PRACTICAL IMPLICATIONS
In patients with acute-onset paraparesis inferior, the concurrent presence of new onset cortical signs (abulia or mutism), and more rarely extrapyramidal signs, should alert clinicians to consider acute anterior bihemispheric ischemia. Prompt recognition of this rare form of acute cerebral stroke can enable timely delivering of acute thrombolytic or endovascular treatment.
Acute cerebral stroke due to bilateral ischemia corresponding to the vascular supply of the anterior cerebral arteries (ACAs) is rare1 and may result in a clinical presentation that could be confused with, e.g., spinal cord infarction.2 We present a case of acute anterior bihemispheric stroke due to an absent proximal portion (A1 segment) of the right ACA.
Case
A 77-year-old right-handed man developed sudden-onset severe weakness in both legs. On admission, 90 minutes after symptom onset, the patient presented with severe and slightly asymmetric paraparesis inferior (Medical Research Council grade [MRC] 1–2/5) with a bilateral Babinski sign. The patient was drowsy and disorientated to time and place, with decreased verbal output and apathy consistent with mutism and abulia, In addition, he presented with rigidity in the upper extremities with a right-sided predominance. The patient could not comply with sensory system examination.
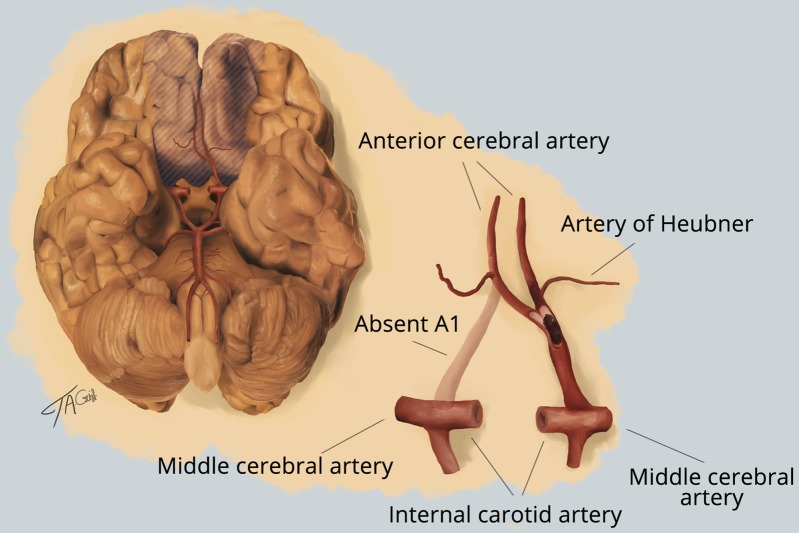
Initial brain CT angiography and perfusion images revealed bilateral hypoperfusion of the ACA vascular supply (figure 1, A and B), consistent with both A2/pericallosal arteries being supplied from the left side, as outlined in the illustration (figure 2). Intravenous thrombolysis did not result in clinical improvement. Subsequent digital subtraction angiography confirmed occlusion of the distal unique left A1 segment (aplasia of the right A1 segment) (figure 1C). The thrombus was successfully removed, with control arteriography showing full recanalization (figure 1D). CT 36 hours later was consistent with bilateral subacute infarction of the inferior part of the caudate nucleus, the anterior portion of the lentiform nucleus, the anterior limb of the internal capsule, and, further, a punctate infarct located in the right rostrum of corpus callosum—implying that both Heubner recurrent arteries (HRAs) were supplied from the left anterior circulation (figure 1E). Subsequent MRI confirmed these findings and also revealed infarction of the bilateral basofrontal cortex and small infarctions in the anterior artery supply of both hemispheres, more pronounced on the left side.
Figure 1. Neuroimaging.
Neuroimaging studies of a 77-year-old man with sudden-onset symptoms. CT (A) and perfusion of the brain (B) within 90 minutes of onset; angiography before (C; arrow points at the thrombus) and after (D) the removal of thrombus, and subsequent brain MRI (E) compatible with infarct lesions in cortical areas supplied by both anterior cerebral arteries.
Figure 2. Bihemispheric supply.
Illustration of bihemispheric supply from the left anterior cerebral artery in a patient with acute stroke due to occlusion of the distal unique left A1 segment of the anterior communicating artery by thrombus (infarct tissue shaded). Illustrator: Thomas Agerbo Gaist.
On the third day after admission, the patient still appeared drowsy, but with marked clinical improvement of the paraparesis inferior (MRC 4+/5) and could walk unaided. However, clear extrapyramidal symptoms had become more evident with rigidity and bradykinesia (right > left) of the upper extremities and right lower extremity. The gait also appeared parkinsonian with shuffling and reduced arm swing. Retropulsion was present on pull test.
Discussion
Recent advances in stroke therapy have led to the need for rapid patient evaluation when acute stroke is suspected. Our case presented with acute paraparesis as the main motor symptom, which is usually associated with medullopathy. However, speech disturbance and abulia revealed involvement of higher brain functions and raised suspicion of acute cortical involvement. Symptoms and signs of acute cortical vs acute spinal stroke resulting in paraplegia are compared in the table
Table.
Clinical features of acute bilateral anterior artery vs spinal cord infarction

Aplasia of an ACA A1 segment with resulting bihemispheric anterior supply is seen in only 0.2%–2% of autopsy cases.3 Bilateral infarctions in the vascular territory corresponding to HRAs, as observed in the present case, are rare,4 and only few cases describe this in association with A1 aplasia.3,5 Hypobulia has previously been associated with lesions in the frontal pole but have also been reported with isolated basal ganglia lesions.6 We believe that the patient's residual extrapyramidal signs and abulia can be attributed to bilateral infarcts in the vascular territory corresponding to the HRAs. The most consistent symptom reported in bilateral HRA infarctions is abulia,5 but also akinetic mutism, attention disorder, and memory disturbances. Acute parkinsonism or other extrapyramidal signs have been reported previously in single cases of bilateral HRA.7
In an era of increased acute therapeutic options, our case demonstrates the importance of considering cerebral stroke in patients with the challenging clinical presentation of acute-onset “paraparesis inferior plus.”
Appendix. Authors

Study funding
No targeted funding reported.
Disclosure
The authors report no disclosures relevant to the manuscript. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
References
- 1.Bogousslavsky J, Regli F. Anterior cerebral artery territory infarction in the Lausanne Stroke Registry. Clinical and etiologic patterns. Arch Neurol 1990;47:144–150. [DOI] [PubMed] [Google Scholar]
- 2.Zalewski NL, Rabinstein AA, Krecke KN, et al. Characteristics of spontaneous spinal cord infarction and proposed diagnostic criteria. JAMA Neurol 2019. 76:56–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.den Heijer T, Ruitenberg A, Bakker J, Hertzberger L, Kerkhoff H. Neurological picture. Bilateral caudate nucleus infarction associated with variant in circle of Willis. J Neurol Neurosurg Psychiatry 2007;78:1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bhatia KP, Marsden CD. The behavioural and motor consequences of focal lesions of the basal ganglia in man. Brain 1994;117:859–876. [DOI] [PubMed] [Google Scholar]
- 5.Fukuoka T, Osawa A, Ohe Y, Deguchi I, Maeshima S, Tanahashi N. Bilateral caudate nucleus infarction associated with a missing A1 segment. J Stroke Cerebrovasc Dis 2012;21:908.e11–908.e12. [DOI] [PubMed] [Google Scholar]
- 6.Kobayashi S, Maki T, Kunimoto M. Clinical symptoms of bilateral anterior cerebral artery territory infarction. J Clin Neurosci 2011;18:218–222. [DOI] [PubMed] [Google Scholar]
- 7.Rodier G, Tranchant C, Mohr M, Warter JM. Neurobehavioral changes following bilateral infarct in the caudate nuclei: a case report with pathological analysis. J Neurol Sci 1994;126:213–218. [DOI] [PubMed] [Google Scholar]