Abstract
The retrotympanic anatomy is complex and variable but has received little attention in the radiological literature. With advances in CT technology and the application of cone beam CT to temporal bone imaging, there is now a detailed depiction of the retrotympanic bony structures.
With the increasing use of endoscopes in middle ear surgery, it is important for the radiologist to appreciate the nomenclature of the retrotympanic compartments in order to aid communication with the surgeon. For instance, in the context of cholesteatoma, clear imaging descriptions of retrotympanic variability and pathological involvement are valuable in pre-operative planning.
The endoscopic anatomy has recently been described and the variants classified. The retrotympanum is divided into medial and lateral compartments with multiple described potential sinuses separated by bony crests.
This pictorial review will describe the complex anatomy and variants of the retrotympanum. We will describe optimum reformatting techniques to demonstrate the structures of the retrotympanum and illustrate the associated anatomical landmarks and variants with CT. The implications of anatomical variants with regards to otologic surgery will be discussed.
Introduction
Advances in CT technology and the application of cone beam CT (CBCT) to temporal bone imaging have allowed increasingly detailed demonstration of the middle ear structures. Despite these improvements, the complex and variable retrotympanic anatomy has received little attention in the radiological literature. The increasing use of angled endoscopes (e.g. 30 and 45°) (),Figures 1–3 during transcanal approaches and canal wall up mastoidectomies has also allowed the retrotympanic anatomy to be better visualized at surgery and for disease to be accessed with less bone removal.1–8 Thus, an understanding of the correlation between radiological and endoscopic anatomical concepts has become increasingly important.
Figure 1. .

(A) Axial CT through the left temporal bone demonstrating the transcanal position of a 30–45° angled endoscope and its field of view, enabling visualization of the the medial but not the lateral retrotympanum. (B) Axial CT through the left temporal bone demonstrating the transcanal position of a 70° angled endoscope and its field of view, enabling visualization of the lateral retrotympanum whilst sacrificing some of the medial view.
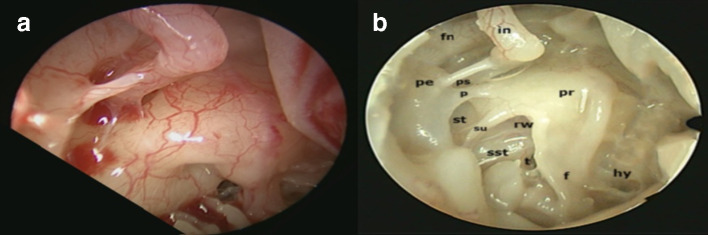
Figure 2. .
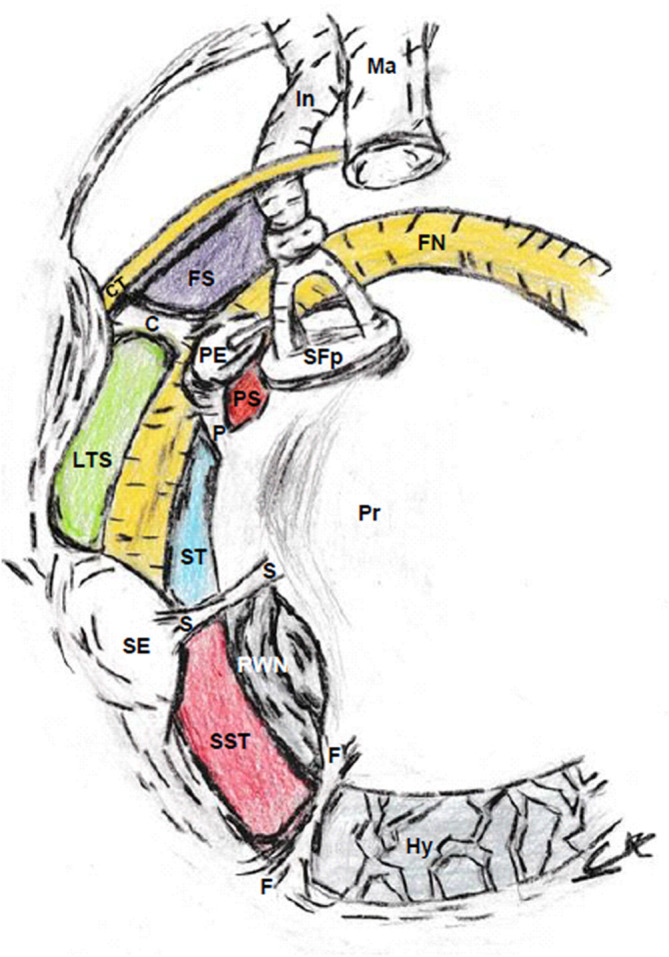
Diagrammatic representation of the retrotympanum from a right ear transcanal view. Key: C, chordiculus; CT, chorda tympani; F, funiculus; FN, facial nerve; FS, facial sinus; Hy, hypotympanum; In, incus; LTS, lateral tympanic sinus; Ma, malleus; P, ponticulus; PE, pyramidal eminence; Pr, cochlear promontory; PS, posterior sinus; RWN, round window niche; S, subiculum; SE, styloid eminence; SFp, stapes footplate; SST, sinus subtympanicum; ST, sinus tympani.
Figure 3. .
Right ear intraoperative middle ear transcanal endoscopic image (a) with comparative labelled endoscopic middle ear image (b) Key: f, funiculus; fn, facial nerve; hy, hypotympanum; in, incus; p, ponticulus; pe, pyramidal eminence; pr, cochlear promontory; ps, posterior sinus; rw, round window; sst, sinus subtympanicus; st, sinus tympani; su, subiculum; t, subcochlear tunnel.
This is of particular importance in the context of pre-operative cholesteatoma surgical planning.1–8 Since the retrotympanum is frequently involved by cholesteatoma, particularly that extending posteriorly from the pars tensa (Figure 4).9 Due to restricted surgical access and unpredictable retrotympanic anatomy (Figures 1–3), the intraoperative assessment of disease location and successful clearance may be challenging and it has traditionally been a common site of residual disease postoperatively.1–8
Figure 4. .
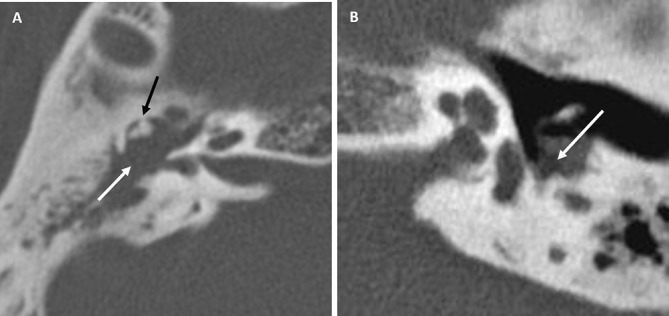
Axial CT images demonstrating pars tensa cholesteatoma. (A) Right ear with cholesteatoma filling the epitympanum (white arrow) and displacing the the incus and malleal head laterally (black arrow). (B) Left ear with cholesteatoma opacification tracking down along the retrotympanum surface (white arrow)
A detailed pre-operative CT interpretation of the retrotympanum (Figure 5 andFigure 6) and communication with the surgical team can highlight areas of surgically occult disease and significant anatomical variations, thus enabling the most efficient surgical approach.1,10 Appreciation of the accepted nomenclature (Table 1) and radiological correlates is key to this communication.
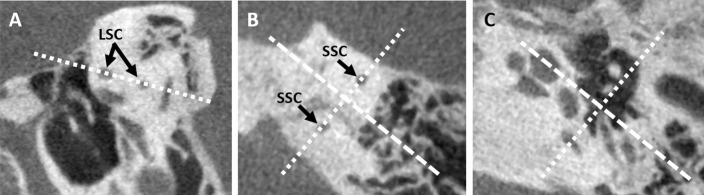
Figure 5. .
(A) Left temporal bone axial CT reformat line (dashed white line) through the LSC. (B) Poschl (dashed white squares), parallel to the SSC and Stenvers’ (dashed white rectangles), perpendicular to the SSC, reformat planes on left temporal bone axial CT. (C) Poschl (dashed squares) and Stenvers’ (dashed rectangles) projection planes through the left temporal bone medial and lateral retrotympanic spaces respectively. LSC, lateral semicircular canal; SCC, superiorsemicircular canal.
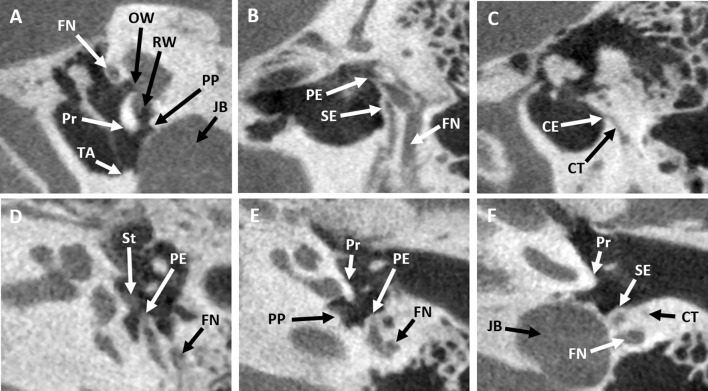
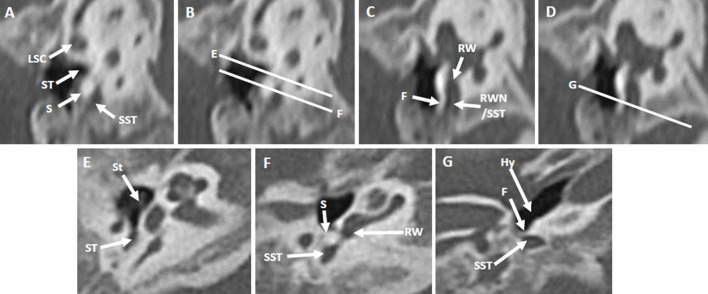
Figure 6. .
CBCT images (left ear) demonstrating key axial and sagittal retrotympanic anatomy. (A) Sagittal oblique (Poschl) image through the medial retrotympanum. (B) Midline image through the plane of the styloid and pyramidal eminences. (C) Coronal oblique (Stenvers’) image through the lateral retrotympanum. (D) Axial images at the level of the stapes demonstrating the pyramidal eminence, (E) at the superior aspect of the cochlear promontory demonstrating the pyramidal eminence, (F) and at the inferior aspect of cochlear promontory demonstrating the styloid eminence. Key: CBCT, cone beam CT; CE, chordal eminence; CT, chorda tympani; FN, facial nerve; JB, jugular bulb; OW, oval window; Pr, cochlear promontory; PE, pyramidal eminence; PP, posterior pillar of the round window; RW, round window; St, stapes; SE, styloid eminence; TA, tympanic annulus.
Table 1. .
A list of the structural imaging criteria for commonly used retrotympanic anatomy nomenclature
| Nomenclature | Structural definition |
|---|---|
| Ridge | A continuous bony crest completely diving two sinus spaces (Figures 7–11). |
| Bridge | A bony crest that is incomplete inferiorly allowing a gap for communication between two sinuses (Figures 7 and 11). |
| Incomplete | A bony crest which terminates prematurely before reaching one of its defined end point landmarks or projects from both landmarks and fails to meet in the middle. |
| Medial retrotympanum | |
| Pyramidal eminence | Superior midline triangular bony projection from the retrotympanum containing the stapedial muscle and giving rise to the stapedius tendon (Figures 2, 3, 6 and 9–11). |
| Styloid eminence | Inferior midline smooth bony elevation of the retrotympanic wall representing the superior end if the styloid process (Figures 2, 6, 10 and 11). |
| Pyramidal ridge | A midline bony crest passing between the pyramidal eminence and the styloid eminence (Figure 10). |
| Ponticulus | A bony crest (ridge, bridge or incomplete) passing between the pyramidal eminence and the cochlear promontory (Figures 2, 3 and 6–8). |
| Subiculum | A bony crest (ridge, bridge or incomplete) passing between the posterior pillar of the round window and the styloid eminence (Figures 2, 3 and 7–10). |
| Funiculus | A bony crest passing between the anterior round window pillar and the jugular bulb along the cochlear promontory (Figures 2, 3, 7–9 and 12). |
| Lateral retrotympanum | |
| Chordal eminence | The anterior superior bony prominence of the canaliculus chordae tympani as the chorda tympani enters the middle ear cavity (Figures 6, 10 and 11). |
| Chordiculus | A bony crest (ridge, bridge or incomplete) passing between the pyramidal eminence superiorly and the chordal eminence inferiorly (Figures 2, 10 and 11). |
| Styloid ridge | A bony crest passing between the chordal eminence and the styloid eminence (Figures 11 and 13) |
There has been a description of the endoscopic anatomy, and a classification of the variants has recently been proposed.10 This divides the retrotympanum into medial and lateral compartments with multiple potential sinuses separated by bony crests. In this pictorial review, we will describe the anatomical nomenclature and correlates in the context of cross-sectional CT studies. We will also indicate the optimal reformatting techniques to demonstrate the structures of the retrotympanum and illustrate the associated anatomical landmarks and variants. In addition, surgically relevant variants will be described and the implications with regards to otologic surgery discussed.
Retrotympanic anatomy
The retrotympanum is divided into medial and lateral portions by the pyramidal and styloid eminences. Sometimes these are linked by a bony crest, the pyramidal ridge, which completely separates the two compartments.1
Medial retrotympanum:
The medial retrotympanum has four described potential sinuses (posterior sinus, sinus tympani, subtympanic sinus and hypotympanum) separated by three bony crests (ponticulus, subiculum and funiculus) (Figures 2 and 3 and Table 1).4,5,10 The posterior sinus sits adjacent to the oval window. This is separated inferiorly from the sinus tympani by the ponticulus bony crest, passing between the cochlear promontory and the pyramidal eminence.10 The sinus tympani is bounded inferiorly by the subiculum bony crest passing from the posterior pillar of the round window niche to the styloid eminence.5,10 The sinus subtympanicus sits below the subiculum and is itself bounded inferiorly by the funiculus bony crest.4,10 The funiculus arises from the anterior pillar of the round window and traverses towards the jugular bulb, separating the sinus subtympanicus from the hypotympanum anteriorly and inferiorly.4,10
Lateral retrotympanum:
The lateral retrotympanum has three described potential sinuses (facial sinus, lateral tympanic sinus and hypotympanum) separated by two bony crests (chordiculus and styloid ridge) (Figure 2 and Table 1).1,10 The chordiculus extends between the chordal eminence (covering the anterosuperior portion of canaliculus chordae tympani) and the pyramidal eminence, separating the facial sinus above from the lateral tympanic sinus below.1 The lateral tympanic sinus is itself bounded inferiorly by the styloid ridge extending between the chordal eminence and the styloid eminence.10
CT reformatting technique
To assess the retrotympanum CT images should first be reformatted axially in plane with the ipsilateral lateral semicircular canal. The plane of subsequent sagittal reformats depend on whether the medial or lateral structures are to be interrogated(Figure 5). The medial retrotympanum requires oblique sagittal reformats in a Poschl projection (parallel to the superior semicircular canal). The lateral retrotympanum requires oblique coronal reformats in a Stenvers’ projection (perpendicular to the superior semicircular canal). Both oblique reformats require minor case by case modification to the axis of the bony crests.
CT anatomical correlates
To navigate the middle ear and retrotympanic anatomy there are several key basic anatomical landmarks, which act as boundaries and attachments for bony crests, which must first be understood and identified. On axial images from superior to inferior the key landmarks are the pyramidal eminence, cochlear promontory, posterior pillar of the round window, styloid eminence, chorda tympani and jugular bulb (Figure 6, images D–F). Sagittal oblique reformats allow identification of the cochlear promontory, round window and its posterior pillar (Figure 6, image A). Midline sagittal oblique reformats through the pyramidal eminence enable an appreciation of the pyramidal and styloid eminences as dividers between the medial and lateral retrotympanic compartments (Figure 6, image B). Coronal oblique reformats allow identification of the chorda tympani emerging into the retrotympanum at the chordal eminence (Figure 6, image C).
Imaging examples
Medial retrotympanum
Case 1 (Figure 7)
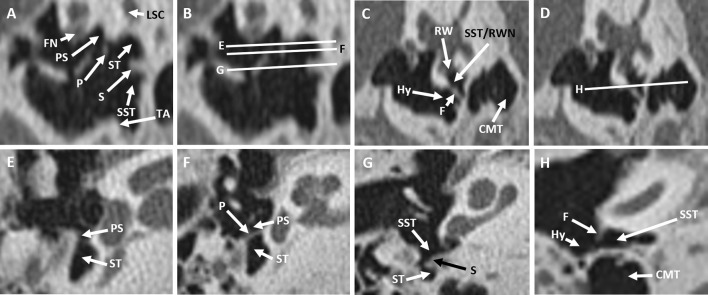
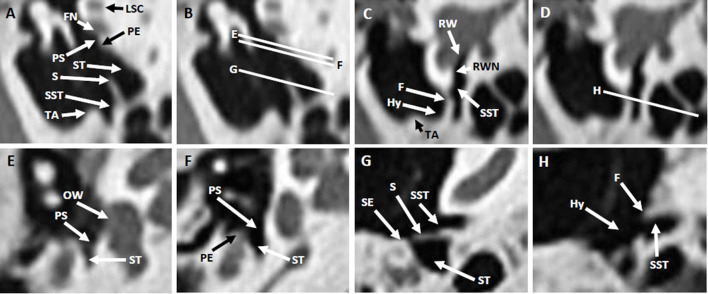
Figure 7. .
(A–D) Sagittal oblique (Poschl) reformats through the right temporal bone medial retrotympanum with axial slices corresponding to images E–H (images B, D). (E–H) Axial images superior to the ponticulus (E), at the ponticulus bridge (D), at the subiculum ridge (G), and at the funiculus (H). Key: F, funiculus; FN, facial nerve; Hy, hypotympanum; LSC, lateral semicircular canal; CMT, central mastoid tract; P, ponticulus; PS, posterior sinus; RW, round window; RWN; round window niche; S, subiculum; SST, sinus subtympanicus; ST, sinus tympani; TA, tympanic annulus.
This CT demonstrates three bony crests: ponticulus bridge, subiculum ridge and funiculus ridge. These divide the retrotympanum into four separate sinuses: posterior sinus, sinus tympani, sinus subtympanicus and hypotympanum.
Case 2 (Figure 8)
Figure 8. .
(A–D) Sagittal oblique (Poschl) reformats through the right temporal bone medial retrotympanum with axial slices corresponding to images E–G (images B, D). Axial images at the ponticulus ridge (E), at the subiculum ridge (F) and at the funiculus (G). Key: F, funiculus; Hy, hypotympanum; LSC, lateral semicircular canal; P, ponticulus; PS, posterior sinus; RW, round window; RWN, round window niche; S, subiculum; SST, sinus subtympanicus; ST, sinus tympani; TA, tympanic annulus.
This CT demonstrates three bony crests: ponticulus ridge, subiculum ridge and funiculus ridge. These divide the retrotympanum into four separate sinuses: posterior sinus, sinus tympani, sinus subtympanicus and hypotympanum.
Case 3 (Figure 9)
Figure 9. .
(A–D) Sagittal oblique (Poschl) reformats through the right temporal bone medial retrotympanum with axial slices corresponding to images E–H (images B, D). (E–H) Axial images at the oval window (E), at the pyramidal eminence with an absent ponticulus (F), at the subiculum ridge (G) and at the funiculus (H). Key: F, funiculus; FN, facial nerve; Hy, hypotympanum; LSC, lateral semicircular canal; OW, oval window; PE, pyramidal eminence; PS, posterior sinus; RW, round window; RWN, round window niche; S, subiculum; SST, sinus subtympanicus; ST, sinus tympani; TA, tympanic annulus.
This CT demonstrates two bony crests: subiculum ridge and funiculus ridge with an absent ponticulus. These divide the retrotympanum into three separate sinuses: continuous posterior sinus and sinus tympani, sinus subtympanicus and hypotympanum.
Lateral retrotympanum:
Case 4 (Figure 10)
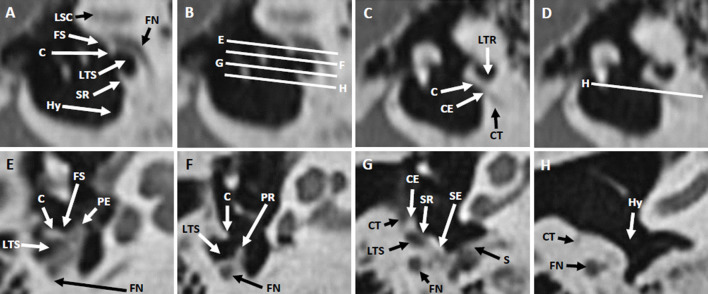
Figure 10. .
(A–D) Coronal oblique (Stenvers’) reformats through the right temporal bone lateral retrotympanum with axial slices corresponding to images E–H (images B, D). (E–H) Axial images at the chordiculus insertion into the pyramidal eminence (E), at the proximal chordiculus ridge (F), at the styloid ridge (G) and at the hypotympanum (H). Key: C, chordiculus; CE, chordal eminence; CT, chorda tympani; FN, facial nerve; FS, facial sinus; Hy, hypotympanum; LSC, lateral semicircular canal; LTS, lateral tympanic sinus; PE, pyramidal eminence; PR, pyramidal ridge; S, subiculum; SR, styloid ridge.
This CT demonstrates two bony crests: chordiculus and styloid ridges. These divide the lateral retrotympanum into three separate sinuses; facial recess, lateral tympanic sinus and hypotympanum.
Case 5 (Figure 11)
Figure 11. .
(A–D) Coronal oblique (Stenvers’) reformats through the left temporal bone lateral retrotympanum with axial slices corresponding to images E–H (images B, D). (E–H) Axial images at the facial sinus (E), at the chordiculus bridge (F), at the styloid ridge (G) and at the chordal eminence (H). Key: C, chordiculus; CE, chordal eminence; CT, chorda tympani; FS, facial sinus; Hy, hypotympanum; LTS, lateral tympanic sinus; PE, pyramidal eminence; SE, styloid eminence; SR, styloid ridge.
This CBCT demonstrates two bony crests: chordiculus bridge and styloid ridge. These divide the lateral retrotympanum into three separate sinuses; facial recess, lateral tympanic sinus and hypotympanum.
Dysplastic retrotympanum:
Case 6 (Figure 12)
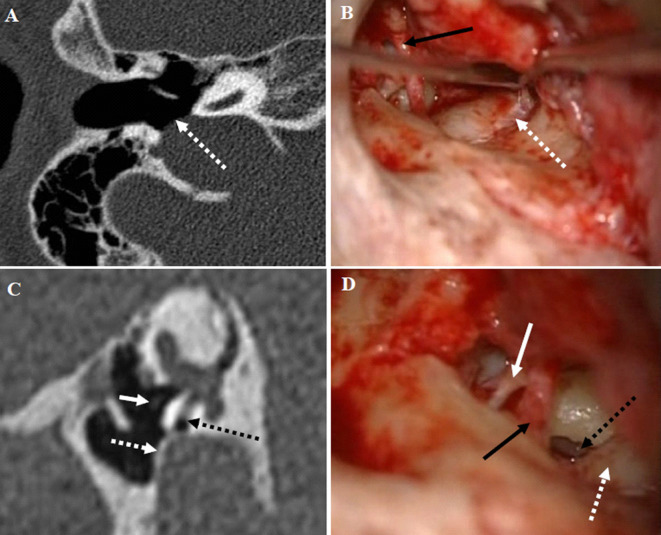
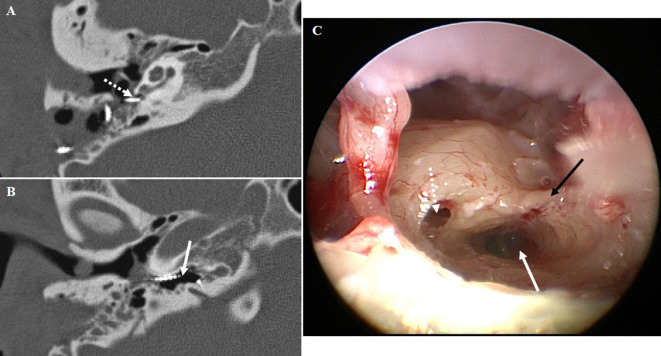
Figure 12. .
(A) Right temporal bone axial CT image at the level of the handle of malleus demonstrating a high riding jugular bulb with dehiscent sigmoid plate (dashed white arrow) bulging into the hypotympanum. (B) Right ear intraoperative endoscopic image (cranial caudal axis is left to right) demonstrating a dehiscent jugular bulb (dashed white arrow) with the chorda tympani seen coursing through the mesotympanum (black arrow). (C) Right temporal bone sagittal oblique (Poschl) reformat CT image demonstrating a high riding jugular bulb with intact sigmoid plate (dashed white arrow) bulging into the hypotympanum and severely narrowing the round window niche (black dashed arrow), stapes head (solid white arrow) demonstrated for reference to image D. (D) Right ear intraoperative endoscopic image (cranial caudal axis is left to right) demonstrating a high riding jugular bulb (dashed white arrow) encroaching on the round window niche (dashed black arrow) with the stapes body (solid white arrow) and chorda tympani (solid black arrow) also visualized.
In congenital aural atresia the middle ear cavity structures, including the retrotympanum, can demonstrate severe dysplasia and aberrant anatomy. This CT in a patient with Treacher Collins syndrome demonstrates a hypoplastic middle ear cavity, dysplastic stapes and an abnormally large subiculum which almost completely blocks the round window niche.
Imaging challenges
The retrotympanum is a challenge to depict on CT due to the highly variable orientation, morphology and thickness of the defining bony structures. An oblique sagittal reformat orientated perpendicular to the long axis of these bony crests is most useful. This somewhat overcomes the variability in the angle of the crests which markedly influences their appearance on axial sections. It is possible that thin or partially incomplete (e.g. bridges) bony structures may not be visible due to partial volume. The structures are also known to be deficient as variant anatomy: for instance the ponticulus and subiculum are absent or incomplete at endoscopy in up to a 1/4 and a 1/3 of cases respectively.10 Further, in patients with a markedly pneumatized middle ear floor it can be difficult to distinguish thin bony ridges from the prominent walls of adjacent air cells.
Other significant retrotympanic variants to evaluate pre-operatively
There are several further anatomical variants with associated operative risks and challenges, which are important to identify and relay to the otologist pre-operatively.
Round window stenosis
The round window and its niche are a key portal for cochlear and active middle ear implant insertion.11 Stenosis of the window itself or encroachment on the niche of other structures such as a high jugular bulb (Figures 13 and 14), can significantly complicate, or render insertion/placement impossible.
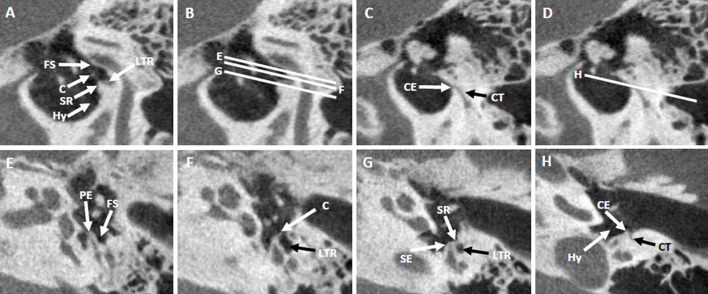
Figure 13. .
(A–D) Sagittal oblique (Poschl) reformats through the right temporal bone medial retrotympanum with axial slices corresponding to images E–G (images B, D). Axial images at the stapes (E), at the dysplastic subiculum (F) and at the funiculus (G). Key: F, funiculus; Hy, hypotympanum; LSC, lateral semicircular canal; RW, round window; RWN, round window niche; S, subiculum; SST, sinus subtympanicus; St, stapes; ST, sinus tympani.
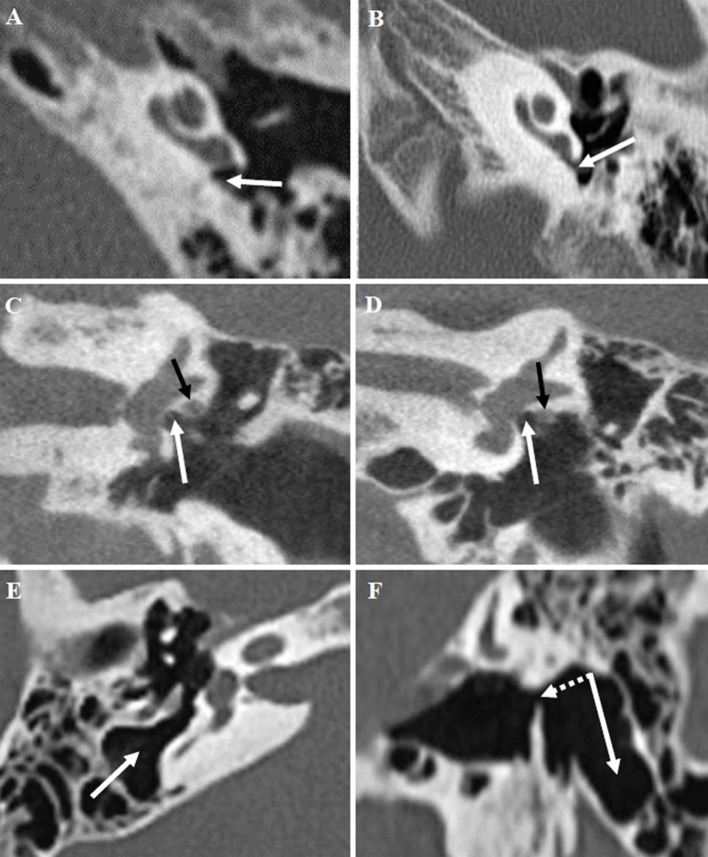
Figure 14. .
(A) Axial CT image demonstrating a normal calibre round window niche (white arrow). (B) Axial CT image demonstrating round window niche stenosis (white arrow). (C) Coronal CT image at the level of the oval window niche (white arrow) demonstrating a well developed tympanic facial nerve canal with no suspicion of dehiscence. (D) Coronal CT image at the level of the oval window niche (white arrow) demonstrating a very shallow tympanic facial nerve canal with likely dehiscence. (E) Axial CT image through a deepsinus tympani (white arrow). (F) Corresponding sagittal oblique (Poschl) reformat to image E demonstrating the full superior (dashed white arrow) to inferior (white arrow) extent of the sinus tympani.
Infracochlear canaliculus
The presence of an infracochlear canaliculus may pose a challenge during cochlear implantation. This is a pneumatized tunnel extending inferior to the cochlear promontory to connect with the petrous apex. Due to their close proximity this may be confused with the round window niche and lead to implant electrode misplacement (Figure 15).
Figure 15. .
(A, B) Right temporal bone axial CT images from the same patient demonstrating; (A) superiorly the cochlear implant passing through the round window niche (dashed white arrow), and (B) inferiorly the electrode array missing the round window and coiling within the infracochlear canaliculus. (C) Right ear intraoperative endoscopic image image (cranial caudal axis is left to right) demonstrating the round window niche (dashed white arrow) and a large infracochlear canaliculus (solid white arrow) located just inferiorly. This image also demonstrates a funiculus ridge (black arrow).
Deep sinus tympani
The extension of the sinus tympani in relation to the facial nerve mastoid segment has been classified into three categories (A, B and C).12 A type C sinus tympani (Figure 13) extends both medially and posteriorly to the facial nerve and can hide pathology such as cholesteatoma.12 This risks incomplete surgical clearance of disease and an alternative surgical approach (retro-facial) may be required.12
Dehiscent facial nerve
Tympanic and mastoid facial nerve dehiscence has been shown to occur in 20–27% of temporal bones with cholesteatoma.13,14 Tympanic portion dehiscence can often only be inferred on CT (best assessed on standard coronal reformats) by observing a shallow canal adjacent to the oval window niche (Figure 13). Suspected dehiscence comes with the risk of iatrogenic neural injury or limiting access to the oval window niche at stapedectomy.13,14
Jugular bulb extension and dehiscence in the hypotympanum
A prominent jugular bulb can bulge superiorly into the hypotympanum floor obliterating the normal space (Figure 14). This can complicate middle ear surgery and access to the round window for implants, due to a lack of space and the risk of vascular injury.15 Sometimes the bony covering of the jugular bulb (sigmoid plate) can be dehiscent further increasing the risk (Figure 14).
Conclusion
The complex and variable anatomy of the retrotympanum poses a challenge to radiological depiction and interpretation. The evolution of endoscopic techniques and the increasing contribution of imaging to surgical planning, has made it important for the radiologist to understand the imaging correlates of the retrotympanic structures. This allows the radiologist to add value by enabling communication of pertinent detailed preoperative findings to the surgeon.
Contributor Information
Christian Burd, Email: cburd66@gmail.com.
Irumee Pai, Email: irumee.pai@gstt.nhs.uk.
Stephen Connor, Email: sejconnor@gmail.com.
REFERENCES
- 1.Alicandri-Ciufelli M, Fermi M, Bonali M, Presutti L, Marchioni D, Todeschini A, et al. Facial sinus endoscopic evaluation, radiologic assessment, and classification. Laryngoscope 2018; 128: 2397–402. doi: 10.1002/lary.27135 [DOI] [PubMed] [Google Scholar]
- 2.Ayache S, Tramier B, Strunski V. Otoendoscopy in cholesteatoma surgery of the middle ear: what benefits can be expected? Otol Neurotol 2008; 29: 1085–90. doi: 10.1097/MAO.0b013e318188e8d7 [DOI] [PubMed] [Google Scholar]
- 3.Barakate M, Bottrill I. Combined approach tympanoplasty for cholesteatoma: impact of middle-ear endoscopy. J. Laryngol. Otol. 2008; 122: 120–4. doi: 10.1017/S0022215107009346 [DOI] [PubMed] [Google Scholar]
- 4.Marchioni D, Alicandri-Ciufelli M, Piccinini A, Genovese E, Presutti L. Inferior retrotympanum revisited: an endoscopic anatomic study. Laryngoscope 2010; 120: 1880–6. doi: 10.1002/lary.20995 [DOI] [PubMed] [Google Scholar]
- 5.Marchioni D, Alicandri-Ciufelli M, Pothier DD, Rubini A, Presutti L. The round window region and contiguous areas: endoscopic anatomy and surgical implications. Eur Arch Otorhinolaryngol 2015; 272: 1103–12. doi: 10.1007/s00405-014-2923-8 [DOI] [PubMed] [Google Scholar]
- 6.Marchioni D, Molteni G, Presutti L. Endoscopic anatomy of the middle ear. Indian J Otolaryngol Head Neck Surg 2011; 63: 101–13. doi: 10.1007/s12070-011-0159-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Badr-el-Dine M. Value of ear endoscopy in cholesteatoma surgery. Otol Neurotol 2002; 23: 631–5. doi: 10.1097/00129492-200209000-00004 [DOI] [PubMed] [Google Scholar]
- 8.Corrales CE, Blevins NH. Imaging for evaluation of cholesteatoma: current concepts and future directions. Curr Opin Otolaryngol Head Neck Surg 2013; 21: 461–7. doi: 10.1097/MOO.0b013e328364b473 [DOI] [PubMed] [Google Scholar]
- 9.Palva T. The pathogenesis and treatment of cholesteatoma. Acta Otolaryngol 1990; 109(5-6): 323–30. doi: 10.3109/00016489009125151 [DOI] [PubMed] [Google Scholar]
- 10.Bonali M, Anschuetz L, Fermi M, Villari D, Mariani GA, Manzoli L, et al. The variants of the retro- and hypotympanum: an endoscopic anatomical study. Eur Arch Otorhinolaryngol 2017; 274: 2141–8. doi: 10.1007/s00405-017-4492-0 [DOI] [PubMed] [Google Scholar]
- 11.Luers JC, Hüttenbrink KB, Beutner D. Surgical anatomy of the round window-Implications for cochlear implantation. Clin Otolaryngol 2018; 43: 417–24. doi: 10.1111/coa.13048 [DOI] [PubMed] [Google Scholar]
- 15.Huang B-R, Wang C-H, Young Y-H. Dehiscent high jugular bulb: a pitfall in middle ear surgery. Otol Neurotol 2006; 27: 923–7. doi: 10.1097/01.mao.0000226310.97316.99 [DOI] [PubMed] [Google Scholar]
- 12.Marchioni D, Mattioli F, Alicandri-Ciufelli M, Presutti L. Transcanal endoscopic approach to the sinus tympani: a clinical report. Otol Neurotol 2009; 30: 758–65. doi: 10.1097/MAO.0b013e3181b0503e [DOI] [PubMed] [Google Scholar]
- 13.Moody MW, Lambert PR. Incidence of dehiscence of the facial nerve in 416 cases of cholesteatoma. Otol Neurotol 2007; 28: 400–4. doi: 10.1097/01.mao.0000247824.90774.22 [DOI] [PubMed] [Google Scholar]
- 14.Magliulo G, Colicchio MG, Appiani MC, Ciniglio M. Facial nerve dehiscence and cholesteatoma. Ann Otol Rhinol Laryngol 2011; 120: 261–7. doi: 10.1177/000348941112000408 [DOI] [PubMed] [Google Scholar]