Abstract
Background:
Patients with anterior cruciate ligament (ACL)–deficient knees risk recurrent instability of the affected knee, which may predispose to meniscal injuries. Various studies have correlated the incidence of meniscal tear with elapsed time from ACL tear and number of instability events. However, it is not clear how significant an instability event needs to be to contribute to a meniscal tear.
Purpose/Hypothesis:
The purpose of this study was to (1) define a significant instability episode and (2) develop a checklist and scoring system for predicting meniscal tears based on significant instability episode. We hypothesized that patients with ACL-deficient knees who met the scoring threshold for a significant instability episode would have a higher incidence of meniscal tears compared with those who did not meet the threshold.
Study Design:
Cohort study (prognosis); Level of evidence, 2.
Methods:
This retrospective study included patients with magnetic resonance imaging (MRI)–confirmed isolated ACL tear for longer than 3 months. We determined parameters for assessing instability episodes and defined any instability events between the MRI and ACL reconstruction as significant or insignificant. Patients were then grouped into a significant instability group (≥1 significant episode) and an insignificant instability group, and the incidence and types of meniscal tears found during surgery were compared between groups.
Results:
There were 108 study patients: 62 in the significant instability group and 46 in the insignificant instability group. During surgery, 58 meniscal tears (46 medial, 12 lateral) were recorded, for an overall meniscal injury rate of 53.70%. In the significant instability group, 47 patients (75.81%) had a meniscal tear and 15 (24.19%) had intact menisci (P < .001). In the insignificant instability group, 11 patients (23.91%) had a meniscal tear and 35 (76.08%) had intact menisci (P < .001). Regarding the 58 patients with a meniscal tear, 47 (81.03%) had ≥1 significant episode of instability before surgery, as compared with 11 (18.97%) who had insignificant or no instability. The odds of having a medial meniscal tear at ACL reconstruction was 10 times higher in the significant instability group versus the insignificant instability group.
Conclusion:
The incidence of a medial meniscal tear was 10 times greater in patients with a significant episode of instability versus those with insignificant instability, as defined using a predictive scoring system. The incidence of lateral meniscal tear did not change with instability episodes.
Keywords: meniscal tear, anterior cruciate ligament deficiency, instability, predictive scoring system
Anterior cruciate ligament (ACL) reconstruction (ACLR) is one of the most commonly performed ligament reconstructions worldwide.4,14 The outcomes of ACLR are generally good, but poorer outcomes have been associated with concurrent meniscal injuries.6,7,18,23,24 Several studies have mentioned that the incidence of meniscal injuries is significantly higher if surgery is delayed beyond 6 to 12 months postinjury.1,3,5,11
Although instability is a frequent complaint following ACL deficiency, no study has defined the term instability. The number of instability episodes was described as a predictive factor for meniscal injury by Kluczynski et al,13 however, their study also did not define instability. We believe that predictive factors for meniscal injury should not be limited to (1) time duration from ACL deficiency to definitive surgery and (2) number of instability episodes. We also believe that if a meniscal tear did not occur during the index injury that caused the ACL tear, then a significant episode of instability after the index injury, rather than the number of instability episodes, has to be the cause of meniscal tear in patients with ACL deficiency.
In this study, we sought to define the characteristics of a significant episode of instability and use the definition to develop a scoring system for predicting meniscal tears in ACL-deficient knees. On the basis of the proposed Predictive Scoring System for Significant Instability (PSSSI), we hypothesized that the incidence of meniscal injury in patients who had a significant episode of instability after index injury is higher compared with those who had no significant episode of instability. The secondary aim of this study was to identify the incidence of meniscal tear in different age groups.
Methods
Ethical approval for this study was obtained from an institutional review committee. This was a retrospective case series of patients seen between September 2014 and September 2016 at a tertiary care center. The case records of all patients with magnetic resonance imaging (MRI)–confirmed isolated ACL tear who underwent ACLR at least 3 months after the MRI diagnosis were reviewed. All patients with MRI (1.5 T)–diagnosed isolated ACL deficiency >3 months who were able to explain and remember the details of any injury-related incidents before surgery were included in the study. Patients who underwent ACLR within 3 months of injury were excluded from the study. Patients with incomplete information on their case records were contacted by the principal author (A.J.); those who could not be contacted and those who were unable to remember the details of any injury-related incidents before surgery were also excluded from the study. The case sheets of all eligible patients were reviewed, and the details of the patients, injury, and surgery were noted.
To define a significant episode of instability, we incorporated 4 parameters—fall attributed to knee buckling, effusion, need of analgesics for knee pain and inability to walk because of it, and restriction of movement following knee buckling—and developed a scoring system (Table 1). Fall attributed to knee buckling is considered a higher grade of instability since it will frequently have effusion, pain, and restriction of movement, as reported by Nevitt et al.21 For this reason, we allotted fall attributed to knee buckling 3 points, as compared with 1 point each for effusion, pain requiring analgesics, and restriction of mobility.
TABLE 1.
The Predictive Scoring System for Significant Instabilitya
| Parameter | No. of Points | |
|---|---|---|
| Yes | No | |
| Fall attributed to knee buckling | 3 | 0 |
| Knee effusion | 1 | 0 |
| Pain requiring analgesics | 1 | 0 |
| Restriction of mobility | 1 | 0 |
| Total possible score | 6 (maximum) | 0 (minimum) |
aA score of ≥3 indicates significant instability.
This scoring system was first tested on 20 consecutive patients with knee injury who were undergoing ACLR/arthroscopy to evaluate their ability to recall a significant episode of instability based on these parameters. All of them could confirm the presence or absence of a significant instability episode based on these parameters, but only 11 of them could confidently recall the number of instability episodes. This led us to apply our PSSSI and not the number of instability episodes for our study.
The PSSSI was used to categorize patients into 2 groups: those who had sustained at least 1 significant episode of instability between the MRI scan and the time of ACLR and those who had not experienced any significant instability events.
The following definitions were adopted for this study:
Significant instability episode after index injury (PSSSI score ≥3): Those episodes of giving way after the index injury that resulted in knee buckling leading to a fall, or knee buckling not leading to a fall but requiring analgesics for pain associated with swelling of knee and restriction of mobility for a few days.
Insignificant instability episode after index injury (PSSSI score <3): Those episodes of giving way after the index injury that did not result in a fall attributed to knee buckling, analgesics for pain, swelling of the knee, or restriction of mobility.
Statistical Analysis
Completed questionnaires with patient data and PSSSI results were coded by numbers and entered into SPSS Statistics (v 23; IBM) for analysis. A descriptive analysis was performed to calculate means and standard deviations, and the Student t test was used to test for differences between the 2 groups. All statistical results were considered significant if the 2-sided P value was <.05. The odds ratio with a 95% CI was calculated for the occurrence of a tear in the significant instability group in comparison with the insignificant instability group.
Results
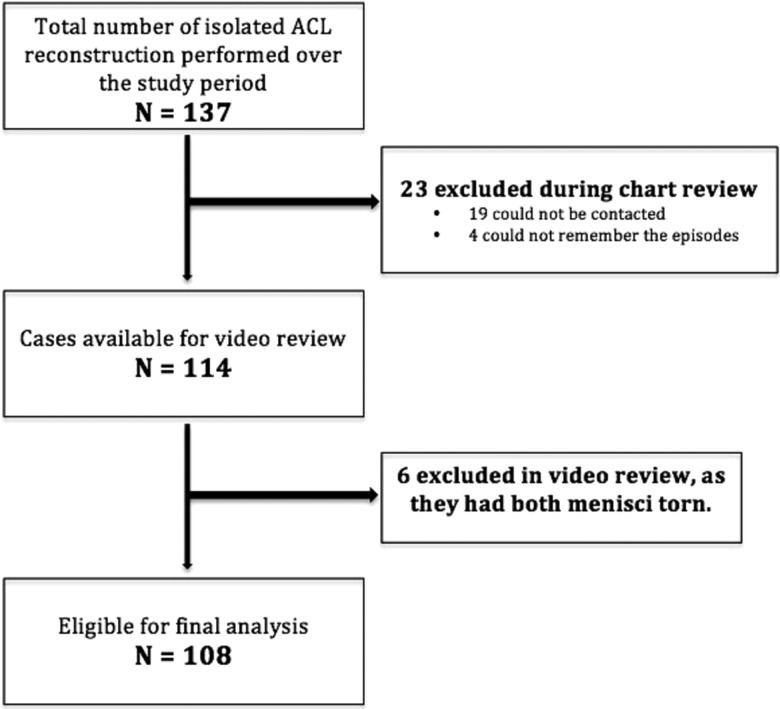
A total of 137 patients underwent ACLR during the study period. Nineteen patients could not be contacted, and 4 did not remember the parameters of the PSSSI. With these 23 cases excluded, the surgical video recordings of all 114 patients were reviewed to document the presence of meniscal injuries and their types. Out of these 114 cases, 6 (5.26%) had medial and lateral meniscal tears; these were also excluded from the study, as we aimed to analyze only isolated tears of menisci. The remaining 108 cases were included for final analysis (Figure 1).
Figure 1.
Patient selection flowchart. ACL, anterior cruciate ligament.
The mean age of the study population was 29.34 ± 8.77 years (range, 16-59 years). The majority (86.1%) were male, and right and left knees were equally involved. There were no significant differences in the demographics of patients who sustained episodes of injury versus those who did not (Table 2).
TABLE 2.
Demographic Data of the Study Population (N = 108)
| Parameters | Total, n (%) | Insignificant Instability Group (n = 46) | Significant Instability Group (n = 62) | P |
|---|---|---|---|---|
| Age,a y | 29.34 ± 8.77 | 30.33 ± 8.69 | 28.61 ± 8.83 | .85 |
| Age group | .39 | |||
| <20 | 15 (13.9) | 4 | 11 | |
| 20-30 | 51 (47.2) | 23 | 28 | |
| 31-40 | 30 (27.8) | 12 | 18 | |
| >40 | 12 (11.4) | 7 | 5 | |
| Sex | .73 | |||
| Male | 93 (86.1) | 39 | 54 | |
| Female | 15 (13.9) | 7 | 8 | |
| Side involvement | .34 | |||
| Right | 60 (55.6) | 28 | 32 | |
| Left | 48 (44.4) | 18 | 30 | |
| Mode of initial | .65 | |||
| injury | .65 | |||
| Sports related | 53 (49.1) | 21 | 32 | |
| Road traffic accident | 36 (33.3) | 18 | 18 | |
| Fall | 10 (9.3) | 3 | 7 | |
| Other | 9 (8.3) | 4 | 5 |
aMean ± SD.
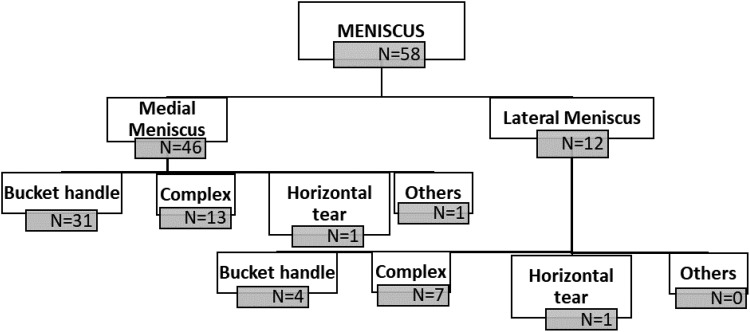
Out of 108 cases, 58 (53.70%) had meniscal tears, and 50 (46.30%) had intact menisci. Among 58 cases with a meniscal tear, 46 (79.3%) had a medial meniscal tear, and 12 (20.7%) had a lateral meniscal tear. The various meniscal tear patterns are described in Figure 2.
Figure 2.
Meniscal tear patterns in the study participants.
A total of 62 patients (57.41%) experienced at least 1 episode of significant instability after the index injury and before surgery, and 46 (42.59%) did not give any history of a significant episode of instability before surgery. Among the patients who had a significant episode of instability, 47 (75.81%) had a meniscal tear, and 15 (24.19%) had intact menisci (P < .001). Among the 46 patients who had no history of a significant episode of instability, 11 (23.91%) had a meniscal tear, and 35 (76.08%) had intact menisci (P < .001). Of the 58 patients who had a meniscal tear, 47 (81.03%) had at least 1 significant episode of instability before surgery, as opposed to 11 (18.97%) who had an insignificant or no episode of instability. There were 50 patients with intact menisci, out of which 35 (70%) had no significant episode of instability and 15 (30%) had a significant episode of instability (Table 3).
TABLE 3.
Incidence of a Tear in Patients With and Without a Significant Episode of Instability
| Meniscal Tear, n (%) | ||||
|---|---|---|---|---|
| Study Group | n | Yes | No | P |
| Significant instability episode | <.001 | |||
| Yes | 62 | 47 (75.81) | 15 (24.2) | |
| No | 46 | 11 (23.91) | 35 (76.08) | |
| Total | 108 | 58 | 50 | |
The comparison between medial and lateral meniscal tears is described in Table 4. In the significant instability group, there were 41 medial meniscal tears, as opposed to 6 lateral meniscal tears. In the group with no significant episode of instability, there were 5 medial meniscal tears and 6 lateral meniscal tears (Figure 2). The difference in medial meniscal tears between groups was statistically significant (P < .001).
TABLE 4.
Comparisons of Parameters Between Medial and Lateral Meniscal Tears (n = 58)
| Meniscal Tear | ||||
|---|---|---|---|---|
| Parameter | n (%) | Medial (n = 46) | Lateral (n = 12) | P |
| Significant instability episode | <.001 | |||
| Yes | 47 (43.52) | 41 | 6 | |
| No | 11 (10.19) | 5 | 6 | |
| Age,a y | 29.34 ± 8.77 | 29.28 ± 9.32 | 28.42 ± 9.37 | .97 |
| Age group | .94 | |||
| <20 | 15 (13.9) | 8 | 2 | |
| 20-30 | 51 (47.2) | 20 | 6 | |
| 31-40 | 30 (27.8) | 12 | 3 | |
| >40 | 12 (11.4) | 6 | 1 | |
| Sex | .77 | |||
| Male | 93 (86.1) | 40 | 11 | |
| Female | 15 (13.9) | 6 | 1 | |
| Side involved | .96 | |||
| Right | 60 (55.6) | 25 | 7 | |
| Left | 48 (44.4) | 21 | 5 | |
| Mode of injury | .32 | |||
| Sports related | 53 (49.1) | 23 | 5 | |
| Road traffic accident | 36 (33.3) | 12 | 7 | |
| Fall | 10 (9.3) | 5 | 0 | |
| Other | 9 (8.3) | 6 | 0 | |
aValues reported as mean ± SD.
The mean age, sex, side involved, and mode of injury were not statistically different between the medial meniscus and lateral meniscus groups. Also, the incidence of medial and lateral meniscal tears in the different age groups was not statistically significant (Table 4).
Discussion
Different recommendations have been made regarding the timing of ACLR, ranging from 8 weeks to 1 year following the index injury.1,3,11 It has been emphasized that if surgery is delayed for more than the recommended period, the incidence of a meniscal tear is significantly higher.1,3 In our study, the cutoff time for inclusion was 3 months after the index injury. This cutoff time was chosen because of our rehabilitation protocol for the acutely injured knee, which lasts for 8 weeks, with the next 4 weeks usually required for patients to feel comfortable and achieve normal gait pattern after the index injury. In a review article, Delincé and Ghafil8 also mentioned the need of 3 months to achieve normal activities when an ACL tear was treated conservatively.
We recorded 58 meniscal tears (46 medial and 12 lateral), with an overall meniscal injury rate of 53.70%, in the patients undergoing surgery for ACL deficiency in this series. Our incidence is similar to that reported by Fok and Yau10 and Brambilla et al,3 who documented 59.8% and 61%, respectively, for meniscal injury in patients undergoing ACLR. However, there is a possibility that some of their patients may have sustained the meniscal tear at the time of the initial injury. Fok and Yau also mentioned that the incidence increased to 77.4% if ACLR was delayed for >12 months. In another study by Fok and Yau,9 the reported incidence was 53.1%. Jacob and Oommen12 found the incidence of meniscal tear to be as high as 86.5%. They described that the incidence of meniscal injury was 50% if ACLR was performed within 6 weeks of injury. The incidence increased to 74.4% and 95.1% if surgery was performed between 6 and 24 weeks and beyond 25 weeks, respectively. Hagino et al11 found an incidence of 72.7% in patients undergoing ACLR within 8 weeks and 84.8% if surgery was delayed beyond 8 weeks. The reason for the higher incidence in some of the studies is due to their study population, which sustained injury owing to sports-related activities. In contrast, only 49.1% of our patients sustained sports-related injuries (Table 2).
The majority of our patients were young (mean age, 29.34 ± 8.77; range, 16-59 years), similar to the study by Mall and colleagues.19 In their study on 129,836 patients, the mean age of patients undergoing ACLR was 29.6 ± 13 years. In our study, we found the highest rate of ACL tears in the age group of 20 to 40 years (75%), similar to the study by Astur and colleagues.2 They also mentioned that there are differences in physical and behavioral maturity in the adult population, which may be the reason for the increased incidence of repeated injury they found in this group. In our study, the youngest patient was 16 years old, indicating that ACL tears are rare in patients younger than 16 years in the patients we see at our institution. This may be attributed to the behavioral pattern. As the population of this age group is school-going and competitive sports are not a part of the school program in our country, students are less exposed to sports injury leading to an ACL tear and subsequent meniscal injuries. In contrast to our results, Leathers et al16 found the highest incidence of an ACL tear in the 10- to 19-year age group. Theirs was a demographic study conducted in the United States, where school-level competitive sports are very well developed as compared with our scenario. We found no significant difference in the incidence of meniscal tear in the different age groups (P = .69), indicating that age is not a predictive factor of a meniscal tear. Jacob and Oommen,12 Kluczynski et al,13 Chhadia et al,5 and Brambilla et al3 also mentioned that the incidence of a meniscal tear is not associated with age at presentation but with the level of activity.
The male:female ratio of meniscal injury in our study was 6.2:1, which is higher than the reported ratios in various studies. Leathers et al16 found a male:female ratio of 2:1 in an American population. Population-based research conducted in Sweden indicated that 60.0% of outpatient ACLRs were being performed on males (53.1 per 100,000 capita male vs 34.0 per 100,000 capita female), and the ratio had a decreasing trend in successive years.22 Kumar et al15 reported a ratio similar to ours from an Indian subcontinent population. The cultural and behavioral differences of our population with those of the Western population may be the cause of this difference, as supported by the study of Kumar et al.
Jacob and Oommen12 reported that meniscal tears occur during the initial traumatic event or subsequently over time owing to repeated trauma because of ongoing instability. This was reaffirmed by Kluczynski et al.13 They mentioned that the number of instability episodes directly correlates with medial meniscal tear when adjusted for time from injury to surgery. This indicates that, rather than time elapsed, the number of episodes of instability is more predictive of a meniscal tear. On the basis of these descriptions, we believe that if a meniscal tear did not occur during the index injury, there had to be another episode of injury, in the form of instability or new injury, and this episode of instability had to be significant enough to cause the meniscal tear. This was the aim behind our developing a scoring system to distinguish a significant versus an insignificant instability episode. The exception to our belief is the “ramp lesion,” which can occur (1) from repetitive anterior subluxation, causing meniscocapsular separation of the medial meniscus, and (2) without a true instability event.17 Our primary hypothesis that the incidence of meniscal injury would be higher in the significant instability group was confirmed by our results.
Nevitt et al21 reported knee buckling as a symptom of knee instability and used it to predict the possibility of falling. They defined severe symptoms as fall and less severe symptoms as buckling without fall. In our series, out of 62 patients who had a significant episode of instability, 23 (37%) had a fall from knee buckling, and 43 (63%) had other symptoms of instability. Kluczynski et al13 discussed episodes of instability without any detailed description of severity and definition. Since not many patients experience a fall from knee buckling, defining the significant episode of instability may be difficult. We know that if there is a meniscal tear, there will be effusion, pain, and restriction of mobility. Given this reason, we have defined the significant instability episodes combining all these parameters and proposed the PSSSI. No literature to date has clearly defined significant instability episodes.
Our data demonstrated that patients who have significant episodes of instability have a ten-fold higher chance of developing medial meniscal tear as compared with those who have insignificant or no episodes of instability (odds ratio, 9.97; 95% CI, 4.08-24.34), but there was no difference in the incidence of the lateral meniscal tear (Table 4) between the groups. Our findings differed from those of Kluczynski et al,13 who found a 4-times higher risk of a medial meniscal tear in those who have multiple episodes of instability before surgery. Fok and Yau10 found that the incidence of meniscal tear almost doubled in those who had a surgical delay >12 months. They also mentioned that the rate of lateral meniscal injury remained static, similar to our study findings. Brambilla and colleagues3 reported that 60% of patients with delayed surgery had medial meniscal tear, and the probability of having medial meniscal tear increased significantly with a delay in surgery. They emphasized that the possibility of lateral meniscal tear did not increase with the delay in surgery.
The aforementioned reasoning confirms that the lateral meniscal tear usually occurs during the index trauma, whereas subsequent instability episodes can lead to medial meniscus tear.5,20 We believe that, rather than the number of instability episodes, the significance of the instability episode predicts medial meniscal tear more precisely following ACL deficiency. As mentioned earlier, 11 patients in the insignificant instability group had a meniscal tear (n = 5, medial; n = 6, lateral). The possible reason for medial meniscal tears in the insignificant episode group may be a false-negative MRI of the knees, or it may be due to repeated insignificant episodes of instability that converted incomplete tears present during the index injury to complete meniscal tears. The cited studies3,10 described that the lateral meniscal tear is not affected by instability episodes, which explains the higher rate of lateral meniscal tears in the insignificant instability group compared with the significant instability group.
The strength of our study includes its consistency with previous epidemiological data and the addition of a new scoring system to define a significant episode of instability, which we found to be associated with the incidence of a medial meniscal tear. In contrast to using the number of episodes, which is relatively difficult for the patient to recall, we propose a new concept of a significant episode of instability that patients can recall easily. However, this scoring system does not really help us predict who can be successfully treated nonoperatively and who should undergo ACLR to try to prevent further injury. Our findings suggest that, once a significant instability event occurs, the meniscal damage has been done.
Limitations
This was a retrospective study with a small sample size. Our study was conducted on patients electing surgery, and it may not allow generalization to all patients with an ACL tear. Our initial testing of the PSSSI was on 20 patients, in which all 20 of them invariably recalled the parameters of the PSSSI more effectively than the number of instability episodes; thus, we did not validate the PSSSI on a larger number of patients. The validation on a small number of patients is another limitation of the study. We suggest that further studies be conducted to validate the scoring system. Since we used MRI alone for the diagnosis of isolated ACL, we might have had false-negative cases, which is another limitation of the study. Also, we did not establish a correlation of instability (significant and insignificant) with timing of surgery and number of instability episodes.
Conclusion
The incidence of a medial meniscal tear was higher in patients with significant episodes of instability as compared with those who did not have a significant episode of instability. A medial meniscal tear was 10 times more likely to occur if there had been a significant episode of instability after an ACL tear. The incidence of lateral meniscal tear did not change with instability. The incidence of meniscal tear did not correlate with age, sex, mechanism of injury, or side of the injury. We conclude that the PSSSI will help clinicians in determining which patients will have medial meniscal tears and in planning their management accordingly. We also conclude that if patients have a significant episode of instability based on the PSSSI, they should be counseled regarding the surgery as early as possible and discard conservative management of ACL deficiency, as they may have a higher likelihood of developing medial meniscal tears.
Footnotes
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Institutional Research Committee of B&B Hospital.
References
- 1. Anstey DE, Heyworth BE, Price MD, Gill TJ. Effect of timing of ACL reconstruction in surgery and development of meniscal and chondral lesions. Phys Sportsmed. 2012;40(1):36–40. [DOI] [PubMed] [Google Scholar]
- 2. Astur DC, Cachoeira CM, da Silva Vieira T, Debieux P, Kaleka CC, Cohen M. Increased incidence of anterior cruciate ligament revision surgery in paediatric verses adult population. Knee Surg Sports Traumatol Arthrosc. 2018;26(5):1362–1366. [DOI] [PubMed] [Google Scholar]
- 3. Brambilla L, Pulici L, Carimati G, et al. Prevalence of associated lesions in anterior cruciate ligament reconstruction: correlation with surgical timing and with patient age, sex, and body mass index. Am J Sports Med. 2015;43(12):2966–2973. [DOI] [PubMed] [Google Scholar]
- 4. Budny J, Fox J, Rauh M, Fineberg M. Emerging trends in anterior cruciate ligament reconstruction. J Knee Surg. 2017;30(1):63–69. [DOI] [PubMed] [Google Scholar]
- 5. Chhadia AM, Inacio MC, Maletis GB, Csintalan RP, Davis BR, Funahashi TT. Are meniscus and cartilage injuries related to time to anterior cruciate ligament reconstruction? Am J Sports Med. 2011;39(9):1894–1899. [DOI] [PubMed] [Google Scholar]
- 6. Cohen M, Amaro JT, Ejnisman B, et al. Anterior cruciate ligament reconstruction after 10 to 15 years: association between meniscectomy and osteoarthrosis. Arthroscopy. 2007;23(6):629–634. [DOI] [PubMed] [Google Scholar]
- 7. Cox CL, Huston LJ, Dunn WR, et al. Are articular cartilage lesions and meniscus tears predictive of IKDC, KOOS, and Marx activity level outcomes after anterior cruciate ligament reconstruction? A 6-year multicenter cohort study. Am J Sports Med. 2014;42(5):1058–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Delincé P, Ghafil D. Anterior cruciate ligament tears: conservative or surgical treatment? A critical review of the literature. Knee Surg Sports Traumatol Arthrosc. 2012;20(1):48–61. [DOI] [PubMed] [Google Scholar]
- 9. Fok AW, Yau WP. Anterior cruciate ligament tear in Hong Kong Chinese patients. Hong Kong Med J. 2015;21(2):131–135. [DOI] [PubMed] [Google Scholar]
- 10. Fok AW, Yau WP. Delay in ACL reconstruction is associated with more severe and painful meniscal and chondral injuries. Knee Surg Sports Traumatol Arthrosc. 2013;21(4):928–933. [DOI] [PubMed] [Google Scholar]
- 11. Hagino T, Ochiai S, Senga S, et al. Meniscal tears associated with anterior cruciate ligament injury. Arch Orthop Trauma Surg. 2015;135(12):1701–1706. [DOI] [PubMed] [Google Scholar]
- 12. Jacob KM, Oommen AT. A retrospective analysis of risk factors for meniscal co-morbidities in anterior cruciate ligament injuries. Indian J Orthop. 2012;46(5):566–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kluczynski MA, Marzo JM, Bisson LJ. Factors associated with meniscal tears and chondral lesions in patients undergoing anterior cruciate ligament reconstruction: a prospective study. Am J Sports Med. 2013;41(12):2759–2765. [DOI] [PubMed] [Google Scholar]
- 14. Kraeutler MJ, Welton KL, McCarty EC, Bravman JT. Revision anterior cruciate ligament reconstruction. J Bone Joint Surg Am. 2017;99(19):1689–1696. [DOI] [PubMed] [Google Scholar]
- 15. Kumar C, Gupta AK, Singh SK, Jain R. Transportal anterior cruciate ligament reconstruction with quadrupled hamstring tendon graft: a prospective outcome study. Indian J Orthop. 2017;51(5):600–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Leathers MP, Merz A, Wong J, Scott T, Wang JC, Hame SL. Trends and demographics in anterior cruciate ligament reconstruction in the United States. J Knee Surg. 2015;28(5):390–394. [DOI] [PubMed] [Google Scholar]
- 17. Liu X, Feng H, Zhang H, Hong L, Wang XS, Zhang J. Arthroscopic prevalence of ramp lesion in 868 patients with anterior cruciate ligament injury. Am J Sports Med. 2011;39(4):832–837. [DOI] [PubMed] [Google Scholar]
- 18. Magnussen RA, Mansour AA, Carey JL, Spindler KP. Meniscus status at anterior cruciate ligament reconstruction associated with radiographic signs of osteoarthritis at 5- to 10-year follow-up: a systematic review. J Knee Surg. 2009;22(4):347–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mall NA, Chalmers PN, Moric M, et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med. 2014;42(10):2363–2670. [DOI] [PubMed] [Google Scholar]
- 20. Millett PJ, Willis AA, Warren RF. Associated injuries in pediatric and adolescent anterior cruciate ligament tears: does a delay in treatment increase the risk of meniscal tear? Arthroscopy. 2002;18(9):955–959. [DOI] [PubMed] [Google Scholar]
- 21. Nevitt MC, Tolstykh I, Shakoor N, et al. Symptoms of knee instability as risk factors for recurrent falls. Arthritis Care Res (Hoboken). 2016;68(8):1089–1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Nordenvall R, Bahmanyar S, Adami J, Stenros C, Wredmark T, Felländer-Tsai L. A population-based nationwide study of cruciate ligament injury in Sweden, 2001-2009: incidence, treatment, and sex differences. Am J Sports Med. 2012;40(8):1808–1813. [DOI] [PubMed] [Google Scholar]
- 23. Øiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009;37(7):1434–1443. [DOI] [PubMed] [Google Scholar]
- 24. Shelbourne KD, Gray T. Results of anterior cruciate ligament reconstruction based on meniscus and articular cartilage status at the time of surgery: five- to fifteen-year evaluations. Am J Sports Med. 2000;28(4):446–452. [DOI] [PubMed] [Google Scholar]