of BAM8-22 at 100, 300, and 1000 nM, (n = 6 per dose) significantly increased ICI at doses of 300 nM or higher (101.2 ±4.8%, 115.5 ±8.7%, and 119.4 ±10.5% of the control value, respectively) (Table 1). Intravesical administration of BAM8-22 at 100, 300 and 1000 nM also increased PT at doses of 300 nM or higher (5.83 ±1.35 cmH2O, 8.85 ±2.16 cmH2O, and 8.96 ±2.74 cmH2O, respectively, from the control value of 5.28 ±1.61 cmH2O) (Table 1). However, there were no significant changes in BP or MP at any doses tested (Table 1). Intravesical administration of vehicle (saline) had no effect on the ICI, TP, BP, or MP (Table 1). The inhibitory effect of intravesical administered BAM8-22 (1000 nM, n = 6) still occurred after capsaicin pretreatment (Figure 1B). Intravesical administration of BAM8-22 in capsaicin-pretreated rats increased ICI with a similar efficacy as in normal rats, and increased TP significantly (Table 1). There was no significant change in BP or MP. No responses were observed in the eye wiping test with capsaicin in these animals (Table 1).
Figure 1.
Representative cystometrograms showing the effects of intravesical administration of BAM8-22 (1000 nM) on bladder activity in normal rats. B. Representative cystometrograms showing the effects of intravesical administration of BAM8-22 (1000 nM) on bladder activity in capsaicin-pretreated rats.
Table 1.
Changes in cystometric parameters after intravesical BAM8-22 administration in normal rats
| Variable | Vehicle | BAM8-22 (100 nM) | BAM8-22 (300 nM) | BAM8-22 (1000 nM) | Capsaicin Pretreatment |
|---|---|---|---|---|---|
| BAM8-22 (1000 nM) | |||||
| Number of rats | 6 | 6 | 6 | 6 | 6 |
| Mean ±SD | |||||
| ICI, mins before after |
11.6 ±3.45 11.8 ±4.56 |
10.5 ±3.18 10.6 ±2.85 |
10.2 ±5.73 11.7 ±6.56* |
10.8 ±4.67 12.8 ±7.67* |
10.4 ±2.62 12.5 ±6.78* |
| %ICI, % | 102.6 ±5.1 | 101.2 ±4.8 | 115.5 ±8.7† | 119.4 ±10.5† | 123.5 ±12.6† |
| BP, cmH2O before after |
4.67 ±1.56 4.59 ±0.92 |
3.78 ±1.23 3.82 ±1.37 |
3.67 ±1.52 3.78 ±1.38 |
4.26 ±2.18 4.29 ±1.92 |
4.01 ±0.86 3.98 ±0.67 |
| TP, cmH2O before after |
5.35 ±1.78 5.28 ±1.61 |
5.48 ±1.28 5.83 ±1.35 |
5.05 ±1.23 8.85 ±2.16* |
5.81 ±1.56 8.96 ±2.74* |
7.02 ±3.27 11.6 ±6.78* |
| MP, cmH2O before after |
25.1 ±3.95 25.0 ±4.19 |
26.1 ±3.28 28.5 ±4.78 |
25.9 ±3.28 28.1 ±5.18 |
26.3 ±4.27 27.8 ±4.86 |
26.5 ±4.78 29.0 ±8.46 |
p <0.01 (paired t-test);
p <0.01 vs. vehicle injection (Dunnett’s multiple comparison test)
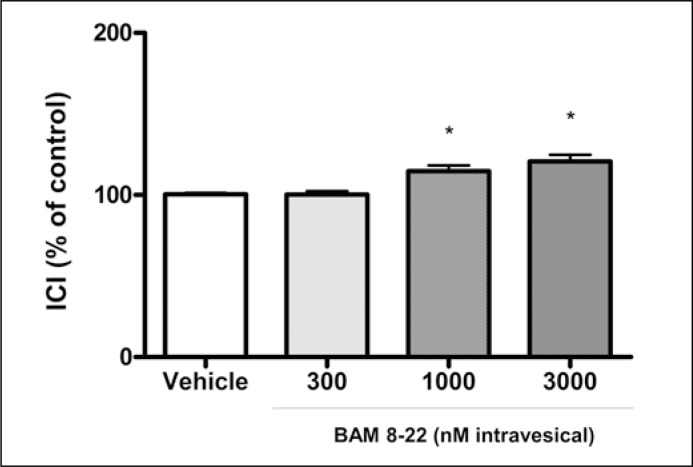
Intravesical administration of BAM8-22 in CYP-treated rats
CYP treatment induced a higher BP and a shorter ICI compared with the control group (Table 2). As shown in Figure 2 and 3, intravesical administration of BAM8-22 inhibited the micturition reflex as evidenced by increases in ICI. Intravesical administration of BAM8-22 at 300, 1000, and 3000 nM (n = 6 per dose) significantly increased ICI at doses of 1000 and 3000 nM to 115.6 ±7.2%, and 120.5 ±7.6% of the control value, respectively (p <0.05) in CYP-treated rats (Table 2). However, intravesical administration of BAM8-22 did not change BP or MP at any doses tested in the CYP-treated rats (Table 2). Intravesical administration of vehicle (saline) had no effects on the ICI, TP, BP, or MP (Table 2).
Table 2.
Changes in cystometric parameters after intravesical BAM8-22 administration in CYP cyclophosphamide-treated or control rats
| Variable | CYP-treated rats | Control rats | |||
|---|---|---|---|---|---|
| Vehicle | BAM8-22 (300 nM) | BAM8-22 (1000 nM) | BAM8-22 (3000 nM) | Vehicle | |
| Number of rats | 6 | 6 | 6 | 6 | 6 |
| Mean ±SD | |||||
| ICI, mins before after |
3.21 ±0.81 3.25 ±0.75 |
3.06 ±0.67 3.25 ±0.98 |
3.57 ±1.24 4.16 ±1.01* |
3.07 ±0.98 3.71 ±1.16* |
11.8 ±4.58 11.9 ±5.21 |
| %ICI, % | 101.6 ±4.7 | 98.6 ±5.8 | 115.6 ±7.2† | 120.5 ±7.6† | 100.6 ±8.1 |
| BP, cmH2O before after |
9.67 ±3.56 9.59 ±4.05 |
8.96 ±3.21 9.14 ±2.78 |
9.56 ±4.51 9.41 ±3.78 |
10.2 ±4.37 9.95 ±3.95 |
4.38 ±1.12 4.19 ±0.98 |
| TP, cmH2O before after |
13.7 ±6.89 13.5 ±7.51 |
14.7 ±6.19 15.1 ±5.78 |
15.7 ±4.89 16.5 ±6.81 |
14.4 ±5.99 15.7 ±8.17 |
7.67 ±4.38 7.55 ±3.78 |
| MP, cmH2O before after |
43.6 ±9.56 41.9 ±8.78 |
40.6 ±7.81 41.8 ±9.16 |
43.7 ±11.7 45.1 ±10.6 |
38.7 ±8.78 37.5 ±9.18 |
32.8 ±6.39 31.8 ±7.61 |
p <0.05 (paired t-test);
p <0.05 vs. vehicle injection (Dunnett’s multiple comparison test)
Figure 2.
Representative cystometrograms showing the effects of intravesical administration of BAM8-22 (3000 nM) on bladder activity in cyclophosphamide-treated rats.
Figure 3.
Changes in the intercontraction interval (ICI) (% of control [Pre]) after intravesical administration of vehicle or BAM8-22 in cyclophosphamide-treated rats. Histograms represent mean ± standard deviation values.
*<0.01 vs. vehicle administration
DISCUSSION
The goal of this study was to assess the effects of intravesical administration of a SNSR1 agonist on the micturition reflex in urethane-anesthetized normal rats and rats with cyclophosphamide (CYP)-induced bladder overactivity. Our findings indicate that in urethane-anesthetized rats, local activation of SNSRs by intravesically administered SNSR1 agonist has an inhibitory effect on the micturition reflex, as shown by the significant increases in ICI and TP.
BAM8-22 is a synthesized peptide with 15 amino acids. It differs from bovine adrenal medulla 22 (BAM22), an opioid peptide with 22 amino acids and one of the natural cleavage products of proenkephalin A [13], in that BAM8-22 does not contain the N-terminal YGGFM motif of BAM22 [5]. It has also been demonstrated that in vitro BAM8-22 does not interact directly with the opioid receptor [5]. Furthermore, it has been demonstrated that the effect of BAM8-22 on nociception was not mediated by opioid receptors since this peptide displayed identical efficacy in inhibiting the nocifensive behaviors in the absence or presence of naloxone, a non-selective opioid receptor antagonist [11]. In addition, endogenous BAM8-22 has not been found to exist up to date although BAM22, an opioid peptide, is widely distributed in the central nervous system [14, 15]. Therefore, it seems reasonable to assume that the inhibitory effects of BAM8-22 on normal bladder activity were mediated by activation of SNSR1. BAM8-22 induces inhibition of high voltage-activated Ca2+ current in rat DRG and superior cervical ganglion neurons [16], which may lead to inhibition of excitatory neurotransmitter release at synapses formed between small-diameter DRG neurons and the spinal dorsal horn neurons [17]. These events may underline the results obtained in the present study. If this is true, SNSRs could be categorized as the type of receptors that are expressed in the small-sized neurons in the DRG and function to negatively modulate excitability of the central terminals of primary afferents, similar to opioid [18], acetylcholine [19], and GABA receptors [20].
The current study also indicated that the activation of SNSR1 can inhibit the micturition reflex via capsaicin-resistant afferents pathways. In the present study, ICI and TP in capsaicin-pretreated rats were significantly increased compared to normal rats, as reported in previous studies using anesthetized rats with afferent desensitization induced by pretreatment with capsaicin, a C-fiber neurotoxin [21]. The inhibitory effects of intravesical administration of BAM8-22 were still observed after capsaicin pretreatment. A study using in situ hybridization (ISH) analysis, rat SNSR mRNA was detected in a subset of small neurons within the trigeminal ganglia and DRG, but not in the sympathetic superior cervical ganglion or in the nodose ganglion, indicating SNSR is uniquely associated with sensory afferents in the rat [5]. Moreover, in RT-PCR analyses of 25 different human tissues using oligonucleotides designed to conserved regions of SNSR 1-6, SNSR mRNA expression was detected exclusively in human DRG [5]. Lembo et al. [5] used double-labeling studies combining ISH with the immunohistochemical detection of neuronal markers such as substance P, calcitonin gene-related peptide (CGRP), vanilloid receptor (TRPV1), isolectin B4 (IB4) on rat DRG tissue sections to identify the neuronal phenotype of SNSR-expressing cells. Most SNSR-positive neurons were found in the non-peptidergic, IB4-positive population. Also, a half of them were not co-localized with TRPV1 capsaicin receptor. Therefore, it is possible that the effects of BAM8-22 are mediated by capsaicin-resistant C-fiber afferents that do not express TRPV1.
The current study also indicates that activation of SNSR1 by intravesical BAM8-22 can improve CYP-induced bladder overactivity, which is induced by activation of capsaicin sensitive C-fiber afferent pathways because capsaicin pretreatment significantly reduces CYP-induced bladder overactivity in rats [22]. Thus, the main function of BAM8-22 in CYP treated rats seems to be mediated by modulation of afferent activity, rather than efferent or smooth muscle activity, because BAM8-22 induced increases in ICI without affecting MP or BP. On the other hand, our current study demonstrated that the inhibitory effects of intravesical administration of BAM8-22 on ICI and TP were still observed in rats with C-fiber afferent desensitization induced by pretreatment with capsaicin, a C-fiber neurotoxin, suggesting that the activation of SNSR1 by intravesical BAM8-22 can inhibit the micturition reflex via the pathways of capsaicin-resistant C-fiber afferents in normal rats. However, the effects of activation of SNSR1 by intravesical BAM8-22 could involve the suppression of capsaicin sensitive C-fiber afferents in addition to capsaicin-insensitive ones in CYP-treated rats.
Many receptors that can modulate micturition are also distributed in the neuronal pathways that regulate other functions, such as respiration and brain activity, etc. Targeting this type of receptors concurrently results in modulating the micturition reflex and producing unwanted effects. For example, opioids have been used clinically as effective analgesics for many pain conditions, but their use is limited by their considerable central nervous system-mediated adverse events. To date, it has been found that SNSRs are exclusively expressed in a subset of sensory neurons in the DRG and the trigeminal ganglion [5, 10]. Intravesical therapy/drug delivery is widely used for treatment of bladder dysfunctions such as overactive bladder and painful bladder syndrome/interstitial cystitis as well as prevention of the recurrence of superficial bladder cancer after transurethral resection of bladder tumor [23]. Instillation of drugs through a catheter into the bladder provides a high concentration of drugs locally at the disease site in the bladder without an increase in systemic levels, which can explain the low risk of systemic adverse events [23]. Thus, it is assumed that intravesical administration of SNSR agonists could be effective for the pharmacological treatment of bladder dysfunction with less adverse events.
CONCLUSIONS
The results of the present study have shown that sensory neuron-specific receptors (SNSRs) play an important role in the local modulation of bladder afferent activity in normal rats and activation of SNSRs can ameliorate cyclophosphamide (CYP)-induced bladder overactivity in rats. Thus, SNSRs could be an effective target for the treatment of bladder dysfunctions such as overactive bladder and painful bladder syndrome/interstitial cystitis, for which C-fiber afferent hyperexcitability has been proposed to be an important pathophysiological basis.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
References
- 1.de Groat WC. Anatomy and physiology of the lower urinary tract. Urol Clin North Am. 1993;20:383–401. [PubMed] [Google Scholar]
- 2.Vera PL, Nadelhaft I. Afferent and sympathetic innervation of the dome and the base of the urinary bladder of the female rat. Brain Res Bull. 1992;29:651–658. doi: 10.1016/0361-9230(92)90134-j. [DOI] [PubMed] [Google Scholar]
- 3.Maggi CA, Conte B. Effect of urethane anesthesia on the micturition reflex in capsaicin-treated rats. J Auton Nerv Syst. 1990;30:247–251. doi: 10.1016/0165-1838(90)90256-i. [DOI] [PubMed] [Google Scholar]
- 4.Yoshimura N, Chancellor MB. Current and future pharmacological treatment for overactive bladder. J Urol. 2002;168:1897–1913. doi: 10.1016/S0022-5347(05)64261-9. [DOI] [PubMed] [Google Scholar]
- 5.Lembo PM, Grazzini E, Groblewski T, et al. Proenkephalin A gene products activate a new family of sensory neuron - specific GPCRs. Nat Neurosci. 2002;5:201–209. doi: 10.1038/nn815. [DOI] [PubMed] [Google Scholar]
- 6.Dong X, Han SK, Zylka MJ, Simon MI, Anderson DJ. A diverse family of GPCRs expressed in specific subsets of nociceptive sensory neurons. Cell. 2001;106:619–632. doi: 10.1016/s0092-8674(01)00483-4. [DOI] [PubMed] [Google Scholar]
- 7.Bender E, Buist A, Jurzak M, et al. Characterization of an orphan G protein-coupled receptor localized in the dorsal root ganglia reveals adenine as a signaling molecule. Proc Natl Acad Sci USA. 2002;99:8573–8578. doi: 10.1073/pnas.122016499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Han SK, Dong X, Hwang JI, Zylka MJ, Anderson DJ, Simon MI. Orphan G protein-coupled receptors MrgA1 and MrgC11 are distinctively activated by RF-amide-related peptides through the Galpha q/11 pathway. Proc Natl Acad Sci USA. 2002;99:14740–14745. doi: 10.1073/pnas.192565799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zylka MJ, Dong X, Southwell AL, Anderson DJ. Atypical expansion in mice of the sensory neuron-specific Mrg G protein-coupled receptor family. Proc Natl Acad Sci USA. 2003;100:10043–10048. doi: 10.1073/pnas.1732949100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grazzini E, Puma C, Roy MO, et al. Sensory neuron-specific receptor activation elicits central and peripheral nociceptive effects in rats. Proc Natl Acad Sci USA. 2004;101:7175–7180. doi: 10.1073/pnas.0307185101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen T, Cai Q, Hong Y. Intrathecal sensory neuron-specific receptor agonists bovine adrenal medulla 8-22 and (Tyr6)-gamma2-MSH-6-12 inhibit formalin-evoked nociception and neuronal Fos-like immunoreactivity in the spinal cord of the rat. Neuroscience. 2006;141:965–975. doi: 10.1016/j.neuroscience.2006.04.011. [DOI] [PubMed] [Google Scholar]
- 12.Honda M, Takenaka A, Inoue S, Chancellor MB, Yoshimura N. Sensory neurone-specific receptor-mediated regulation of micturition reflex in urethane-anaesthetized rats. BJU Int. 2011;109:628–633. doi: 10.1111/j.1464-410X.2011.10400.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dores RM, Mcdonald LK, Steveson TC, Sei CA. The molecular evolution of neuropeptides: prospects for the '90s. Brain Behav Evol. 1990;36:80–99. doi: 10.1159/000115300. [DOI] [PubMed] [Google Scholar]
- 14.Khachaturian H, Lewis ME, Watson SJ. Colocalization of proenkephalin peptides in rat brain neurons. Brain Res. 1983;279:369–373. doi: 10.1016/0006-8993(83)90212-3. [DOI] [PubMed] [Google Scholar]
- 15.Pittius CW, Seizinger BR, Pasi A, Mehraein P, Herz A. Distribution and characterization of opioid peptides derived from proenkephalin A in human and rat central nervous system. Brain Res. 1984;304:127–136. doi: 10.1016/0006-8993(84)90868-0. [DOI] [PubMed] [Google Scholar]
- 16.Chen H, Ikeda SR. Modulation of ion channels and synaptic transmission by a human sensory neuron-specific G-protein-coupled receptor, SNSR4/mrgX1, heterologously expressed in cultured rat neurons. J Neurosci. 2004;24:5044–5053. doi: 10.1523/JNEUROSCI.0990-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bao J, Li JJ, Perl ER. Differences in Ca2+ channels governing generation of miniature and evoked excitatory synaptic currents in spinal laminae I and II. J Neurosci. 1998;18:8740–8750. doi: 10.1523/JNEUROSCI.18-21-08740.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Beland B, Fitzgerald M. Mu- and delta-opioid receptors are downregulated in the largest diameter primary sensory neurons during postnatal development in rats. Pain. 2001;90:143–150. doi: 10.1016/s0304-3959(00)00397-3. [DOI] [PubMed] [Google Scholar]
- 19.Genzen JR, Van Cleve W, McGehee DS. Dorsal root ganglion neurons express multiple nicotinic acetylcholine receptor subtypes. J Neurophysiol. 2001;86:1773–1782. doi: 10.1152/jn.2001.86.4.1773. [DOI] [PubMed] [Google Scholar]
- 20.Stoyanova I, Dandov A, Lazarov N, Chouchkov C. GABA- and glutamate-immunoreactivity in sensory ganglia of cat: a quantitative analysis. Arch Physiol Biochem. 1998;106:362–369. doi: 10.1076/apab.106.5.362.4360. [DOI] [PubMed] [Google Scholar]
- 21.Maggi CA, Santicioli P, Giuliani S, Furio M, Meli A. The capsaicin-sensitive innervation of the rat urinary bladder: further studies on mechanisms regulating micturition threshold. J Urol. 1986;136:696–700. doi: 10.1016/s0022-5347(17)45030-0. [DOI] [PubMed] [Google Scholar]
- 22.Saitoh C, Yokoyama H, Chancellor MB, de Groat WC, Yoshimura N. Comparison of voiding function and nociceptive behavior in two rat models of cystitis induced by cyclophosphamide or acetone. Neurourol Urodyn. 2010;29:501–505. doi: 10.1002/nau.20777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hsu CC, Chuang YC, Chancellor MB. Intravesical drug delivery for dysfunctional bladder. Int J Urol. 2013;20:552–562. doi: 10.1111/iju.12085. [DOI] [PubMed] [Google Scholar]