Abstract
Modifications in the structure of pharynx following adenotonsillectomy are presumed to cause changes in the voice characteristics of patients. Data on effect of tonsillectomy/adenotonsillectomy on changes in voice among Indian children are sparse. This study was thus conducted to study the effect of adenotonsillectomy/tonsillectomy on childrens’ voice. It was a prospective observational study of children aged 4–15 years undergoing tonsillectomy with or without adenoidectomy. Measures of voice were noted preoperatively, 1 and 3 months post-operatively. Subjective evaluation was done using Paediatric Voice Outcome Survey (PVOS) questionnaire administered to participants’ parents. Objective evaluation was done by recording and analyzing using PRAAT voice analysis software which is an open-software tool. Statistical analysis was done using the statistical software SPSS 17.0 version. There were 31 children between 4 and 14 years of age 65% being male. Adenotonsillectomy was done in 83.5%. There was statistically significant difference in the subjective scores (PVOS) pre-operatively and 3 month postoperative score (p value = 0.001). However, there was no statistically significant difference between any other pre op and post op parameters. Though the only significant post tonsillectomy voice changes noted was subjective by parents 3 months later, it does raise concern whether this could be a reality and not a myth. Further studies with larger number of patients, including involving the subjective evaluation (PVOS) by another person in addition to patients’ parent need to be undertaken to address this issue.
Electronic supplementary material
The online version of this article (10.1007/s12070-018-1412-6) contains supplementary material, which is available to authorized users.
Keywords: Voice, PVOS, Adenotonsillectomy, Nasal resonance
Introduction
Adenotonsillectomy is one of the most commonly performed surgical procedures in the field of Otolaryngology, being performed for recurrent tonsillitis, recurrent peritonsillar abscess sleep disordered breathing, obstructive sleep apnoea, and asymmetrical enlarged tonsils (to rule out neoplasm/granulomata) [1, 2].
Change in voice is a concern which many patients and parents have when surgical details of tonsillectomy are being explained. Hypertrophied tonsils are assumed to obstruct transmission of sound into the oral and nasal cavities, thus altering the resonance of the voice [3]. So following surgery, it has been hypothesized that with the changes in the dimensions of the resonating chamber of the vocal tract which extends from the glottis to the lips, there could be a change in voice after tonsillectomy or adenotonsillectomy [4]. However, the data on the effect of tonsillectomy or adenotonsillectomy on changes in voice among the Indian children is yet to be reported. This prospective study was thus undertaken to evaluate the impact of tonsillectomy or adenotonsillectomy on voice of these children.
Materials and Methods
This prospective observational study was conducted in the department of Otorhinolaryngology, Christian Medical College, and Vellore after approval of the institutional review board. Children between 4 and 15 years scheduled to undergo tonsillectomy or adenotonsillectomy, whose parents provided consent for being included in the study and willing for follow up after 1 and 3 months after surgery were included in the study.
A detailed ear, nose, and throat examination done in study subjects revealed no other abnormality. Brodsky grading of tonsils (Fig. 1) was performed [5]. The outcome measures were done subjectively and objectively. Paediatric Voice Outcome Survey (PVOS) questionnaire for subjective assessment of the child’s voice was administered to the parents of the participants for baseline measures which was repeated after 1 and 3 months following surgery. PVOS was first developed and validated by Hartnick in 2002, is a convenient, 4-question parent-proxy instrument to measure voice-related quality of life in children and adolescents. Raw score of PVOS is first obtained. The score is measured on a scale from 0 to 100, with a low score representing worse voice-related quality of life [6]. For the objective voice analysis study subjects’ voice was recorded for sustained phonation of vowel/a/in a sound treated room (ambient noise less than 40 dB) and analysed using PRAAT voice analysis software (version 5.1.04). PRAAT is an open-software tool for speech signal edition and labeling, as well as for various acoustic analyses (spectral, formant, pitch, intensity) [7]. The following parameters of voice were estimated: Fundamental frequency, jitter percent shimmer percent, Harmonics to noise ratio (HNR) and the centre frequencies of formant 1–4 (F1, F2, F3, F4). F1 is the result of the back cavity resonance and that F2 is the result of the front cavity resonance. The higher formants –F3 and F4 reflect speaker’s characteristics (voice quality). Formant frequency (F1, F2 F3 and F4)—Midpoint of the visible dark bands of energy appropriate to the first four vowel resonances. Formants on spectrograms occur around frequencies that correspond to the resonances of the vocal tract [8]. Mean and standard deviation of the above parameters were calculated. In our study we used the formant frequencies to assess resonance.
Fig. 1.
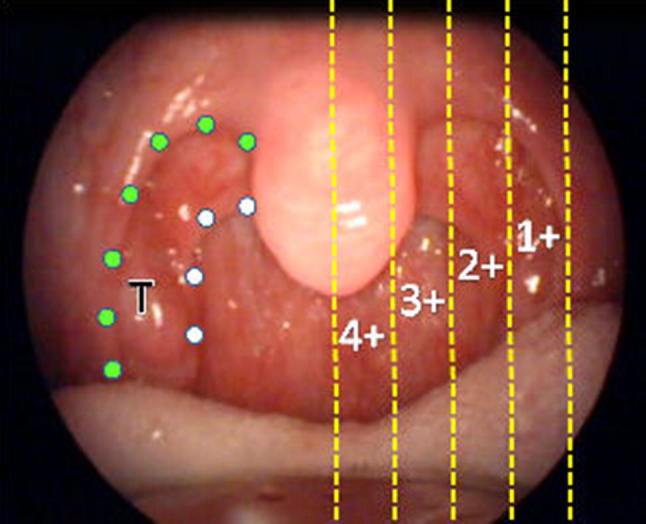
Brodsky grading of tonsil
Statistical Analysis
Statistical analysis was done using the statistical software SPSS 17.0 version. The frequencies and descriptive statistics such as mean and standard deviation (SD) were calculated to describe the normal data and median and inter quartile range (IQR) were used to describe the skewed data. The sample size was calculated based on a similar study done by Salami et al. [9]. Paired t test and Wilcoxon signed rank test were used for the comparison of the pre–post operative values. Independent samples t test, Mann–Whitney U test and Kruskall Wallis H test were used for between group comparisons. The association between the demographic and clinical variables and outcome measure categories was done with χ2 test and represented graphically with a clustered bar chart. A p value < 0.05 was considered as statistically significant.
Results
Parents of 50 children scheduled for tonsillectomy or adenotonsillectomy consented for their children to be enrolled in the study and 31 children who completed both follow up visits were included in the data analysis.
Baseline Characteristics
The age of children ranged from 4 to 14 years with a mean (SD) of 8.3(2.9) years. Of the 31 children, 20(65%) were males and 11(35%) were females. 29 (83.5%) subjects of our study group underwent adenotonsillectomy and 2 (6.5%) children underwent only tonsillectomy.
As our study had only 2 patients who underwent tonsillectomy alone, they were not independently studied.
Size of Tonsils and Adenoids [10]
The size of tonsils ranged from grade 2–4, with 71% (n = 22) of children having grade 3 tonsils. The size of the adenoids (assessed from the X-ray Nasopharynx lateral view) ranged from grades of 1–4 with 45 and 36% of children having grade 2 and 3 adenoids respectively (Table 1).
Table 1.
Frequency table of size of tonsils and adenoids
| n (%) | |
|---|---|
| Grade of tonsils | |
| 1 | 0 (0) |
| 2 | 6 (19.4) |
| 3 | 22 (71) |
| 4 | 3 (9.7) |
| Grade of adenoids | |
| 1 | 2 (7) |
| 2 | 14 (45) |
| 3 | 11 (36) |
| 4 | 4 (13) |
PVOS Analysis
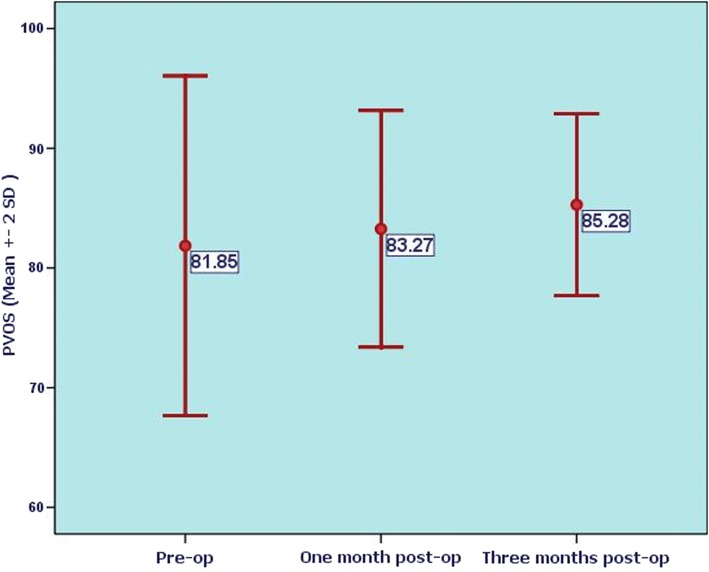
The mean (SD) pre-op scores of PVOS were 81.85(7.1) and post op PVOS scores 1 month after surgery was 83.27(4.94) and this difference was not statistically significant (p = 0.090). However, 3 months after surgery the mean and SD scores were 85.28(3.80) and this difference was significant when compared to the scores prior to surgery (p = 0.001) (Figs. 2, 3). The pre- and post operative PVOS scores did not have a significant change when compared to the grade of the tonsils (p = NS).
Fig. 2.
Comparison of PVOS scores preop, one month and 3 months after surgery
Fig. 3.
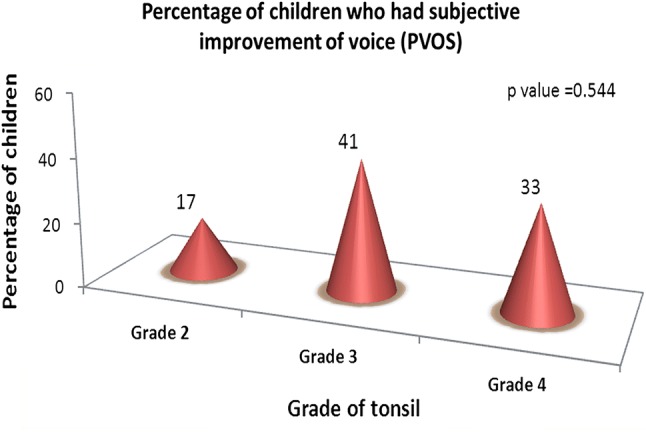
Percentage of children who had subjective improvement of voice (PVOS)
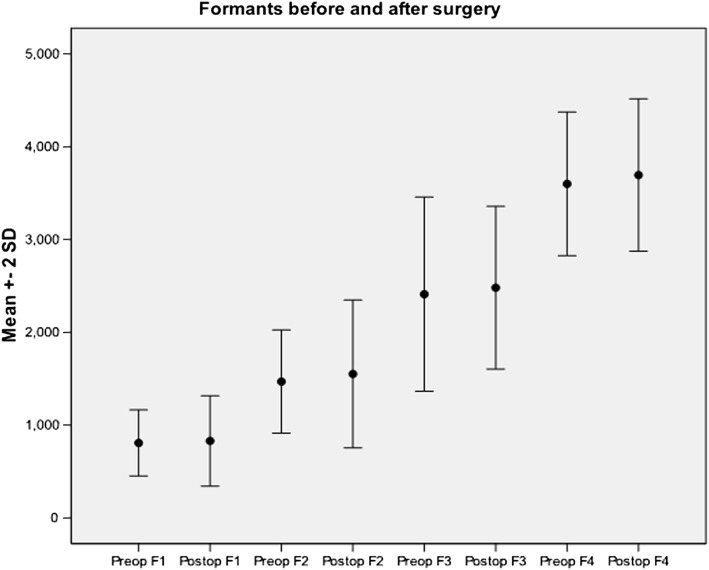
Voice Analysis
In this study, there was no statistically significant difference between the pre- and post operative analysis of any of the voice parameters (Table 2). The pre and post op formant frequency values that were checked to assess resonance were also found to be not significant (Fig. 4).
Table 2.
Comparison of voice parameters before and after surgery
| Voice parameter | Pre op value | Post op value (1 month follow up) | p value | Post op (3 months after follow up) | p value |
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | |||
| Fundamental frequency | 260.03 (58.94) | 255.97 (52.96) | 0.677 | 262.67 (50.86) | 0.802 |
| Jitter | 0.65 (0.50) | 0.70 (0.72) | 0.772 | 0.66 (0.48) | 0.967 |
| Shimmer | 5.89 (4.50) | 5.74 (4.99) | 0.846 | 4.46 (4.57) | 0.172 |
| Harmonics to noise ratio | 14.81 (6.32) | 16.21 (5.77) | 0.361 | 14.72 (6.13) | 0.950 |
| Formants | |||||
| F1 | 815.37 (190.26) | 805.15 (250.43) | 0.849 | 836.72 (197.47) | 0.591 |
| F2 | 1501.38 (303.30) | 1521.22 (412.37) | 0.875 | 1604.83 (327.44) | 0.152 |
| F3 | 2448.62 (519.40) | 2451.93 (451.85) | 0.821 | 2625.76 (466.87) | 0.223 |
| F4 | 3658.97 (375.12) | 3685.54 (419.95) | 0.535 | 3725.76 (335.76) | 0.501 |
Fig. 4.
Formants before and after surgery
Discussion
Adenotonsillectomy is the most common surgery performed by otolaryngologists in pediatric age. Parents and caregivers of these children often ask whether there could be a change in their voice following surgery. Hypertrophied tonsils decrease the oropharyngeal airway pushing the tongue anteriorly resulting in hypernasal speech, mouth breathing and an unclear voice. Enlarged adenoids or tonsils often decrease nasal airflow resulting in hyponasal or muffled speech, whereas hypernasal speech may occur rarely due to velopharyngeal insufficiency (VPI) resulting from tonsil enlargement [11].The human voice production is made possible by the lungs, the vocal folds within the larynx, and the resonating chamber. The lung must produce adequate airflow and air pressure to vibrate the vocal folds. The oral and nasal resonating cavities filter the sound emanating from the larynx and can interact with the laryngeal airflow to strengthen it or weaken it. Thus modifications in the structure of the vocal tract after tonsillectomy or adenotonsillectomy are presumed to cause changes in the voice characteristics of patients [4].
In a study conducted by Yasan et al. [12] in which the volume of the palatine tonsil was assessed, they noted there was as much enlargement in the lateral, inferior and superior directions as the medial direction. However in our study, the pre- and post operative PVOS scores of our patients did not have a significant change when compared to the grade of the tonsils.
In our study, the Paediatric Voice Outcome Score (PVOS) questionnaire did show a subjective improvement of the voice noticed by the parents at 3 months after surgery which was statistically significant. This was in contrast to report by Chuma et al. [10] who did not find any noticeable voice change postoperatively by means of the Buffalo Voice profile, interviews and questionnaires of the parents. They had concluded that changes in voice following tonsillectomy or adenotonsillectomy were not obvious and not detected perceptually. However, it is also important to recognize that in people who use their voices professionally, small changes in voice characteristics may have a significant effect psychologically and professionally. This possibility should be considered while planning for a tonsillectomy/adenotonsillectomy and appropriate counseling rendered to the patient [13, 14].
In our study none of the parameters of voice (fundamental frequency, jitter percent, shimmer percent, Harmonics-to-noise ratio (HNR) and the centre frequencies of formant 1–4 (F1, F2, F3, F4) which were analyzed had any significant change following adenotonsillectomy. The voice parameters assessed in this study to estimate laryngeal behavior showed that there was no significant change in the fundamental frequency also after surgery. This is expected because tonsillectomy and adenotonsillectomy are surgeries that don’t affect the larynx directly and hence should not affect the rate at which vocal cords open or close during sustained phonation. However Salami et al. [9] reported significant change in the fundamental frequency postoperatively. Chuma et al. [10] in their study assessed voice change 3 months post-operatively and reported no significant changes. He suggested that removal of soft tissue from the oropharyngeal region had no significant effect on the perceptual and vocal parameters. Our findings regarding objective voice analysis are similar to the findings in few studies that no significant change noted after adenotonsillectomy [12, 15]. Dimatos et al. [16] on the contrary did reported transient changes in acoustic parameters in post adenotonsillectomy children, which normalized in the 3rd postoperative month.
Limitations
Our study was performed on a small sample size with a postoperative follow up period of 1 and 3 months. A larger sample size with a follow up period of 6 months to a year would be required to conclusively establish the relationship between adenotonsillectomy and change in voice. Though resonance was assessed using formant frequency, nasalence was not separately evaluated for effects of adenoidectomy in this procedure.
Conclusions
Our study revealed statistically significant subjective post tonsillectomy voice change in children 3 months after surgery as documented by parents with no other significant subjective changes at 1 month and no objective changes at either 1 and 3 months. Subjective tests are perceptual and qualitative. This observation necessitates subjective evaluation of PVOS of another person in addition to the patients’ parents. A larger sample size and post op follow up with both subjective and objective evaluation for a longer period (6 months to a year) is also suggested to enable otolaryngologists to give an evidenced based answer to this frequently asked question ‘Is there voice change after adenoid and tonsil surgery?’
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to acknowledge and thank Dr. Mary Kurien, Head of ENT department of Pondicherry Institute of Medical Sciences for her critical review of this journal and input.
Compliance with ethical standards
Conflict of interest
The authors declares that they have no conflict of interests.
References
- 1.Ramos SD, Mukerji S, Pine HS. Tonsillectomy and adenoidectomy. Pediatr Clin North Am. 2013;60(4):793–807. doi: 10.1016/j.pcl.2013.04.015. [DOI] [PubMed] [Google Scholar]
- 2.Baugh RF, Archer SM, Mitchell RB, Rosenfeld RM, Amin R, Burns JJ, et al. Clinical practice guideline: tonsillectomy in children. Otolaryngol-Head Neck Surg Off J Am Acad Otolaryngol-Head Neck Surg. 2011;144(1 Suppl):S1–S30. doi: 10.1177/0194599810389949. [DOI] [PubMed] [Google Scholar]
- 3.Kummer AW, Billmire DA, Myer CM., 3rd Hypertrophic tonsils: the effect on resonance and velopharyngeal closure. Plast Reconstr Surg. 1993;91(4):608–611. doi: 10.1097/00006534-199304000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Ilk HG, Eroğul O, Satar B, Ozkaptan Y. Effects of tonsillectomy on speech spectrum. J Voice Off J Voice Found. 2002;16(4):580–586. doi: 10.1016/S0892-1997(02)00133-9. [DOI] [PubMed] [Google Scholar]
- 5.Ng SK, Lee DLY, Li AM, Wing YK, Tong MCF. Reproducibility of clinical grading of tonsillar size. Arch Otolaryngol Head Neck Surg. 2010;136(2):159–162. doi: 10.1001/archoto.2009.170. [DOI] [PubMed] [Google Scholar]
- 6.Hartnick CJ. Validation of a pediatric voice quality-of-life instrument: the pediatric voice outcome survey. Arch Otolaryngol Head Neck Surg. 2002;128(8):919–922. doi: 10.1001/archotol.128.8.919. [DOI] [PubMed] [Google Scholar]
- 7.Sundberg J. Formant structure and articulation of spoken and sung vowels. Folia Phoniatrica (Basel) 1970;22(1):28–48. doi: 10.1159/000263365. [DOI] [PubMed] [Google Scholar]
- 8.Saida H, Hirose H. Acoustic changes in voice after tonsillectomy. Acta Oto-Laryngol Suppl. 1996;523:239–241. [PubMed] [Google Scholar]
- 9.Salami A, Jankowska B, Dellepiane M, Crippa B, Mora R. The impact of tonsillectomy with or without adenoidectomy on speech and voice. Int J Pediatr Otorhinolaryngol. 2008;72(9):1377–1384. doi: 10.1016/j.ijporl.2008.05.019. [DOI] [PubMed] [Google Scholar]
- 10.Chuma AV, Cacace AT, Rosen R, Feustel P, Koltaii PJ. Effects of tonsillectomy and/or adenoidectomy on vocal function: laryngeal, supralaryngeal and perceptual characteristics. Int J Pediatr Otorhinolaryngol. 1999;47(1):1–9. doi: 10.1016/S0165-5876(98)00162-1. [DOI] [PubMed] [Google Scholar]
- 11.Darrow DH, Siemens C. Indications for tonsillectomy and adenoidectomy. The Laryngoscope. 2002;112(8 Pt 2 Suppl 100):6–10. doi: 10.1097/00005537-200208001-00004. [DOI] [PubMed] [Google Scholar]
- 12.Yasan H, Aynali G, Erdoğan O, Yariktaş M. Does subjective tonsillar grading reflect the real volume of palatine tonsils? Int J Pediatr Otorhinolaryngol. 2011;75(5):618–619. doi: 10.1016/j.ijporl.2011.01.030. [DOI] [PubMed] [Google Scholar]
- 13.Spiegel JR, Sataloff RT, Emerich KA. The young adult voice. J Voice Off J Voice Found. 1997;11(2):138–143. doi: 10.1016/S0892-1997(97)80069-0. [DOI] [PubMed] [Google Scholar]
- 14.Hori Y, Koike Y, Ohyama G, Otsu SY, Abe K. Effects of tonsillectomy on articulation. Acta Oto-Laryngol Suppl. 1996;523:248–251. [PubMed] [Google Scholar]
- 15.Liu X, Zheng Y, Tian P, Yang J, Zou H. The impact of tonsillectomy with or without adenoidectomy on voice: acoustic and aerodynamic assessments. J Voice Off J Voice Found. 2015;29(3):346–348. doi: 10.1016/j.jvoice.2014.08.014. [DOI] [PubMed] [Google Scholar]
- 16.Dimatos SC, Neves LR, Beltrame JM, Azevedo RR, Pignatari SSN. Impact of adenotonsillectomy on vocal emission in children. Braz J Otorhinolaryngol. 2016;82(2):151–158. doi: 10.1016/j.bjorl.2015.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.