Abstract
Background
Psychopathy is a personality disorder characterised by two underlying factors. Factor 1 (affective and interpersonal deficits) captures affective deficits, whilst Factor 2 (antisocial and impulsive/disorganised behaviours) captures life course persistent antisocial behaviours. Impaired processing of threat has been proposed as an aetiologically salient factor in the development of psychopathy, but the relationship of this impairment to the factorial structure of the disorder in adult male offenders is unclear.
Objectives
To investigate whether threat processing deficits are characteristic of psychopathy as a unitary construct or whether such deficits are specifically linked to higher scores on individual factors.
Data sources
A systematic review of the literature was conducted by searching PubMed, Web of Science and PsycINFO.
Methods
Studies were included if they (1) reported physiological measures of threat response as the primary outcome measure (2) indexed psychopathy using a well-validated clinician rated instrument such as the PCL-R (3) investigated male offenders between 18 and 60 years of age (4) reported threat processing analyses using both Factor 1 and Factor 2 scores (5) provided sufficient data to calculate effect sizes and (6) were published in English-language peer-reviewed journals. We identified twelve studies with data on 1112 participants for the meta-analysis of the relationship with Factor 1 scores, and nine studies with data on 801 participants for the meta-analysis of the relationship with Factor 2 scores. We conducted the meta-analyses to calculate correlations using random-effects models.
Results
PCL-R/SV Factor 1 scores were significantly and negatively related to threat processing indices (r = -0.22, (95%CI [-0.28, -.017]). Neither PCL-R/SV Factor 2 scores (r = -0.005, 95%CI [-0.10, 0.09]), nor PCL-R total score (r = -0.05, (95%CI [-0.15, -0.04]) were related to threat processing indices. No significant heterogeneity was detected for the Factor score results.
Conclusions
The meta-analyses of the distinct psychopathy factors suggest that the threat processing deficits observed in male offenders with psychopathy are significantly associated with higher scores on Factor 1. A similar relationship does not exist with Factor 2 scores. Our findings highlight the importance of investigating the potentially discrete relationships between aetiological variables and the two factor constructs in the disorder.
Introduction
Violence is a global public health problem, with most violent crimes being committed by a small group of males who meet diagnostic criteria for conduct disorder in childhood and for antisocial personality disorder (ASPD) in adulthood [1]. Within this population, a subgroup of individuals additionally presents with psychopathy. This is a severe personality disorder encompassing two distinguishable symptomatic factors–affective and interpersonal deficits (interpersonal manipulation, callousness, shallow affect, lack of empathy, known as Factor 1 traits) and life course persistent antisocial and impulsive behaviours (impulsive and reckless behaviour, juvenile delinquency, and early behavioural problems, known as Factor 2 traits) [2]. The antisocial personality disordered group with additional diagnoses of psychopathy begin offending at a younger age, commit a disproportionate number of violent offences, typically fail to benefit from rehabilitation programs and present with higher rates of violent recidivism on release from custodial settings [3].
One measure that has been identified as potentially aetiologically salient in the psychopathic group is the aberrant processing of threatening cues in the social environment [4]. Threat processing is defined as the automatic bodily reactivity to threatening stimuli which elicits defensive responses [5]. Threat processing therefore denotes the activation of a neurobiological mechanism which prepares an organism to react appropriately to imminent threat. In healthy individuals, presentation of aversive or threatening cues such as a shock or loud noise in conditioning paradigms, or startle probes while viewing unpleasant pictures, results in the mobilization of defensive actions, which can be measured by threat-associated responses such as skin conductance levels and startle reflex responding [5, 6, 7]. These autonomic and central nervous system responses are hypothesised to reflect responses to the dimensional aspects of such threatening cues, namely arousal and valence [8, 9], and underpin both the core affective response to such cues, and the preparation for instrumental action [10, 11].
Many studies have demonstrated an abnormal response to aversive stimuli in antisocial individuals, particularly those with high psychopathic traits. For example, Lykken’s landmark study [12] showed that psychopathic individuals had diminished skin-conductance reactivity to a conditioned stimulus associated with shock and less avoidance of punished responses on an avoidance learning task. These findings gave rise to the low-fear hypothesis of psychopathy, positing threat processing deficits as the core underlying feature of the disorder [12]. Numerous studies have since provided support for this theory by demonstrating that offenders with high psychopathic traits show smaller electrodermal responses when anticipating aversive shock [13–17]. Psychopathic individuals also show reduced autonomic reactivity relative to non-psychopathic individuals while processing unpleasant visual images capable of provoking a distressed or fearful response, as expressed by diminished or absent startle modulation and skin-conductance responses [18–22]. Further, startle potentiation in response to aversive events [23, 24] and anticipatory skin conductance response [25] are known to be mediated by a “limbic” network including vmPFC, the amygdala, the thalamus and brainstem (including the peri-aqueductal grey [PAG] and locus coeruleus), suggesting a functional deficit in the amygdala or affiliated structures in psychopathic individuals. Consistent with this, neuroimaging studies of psychopathic individuals have suggested that impaired amygdalar activation occurs during threat processing paradigms including fear conditioning and instrumental learning tasks [26–31].
Recent studies have suggested that deficits in threat processing, such as abnormal responding to aversive stimuli, are more characteristic of Factor 1 of the psychopathy construct (affective and interpersonal deficits). Factor 2 (antisocial and impulsive/disorganised behaviours) scores appear more related to impaired cognitive-executive functioning [32]. In keeping with this, investigations of the physiological measures of threat processing, such as fear-potentiated startle responses and startle blink modulation during aversive stimulation, have shown reduced reactivity in individuals scoring high on Factor 1, but not on Factor 2 [22, 33, 34]. Similarly, reduced skin-conductance response during anticipation of aversive stimuli, one of the most replicated findings in psychopathic individuals, has recently been distinctively associated with Factor 1 [35].
Taken together, these studies suggest that the impaired threat processing seen in psychopathy may be particularly related to Factor 1 (affective and interpersonal deficits) scores in this group. Negatively valenced stimuli do not elicit the same defensive response as they do in non-psychopathic antisocial populations and healthy controls. Further support for this conclusion comes from recent findings indicating that controlling for the correlation between Factor 1 and Factor 2 strengthens the negative association between Factor 1 and threat processing, whilst having no effect on the association between Factor 2 and threat processing [36–38]. Using a global measure of psychopathy based on combined Factor 1 and Factor 2 scores provides limited insights when considering the underlying aetiology of the social cognitive abnormalities in the disorder. A meta-analysis examining the processing of facial or vocal emotional information in psychopathy [39], demonstrated that while the unitary construct of psychopathy was found to be associated with pervasive emotion recognition deficits, a targeted analysis showed that Factor 1 scores were only related to deficits in recognising fear, while Factor 2 scores were associated with deficits in recognising other emotions [39].
Threat processing and other aetiological components of psychopathy may therefore also be best understood and investigated as being related in different ways to Factor 1 and Factor 2 traits within the disorder. To date however, no systematic review or meta-analysis has attempted to disentangle the link between the factorial constructs of psychopathy and threat processing impairments. Consequently, it remains unclear whether the observed deficits in threat processing are characteristic of the condition or of only one of its constituent factors. This ambiguity needs to be resolved to help to promote a better understanding of causal mechanisms and to help to develop effective interventions [40]. To our knowledge, only one previous systematic review investigating threat processing in psychopathy (dimensionally conceptualised to include clinician-assessed offender samples and self-rated community and student populations) has been published [4]. The review aimed to determine whether the fear processing abnormalities in psychopathy were best characterised as impairments in automatic threat processing, impairments in the conscious experience of fear, or both. The findings suggested that psychopathy is characterised by impaired automatic threat processing. However, their analysis of the relationship between the distinct psychopathy factors and threat processing returned nonsignificant results. The current work will seek to extend these findings by examining automatic threat processing in psychopathy, but solely in the context of offender populations subject to detailed clinician assessment in studies that report factor-based analyses. Furthermore, the project uses standardised PRISMA approaches to reporting to ensure clarity and transparency of the review process [41]. Research has suggested that community samples manifest lower degrees of both psychopathy factors and predominantly possess the affective deficits with relatively reduced degrees of antisocial features (whereas offenders with psychopathy possess high scores on both factors [42, 43]). The strength of the association between the two factors is also stronger among offender in comparison to community samples [44]. Restricting our consideration to offender populations therefore serves to limit confounds and to ensure consistency across included studies. The aim of the present work was to systematically review the psychopathy literature which has reported factorial data and conduct meta-analyses to examine whether threat processing deficits are characteristic of psychopathy as a unitary construct or whether such deficits are specifically linked to higher scores on individual factors. Based on findings in previous work, we hypothesised that impaired threat processing would be related to higher scores on Factor 1 items of the disorder.
Methods
The systematic review and meta-analyses were conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses [41] guideline.
Search strategy
We searched for studies indexed in three databases from their start dates: PsycINFO (1960–28 February 2019), PUBMED (1960–28 February 2019) and Web of Science (1945–28 February 2019). Combinations of search terms relating to threat processing (threat OR fear OR arousal) and psychopathy (psychopathy OR psychopathic OR antisocial OR “offender sample” OR “forensic sample” OR “antisocial personality”) were used. On PsycINFO, additional limits were used for the methodology (male population groups) and publication type (peer reviewed); the other databases did not provide the function required to enable these limits. Reference lists were scanned by hand to identify additional studies. Non-English language articles were excluded.
To ensure rigorous systematic search and identification of all relevant papers, we carried out an additional systematic search looking for studies utilising neuroimaging metrics of threat responsivity. The same databases were searched with a combination of the following search terms: (fear OR threat OR arousal) AND (functional imaging OR functional MRI or fMRI) AND (psychopathy OR psychopathic OR antisocial OR ''offender sample'' OR ''forensic sample'' OR ''antisocial personality''). This secondary search did not reveal any additional papers.
Study eligibility
Threat processing studies had to report physiological measures of threat response as the primary outcome measure (i.e. the dependent variable in analyses). These physiological indices of autonomic nervous system activation included skin conductance response, heart rate, blood pressure, startle blink reflex, fear potentiated startle, theta coherence, event related potentials or neuroimaging derived metrics [6]. Psychopathy had to be defined using a well-validated clinician administered instrument (the PCL-R [2] or SV [45] instrument). Studies were included if a) they investigated male offenders between the ages of 18 and 60 with current or historical criminal convictions, b) they employed sample sizes greater than 10 participants (following guidance on required sample size for accurate effect size estimation, [46]), c) they reported threat processing analyses using factor-based approaches (that is, their analytic approach enabled factor level data to be appraised) d) they provided sufficient data to calculate effect sizes for the separate factor analyses and e) they were published in English-language peer-reviewed journals.
Studies were excluded if a) they examined only female offenders (because psychopathy may be differentially expressed across biological sex [47, 48]), and if b) they had included participants with brain injuries, learning disabilities or major mental illnesses such as schizophrenia or bipolar affective disorder. When suitability for inclusion was in question, this was resolved through discussion between the authors. No effects from non-published data were included in this analysis.
Twelve studies involving 1112 participants were included in the meta-analysis of the relationship between threat processing indices and Factor 1 scores. Nine studies involving 801 participants were included in the meta-analysis of the relationship between threat processing indices and Factor 2 scores. This is due to some papers not providing specific effect sizes for Factor 2 (instead, choosing solely to report the relevant results as ‘‘non-significant”). Fig 1 illustrates the paper selection process (see S1 Table in supplementary material for details on number of papers and reasons for exclusions).
Fig 1. Flowchart of the systematic search strategy.
Data extraction
A standardized form was used to extract data based on a template by the Cochrane Consumers and Communication Review Group (2016) and refined for the purposes of the current paper in view of the use of cross-sectional studies. The following information was collected: (1) authors and year of publication, (2) methods and measures (i.e. tasks), (3) sample size, (4) psychopathy assessment instrument, (5) physiological index of threat processing and (6) main findings. Studies did not report data from overlapping samples.
Quality assessment
To ascertain the quality and susceptibility to bias of individual studies the authors tailored a ten-item scale using items from the STROBE Statement for cross-sectional studies (see S1 File, [49]). Each item was scored 0 or 1. The total score range was 0 to 10. The quality index was calculated at the study level by summing the items across all criteria. Uncertainties about quality were resolved through discussions between authors. Samples were considered of low quality if they scored from 0 to 3 points; medium quality, from 4 to 6 points; and high quality, from 7 to 10 points.
Statistical analysis
All analyses were completed using the meta package for R [50]. The meta-analyses were performed using a random effects model, as we expected considerable heterogeneity due to the small number of studies [51]. Pearson’s r was used as a measure of effect size and was transformed to Fisher’s z for the purposes of analyses [52]. The pooled effect size and its confidence intervals were converted back into the original scale and reported as such. Standardized beta coefficients were converted to r’s using the procedures outlined by Peterson [53]; relevant F value statistics were converted to r using formulas outlined by Field [54]. The relevant beta and F statistics were taken from models including other predictors: S2 Table provides a summary of these models. Cohen’s [55] rules for interpretation were used: r ~ 0.10 is a small effect size, r ~ 0.30 is a medium effect size, r ~ 0.50 is a large effect size.
We tested for heterogeneity with the chi-squared test Cochran’s Q and I2 statistics [56]. The heterogeneity analyses were performed with a random-effects model, with 95% confidence intervals and a two-tailed test. If heterogeneity tests returned significant results, we planned to conduct a further moderator analysis via meta-regression with quality of studies as a moderator (low/moderate/high).
Potential publication bias for relationships with factor 1 and factor 2 scores were assessed graphically and statistically using published methods [57–59].
A summary of the characteristics of the eligible studies and their respective quality indices is included in Table 1. Three studies were classified as having lower quality, six as intermediate and three as higher quality studies.
Table 1. Characteristics of studies included in the meta-analyses.
| Study [ref] | Methods and measures | Participants |
Psychopathy Measure |
Outcome |
Main findings Factor 1 |
Main findings Factor 2 |
Quality index |
|---|---|---|---|---|---|---|---|
| Newman et al, 2010 *‡ [14] | Fear conditioning paradigm | 125 offenders | PCL-R | Fear-potentiated startle (FPS) |
Factor 1 was negatively and significantly associated with outcome. |
No data on Factor 2. | 4 |
| Vaidyanathan et al, 2011 [33] | Startle modulation during affective picture-viewing task | 108 offenders | PCL-R | Startle potentiation | Factor 1 was negatively and significantly associated with outcome. | Factor 2 was negatively and not significantly associated with outcome. | 6 |
| Veit et al, 2013 [60] | Fear conditioning paradigm | 14 offenders | PCL-R | Skin Conductance Response (SCR) | Factor 1 was negatively and not significantly associated with outcome. | Factor 2 was negatively and not significantly associated with outcome. | 4 |
| Baskin-Sommers et al, 2013 ‡ [61] | Startle modulation during affective picture-viewing task |
136 offenders | PCL-R | Emotion modulated startle | Factor 1 was negatively and significantly associated with outcome. | Factor 2 was not associated with outcome. | 5 |
| Venables, 2015 ‡ [32] | Aversive noise during affective picture-viewing task |
139 offenders | PCL-R |
Late positive potential (LPP, measure of affective processing) |
Factor 1 was negatively and significantly associated with outcome. | Factor 2 was positively and not significantly associated with outcome. | 7 |
| Drislane et al, 2013 [62] | Noise probes during affective picture-viewing task |
140 offenders | PCL-R | Event related potentials | Factor 1 was negatively and significantly associated with outcome. | Factor 2 was positively and not significantly associated with outcome. | 4 |
| Baskin-Sommers et al, 2011a *‡ [63] | Fear conditioning paradigm |
87 offenders | PCL-R | Fear-potentiated startle (FPS) | Factor 1 was negatively and significantly associated with outcome. | No data on Factor 2. | 6 |
| Sadeh & Verona, 2012 [64] | Startle probe during an affective-picture viewing task |
63 offenders | PCL-SV | Fear-potentiated startle (FPS) | Factor 1 was negatively and not significantly associated with outcome. | Factor 2 was positively and not significantly associated with outcome. | 6 |
| Casey et al., 2013 † [65] | Emotion regulation during affective picture-viewing task |
61 offenders | PCL-R | Cardiovascular response (heart rate) | Factor 1 was negatively and significantly associated with outcome. | Factor 2 was not associated with outcome. | 6 |
| Verona et al., 2012 [66] | Emotional processing in an emotional-linguistic Go/No-Go task |
45 offenders | PCL-SV | P3 event related potentials | Factor 1 was negatively and not significantly associated with outcome. | Factor 2 was positively and significantly associated with outcome. | 7 |
| Baskin-Sommers et al., 2011b ‡ [67] | Fear conditioning paradigm | 92 offenders | PCL-R | Fear-potentiated startle (FPS) | Factor 1 was negatively and significantly associated with outcome. | Factor 2 was negatively and not significantly associated with outcome | 8 |
| Tillem et al., 2016 *‡ [68] | Picture-viewing paradigm (threat vs neutral pictures) | 99 offenders | PCL-R | EEG theta-coherence | Factor 1 was negatively and significantly associated with outcome. | No data on Factor 2. | 5 |
* Only included in the meta-analysis of Factor 1. This is due to specific papers not providing enough information to calculate effect sizes for Factor 2 (stated as non-significant in the papers).
† Reported standardized beta coefficients, which were converted to r’s
‡ Reported relevant F value statistics, which were converted to r’s
Results
To test whether threat processing is associated with psychopathy as a unitary construct, we carried out pooled analysis of the total PCL-R scores and threat processing measures. The total psychopathy score was not significantly associated with threat processing metrics, r = -0.05 (95% CI [-0.15, - 0.04]). Significant heterogeneity was detected across the pooled studies (Q2 = 20.70, df = 11, p = 0.04/ I2 = 46.9%), indicating that there is considerable variation in study outcomes between the included studies (see S1 Fig). Visual inspection of the funnel plot did not suggest presence of publication bias (see S2 Fig).
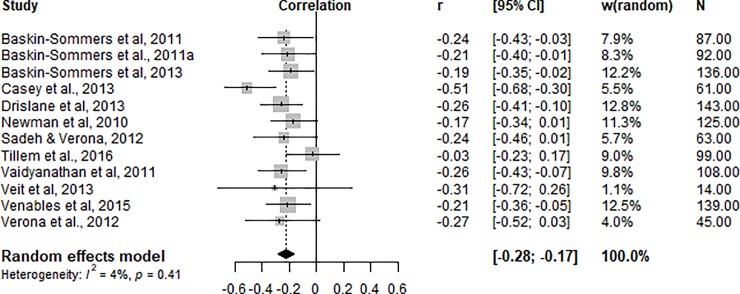
Factor 1
As shown in Fig 2, the pooled analysis of 12 studies showed that Factor 1 (affective and interpersonal deficits) scores had a negative and significant moderate effect on threat processing indices, r = -0.22 (95% CI [-0.28, -0.17]).
Fig 2. Correlations (r) between physiological threat processing index and PCL-R/SV Factor 1 scores.
No significant heterogeneity was detected across studies (Q2 = 11.46, df = 11, p = 0.41/ I2 = 4.0%). A visual inspection of the funnel plot (Fig 3) revealed that the studies were evenly distributed across varying significance levels and Egger’s regression intercept (intercept = -0.10; t = -0.82; df = 11; p = 0.43) suggested no evidence of publication bias.
Fig 3. Funnel plot showing distribution of studies included in the meta-analysis of Factor 1 scores.
Factor 2
Meta-analysis of nine studies indicated that Factor 2 (antisocial and impulsive/disorganised behaviours, Fig 4) scores were not significantly related to threat processing indices r = -0.005 (95% CI [-0.10, 0.09].
Fig 4. Correlations (r) between physiological threat processing index and PCL-R/SV Factor 2 scores.
Heterogeneity analyses revealed no significant between-study variability (Q2 = 13.75, df = 8, p = 0.09/I2 = 41.8%). A visual inspection of the funnel plot (Fig 5) and Egger’s regression intercept (intercept = -0.07; t = -0.42; df = 8; p = 0.68) suggests that there is no publication bias.
Fig 5. Funnel plot showing distribution of studies included in the meta-analysis of Factor 2 scores.
The meta-analysis of the two separate factors did not return significant heterogeneity results, thus no meta-regression analyses were carried out.
Discussion
This meta-analysis examined the relationship between Factor 1 and 2 scores of the psychopathy construct and physiological indices of threat processing in cross sectional studies of male offenders which reported factorial data, identifying 12 studies involving 1112 individuals for Factor 1 scores, and 9 studies involving 801 individuals for Factor 2 scores. The only previous meta-analysis in the field included data from community and student samples which utilised self-report measures [4], which rendered the potential relationship between threat processing measures such as skin-conductance [60], fear-potentiated startle [14, 63, 67] and startle blink modulation [32] and individual factor scores non-significant. For clinicians who utilise the psychopathy construct categorically to help to inform treatment programmes, this relationship required further exploration in a restricted sample of clinician-assessed offenders.
Our findings support the hypothesis that threat processing deficits in male offenders are significantly related to only one of the psychopathy factors, namely Factor 1. Meta-analytic investigation revealed that psychopathy total score and psychopathy Factor 2 scores are not associated with fear responses. Analysis of Factor 1 and threat processing revealed a significant inverse association, indicating that higher scores on this psychopathy factor are associated with greater deficits in threat processing. The effect size was significant and consistent across studies. Heterogeneity was low and not significant, further supporting the consistency of the effect direction across studies. In contrast, threat processing was not significantly related to the Factor 2 traits of psychopathy. Heterogeneity estimates here were moderate and not significant. A smaller number of studies was included in this meta-analysis, yet they consistently reported non-significant relationships between the variables of interest (see Table 1 and Fig 3).
The current findings cannot be readily integrated into the low-fear model, which argues that diminished responsivity to threat lies at the core of the condition, giving rise to other key deficits [12, 69]. Our results, in line with previous empirical investigations [34, 62, 63, 67–69] do not support the notion that impaired threat responsivity is associated with psychopathy as a unitary construct. By contrast, the dual-process model posits that aetiologically distinct pathways lead to the development of the two factors, with threat processing deficits being particularly associated with emotional detachment traits and deficient regulatory control being particularly associated with the life-span persistent antisocial features [70, 71]. Our results fit in with the larger body of empirical evidence on this model specifically linking factor 1 psychopathic traits, and not life-span persistent antisocial behaviour, to an impaired threat processing system [32, 33, 35].
A substantial number of the studies in the current meta-analyses utilised startle responses as measures of threat processing, and these reactions are presumed to be modulated via limbic systems, with a particularly important role for the amygdala [72]. The significant link between Factor 1 and threat processing impairments reported here is consistent with the view that affective deficits in psychopathy are related to atypical structure and function within affective brain systems [73–78]. The amygdala is also presumed to control the early stage processing of threatening stimuli [79] and studies utilising methods restricting conscious awareness, such as backward masking and continuous flash suppression, have shown that it is precisely the affective deficits in antisocial populations that are positively associated with impairments in early stage processing of fearful stimuli [80, 81].
Study limitations
It should be noted that readers need to interpret the current findings in the context of restrictions inherent in our meta-analytic approach. Thus, we included those studies which examined physiological measures of threat response in male offender populations assessed with a clinician administered diagnostic tool, and where effect size measurements were included for both factors. We were unable to secure unpublished data to help to inform the meta-analysis, which may in turn have impacted on the generalizability of the findings. Nevertheless, we sought to clearly establish factor structure associations in the clinical samples with whom we work in custodial settings to help to inform our aetiological considerations and potential future approaches to treatment. Future work could employ moderation analyses to interrogate the possibility that differences may emerge when community samples on the psychopathy continuum [42–44] or female populations [47, 48] are examined.
It was beyond of the scope of the current work to investigate metrics of threat-processing beyond physiological measures. However, previous meta-analytic work on emotion recognition in psychopathy strongly supports the conclusions drawn here [39]. The global psychopathy construct was associated with pervasive deficits in recognition of emotion (fear, sadness, anger, happy, disgust), but Factor 1 scores were specifically associated with impairments in processing fear. Taken together, the literature suggests that Factor 1 is associated with deficient threat processing across different metrics.
Heterogeneity in the meta-analysis of Factor 2, albeit statistically non-significant, indicated the presence of moderate variation. Our analyses were also limited by missing data. Some of the studies identified as eligible did not report effect sizes for Factor 2 so they could not be included, although their results stated that Factor 2 was not significantly related to the outcome (see Table 1).
Treatment implications
Traditional treatments within the criminal justice system are relatively ineffective for psychopathic offenders [82–84]. One possible explanation is that these treatments do not address the unique patterns of dysfunctions present in psychopathic individuals. Findings that the two factors are associated with distinctive cognitive-affective functions, from our studies and others [40, 85–87], strongly suggest that developing evidence-based treatments depends upon targeting the unique factor-specific deficits. Directly translating the current results into clinical practice would suggest that individuals with higher scores on Factor 1 will not be able to utilise aversive learning to shape behaviour, and so alternative strategies are required. Cognitive remediation training targeting the dysfunctions associated with the two factors have shown promising preliminary results [40].
Conclusions
The current findings suggest that impairments in threat processing among psychopathic offenders are significantly associated with scores on Factor 1 but not Factor 2 of the psychopathy construct. These meta-analyses highlight the importance of investigating and evaluating the discrete relationships the two factorial constructs of psychopathy may have with aetiological variables. Developments in therapeutic approaches require just such a nuanced understanding.
Supporting information
(PDF)
(PDF)
(PDF)
(PDF)
(TIF)
(TIF)
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
Dr John Tully is supported by a Wellcome Clinical Research Fellowship (Grant Number 200099/Z/15/Z). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Frick PJ, Viding E. Antisocial behaviour from a developmental psychopathology perspective. Development and psychopathology. 2009. November;21(4):1111–31. 10.1017/S0954579409990071 [DOI] [PubMed] [Google Scholar]
- 2.Hare RD. The psychopathy checklist–Revised. Toronto, ON. 2003. [Google Scholar]
- 3.Hare RD, Hart SD, Harpur TJ. Psychopathy and the DSM-IV criteria for antisocial personality disorder. Journal of abnormal psychology. 1991. August;100(3):391 10.1037//0021-843x.100.3.391 [DOI] [PubMed] [Google Scholar]
- 4.Hoppenbrouwers SS, Bulten BH, Brazil IA. Parsing fear: A reassessment of the evidence for fear deficits in psychopathy. Psychological bulletin. 2016. June;142(6):573 10.1037/bul0000040 [DOI] [PubMed] [Google Scholar]
- 5.LeDoux JE. Coming to terms with fear. Proceedings of the National Academy of Sciences. 2014. February 25;111(8):2871–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mauss IB, Robinson MD. Measures of emotion: A review. Cognition and emotion. 2009. February 1;23(2):209–37. 10.1080/02699930802204677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Calder AJ, Lawrence AD, Young AW. Neuropsychology of fear and loathing. Nature Reviews Neuroscience. 2001. May;2(5):352 10.1038/35072584 [DOI] [PubMed] [Google Scholar]
- 8.Cacioppo JT, Berntson GG, Larsen JT, Poehlmann KM, Ito TA. The psychophysiology of emotion. Handbook of emotions. 2000. May 25;2:173–91. [Google Scholar]
- 9.Bradley MM, Lang PJ. Measuring emotion: Behavior, feeling, and physiology. Cognitive neuroscience of emotion. 2000;25:49–59. [Google Scholar]
- 10.Buzsáki G. Theta rhythm of navigation: link between path integration and landmark navigation, episodic and semantic memory. Hippocampus. 2005;15(7):827–40. 10.1002/hipo.20113 [DOI] [PubMed] [Google Scholar]
- 11.Lakatos P, O'Connell MN, Barczak A, Mills A, Javitt DC, Schroeder CE. The leading sense: supramodal control of neurophysiological context by attention. Neuron. 2009. November 12;64(3):419–30. 10.1016/j.neuron.2009.10.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lykken DT. A study of anxiety in the sociopathic personality. The Journal of Abnormal and Social Psychology. 1957. July;55(1):6. [DOI] [PubMed] [Google Scholar]
- 13.Verona E, Patrick CJ, Curtin JJ, Bradley MM, Lang PJ. Psychopathy and physiological response to emotionally evocative sounds. Journal of abnormal psychology. 2004. February;113(1):99 10.1037/0021-843X.113.1.99 [DOI] [PubMed] [Google Scholar]
- 14.Newman JP, Curtin JJ, Bertsch JD, Baskin-Sommers AR. Attention moderates the fearlessness of psychopathic offenders. Biological psychiatry. 2010. January 1;67(1):66–70. 10.1016/j.biopsych.2009.07.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hare RD. Psychopathy, fear arousal and anticipated pain. Psychological Reports. 1965. April;16(2):499–502. [DOI] [PubMed] [Google Scholar]
- 16.Ogloff JR, Wong S. Electrodermal and cardiovascular evidence of a coping response in psychopaths. Criminal Justice and Behaviour. 1990. June;17(2):231–45. [Google Scholar]
- 17.Hare RD, Frazelle J, Cox DN. Psychopathy and physiological responses to threat of an aversive stimulus. Psychophysiology. 1978. March 1;15(2):165–72. 10.1111/j.1469-8986.1978.tb01356.x [DOI] [PubMed] [Google Scholar]
- 18.Patrick CJ. Emotion and psychopathy: Startling new insights. Psychophysiology. 1994. July 1;31(4):319–30. 10.1111/j.1469-8986.1994.tb02440.x [DOI] [PubMed] [Google Scholar]
- 19.Patrick CJ, Bradley MM, Lang PJ. Emotion in the criminal psychopath: startle reflex modulation. Journal of abnormal psychology. 1993. February;102(1):82 10.1037//0021-843x.102.1.82 [DOI] [PubMed] [Google Scholar]
- 20.Levenston GK, Patrick CJ, Bradley MM, Lang PJ. The psychopath as observer: Emotion and attention in picture processing. Journal of abnormal psychology. 2000. August;109(3):373 [PubMed] [Google Scholar]
- 21.Carmen Pastor M, Moltó J, Vila J, Lang PJ. Startle reflex modulation, affective ratings and autonomic reactivity in incarcerated Spanish psychopaths. Psychophysiology. 2003. November 1;40(6):934–8. 10.1111/1469-8986.00111 [DOI] [PubMed] [Google Scholar]
- 22.Benning SD, Patrick CJ, Iacono WG. Psychopathy, startle blink modulation, and electrodermal reactivity in twin men. Psychophysiology. 2005. November 1;42(6):753–62. 10.1111/j.1469-8986.2005.00353.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pissiota A, Frans Ö, Michelgård Å, Appel L, Långström B, Flaten MA, et al. Amygdala and anterior cingulate cortex activation during affective startle modulation: a PET study of fear. European Journal of Neuroscience. 2003. September 1;18(5):1325–31. 10.1046/j.1460-9568.2003.02855.x [DOI] [PubMed] [Google Scholar]
- 24.Cook EW, Davis TL, Hawk LW, Spence EL, Gautier CH. Fearfulness and startle potentiation during aversive visual stimuli. Psychophysiology. 1992. November 1;29(6):633–45. 10.1111/j.1469-8986.1992.tb02038.x [DOI] [PubMed] [Google Scholar]
- 25.Bechara A, Damasio H, Damasio AR, Lee GP. Different contributions of the human amygdala and ventromedial prefrontal cortex to decision-making. Journal of Neuroscience. 1999. July 1;19(13):5473–81. 10.1523/JNEUROSCI.19-13-05473.1999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kiehl KA, Smith AM, Hare RD, Mendrek A, Forster BB, Brink J, et al. Limbic abnormalities in affective processing by criminal psychopaths as revealed by functional magnetic resonance imaging. Biological psychiatry. 2001. November 1;50(9):677–84. 10.1016/s0006-3223(01)01222-7 [DOI] [PubMed] [Google Scholar]
- 27.Birbaumer N, Veit R, Lotze M, Erb M, Hermann C, Grodd W, et al. Deficient fear conditioning in psychopathy: a functional magnetic resonance imaging study. Archives of general psychiatry. 2005. July 1;62(7):799–805. 10.1001/archpsyc.62.7.799 [DOI] [PubMed] [Google Scholar]
- 28.Mitchell DG, Fine C, Richell RA, Newman C, Lumsden J, Blair KS, et al. Instrumental learning and relearning in individuals with psychopathy and in patients with lesions involving the amygdala or orbitofrontal cortex. Neuropsychology. 2006. May;20(3):280 10.1037/0894-4105.20.3.280 [DOI] [PubMed] [Google Scholar]
- 29.Cohn MD, Popma A, Van Den Brink W, Pape LE, Kindt M, Van Domburgh L, Doreleijers TA, et al. Fear conditioning, persistence of disruptive behavior and psychopathic traits: an fMRI study. Translational psychiatry. 2013. October;3(10):e319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marsh AA, Blair RJ. Deficits in facial affect recognition among antisocial populations: a meta-analysis. Neuroscience & Biobehavioral Reviews. 2008. January 1;32(3):454–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Marsh AA, Finger EC, Mitchell DG, Reid ME, Sims C, Kosson DS, et al. Reduced amygdala response to fearful expressions in children and adolescents with callous-unemotional traits and disruptive behavior disorders. American Journal of Psychiatry. 2008. June;165(6):712–20 10.1176/appi.ajp.2007.07071145 [DOI] [PubMed] [Google Scholar]
- 32.Venables NC, Hall JR, Yancey JR, Patrick CJ. Factors of psychopathy and electrocortical response to emotional pictures: Further evidence for a two-process theory. Journal of abnormal psychology. 2015. May;124(2):319 10.1037/abn0000032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vaidyanathan U, Hall JR, Patrick CJ, Bernat EM. Clarifying the role of defensive reactivity deficits in psychopathy and antisocial personality using startle reflex methodology. Journal of Abnormal Psychology. 2011. February;120(1):253 10.1037/a0021224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dvorak‐Bertsch JD, Curtin JJ, Rubinstein TJ, Newman JP. Psychopathic traits moderate the interaction between cognitive and affective processing. Psychophysiology. 2009. September 1;46(5):913–21. 10.1111/j.1469-8986.2009.00833.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dindo L, Fowles D. Dual temperamental risk factors for psychopathic personality: Evidence from self-report and skin conductance. Journal of personality and social psychology. 2011. March;100(3):557 10.1037/a0021848 [DOI] [PubMed] [Google Scholar]
- 36.Frick PJ, Lilienfeld SO, Ellis M, Loney B, Silverthorn P. The association between anxiety and psychopathy dimensions in children. Journal of abnormal child psychology. 1999. October 1;27(5):383–92. 10.1023/a:1021928018403 [DOI] [PubMed] [Google Scholar]
- 37.Hicks BM, Patrick CJ. Psychopathy and negative emotionality: analyses of suppressor effects reveal distinct relations with emotional distress, fearfulness, and anger-hostility. Journal of abnormal psychology. 2006. May;115(2):276 10.1037/0021-843X.115.2.276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vanman EJ, Mejia VY, Dawson ME, Schell AM, Raine A. Modification of the startle reflex in a community sample: do one or two dimensions of psychopathy underlie emotional processing?. Personality and Individual Differences. 2003. December 1;35(8):2007–21. [Google Scholar]
- 39.Dawel A, O’kearney R, McKone E, Palermo R. Not just fear and sadness: meta-analytic evidence of pervasive emotion recognition deficits for facial and vocal expressions in psychopathy. Neuroscience & Biobehavioral Reviews. 2012. November 1;36(10):2288–304. [DOI] [PubMed] [Google Scholar]
- 40.Baskin-Sommers AR, Curtin JJ, Newman JP. Altering the cognitive-affective dysfunctions of psychopathic and externalizing offender subtypes with cognitive remediation. Clinical Psychological Science. 2015. January;3(1):45–57. 10.1177/2167702614560744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Moher D, Liberati A, Tetzlaff J, Altman DG, Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS medicine. 2009. July 21;6(7): e1000097 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hall JR, Benning SD. The “successful” psychopath: Adaptive and subclinical manifestations of psychopathy in the general population Patrick C.J. (Ed.), Handbook of psychopathy, Guilford Press, New York, NY: (2006), pp. 459–478. [Google Scholar]
- 43.Mahmut MK, Homewood J, Stevenson RJ. The characteristics of non-criminals with high psychopathy traits: Are they similar to criminal psychopaths?. Journal of Research in Personality. 2008. June 1;42(3):679–92. [Google Scholar]
- 44.Neumann CS, Hare RD, Pardini DA. Antisociality and the construct of psychopathy: Data from across the globe. Journal of personality. 2015. December 1;83(6):678–92. 10.1111/jopy.12127 [DOI] [PubMed] [Google Scholar]
- 45.Cooke DJ, Michie C, Hart SD, Hare RD. Evaluating the Screening Version of the Hare Psychopathy Checklist—Revised (PCL: SV): An item response theory analysis. Psychological Assessment. 1999. March;11(1):3. [Google Scholar]
- 46.Hedges LV. Estimation of effect size from a series of independent experiments. Psychological bulletin. 1982. September;92(2):490. [Google Scholar]
- 47.Cale EM, Lilienfeld SO. Sex differences in psychopathy and antisocial personality disorder: A review and integration. Clinical psychology review. 2002. November 1;22(8):1179–207. [DOI] [PubMed] [Google Scholar]
- 48.Salekin RT, Rogers R, Sewell KW. Construct validity of psychopathy in a female offender sample: A multitrait–multimethod evaluation. Journal of abnormal psychology. 1997. November;106(4):576 10.1037//0021-843x.106.4.576 [DOI] [PubMed] [Google Scholar]
- 49.Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, Strobe Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS medicine. 2007. October 16;4(10): e296 10.1371/journal.pmed.0040296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Schwarzer G. meta: An R package for meta-analysis. R News. 2007. 7(3):40–45. [Google Scholar]
- 51.Sterne JA, Gavaghan D, Egger M. Publication and related bias in meta-analysis: power of statistical tests and prevalence in the literature. Journal of clinical epidemiology. 2000. November 1;53(11):1119–29. 10.1016/s0895-4356(00)00242-0 [DOI] [PubMed] [Google Scholar]
- 52.Borenstein M, Hedges LV, Higgins JP, Rothstein HR. Introduction to meta-analysis. John Wiley & Sons; 2011. August 24. [Google Scholar]
- 53.Peterson RA, Brown SP. On the use of beta coefficients in meta-analysis. Journal of Applied Psychology. 2005. January;90(1):175 10.1037/0021-9010.90.1.175 [DOI] [PubMed] [Google Scholar]
- 54.Field A. Discovering statistics using SPSS. Sage publications; 2009. January 21. [Google Scholar]
- 55.Cohen J. Statistical power analysis for the behavioural sciences 2nd edn.
- 56.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ: British Medical Journal. 2003. September 6;327(7414):557 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994. December 1:1088–101. [PubMed] [Google Scholar]
- 58.Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Bmj. 1997. September 13;315(7109):629–34. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sterne JA, Sutton AJ, Ioannidis JP, Terrin N, Jones DR, Lau J, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. Bmj. 2011. July 22;343: d4002 10.1136/bmj.d4002 [DOI] [PubMed] [Google Scholar]
- 60.Veit R, Konicar L, Klinzing JG, Barth B, Yilmaz Ö, Birbaumer N. Deficient fear conditioning in psychopathy as a function of interpersonal and affective disturbances. Frontiers in Human Neuroscience. 2013. October 25;7:706 10.3389/fnhum.2013.00706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Baskin-Sommers AR, Curtin JJ, Newman JP. Emotion-modulated startle in psychopathy: Clarifying familiar effects. Journal of abnormal psychology. 2013. May;122(2):458 10.1037/a0030958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Drislane LE, Vaidyanathan U, Patrick CJ. Reduced cortical call to arms differentiates psychopathy from antisocial personality disorder. Psychological Medicine. 2013. April;43(4):825–35. 10.1017/S0033291712001547 [DOI] [PubMed] [Google Scholar]
- 63.Baskin-Sommers AR, Newman JP, Sathasivam N, Curtin JJ. Evaluating the generalizability of a fear deficit in psychopathic African American offenders. Journal of Abnormal Psychology. 2011a. February;120(1):71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sadeh N, Verona E. Visual complexity attenuates emotional processing in psychopathy: Implications for fear-potentiated startle deficits. Cognitive, Affective, & Behavioral Neuroscience. 2012. June 1;12(2):346–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Casey H, Rogers RD, Burns T, Yiend J. Emotion regulation in psychopathy. Biological psychology. 2013. March 1;92(3):541–8. 10.1016/j.biopsycho.2012.06.011 [DOI] [PubMed] [Google Scholar]
- 66.Verona E, Sprague J, Sadeh N. Inhibitory control and negative emotional processing in psychopathy and antisocial personality disorder. Journal of abnormal psychology. 2012. May;121(2):498 10.1037/a0025308 [DOI] [PubMed] [Google Scholar]
- 67.Baskin-Sommers AR, Curtin JJ, Newman JP. Specifying the attentional selection that moderates the fearlessness of psychopathic offenders. Psychological Science. 2011b. February;22(2):226–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tillem S, Ryan J, Wu J, Crowley MJ, Mayes LC, Baskin-Sommers A. Theta phase coherence in affective picture processing reveals dysfunctional sensory integration in psychopathic offenders. Biological psychology. 2016. September 1;119:42–5. 10.1016/j.biopsycho.2016.06.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Smith SF, Lilienfeld SO. The response modulation hypothesis of psychopathy: A meta-analytic and narrative analysis. Psychological bulletin. 2015. November;141(6):1145 10.1037/bul0000024 [DOI] [PubMed] [Google Scholar]
- 70.Fowles DC, Dindo L. A dual-deficit model of psychopathy. Handbook of psychopathy. 2006:14–34. [Google Scholar]
- 71.Patrick CJ, Bernat EM. Neurobiology of psychopathy: A two process theory. Handbook of neuroscience for the behavioural sciences. 2009: 1110–1131. [Google Scholar]
- 72.Grillon C. Startle reactivity and anxiety disorders: aversive conditioning, context, and neurobiology. Biological psychiatry. 2002. November 15;52(10):958–75. 10.1016/s0006-3223(02)01665-7 [DOI] [PubMed] [Google Scholar]
- 73.Decety J, Chen C, Harenski C, Kiehl KA. An fMRI study of affective perspective taking in individuals with psychopathy: imagining another in pain does not evoke empathy. Frontiers in human neuroscience. 2013. September 24;7:489 10.3389/fnhum.2013.00489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Boccardi M, Frisoni GB, Hare RD, Cavedo E, Najt P, Pievani M, et al. Cortex and amygdala morphology in psychopathy. Psychiatry Research: Neuroimaging. 2011. August 30;193(2):85–92. 10.1016/j.pscychresns.2010.12.013 [DOI] [PubMed] [Google Scholar]
- 75.Blair RJ. Neuroimaging of psychopathy and antisocial behavior: a targeted review. Current psychiatry reports. 2010. February 1;12(1):76–82. 10.1007/s11920-009-0086-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Blair RJ. Psychopathy, frustration, and reactive aggression: the role of ventromedial prefrontal cortex. British journal of psychology. 2010. August 1;101(3):383–99. [DOI] [PubMed] [Google Scholar]
- 77.Anderson NE, Kiehl KA. The psychopath magnetized: insights from brain imaging. Trends in cognitive sciences. 2012. January 1;16(1):52–60. 10.1016/j.tics.2011.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Decety J, Skelly L, Yoder KJ, Kiehl KA. Neural processing of dynamic emotional facial expressions in psychopaths. Social neuroscience. 2014. January 2;9(1):36–49. 10.1080/17470919.2013.866905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Öhman A. Of snakes and faces: An evolutionary perspective on the psychology of fear. Scandinavian journal of psychology. 2009. December 1;50(6):543–52. 10.1111/j.1467-9450.2009.00784.x [DOI] [PubMed] [Google Scholar]
- 80.Sylvers PD, Brennan PA, Lilienfeld SO. Psychopathic traits and preattentive threat processing in children: a novel test of the fearlessness hypothesis. Psychological Science. 2011. October;22(10):1280–7 10.1177/0956797611420730 [DOI] [PubMed] [Google Scholar]
- 81.Viding E, Sebastian CL, Dadds MR, Lockwood PL, Cecil CA, De Brito SA, et al. Amygdala response to preattentive masked fear in children with conduct problems: the role of callous-unemotional traits. American journal of psychiatry. 2012. October;169(10):1109–16. 10.1176/appi.ajp.2012.12020191 [DOI] [PubMed] [Google Scholar]
- 82.Salekin RT, Worley C, Grimes RD. Treatment of psychopathy: A review and brief introduction to the mental model approach for psychopathy. Behavioral Sciences & the Law. 2010. March 1;28(2):235–66. [DOI] [PubMed] [Google Scholar]
- 83.O'Neil ML, Lidz V, Heilbrun K. Adolescents with psychopathic characteristics in a substance abusing cohort: Treatment process and outcomes. Law and human behavior. 2003. June;27(3):299 [DOI] [PubMed] [Google Scholar]
- 84.Olver ME, Lewis K, Wong SC. Risk reduction treatment of high-risk psychopathic offenders: The relationship of psychopathy and treatment change to violent recidivism. Personality Disorders: Theory, Research, and Treatment. 2013. April;4(2):160. [DOI] [PubMed] [Google Scholar]
- 85.Baskin-Sommers AR, Newman JP. Differentiating the cognition-emotion interactions that characterize psychopathy versus externalizing. Handbook of cognition and emotion. 2013:501–20. [Google Scholar]
- 86.Brook M, Kosson DS. Impaired cognitive empathy in criminal psychopathy: Evidence from a laboratory measure of empathic accuracy. Journal of abnormal psychology. 2013. February;122(1):156 10.1037/a0030261 [DOI] [PubMed] [Google Scholar]
- 87.Ermer E, Kahn RE, Salovey P, Kiehl KA. Emotional intelligence in incarcerated men with psychopathic traits. Journal of personality and social psychology. 2012. July;103(1):194 10.1037/a0027328 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(PDF)
(PDF)
(PDF)
(TIF)
(TIF)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.