Placenta percreta is characterized by invasion of chorionic villi past the myometrium and serosa, toward urogenital organs. Central placenta previa with placenta percreta invading bladder is a very rare obstetrical condition, accounting for 0.3% to 1 per 10,000 births with a mortality rate of 5.6–10% secondary to hemorrhage, infection and damage to adjacent organs [1]. Early diagnosis and timely management has a vital role in reducing morbidity and mortality rate.
We report a case of 34-week placenta previa accrete with history of the previous cesarean section with an unusual clinical scenario.
Case Report
Mrs. X 32-year female G2P1L1 with 34-week gestation was admitted on February 21, 2018, with complaints of spotting per vagina for past 2 days. Her antenatal period was uneventful till 34 weeks of gestation. She had history of one previous cesarean section 2 years back for placenta previa. Her menstrual, personal and medical history was unremarkable.
On general physical examination, she was pale and a 34-week live fetus with cephalic presentation could be palpated on per abdomen examination. Patient was admitted in labor room, and all routine hematological and biochemical investigations were sent. A previous antenatal scan at 20 weeks showed single live fetus of 20 weeks with low-lying placenta. Bleeding subsided spontaneously. Ultrasound Doppler showed single live fetus of 34 + 5 weeks gestation and adequate liquor. Placenta was central completely covering the OS with a succenturiate lobe anteriorly. The boundary between the placenta and myometrium was clear, and there was no evidence of placenta accrete. Patient was administered steroids for expediting lung maturity. Patient was administered 2 units of packed cells to correct hemoglobin of 7 gm%. One day after admission, she started complaining of severe lower abdominal pain. Urinary catheter revealed gross hematuria. Per abdominal examination showed no uterine contractions and no uterine tenderness. Urine microscopy revealed field full of RBCs. Bladder irrigation with normal saline mixed with injection tranaxamic acid was done intermittently on advice of surgeon. Tablet nitrofurantoin 100 mg 8 hourly was started along with bladder irrigation. Cystoscopy was planned for the next day, but at 12:30 am she complained of severe lower abdominal pain and gross hematuria. Per abdominal examinations revealed mild uterine contractions. With a provisional clinical diagnosis of placenta percreta, she was taken for emergency cesarean section under general anesthesia. Patient and relatives were counseled regarding the need of cesarean hysterectomy and unavoidable bladder injury.
Abdomen was opened by a vertical midline incision. Preoperatively, there were prominent tortuous blood vessels on the lower segment of uterus and on the bladder serosa (Fig. 1). A provisional intraoperative diagnosis of placenta accrete was made, and male live baby of 2.2 kg with Apgar of 5/10 was delivered by classical incision. Placenta did not separate spontaneously, so decision of obstetric hysterectomy was taken. The placenta was not invading beyond the uterine surface and the uterovesical plane though highly vascular was clear and not invaded by the placenta. A total hysterectomy was completed. There was generalized oozing from bladder surface. It decreased significantly after bilateral internal iliac ligation was done. Bladder Integrity was confirmed by retrograde filling. Patient was transfused 3 units packed cell and 4 units fresh frozen plasma intraoperatively and was shifted to ICU for further observation. Hematuria continued intraoperatively and persisted for 5 days postoperatively. The initial postoperative hemoglobin of 9 gm% fell to 8.5 on fifth postoperative day. Though the fall was not significant but suspecting some actively bleeding vessel, cystoscopy was done on fifth postoperative day. There were no abnormal findings, and 100 cc of blood clot was removed. Urine became clear after cystoscopy. Catheter was removed on seventh post-op day. She was able to self-void. She was discharged in satisfactory condition on tenth postoperative day after stitch removal. Her routine follow-up 6 weeks later was normal.
Fig. 1.
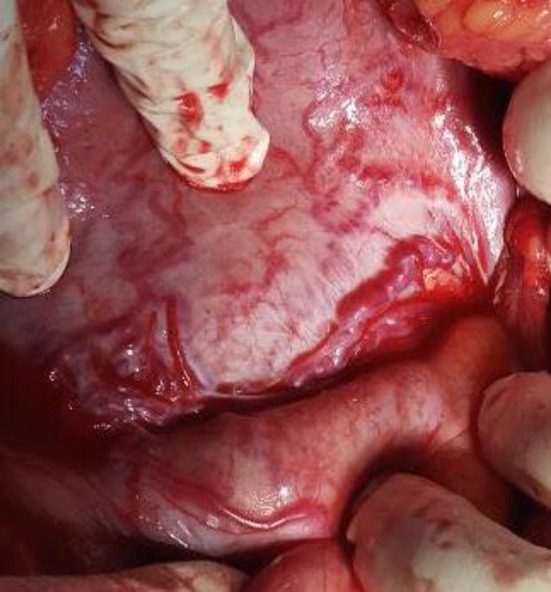
Extensive vascularity on lower uterine segment and bladder
Discussion
Despite extensive advancements in medicine, accrete syndromes remain to be a serious problem in obstetrics significantly increasing maternal morbidity and mortality. Variants of placenta accrete syndrome are classified by the depth of trophoblastic growth. Placenta accreta indicates that villi are attached to the myometrium. With placenta increta, villi actually invade the myometrium, and placenta percreta defines villi that penetrate through the myometrium and to or through the serosa. In clinical practice, these three variants are encountered in an approximate ratio of 80:15:5, respectively [2]. Hematuria is a rare occurrence comprising 25% of all placenta percreta cases. Placenta percreta with bladder invasion should be suspected in any pregnant woman presenting with gross hematuria and a history of previous cesarean section. A multidisciplinary surgical management supported by adequate number of blood products, and the option of uterine artery embolization is essential for successful management. Hysterectomy without any attempts to remove the placenta is the recommended option [3].
Cystoscopy in extensive hematuria may reveal blood clots or actively bleeding vessels. Despite an extensive review of the literature, we could not find any reported case of placenta increta with such gross hematuria. This case probably highlights the enormously increased vascularity associated with accrete syndromes which extended into the uterovesical plane and the bladder mucosa. It needs to be reiterated here that this happened without any evidence of placental invasion outside the uterus.
Evidence indicates that the pathophysiology of accrete syndromes is not limited to anatomical layer deficiency and the cytotrophoblasts may control decidual invasion through factors such as angiogenesis and growth expression [4].
This is further supported by evidence of hyper invasiveness and abnormal vessel distribution seen in accrete syndrome tissue specimens compared with otherwise uncomplicated previa specimens.
Probably this angiogenesis extends to all pelvic tissues and the etiopathogenesis of placenta accrete needs to be demystified further. An informed consent was taken from the patient for publication of her case.
Conclusion
A multidisciplinary team, adequate blood products and devascularization techniques are the key to successful outcome in accrete syndromes. Further studies and evidence are required for a comprehensive understanding of the pathophysiology of accrete syndromes.
Dr Urvashi Miglani
is currently a specialist in gynecology at Deen Dayal Upadhyay Hospital, New Delhi. She has pursued FOGSI Fellowship in Gynae-oncology at Kidwai Memorial Institute, Bengaluru, and WHO Fellowship in endoscopy at the prestigious AIIMS, New Delhi. She has numerous publications in national and international journals to her credit. Her areas of interest are gynae-oncology and endoscopy.
Compliance with Ethical Standards
Conflict of interest
Dr. Urvashi Miglani, Dr. Poonam Laul, Dr. Puneet Chhibbar, Dr. V. K. Kadam and Dr. Neha Jain declare that there is no conflict of interest.
Human and Animal Rights Statement
This article does not contain any studies with human or animal subjects.
Footnotes
Dr. Urvashi Miglani is Specialist (Obs And Gynae) in Deen Dayal Upadhyay Hospital, New Delhi, India; Dr. Poonam Laul is Senior Specialist (Obs And Gynae) in Deen Dayal Upadhyay Hospital, New Delhi, India; Dr. Puneet Chhibber is Senior Specialist and HOU in Department of Surgery, Deen Dayal Upadhyay Hospital, New Delhi, India; Dr. V. K. Kadam is Consultant and Ex HOD (Obs And Gynae) in Deen Dayal Upadhyay Hospital, New Delhi, India and currently Medical Superintendent in Rao Tula Ram Hospital, New Delhi, India; Dr. Neha Jain is Senior Resident in Deen Dayal Upadhyay Hospital, New Delhi, India.
There should be a high degree of clinical suspicion for accrete syndromes in all cases of placenta previa with previous surgery or those presenting with hematuria.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ng MK, Jack GS, Bolton DM, Lawrentschuk N. Placenta percreta with urinary tract involvement: the case for a multidisciplinary approach. Urology. 2009;74(4):778–782. doi: 10.1016/j.urology.2009.01.071. [DOI] [PubMed] [Google Scholar]
- 2.Koukoura O, Lialios G, Garas A, et al. Macroscopic hematuria due to placenta percreta. Report of two cases. Oral presentation. In: Proceedings of the 10th Athens congress on womens health and disease, Athens, Greece, September 2016.
- 3.Silver RM, Fox KA, Barton JR. Center of excellence for placenta accreta. Am J Obstet Gynecol. 2015;212(5):561–568. doi: 10.1016/j.ajog.2014.11.018. [DOI] [PubMed] [Google Scholar]
- 4.Duzyj C, Buhimschi I, Hardy J, et al. Decreased expression of endostatin (ES) And hypoxia-inducible factor 1α (HIF-1α) is associated with excessive trophoblast invasion and aberrant angiogenesis in placenta accreta. Abstract No. 105. Am J Obstet Gynecol. 2013;208(1):58. doi: 10.1016/j.ajog.2012.10.270. [DOI] [Google Scholar]


