Abstract
IMPORTANCE
Hip osteoarthritis (OA) is a common cause of pain and disability.
OBJECTIVE
To identify the clinical findings that are most strongly associated with hip OA.
DATA SOURCES
Systematic search of MEDLINE, PubMed, EMBASE, and CINAHL from inception until November 2019.
STUDY SELECTION
Included studies (1) quantified the accuracy of clinical findings (history, physical examination, or simple tests) and (2) used plain radiographs as the reference standard for diagnosing hip OA.
DATA EXTRACTION AND SYNTHESIS
Studies were assigned levels of evidence using the Rational Clinical Examination scale and assessed for risk of bias using the Quality Assessment of Diagnostic Accuracy Studies tool. Data were extracted using individual hips as the unit of analysis and only pooled when findings were reported in 3 or more studies.
MAIN OUTCOMES AND MEASURES
Sensitivity, specificity, and likelihood ratios (LRs).
RESULTS
Six studies were included, with data from 1110 patients and 1324 hips, of which 509 (38%) showed radiographic evidence of OA. Among patients presenting to primary care physicians with hip or groin pain, the affected hip showed radiographic evidence of OA in 34% of cases. A family history of OA, personal history of knee OA, or pain on climbing stairs or walking up slopes all had LRs of 2.1 (sensitivity range, 33%−68%; specificity range, 68%−84%; broadest LR range: 95% CI, 1.1–3.8). To identify patients most likely to have OA, the most useful findings were squat causing posterior pain (sensitivity, 24%; specificity, 96%; LR, 6.1 [95% CI, 1.3–29]), groin pain on passive abduction or adduction (sensitivity, 33%; specificity, 94%; LR, 5.7 [95% CI, 1.6–20]), abductor weakness (sensitivity, 44%; specificity, 90%; LR, 4.5 [95% CI, 2.4–8.4]), and decreased passive hip adduction (sensitivity, 80%; specificity, 81%; LR, 4.2 [95% CI, 3.0–6.0]) or internal rotation (sensitivity, 66%; specificity, 79%; LR, 3.2 [95% CI, 1.7–6.0]) as measured by a goniometer or compared with the contralateral leg. The presence of normal passive hip adduction was most useful for suggesting the absence of OA (negative LR, 0.25 [95% CI, 0.11–0.54]).
CONCLUSIONS AND RELEVANCE
Simple tests of hip motion and observing for pain during that motion were helpful in distinguishing patients most likely to have OA on plain radiography from those who will not. A combination of findings efficiently detects those most likely to have severe hip OA.
Clinical Scenarios
In the following cases, the clinician wants to determine whether the patient’s symptoms are caused by hip osteoarthritis (OA).
Case 1
A58-year-old woman was experiencing pain in her right groin, which had not changed over the last 6 months. She is a school teacher and the pain was worse on climbing up staircases, which made it difficult for her to get to her classroom. You do not have a goniometer for precise range-of-motion measurement but, compared with the left side, the right hip had decreased passive hip adduction and internal rotation.
Case 2
A 60-year-old man presented to his primary care clinician with a 9-month history of left hip pain, which had remained stable until it worsened over the last 3 weeks and was exacerbated by walking. There was no pain on internal rotation and passive movements on clinical examination were not different to the right side.
Background
OA is a disabling disease that affects multiple components of joints, including articular cartilage, subchondralbone, and the synovial joint lining. OA commonly affects the hips and knees.1 The prevalence of symptomatic hip OA among people aged 60 years and older is 6.2%.2 Population studies suggest that hip OA is twice as common in women as in men, and there is evidence to suggest a strong heritable component.3 Obesity, injury, malalignment, and anatomical abnormalities have also been associated with onset and progression of lower limb OA, possibly due to increased or altered load across articular surfaces.1The pain and restricted motion of hip OA can be debilitating but there is good evidence of benefit for a range of interventions, including weight loss, physiotherapy that includes strengthening of periarticular muscles, intra-articular injections, and total hip replacement.3
The main symptom of hip OA is pain (Figure 1).3–5 A number of structures around the hip are richly innervated by sensory nerve fibers, including the periosteum,6 subchondral bone,6 synovium,7 and surrounding soft tissues. Chronic joint pain is also associated with central sensitization at the spinal and cortical levels, which can lead to referred pain and even tenderness remote from the affected joint.8,9 Long-standing hip OA may also affect gait and so lead to secondary symptoms such as pain in the knees and lumbar spine.10,11
Figure 1.
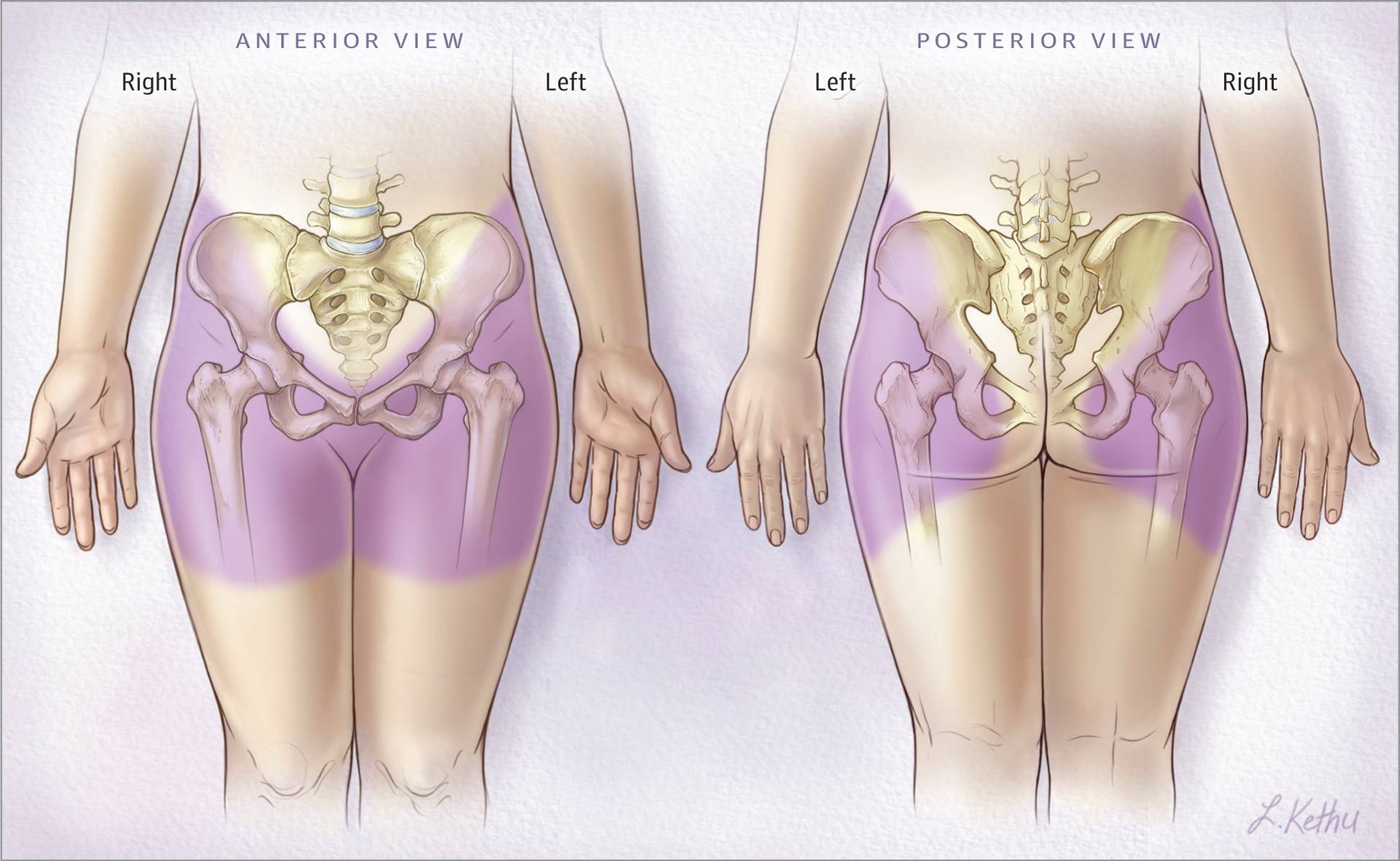
Distribution of Pain Typically Arising From Hip Osteoarthritis
Why Is This an Important Question to Answer With a Clinical Evaluation?
The differential diagnosis of hip pain includes greater trochanteric pain syndrome, piriformis syndrome, stress fracture, inflammatory arthropathies (eg, rheumatoid arthritis), lumbar radiculopathy, pelvis bone tumors, osteonecrosis, pelvic insufficiency fractures, and meralgia parasthetica.3,12 Nonmusculoskeletal conditions (eg, groin hernia, intrapelvic pathology, and leaking abdominal aortic aneurysms) may also present with hip and/or groin pain.13
Plain radiographs are the most commonly used method for diagnosing hip OA.3 This modality does not directly visualize articular cartilage but can reveal features of disease, such as joint space narrowing, osteophytes, subchondral sclerosis, and subchondral cysts,14 as well as excluding alternative causes of pain.14 Although an anterior-posterior pelvis radiograph is inexpensive and simple, intra-articular hip pathology can sometimes be diagnosed by clinical examination alone (Figure 2).3,15 Early radiographs may only be needed when the diagnosis is uncertain or requires confirmation before invasive treatments are undertaken. The evidence-based UK National Institute for Health and Care Excellence recommends diagnosing OA without imaging in persons aged older than 45 years with activity-related joint pain and without prolonged (≥30 minutes) morning stiffness.15 Prolonged morning stiffness may point toward an inflammatory cause for pain such as rheumatoid arthritis.16
Figure 2.
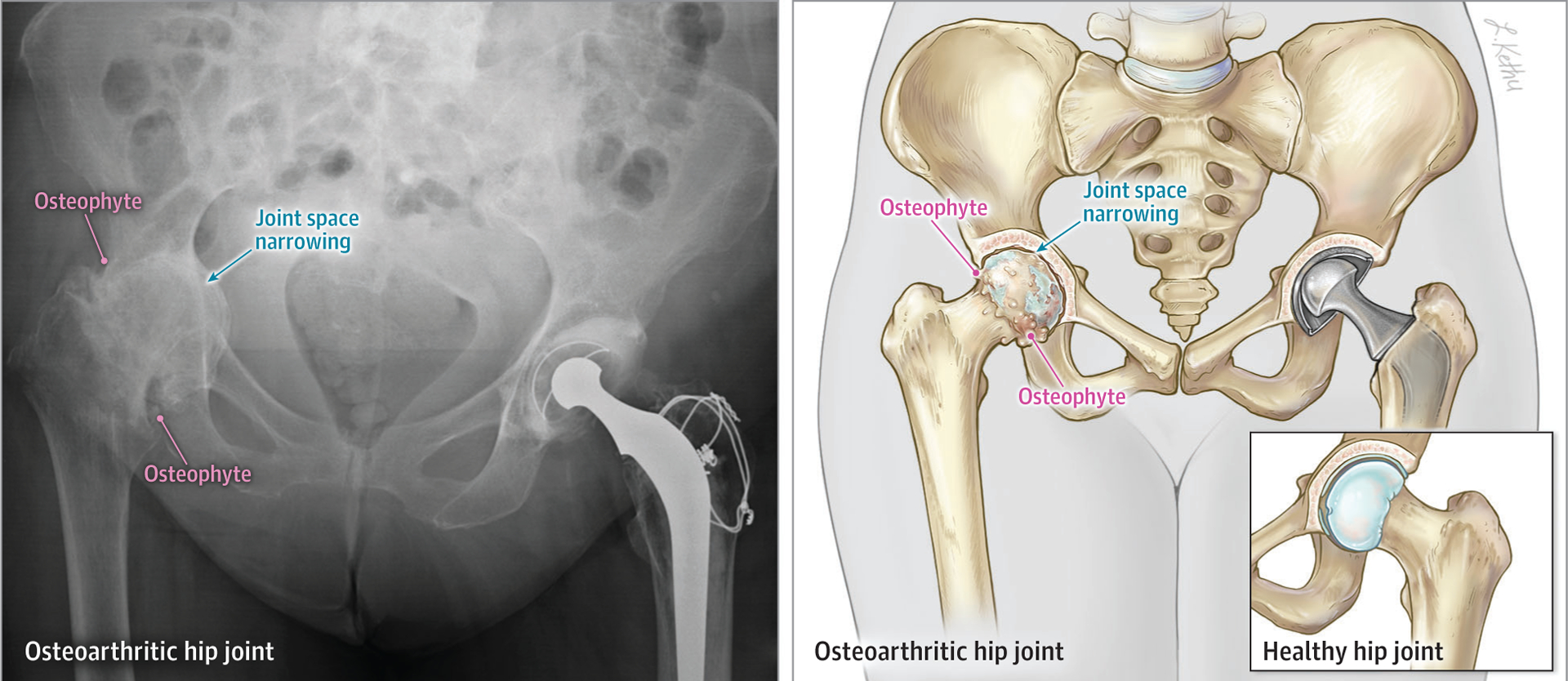
A Plain Radiograph and Illustration Showing Features of Right Hip Osteoarthritis
Radiographic hip OA is common in the general population and is often asymptomatic: the presence of x-ray findings suggestive of hip OA does not always correlate with symptoms. One large population cohort study reported that only 21% of patients with radiographic hip OA experienced pain.17 Therefore, it is particularly important to establish a pretest probability before ordering radiographs. Inadequate clinical assessment risks overdiagnosis of hip OA in patients with symptoms attributable to another cause (eg, lumbar radiculopathy) but with incidental radiographic findings. Such patients might undergo unnecessary treatment that would not improve their symptoms.
We conducted a systematic review to evaluate the diagnostic accuracy of clinical findings in determining the prevalence of radiographic OA among those presenting to primary care clinicians with hip or groin pain and the likelihood of hip OA based on symptoms and signs.
Methods
Search Strategy
Literature searches (eTable 1 in the Supplement) were performed by a specialist information librarian using PubMed, Ovid MEDLINE (1946 to November 2019), Embase (1974 to November 2019), and EBSCO CINAHL (1982 to November 2019). Further items were sought from the reference lists of previous studies and review articles. Once duplicates were removed, all unique database items were downloaded into specialist software for screening abstracts (Rayyan, Qatar Computing Research Institute).
Study Selection
We included all studies that described clinical finding sin patients with hip or groin pain and used plain radiographs as a diagnostic standard. It was also necessary for researchers to prespecify the criteria used to identify patients with radiographic hip OA. Studies were excluded if they were not designed in such a way (eg, uncontrolled case series) that they could determine sensitivity and specificity of clinical findings for abnormalities on plain radiographs. Titles and abstracts were independently screened by 2 authors (D.M. and H.A.C.). If either author promoted an item to the next stage, full texts were retrieved and screened at a single sitting, with disagreements resolved by consensus.
Data Extraction and Quality Assessment
Two authors extracted data from included studies (D.M. and H.A.C.), which were then independently checked by a third author (D.C.P.). Original data were sought from corresponding authors of studies where appropriate. Study quality was summarized using a checklist designed for the Rational Clinical Examination series.18 Level 1 studies require that clinical findings be assessed and categorized independently of the radiographic findings in 200 or more consecutive patients; level 2 studies have the same requirement but include fewer than 200 patients; and level 3 studies include nonconsecutive patients. We excluded level 4 and level 5 studies because they use nonindependent assessment of predictors and outcomes.
The Quality Assessment of Diagnostic Accuracy Studies 2 (QUADAS-2) criteria19 were used to assess individual included studies for risk of bias. This process was undertaken by 2 authors (DM and HAC) and disagreements resolved by a third author (DCP). For included studies, we recorded the study design, setting, population, age of patients, radiographic criteria for defining hip OA, diagnostic accuracy, and whether the denominator for measures of accuracy (sensitivity and specificity) was based on unique patients or number of hips examined. When authors presented data for “any OA” and “severe OA,” these were extracted and separately analyzed. We pragmatically accepted diagnoses of hip OA based on any radiographic criteria prespecified by study authors. “Severe OA” was defined by the 2 studies that reported patients in this category as hips with radiographic joint space less than or equal to 1.5 mm.20,21
Statistical Methods
Sensitivity, specificity, and likelihood ratios (LRs) were calculated using data extracted from each study together with their 95% CIs. The unit of analysis was individual hips. The positive LR is defined as the ratio between probability of a positive clinical finding when the disease is present and the probability of a positive finding when the disease is absent (LR = sensitivity/[1-specificity]). The negative LR (LR–) is the ratio between the probability of a negative clinical finding when the disease is present and the probability of a negative finding when the disease is absent (LR– = [1-sensitivity]/specificity).22
Clinical tests reported by only 1 study were presented as individual data points. Those reported by 2 studies were presented as ranges. Data for clinical tests reported by 3 studies were pooled using univariate random-effects models and data reported by more than 4 studies were pooled by fitting a multilevel mixed-effects logistic regression model. All analyses were undertaken using StataSE version 15 (StataCorp) together with its metan23 and metandi24 modules.
We highlighted features with a point estimate positive LR of greater than or equal to 2.0 or a negative LR of less than 0.5, and a confidence interval that excludes 1.0, as being most likely to be useful in routine clinical practice.25 Given an initial pretest probability of 10%, the presence of a feature with a positive LR of 2.0 would increase the probability to 18%. The absence of a feature with a negative LR of 0.5 would conversely reduce a pretest probability of 10% to 5.3%.
Results
There were 2985 unique items retrieved by the online database search, which were reduced to 6 studies by the screening process (Figure 3). The 6 included studies reported data from 1110 patients and 1324 hips, 509 (38%) of which were found to have radiographic evidence of OA (eTable 2 in the Supplement). There were 5 prospective cohort studies and 1 case-control study. Five studies were judged to be Rational Clinical Examination25 level 1,none were level2, and 1 was level 3 (eTable 3 in the Supplement).
Figure 3.
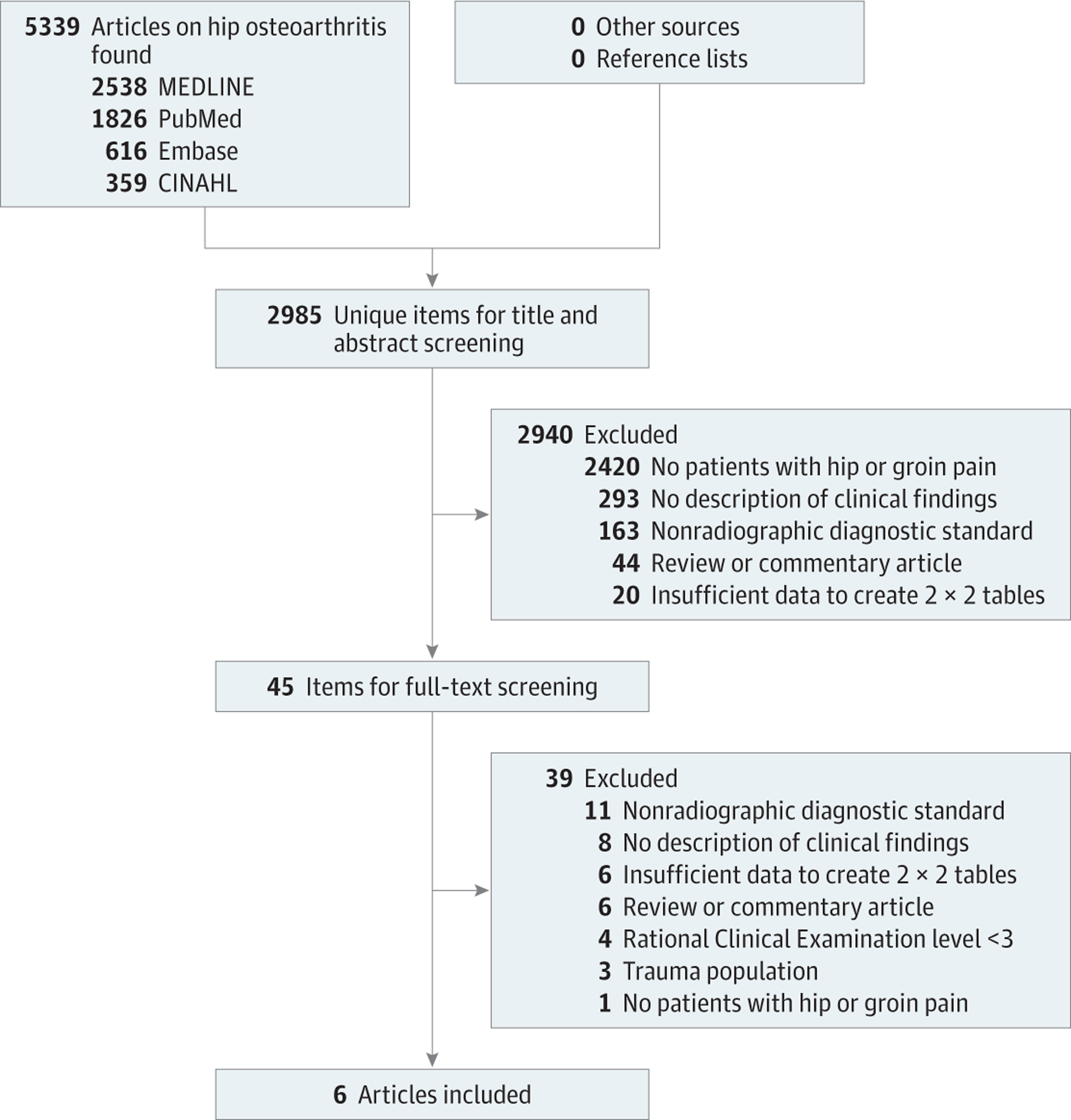
Flow Diagram Showing Inclusion and Exclusion of Studies
Prevalence
The population prevalence of symptomatic hip OA in those aged older than 60 years is around 6.2%.2 Two consistent studies included in this review found that, among patients presenting to a primary care practitioner (mean age, 63–66 years) with hip and/or groin pain, just over a third (34%–35%) had at least mild to moderate OA and 11% to 14% had severe OA.20,21
Risk Factors and Symptoms
Four studies4,20,26,27 evaluated features in the patient history (Table 1). Three findings were associated with the presence of hip OA: a family history of OA (sensitivity, 34%; specificity, 84%; LR, 2.1 [95% CI, 1.2–3.6]), a personal history of knee OA (sensitivity, 33%; specificity, 84%; LR, 2.1 [95% CI, 1.1–3.8]), and pain on climbing stairs or walking down slopes (sensitivity, 68%; specificity, 68%; LR, 2.1 [95% CI, 1.6–2.8]). While the worst pain located in the medial thigh was infrequently found (2.7% of patients), this location of the worst pain had the highest LR (sensitivity, 12%; specificity, 98%; LR, 7.8 [95% CI, 1.7–37]).
Table 1.
History Findings and Likelihood of Hip Osteoarthritis With Positive Likelihood Ratio of 2.0 or Greater or Negative Likelihood Ratio of 0.5 or Lessa
| % (95% Cl) or % Range | |||||
|---|---|---|---|---|---|
| Sensitivity | Specificity | Positive Likelihood Ratio | Negative Likelihood Ratio | ||
| General Features | |||||
| Family history of osteoarthritis26 | 191 (21) | 34 (25–44) | 84 (74–91) | 2.1 (1.2–3.6) | 0.79 (0.67–0.93) |
| History of knee osteoarthritis26 | 173 (26) | 33 (24–43) | 84 (73–92) | 2.1 (1.1–3.8) | 0.80 (0.68–0.95) |
| Age, y | |||||
| >6020 | 220 (68) | 96 (80–99.9) | 25 (29–42) | 1.5 (1.3–1.7) | 0.11 (0.02–0.78) |
| >5026 | 199 (83) | 91 (84–96) | 28 (19–39) | 1.3 (1.1–1.5) | 0.32 (0.16–0.62) |
| Morning stiffness <60 min20,26 | 415 (55) | 56–91 | 41–67 | 1.5–1.7 | 0.22–0.65 |
| Location of Pain | |||||
| Worst pain in medial thigh20 | 220 (2.7) | 12 (2.5–31) | 98 (96–99.7) | 7.8 (1.7–37) | 0.89 (0.77–1.0) |
| Worst pain in buttock20,27 | 292 (34) | 12–67 | 57–69 | 0.38–2.0 | 0.38–0.76 |
| Activity Effect on Pain | |||||
| Climbing stairs or walking down slopes4 | 230 (47) | 68 (59–76) | 68 (58–76) | 2.1 (1.6–2.8) | 0.47 (0.35–0.63) |
| Pain on initial steps after rest20 | 220 (76) | 92 (74–99) | 26 (20–32) | 1.2 (1.1–1.4) | 0.31 (0.08–1.2) |
| Pain on walking20,26 | 415 (80) | 80–97 | 12–34 | 1.1–1.2 | 0.25–0.58 |
| Pain relieved by sitting20 | 220 (30) | 92 (1.0–26) | 33 (60–73) | 1.4 (0.2–1.6) | 0.24 (0.06–0.92) |
eTable 4 provides results from individual studies and findings not meeting the likelihood ratio thresholds.
With proportion (%) of hips with each clinical finding.
Several features were best at identifying patients unaffected by hip OA. Younger patients (age <60 years) compared with older patients are less likely to have hip OA (sensitivity, 96%; specificity, 25%; LR–, 0.11 [95% CI, 0.02–0.78]). While the presence of morning stiffness (sensitivity range, 56%−91%; specificity range, 41%–67%), pain on walking (sensitivity range, 80%−97%; specificity range, 12%−34%), or relief of pain on sitting (sensitivity, 92%; specificity, 33%) did not help identify hip OA in patients (all with LR <2.0), the absence of these features identified patients less likely to have hip OA (absence of morning stiffness <60 minutes: LR– range, 0.22–0.65; absence of pain on walking: LR– range, 0.25–0.58; absence of pain improved on sitting: LR–, 0.24 [95% CI, 0.06–0.92]).
Clinical Signs
Six studies4,20,21,26–28 evaluated physical examination findings and reported on the physical examination findings most likely to be associated with hip OA (Table 2). In general, physical examination findings were more useful than historical features for identifying the presence of OA. The most strongly associated physical findings were (in descending order) as follows: posterior hip pain caused by squatting (sensitivity, 24%; specificity, 96%; LR, 6.1 [95% CI, 1.3–29]), groin pain on hip abduction or adduction (sensitivity, 33%; specificity, 94%; LR, 5.7 [95% CI, 1.6–20]), abductor weakness (sensitivity, 44%; specificity, 90%; LR, 4.5 [95% CI, 2.4–8.4]), decreased hip adduction (sensitivity, 80%; specificity, 81%; LR, 4.2 [95% CI, 3.0–6.0]), and decreased internal rotation (sensitivity, 66%; specificity, 79%; LR, 3.2 [95% CI, 1.7–6.0]) as measured by a goniometer or compared with the contralateral leg.
Table 2.
Physical Examination Findings and Likelihood of Hip Osteoarthritis With Positive Likelihood Ratio of 2.0 or Greater or Negative Likelihood Ratio of 0.5 or Lessa
| % (95 % CI) or % Range | |||||
|---|---|---|---|---|---|
| Sensitivity | Specificity | Positive Likelihood Ratio | Negative Likelihood Ratio | ||
| General Findings | |||||
| Abductor weakness20 | 220 (14) | 44 (24–65) | 90 (85–94) | 4.5 (2.4–8.4) | 0.62 (0.43–0.88) |
| Limp26 | 165 (73) | 85 (76–92) | 43 (31–55) | 1.5 (1.2–1.9) | 0.35 (0.20–0.61) |
| Pain on Palpation | |||||
| Inguinal ligament tenderness20 | 220 (29) | 60 (39–79) | 75 (68–81) | 2.4 (1.6–3.8) | 0.53 (0.33–0.87) |
| Tensor fascia lata tenderness20 | 220 (23) | 40 (21–61) | 80 (73–85) | 2.0 (1.1–3.4) | 0.75 (0.54–1.1) |
| Pain on Movement and Provocation Tests | |||||
| Squat causing posterior pain27 | 72 (53) | 24 (8.2–47) | 96 (86–99.5) | 6.1 (1.3–29) | 0.79 (0.62–1.0) |
| Groin pain on abduction or adduction27 | 72 (14) | 33 (15–57) | 94 (84–99) | 5.7 (1.6–20) | 0.71 (0.52–0.97) |
| Scour test27c | 72 (36) | 62 (42–82) | 74 (60–86) | 2.4 (1.4–4.3) | 0.51 (0.29–0.90) |
| Pain on hip adduction20,26 | 410 (58) | 68–80 | 46–54 | 1.5–1.5 | 0.43–0.59 |
| Pain on hip internal rotation20,26 | 412 (68) | 82–88 | 38–39 | 1.4–1.4 | 0.31–0.45 |
| Tests of Motion | |||||
| Restricted movement21 | |||||
| 3 planes | 39 (16) | NAd | NAd | 4.4 (2.4–8.3) | NAd |
| 2 planes | 46 (18) | NAd | NAd | 1.5 (0.90–2.6) | NAd |
| 1 plane | 63 (25) | NAd | NAd | 1.3 (0.85–2.0) | NAd |
| 0 planes | 102 (41) | NAd | NAd | 0.91 (0.78–1.1) | NAd |
| Decreased hip adduction20e | 220 (26) | 80 (59–93) | 81 (75–86) | 4.2 (3.0–6.0) | 0.25 (0.11–0.54) |
| Decreased hip internal rotation20,26–28e | 788 (30) | 66 (47–81) | 79 (57–92) | 3.2 (1.7–6.0) | 0.43 (0.31–0.60) |
| Decreased range of movement4e | 230 (51) | 75 (66–82) | 74 (65–82) | 2.9 (2.1–4.0) | 0.34 (0.25–0.47) |
| Decreased hip extension20e | 220 (37) | 76 (55–91) | 68 (61–75) | 2.4 (1.8–3.2) | 0.35 (0.17–0.71) |
| Decreased hip extension20e | 220 (40) | 76 (55–91) | 64 (57–71) | 2.1 (1.6–2.8) | 0.37 (0.19–0.76) |
| Decreased hip abduction20e | 220 (58) | 88 (69–98) | 46 (38–53) | 1.6 (1.3–2.1) | 0.26 (0.09–0.77) |
Abbreviation: NA, not applicable.
eTable 5 provides results from individual studies and findings not meeting likelihood ratio thresholds.
With proportion (%) of hips with each clinical finding.
The Scour test is an impingement test where the examiner compresses the femoral neck against the acetabulum while the femur is at maximal flexion and while applying axial pressure, the knee is moved in an arc toward the shoulders. A positive test consists of “bumps” in movement, pain, or patient apprehension with the motion.
For ordinal data shown from 0 planes to 3 planes, sensitivity and specificity do not apply. Results shown as serial likelihood ratios to show the increasing likelihood of restricted movements from 0 to 3 different affected planes.
Measured with goniometer and/or comparison with contralateral hip.
While the presence of pain during the range-of-motion test was useful for identifying affected patients, decreased range-of-motion findings were more useful than those that simply recorded pain provoked by movement (Figure 4).The presence of normal hip passive adduction (sensitivity, 80%; specificity, 81%; LR–,0.25 [95% CI, 0.11–0.54]) or abduction (sensitivity, 88%; specificity, 46%; LR–, 0.26 [95% CI, 0.09–0.77]) were most useful for identifying patients with hip pain who were less likely to have OA.
Figure 4.
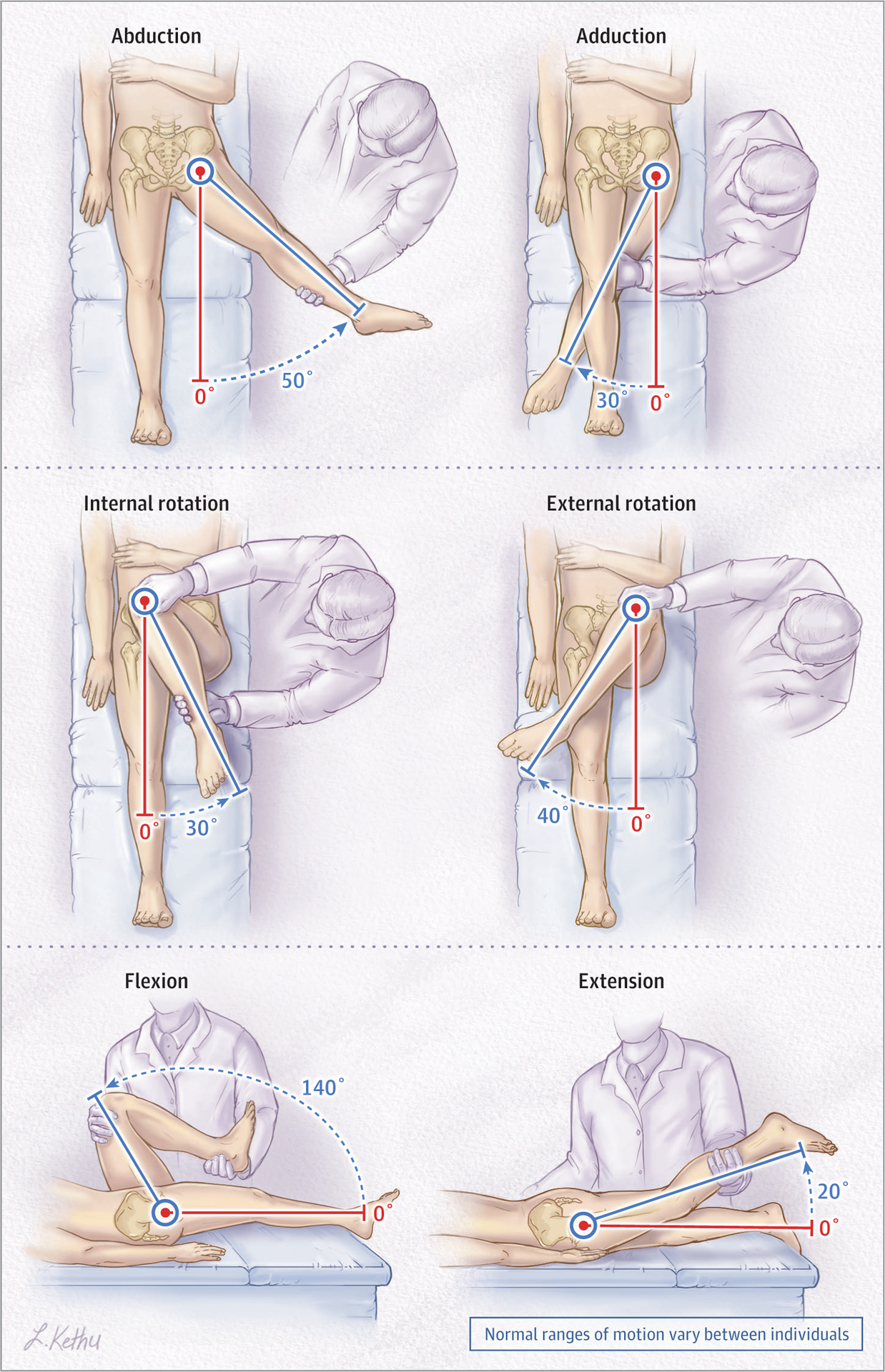
Normal Hip Ranges of Motion
Simple Laboratory Tests
Only a single study evaluated the role of 2 blood tests in the evaluation of hip OA: rheumatoid factor and erythrocyte sedimentation rate.26 The presence of rheumatoid factor at a titer of 1:80 or greater was present in 34% of patients and significantly decreased the likelihood of OA (sensitivity, 96%; specificity, 62%; LR, 0.06 [95% CI, 0.01–0.23]). The absence of a rheumatoid factor titer less than 1:80 increased the likelihood of OA as the cause of the patient’s hip discomfort (LR, 2.6 [95% CI, 1.8–3.6]). In those with an erythrocyte sedimentation rate of 40 mm/h or greater, an alternative diagnosis was more likely to be the cause of pain (LR, 0.42 [95% CI, 0.21–0.83]).
Combination of Findings
In one study, factors found to be associated with OA were age older than 60 years, pain lasting longer than 3 months, groin tenderness, decreased external rotation, and absence of pain aggravation by sitting (Table 3).20 Hip OA was strongly associated with the presence of 4 or more findings (LR, 4.9 [95% CI, 2.8–8.7]) while no or 1 finding indicated a reduced likelihood of hip OA (LR, 0.24 [95% CI, 0.09–0.64]).
Table 3.
Combinations of Clinical Signs and Likelihood of Hip Osteoarthritisa
| Feature | Thresholdb | No. (%)c | Positive Likelihood Ratiod |
|---|---|---|---|
| Any Hip Osteoarthritis | |||
No. of signs20
|
≥4 Present | 48 (22) | 4.9 (2.8–8.7) |
| 2–3 | 137 (62) | 0.72 (0.57–0.93) | |
| ≤1 | 35 (16) | 0.24 (0.09–0.64) | |
| Severe Hip Osteoarthritis | |||
No. of signs20
|
|||
| ≥5 Present | 22 (10) | 35 (13–95) | |
| 4 | 30 (14) | 2.0 (0.88–4.3) | |
| ≤3 | 168 (76) | 0.05 (0.01–0.32) |
eTable 6 provides the results at each threshold value.
Number of clinical signs that were present.
Number of hips and proportion (%) with each clinical finding.
Results are serial likelihood ratios (so sensitivity and specificity do not apply). As the number of findings increase, the likelihood of any hip osteoarthritis or severe hip osteoarthritis increases. Serial likelihood ratios were derived from the study by Bierma-Zeinstra et al.20
This same study evaluated a combination of 7 findings for severe OA (minimal joint space ≤1.5 mm): patient age older than 60 years, inguinal ligament tenderness, decreased external rotation, decreased internal rotation, and decreased adduction, bony restriction using passive hip movement, and hip abductor weakness (Table 3).20 The presence of 5 or more findings was highly suggestive of severe OA (LR, 35 [95% CI, 13–95]) while those with 3 or fewer findings were much less likely to have severe OA (LR, 0.05 [95% CI, 0.01–0.32]). However, the authors noted that inguinal ligament tenderness has not previously been identified as a clinical sign of hip OA and that this finding should by tested in further studies.20
Discussion
The studies included in this review showed that a small number of clinical findings can help estimate the likelihood of hip OA among patients presenting with hip and/or groin pain. These data are consistent with the pragmatic approach recommended by some national organizations.15
Hip OA can be diagnosed in patients that present with typical features, such as posterior hip pain with squatting, reduced range of movement of the affected hip, or groin pain on abduction or adduction. These findings may be sufficient for a clinical diagnosis of OA (without need for imaging) in a patient with mild symptoms. With features that are atypical for hip OA, such as normal range of motion and painless internal rotation, plain radiographs may be unhelpful and even confuse the diagnostic picture by identifying incidental hip OA. Alternatively, patients with severe pain lasting more than 3 months, extended morning stiffness, weight loss, or extreme pain with range-of-motion testing may require further investigation. Patients with OA features whose symptoms are sufficiently limiting that they might consider surgery may also require radiographic confirmation of the diagnosis before referral to an orthopedic surgeon. A combination of clinical findings (≥5 findings from age >60 years, inguinal ligament tenderness, decreased external rotation, decreased internal rotation, bony restriction on passive hip movement, and hip abductor weakness) may provide the most useful clinical means of predicting severe radiographic hip OA. However, further studies may be necessary to confirm the association between inguinal ligament tenderness and hip OA.20 Figure 5 summarizes one approach that clinicians might adopt when evaluating a patient with atraumatic hip or groin pain, although this has not been independently validated.
Figure 5. Algorithm for Rationalizing Use of Imaging in Adults Presenting With Atraumatic Hip or Groin Pain.
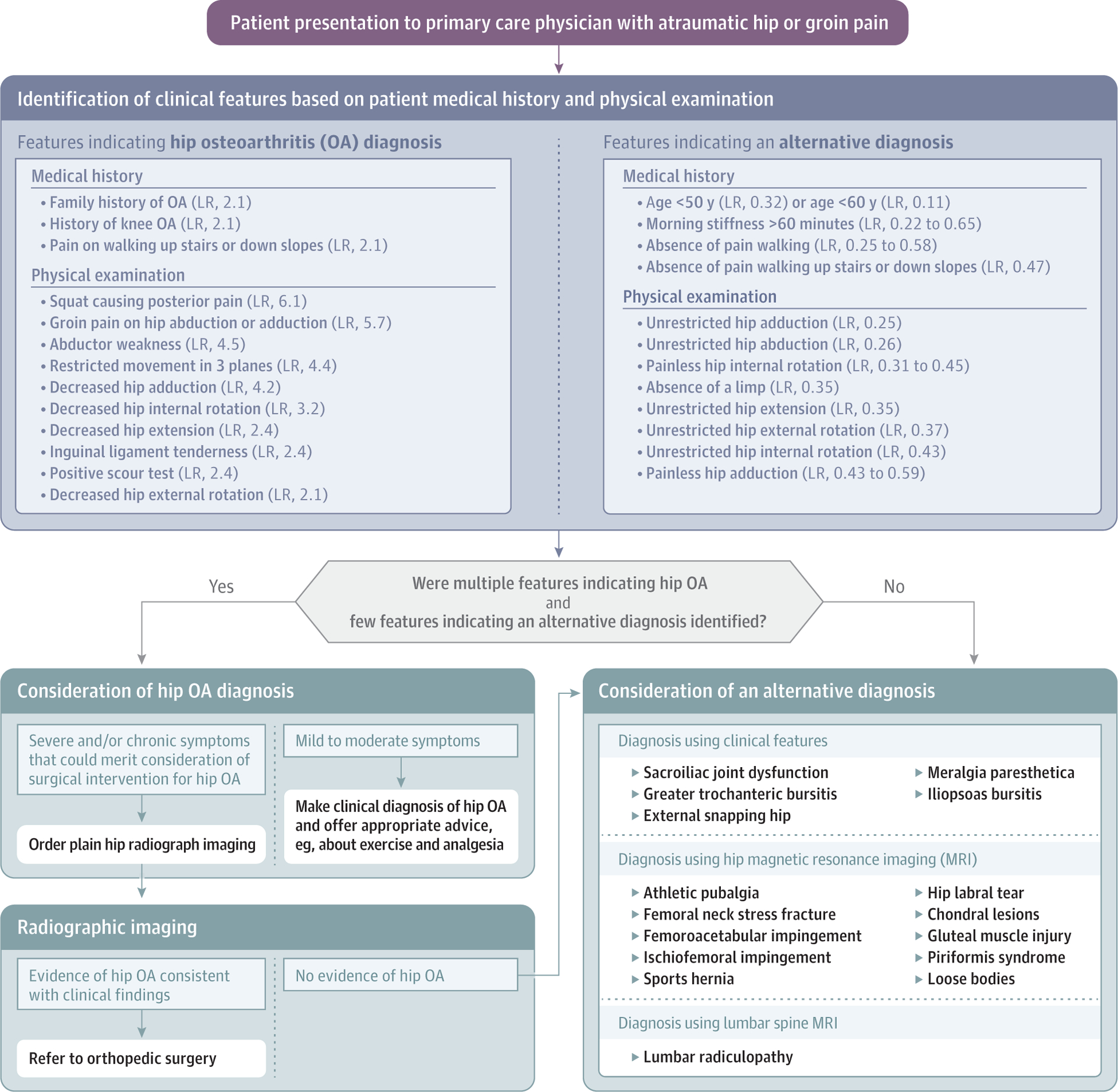
This approach shown has not been independently validated. LR indicates likelihood ratio.
Our findings suggest that clinicians should focus on ensuring that they are confident in the examination of hip movements. Although affected hips may be examined with reference to the unaffected side in many patients, OA often occurs bilaterally.29 Clinicians should, therefore, aim to recognize “normal” hip movement so that they can become proficient at eliciting signs in patients with bilateral disease. This is particularly true as most primary care offices do not have a goniometer.
The competent clinical evaluation of patients with hip pain is necessary because overinvestigation is likely to lead to erroneous diagnoses of significant hip OA in patients with incidental radiographic findings17 but who have an alternative cause for their symptoms. Overuse of imaging may also expose patients unnecessarily to ionizing radiation.3,30 The LRs provided in this study should be used to rationally identify the patients whose pretest probability for hip OA is sufficient to justify radiographic imaging. They may also be sufficient to clinically diagnose hip OA in patients with mild symptoms that do not yet warrant surgical referral.3,15
Limitations
The certainty of these recommendations is reduced by the small evidence base. In particular, there is a lack of data from patients presenting with pain in primary care. Only 2 studies20,21 reported on the factors associated with hip OA among patients presenting initially to a generalist physician. As some of the clinical tests performed by specialists are likely to be unfamiliar to generalists (eg, the Scour test), it is possible that the test would either not be performed or be performed differently. It is reassuring that the features that were most associated with OA were either found on the clinical history (eg, pain on climbing stairs or walking down slopes) or physical examination (eg, decreased hip movements and pain on internal/external rotation) that should be familiar to, and readily elicited by, most clinicians. Previous studies have found that there is good inter-rater reliability for interpreting simple hip clinical signs among clinicians from different disciplines.31,32 However, there were differences in terms of how clinical signs were elicited even between studies included within this review. It is also uncertain whether these signs would be interpreted exactly the same by generalists as by specialists.
The lack of primary care studies also challenges the external validity of our findings. The LRs of each clinical sign were based largely on hospital outpatients and may not be generalizable to the population presenting within primary care. For example, the prevalence of radiographic hip OA in the 3 studies4,26,28 from consecutive patients referred to specialists was higher than the 2 studies20,21 of consecutive patients seen in primary care (42% vs 28%). Such a difference occurs because patients whose symptoms improve are less likely to be referred. This selection bias increases disease prevalence in secondary care populations but also leads to verification bias because only those with persistent hip symptoms are referred and so undergo radiographic imaging. The effect of verification bias is usually to produce a specificity estimate that is too low and a sensitivity estimate that is too high.18 It is, therefore, possible that clinical findings in primary care settings will have higher specificity (positive findings have a greater LR in primary care than in specialty care) but lower sensitivity than the estimates reported in this study (negative findings are not as useful at ruling out hip OA in primary care compared with specialty care).
The quality of the underlying evidence was mixed. We did not include data from studies with the lowest QUADAS-2 scores (ie, nonindependent comparisons of clinical signs) but one included study was assigned QUADAS-2 level 3. Although our study reported data on 62 different clinical findings, only 20 (32%) were evaluated by more than a single study. The factors most strongly associated with hip OA were generally evaluated by multiple studies and so few of our recommendations were based on single point estimates. It is, therefore, likely that the findings of future studies would fall within our estimated confidence intervals. Larger studies would be helpful to narrow the confidence intervals, particularly for those clinical findings that were only evaluated by single studies. There is a clear need for prospective diagnostic studies in primary care (where patients with hip pain are likely to initially present), particularly aimed at validating the predictive properties of combinations of clinical signs. It is nevertheless possible that other clinical signs would have proven useful if evaluated in larger, better-quality, or multiple studies.
Scenario Resolution
Before taking the individual characteristics of the presented cases, there is a pretest probability of 35% for hip OA, as this is the prevalence among patients with hip and/or groin pain presenting to a primary care practitioner for initial assessment. This pretest probability will increase or decrease as outlined below based on the features of the clinical assessment.
Case 1
The 58-year-old woman experienced groin pain (sensitivity, 39%; specificity, 74%; LR, 1.7), which persisted for more than 3 months (sensitivity, 80%; specificity, 38%; LR, 1.3). It was worse on walking up steps (sensitivity, 68%; specificity, 68%; LR, 2.1). She had decreased hip adduction (sensitivity, 80%; specificity, 81%; LR, 4.2) and internal rotation (sensitivity, 66%; specificity, 79%; LR, 3.2).The single best test (ie, decreased hip adduction) alone would convert the pretest probability of 35% to 69%.There have not been any studies to evaluate these tests in combination but the pretest likelihood for hip OA is clearly high.
Case 2
The 60-year-old man presented with hip pain that persisted for more than 3 months (sensitivity, 80%; specificity, 38%; LR, 1.3). This might have been interpreted as increasing pretest probability from 35% to 41%. However, the findings on physical examination did not support a diagnosis of hip OA. If these features were independent of each other, the absence of pain on internal rotation (LR, 0.31) and the unrestricted hip movement (LR, 0.34) would have reduced his pretest probability of hip OA to only 5.3%. If radiographs were obtained, it is possible that these would have revealed incidental hip OA, which might have confused the clinical picture. This man required careful consideration of alternative causes for his hip pain, which should include an examination for referred pain.
Clinical Bottom Line
Simple tests of hip motion and elicitation of pain during those movements can help identify patients who have radiographic evidence of hip OA. The best overall physical examination findings are squat causing posterior hip pain, pain on abduction or adduction, adductor weakness, and decreased adduction. These are strongly associated with hip OA when present and of an alternative diagnosis when absent. Patients at high likelihood of severe hip OA may be best identified initially using a combination of clinical signs.
Supplementary Material
Key Points.
Question
How can physicians identify patients who are most likely to have hip osteoarthritis (OA)?
Findings
The most useful findings for identifying patients with hip OA are squat causing posterior pain, groin pain on passive abduction or adduction, abductor weakness, and decreased passive hip adduction or internal rotation. Hip OA is unlikely in the presence of normal passive hip adduction.
Meaning
A number of simple range-of-motion tests can be used to identify patients with hip or groin pain that are most likely to have evidence of OA on hip radiographs.
Funding/Support:
Dr Metcalfe was funded by a Royal College of Surgeons of England Fulbright Scholarship and a UCB-Oxford Prize Fellowship in Biomedical Research. Dr Simel’s work was supported by the Durham Center of Innovation to Accelerate Discovery and Practice Transformation (ADAPT) (CIN 13-410) at the Durham VA Health Care System.
Role of the Funder/Sponsor: The authors’ funding bodies did not have any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Publisher's Disclaimer: Disclaimer: The views expressed are those of the authors and not necessarily those of the UK National Health Service, the NIHR, the UK Department of Health, the US Department of Veterans Affairs, or the US government. Dr Simel is a Section Editor for the Rational Clinical Examination series in JAMA but was not involved in the editorial review of or decision to publish this study.
Conflict of Interest Disclosures: Dr Perry reported receiving a National Institute for Health Research Clinician Scientist Award (CS-2014–14-012). Dr Simel reported receiving nonfinancial support from Veterans Health Affairs during the conduct of the study and personal fees from JAMAEvidence outside the submitted work. No other disclosures were reported.
REFERENCES
- 1.Metcalfe D, Harte AL, Aletrari MO, et al. Does endotoxaemia contribute to osteoarthritis in obese patients? Clin Sci (Lond). 2012;123(11):627–634. doi: 10.1042/CS20120073 [DOI] [PubMed] [Google Scholar]
- 2.Kim C, Linsenmeyer KD, Vlad SC, et al. Prevalence of radiographic and symptomatic hip osteoarthritis in an urban United States community: the Framingham osteoarthritis study. Arthritis Rheumatol. 2014;66(11):3013–3017. doi: 10.1002/art.38795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aresti N, Kassam J, Nicholas N, Achan P. Hip osteoarthritis. BMJ. 2016;354:i3405. doi: 10.1136/bmj.i3405 [DOI] [PubMed] [Google Scholar]
- 4.Morvan J, Roux CH, Fautrel B, et al. A case-control study to assess sensitivity and specificity of a questionnaire for the detection of hip and knee osteoarthritis. Arthritis Rheum. 2009; 61(1):92–99. doi: 10.1002/art.24079 [DOI] [PubMed] [Google Scholar]
- 5.O’Neill TW, Felson DT. Mechanisms of osteoarthritis (OA) pain. Curr Osteoporos Rep. 2018; 16(5):611–616. doi: 10.1007/s11914-018-0477-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grönblad M, Liesi P, Korkala O, Karaharju E, Polak J. Innervation of human bone periosteum by peptidergic nerves. Anat Rec. 1984;209(3):297–299. doi: 10.1002/ar.1092090306 [DOI] [PubMed] [Google Scholar]
- 7.Mapp PI. Innervation of the synovium. Ann Rheum Dis. 1995;54(5):398–403. doi: 10.1136/ard.54.5.398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Coderre TJ, Katz J, Vaccarino AL, Melzack R. Contribution of central neuroplasticity to pathological pain: review of clinical and experimental evidence. Pain. 1993;52(3):259–285. doi: 10.1016/0304-3959(93)90161-H [DOI] [PubMed] [Google Scholar]
- 9.Gwilym SE, Keltner JR, Warnaby CE, et al. Psychophysical and functional imaging evidence supporting the presence of central sensitization in a cohort of osteoarthritis patients. Arthritis Rheum. 2009;61(9):1226–1234. doi: 10.1002/art.24837 [DOI] [PubMed] [Google Scholar]
- 10.Stief F, Schmidt A, van Drongelen S, et al. Abnormal loading of the hip and knee joints in unilateral hip osteoarthritis persists two years after total hip replacement [published March 14, 2018]. J Orthop Res. doi: 10.1002/jor.23886 [DOI] [PubMed] [Google Scholar]
- 11.Warashina H, Kato M, Kitamura S, Kusano T, Hasegawa Y. The progression of osteoarthritis of the hip increases degenerative lumbar spondylolisthesis and causes the change of spinopelvic alignment. J Orthop. 2019;16(4):275–279. doi: 10.1016/j.jor.2019.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wilson JJ, Furukawa M. Evaluation of the patient with hip pain. Am Fam Physician. 2014;89(1):27–34. [PubMed] [Google Scholar]
- 13.Metcalfe D, Sugand K, Thrumurthy SG, Thompson MM, Holt PJ, Karthikesalingam AP. Diagnosis of ruptured abdominal aortic aneurysm: a multicentre cohort study. Eur J Emerg Med. 2016; 23(5):386–390. doi: 10.1097/MEJ.0000000000000281 [DOI] [PubMed] [Google Scholar]
- 14.Karachalios T, Karantanas AH, Malizos K. Hip osteoarthritis: what the radiologist wants to know. Eur J Radiol. 2007;63(1):36–48. doi: 10.1016/j.ejrad.2007.03.022 [DOI] [PubMed] [Google Scholar]
- 15.National Institute for Health and Care Excellence. Osteoarthritis: Care and Management. London, UK: National Institute for Health and Care Excellence; 2014. [Google Scholar]
- 16.Manek NJ, Lane NE. Osteoarthritis: current concepts in diagnosis and management. Am Fam Physician. 2000;61(6):1795–1804. [PubMed] [Google Scholar]
- 17.Kim C, Nevitt MC, Niu J, et al. Association of hip pain with radiographic evidence of hip osteoarthritis: diagnostic test study. BMJ. 2015;351: h5983. doi: 10.1136/bmj.h5983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Simel DL, Drummond R. Update: primer on precision and accuracy In: Simel DL, Rennie D, eds. The Rational Clinical Examination: Evidence-Based Clinical Diagnosis. New York, NY: McGraw-Hill; 2009. [Google Scholar]
- 19.Whiting PF, Rutjes AW, Westwood ME, et al. ; QUADAS-2 Group. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155(8):529–536. doi: 10.7326/0003-4819-155-8-201110180-00009 [DOI] [PubMed] [Google Scholar]
- 20.Bierma-Zeinstra SM, Oster JD, Bernsen RM, Verhaar JA, Ginai AZ, Bohnen AM. Joint space narrowing and relationship with symptoms and signs in adults consulting for hip pain in primary care. J Rheumatol. 2002;29(8):1713–1718. [PubMed] [Google Scholar]
- 21.Birrell F, Croft P, Cooper C, Hosie G, Macfarlane G, Silman; PCR Hip Study Group. Predicting radiographic hip osteoarthritis from range of movement. Rheumatology (Oxford). 2001;40(5): 506–512. doi: 10.1093/rheumatology/40.5.506 [DOI] [PubMed] [Google Scholar]
- 22.Deeks JJ, Altman DG. Diagnostic tests 4: likelihood ratios. BMJ. 2004;329(7458):168–169. doi: 10.1136/bmj.329.7458.168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.metan Stata module for fixed and random effects meta-analysis [computer program]. Version S456798 Boston, MA: Boston College Department of Economics; 2010. [Google Scholar]
- 24.metandi Stata module to perform meta-analysis of diagnostic accuracy [computer program]. Version S456932 Boston, MA: Boston College Department of Economics; 2008. [Google Scholar]
- 25.Hermans J, Luime JJ, Meuffels DE, Reijman M, Simel DL, Bierma-Zeinstra SM. Does this patient with shoulder pain have rotator cuff disease? the Rational Clinical Examination systematic review. JAMA. 2013;310(8):837–847. doi: 10.1001/jama.2013.276187 [DOI] [PubMed] [Google Scholar]
- 26.Altman R, Alarcón G, Appelrouth D, et al. The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum. 1991;34(5):505–514. doi: 10.1002/art.1780340502 [DOI] [PubMed] [Google Scholar]
- 27.Sutlive TG, Lopez HP, Schnitker DE, et al. Development of a clinical prediction rule for diagnosing hip osteoarthritis in individuals with unilateral hip pain. J Orthop Sports Phys Ther. 2008;38(9):542–550. doi: 10.2519/jospt.2008.2753 [DOI] [PubMed] [Google Scholar]
- 28.Holla JF, van der Leeden M, Roorda LD, et al. Diagnostic accuracy of range of motion measurements in early symptomatic hip and/or knee osteoarthritis. Arthritis Care Res (Hoboken). 2012;64(1):59–65. doi: 10.1002/acr.20645 [DOI] [PubMed] [Google Scholar]
- 29.Amstutz HC, Le Duff MJ. The natural history of osteoarthritis: what happens to the other hip? Clin Orthop Relat Res. 2016;474(8):1802–1809. doi: 10.1007/s11999-016-4888-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lewis PB, Weber AE, Nho SJ. Imaging for nonarthritic hip pathology. Am J Orthop (Belle Mead NJ). 2017;46(1):17–22. [PubMed] [Google Scholar]
- 31.Bagwell JJ, Bauer L, Gradoz M, Grindstaff TL. The reliability of Faber test hip range of motion measurements. Int J Sports Phys Ther. 2016;11(7): 1101–1105. [PMC free article] [PubMed] [Google Scholar]
- 32.Prather H, Harris-Hayes M, Hunt DM, Steger-May K, Mathew V, Clohisy JC. Reliability and agreement of hip range of motion and provocative physical examination tests in asymptomatic volunteers. PM R 2010;2(10):888–895. doi: 10.1016/j.pmrj.2010.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


