Abstract
Background/purpose of the study
Aim of the study was to investigate whether ellipsoid sign (ES) in the region corresponding to the cartilaginous facet of the medial femoral condyle (MFC) indicates early cartilage lesion. The finding has not been defined in the literature yet.
Methods
The study was performed retrospectively with 50 patients who underwent articular cartilage examination and arthroscopy between 2015 and 2018. Patients were divided into two according to the presence or absence of ES. There were 24 patients in case group (Group A) and 26 patients in controls (Group B). Weight-bearing cartilage areas of MFC in the region where ES was found in both groups were classified according to arthroscopic Outerbridge classification (OC) and compared statistically with each other.
Results
There was no significant difference in terms of age, gender and alignment between Group A and Group B (p > 0.05). All OC grades were higher in Group A (p < 0.001). Positive correlation between ES and MFC chondromalacia grade was detected (r: 0.671, t: 6.266, p < 0.05).
Conclusion
ES, which refers to the difference in bone density in MFC seen in antero-posterior (AP) X-Ray, is a result of changes in subchondral bone due to chronic cartilage loss. ES detected on AP X-Ray may help in early diagnosis of medial femoral articular cartilage chondromalacia, even at grade 0 or 1. We recommend searching for ES, as the earliest symptom of chondromalacia, which occurs even before MRI lesions. Future studies may reveal additional information about ES.
Keywords: Ellipsoid sign, Osteoarthritis, Cartilage, Chondromalacia, Femoral condyle
Introduction
The prevalence of osteoarthritis due to cartilage lesions increases with prolonged life expectancy. Early diagnosis and treatment of cartilage lesions with low repair regeneration capacity is important. Although Magnetic Resonance Imaging (MRI) is the gold standard non-invasive imaging method for the diagnosis of cartilage lesions, early cartilage lesions cannot be diagnosed in all MRI sequences. T1A and T2A sequences are insufficient to show focal chondral lesions and defects [1, 2]. Standard hyaline cartilage imaging is performed with 1.5 T or 3 T MRI devices. Spin echo (SE), fast spin echo (FSE), turbo spin echo (TSE), gradient echo (GRE), three-dimensional SE and three-dimensional GRE sequences are commonly used for the diagnosis of joint cartilage. Three-dimensional spoiled gradient recalled acquisition in steady state (3D SPGR) MRI with sequential fat suppression technique is the most accurate and commonly used technique showing the cartilage. It shows structural integrity and volume of cartilaginous tissue well [2–4]. As human knee articular cartilage shows diurnal variations, detecting grade 1 chondromalacia in the medial femoral condyle (MFC) may be difficult. It was shown that the thickness of the articular cartilage was changed in MRI images, at the beginning of the day or before the exercise and at the end of the day or after the exercise [5]. Direct radiography (X-Ray) has been used as a diagnostic tool only when large losses develop in joint cartilage.
The aim of the current study was to investigate whether ellipsoid sign (ES), identified on the antero-posterior (AP) X-Ray in the region corresponding to the cartilaginous facet of the MFC is associated with early cartilage lesion (Fig. 1). The finding has not been defined in literature yet.
Fig. 1.

Ellipsoid finding seen on MFC at standing AP X-Ray in both knee medial site
Materials and Methods
The study was performed with 50 patients who underwent articular cartilage examination and arthroscopy from 2015 to 2018. Study was designed as retrospective analysis of radiological and arthroscopy findings of the included patients. Study was performed in Department of Orthopedics and Traumatology in Bagcilar Research and Training Hospital.
The ethical protocol was approved by local ethics committee of Bagcilar Research and Training Hospital on 4.10.2019 with approval number as 2019.10.1.02.071. Informed consents were obtained from all participants before study. All procedures followed guidelines laid down by declaration of Helsinki-for human experiments.
Inclusion criteria were ages from 18 to 45, normal or approximately normal range of alignment (from 0 to 7 degrees of valgus angle on long leg view on AP X-ray), patients’ Kellgren–Lawrence (KL) grade 0 or 1. Exclusion criteria were ages below 18 and above 45, Body Mass Index above 30, presence of previous knee surgery, accompanying lower extremity trauma, patients who were KL grade 2, 3 or 4.
Patients were divided into two groups according to the detection of ES in MFC on standing AP X-Ray of knee preoperatively. All patients underwent to the 70 kV AP X-Ray. X-Ray beams were perpendicular to the knee from 1 m distance. Patients were divided into 2 groups according to ES presence such as Group A (24 patients in whom ES was positive) and Group B (26 patients in whom ES was negative).
All patients were classified according to KL grade 0 or grade 1. According to this classification, 22 patients with grade 0 and 2 patients with grade 1 were present in Group A and 25 patients with grade 0 and 1 patient with grade 1 were present in Group B. The weight bearing cartilage area of MFC corresponding to ES of both groups were graded according to arthroscopic Outerbridge classification (OC) and compared statistically with each other.
Patients in both groups had similar referral diagnosis for arthroscopy. In Group A, 4 diagnostic arthroscopy, 6 isolated meniscus rupture, 10 isolated anterior cruciate ligament (ACL) rupture, 1 cartilage lesion in the MFC and 3 ACL and meniscus rupture combination surgeries were performed. Micro fracture was performed during surgery in two of the diagnostic arthroscopic patients because of the presence of a small, full-thickness cartilage lesion. In Group B; 8 meniscus lesions, 12 isolated ACL rupture, 6 meniscus and ACL rupture combination surgeries were performed.
Statistics
SPSS 22.0 program was used for the analysis. Mean, standard deviation, median lowest, median highest, frequency and ratio values were used in the descriptive statistics of the data. Point biserial correlation analysis was used to measure the strength of association between the variables. Power analysis revealed that 21 cases for each group (totally 42 cases) were sufficient for 5% error margin and 80% power and 1.47 standard effect size.
Results
Mean age (in years) was 29 in Group A and 33.4 in Group B (Table 1). There were 24 patients (17 male, 7 female) in Group A and 26 patients (20 male, 6 female) in Group B (p > 0.09). According to the OC, patients with ES were 0% grade 0, 45% grade 1, 25% grade 2, 20.8% grade 3, 8.3% grade 4, whereas patients without ES were 69.2% grade 0, 23% grade 1 and 7.7% grade 2, 0% grade 3, 0% grade 4 respectively. All OC grades were present in higher ratios in Group A than Group B (p < 0.001) (Table 2; Fig. 2).
Table 1.
Mean and median ages of case and control groups
| Group A | Group B | p | |||
|---|---|---|---|---|---|
| Mean | Median | Mean | Median | ||
| Age | 29 ± 7.0 | 27.5 | 33.4 ± 9.3 | 33 | 0.094 |
Group A: case group; Group B: controls; OC: Outerbridge classification
Table 2.
Distribution of the patients according to Outerbridge classification in case and control groups
| Group A | Group B | p | |||
|---|---|---|---|---|---|
| N | % | N | % | ||
| OC | |||||
| Grade 0 | 0 | 0 | 18 | 69.2 | 0.001 |
| Grade 1 | 11 | 45.8 | 6 | 23.1 | |
| Grade 2 | 6 | 25 | 2 | 7.7 | |
| Grade 3 | 5 | 20.8 | 0 | 0 | |
| Grade 4 | 2 | 8.3 | 0 | 0 | |
Group A:case group; Group B:controls; OC: Outerbridge classification; N:number; %:percentage
Fig. 2.
Comparison of study group and control group according to Outerbridge Classification
ES was detected on right knee in 4 patients, on left knee in 4 patients and on both knees in 14 patients. (p > 0.05). There was no significant difference for meniscus rupture between groups (p > 0.05). However, grade 2 degeneration of medial meniscus in MRI was very significantly higher in Group A (p < 0.001). Mean alignment angle was 4.8 degrees valgus in Group A and 5.1 degrees valgus in Group B (p > 0.05). Diagnostic arthroscopy of 18-year-old and 25-year-old patients with ES revealed OC grade 1 chondromalacia although they had normal MRI (Fig. 3a–e), (Figs. 4a–c, 5a, b). Mosaicplasty which was performed to another 19-year-old patient with ES and full-thickness chondral lesion on MFC revealed more prominent and larger left side ES (Fig. 6a, b). The difference was associated with the severity of cartilage lesion as the patient had no complaints of his right knee. There was OC grade 2 cartilage lesion at the weight bearing articular cartilage of MFC in a 40-year-old patient who had an ES on a knee X-Ray and who was operated for chronic rupture of left ACL (Fig. 7a, b). We found cartilage lesions in varying degrees in some of our patients with ES on knee AP X-Ray, who underwent surgery due to rupture of meniscus (Fig. 8a–c). There was a positive correlation between ES and MFC chondromalacia grade (r: 0.671, t: 6.266, p < 0.05).
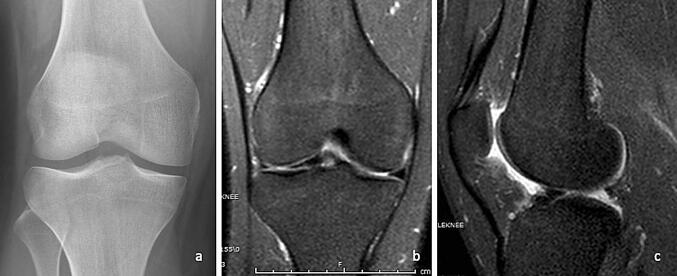
Fig. 3.
a Ellipsoid finding. b Severe condromalacia. c Grade 2 degeneration of the medial meniscus and increased cartilage thickness. d Fat suppressed MRI image. e Fat suppressed MRI image
Fig. 4.
a Ellipsoid finding of both knees. b, c Normal 3 PDW fat suppressed MRI image of right knee
Fig. 5.
a, b Grade 1 chondromalacia in the weight bearing cartilage of MFC
Fig. 6.
a Prominent ellipsoid sign in MFC in left knee. b Arthroscopic images of the cartilage lesion in weight bearing area of MFC
Fig. 7.
a Comparison of both knees with a chronic ACL rupture in left knee (prominent ellipsoid sign in left knee). b Grade 2 chondromalacia according to Outerbridge Classification
Fig. 8.
a Ellipsoid sign in MFC of the left knee. b Posterior rupture of the medial meniscus. c Grade 1 chondromalacia according to Outerbridge Classification
Discussion
The knee joint is the largest joint of the human body that works in harmony with slippery and smooth joint cartilage, menisci, intraarticular and external ligaments and muscles. Since 60% of the axial load in knee joint is absorbed by the cartilage and meniscus, the presence of intact cartilage and meniscus is essential to preserve the biomechanical function of the joint.
Recently, an MRI study has reported that gonarthrosis usually begins in MFC and spreads to other joints [6]. In our study, both MRI and arthroscopy findings revealed that patients with ES had more cartilage loss on the articular surface of MFC as compared with those without ES. We believe that, ES detected on standing AP X-Ray results from the difference in bone density caused by chronic cartilage loss in the subchondral bone of the MFC joint surface.
Meniscus and cartilage degenerations are correlated to each other [7–9]. Posterior horizontal meniscus degeneration and complex medial meniscus ruptures were reported to be associated with OC grade 3 or OC grade 4 chondral lesions in 497 patients [10]. In our study, OC grade 1 or OC grade 2 cartilage degeneration was found on knee arthroscopy in patients with ES.
Cartilages are avascular and nerveless and they are fed with diffusion. As a result, there may be no clinical symptom until severe subchondral bone resorption occurs. Cartilage lesion was more prominent in patients with ES than those without ES (Figs. 9, 10). Subchondral bone resorption occurs in the early stage of osteoarthritis, while sclerosis occurs in the late stage [11]. Several publications have reported that inhibition of bone resorption at early stages increases cartilage healing [11, 12]. Our study revealed that subchondral bones were osteoporotic due to resorption in patients with ES and that this region became more sclerotic as osteoarthritis progressed (Fig. 3a). The earliest change in subchondral bone in osteoarthritis has been reported to be vertical trabecular bone loss and increased horizontal trabeculae [13, 14]. In our study, the vertical trabecular bone in the ES region was very low or absent in accordance with the literature. Consistent with our study, MRI of 51 patients with KL grade 0 or grade 1 degeneration, showed elliptic chondromalacia in MFC [15]. Therefore, ES may be the earliest sign of osteoarthritis, which helps the clinician to request a specific MRI for early diagnosis (Fig. 3d).
Fig. 9.
a AP X-Ray: No ellipsoid sign. b MRI: Medial meniscus rupture. c Anterior cruciate ligament rupture
Fig. 10.
a No chondromalacia in arthroscopy. b Anterior cruciate ligament rupture in arthroscopy. c Bucket handle medial meniscus rupture
ES is not associated with tibio-femoral alignment since it occurs in gonarthrotic varus knees. ES is usually detected in both knees, however it may also be unilateral by affecting the knee with ligament damage occurring in the past. ES is detected in MFC, not in lateral femoral condyle (LFC), because MFC has rounded, larger and distal anatomical structure, has higher joint compliance with tibia and meniscus and has more subchondral bone ratio [14].
There are three anatomical variations in the distal femoral condyle including distal MFC groove variation, distal LFC groove variation, and anterior trochlear groove variation [16]. The distal MFC groove variation can only be identified by MRI and it cannot be seen on the AP X-ray as opposed to ES. In addition, distal MFC groove is confined to medial aspect of the condyle and accommodates anterior part of the medial meniscus on knee flexion (Fig. 3c), however ES appears to be laterally to MFC groove [17]. As a result, ES cannot be thought as an anatomical variation of the condyle.
ES corresponds to cartilage lesion ranging from arthroscopic OC grade 1 to 4 (Figs. 1, 2).
In conclusion, ES in the distal part of MFC may be a sign of arthroscopic OC grade from 1 to 4 cartilage lesion. We recommend to search for ES on standing AP X-Ray because ES may be the earliest sign of osteoarthritis even there is no clinical symptom or MRI finding. Future studies may reveal additional information about ES.
Limitations
Number of patients should have been more.
In further studies, the evaluation of ES in very early stage chondromalacia patients with no finding on MRI but diagnosed by arthroscopy will increase the diagnostic value of ES.
Acknowledgements
No source of support in the form of grants, equipment, drugs, or all of these were used in our study. There are no conflicts of interest. All authors contributed to the study. The manuscript has been read and approved by all the authors. The manuscript represents honest work.
Author contributions
SC contributed to the study by collecting the data and writing the manuscript. CA contributed to the manuscript by collecting the data and literature, and as the corresponding author.
Compliance with Ethical Standards
Conflict of interest
All authors approved the manuscript and all authors declare that are no conflicts of interest regarding the publication.
Ethical standard statement
The current study was approved by the local ethic committee.
Informed consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Sever Çaglar, Email: severcaglar@gmail.com.
Cem Albay, Email: cemalbay@hotmail.com.
References
- 1.Disler G, McCauley TR, Kelman. CG, Fuschs MD, Ratner LM, Wirth CR, et al. Fat suppressed three dimensional spoiled gradient-echo MR imaging of hyaline cartilage defects in the knee: Comparison with Standart MR imaging and arthroscopy. AJR Am J Roentgenol 1996;167:127–132. [DOI] [PubMed]
- 2.Peterfy CG, Schneider E, Nevitt M. The osteoarthritis initiative: report on the design rationale fort the magnetic resonance imaging protocol fort the knee. Osteoarthritis Cartilage. 2008;16:1433–1441. doi: 10.1016/j.joca.2008.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McCaulay RT, Recht MP, Disler DG. Clinical imaging of articular cartilage in the knee. Sem Musc Skel Rad. 2001;5:293–304. doi: 10.1055/s-2001-19040. [DOI] [PubMed] [Google Scholar]
- 4.Cicuttini F, Forbes A, Asbeutah A, Morris K, Stuckey S. Comprasion and reproducibility of fast and conventional spoiled gradient-echo magnetic resonance sequences in the determination of knee cartilage volume. Journal of Orthopaedic Research. 2000;18:580–584. doi: 10.1002/jor.1100180410. [DOI] [PubMed] [Google Scholar]
- 5.Coleman Jeremy L, Widmyer RM, Leddy HA, Utturkar GM, Charles ES, Moorman CT, et al. Diurnal variations in articular cartilage thickness and strain in the human knee. Journal of Biomechanics. 2013;46(3):541–547. doi: 10.1016/j.jbiomech.2012.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bottomley NJ, McNally E, Jones L, Javaid MK, Arden N, Gill HS. The MRI description of early anteromedial gonarthrosis. Journal of Bone and Joint Surgery. British Volume. 2012;94:47. [Google Scholar]
- 7.Yubo S, Mauerhan DR, Honeycutt. PR, Kneisi. JS, Norton. JH, Hanley. EN, et sl. Analysis of meniscal degeneration and meniscal gene expression. BMC Musculoskeletal 2010;11:11–19. [DOI] [PMC free article] [PubMed]
- 8.Englund M. Meniscal tear—a feature of osteoarthritis. Acta Orthopaedica Scandinavica. 2004;75:1–45. doi: 10.1080/03008820410002048. [DOI] [PubMed] [Google Scholar]
- 9.Howell R, Kumar NS, Patel N, Tom J. Degenerative meniscus: pathogenesis, diagnosis, and treatment options. World J Orthop. 2014;5:597–602. doi: 10.5312/wjo.v5.i5.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chritoforakis J, Pradhan R, Sanchez-Ballester. J, Hunt. N, Strachan. RK. Is there an association between articular cartilage changes and degenerative meniscus tears? Arthroscopy J. Arthro 2005;21:1366–1369 [DOI] [PubMed]
- 11.Yu. D, Xu J, Liu F, Wang X, Mao Y, Zhu. Z. Subchondral bone changes and the impacts on joint pain and articular cartilage degeneration in osteoarthritis. Clinical and experimental Rheumatology 2016;34:929–934. [PubMed]
- 12.Karsdal MA, Leeming DJ, Dam EB, Henriksen K, Alexandersen P, Pastoureau P. Should subchondral bone turnover be targeted when treating osteoarthritis? Osteoarthritis and Cartilage. 2008;16:638–646. doi: 10.1016/j.joca.2008.01.014. [DOI] [PubMed] [Google Scholar]
- 13.Messent AE, Ward JR, Tonkin JC, Wright BC. Tibial cancellous bone in patients with knee osteoarthritis. Osteoarthritis and Cartilage. 2005;13:463–470. doi: 10.1016/j.joca.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 14.Wright BC. Subchondral bone changes in hand and knee osteoarthritis detected by radiography. Osteoarthritis and Cartilage. 2004;12:10–19. doi: 10.1016/j.joca.2003.09.007. [DOI] [PubMed] [Google Scholar]
- 15.Taguchi K, Chiba K, Okazaki N, Kido Y, Miyamato T, Yonekura A, et al. Characterization of cartİlage defects detected by MRI in Kellgren Lawrence grade 0 or 1 knees. J Orthop Sci. 2017;22(5):868–873. doi: 10.1016/j.jos.2017.06.013. [DOI] [PubMed] [Google Scholar]
- 16.Tylor P, Datir A, Saifuddin A. Magnetic resonance imaging of anatomical variations in the knee part 2: miscellaneous. Skletal Radiol. 2010;12:1175–1186. doi: 10.1007/s00256-010-0904-6. [DOI] [PubMed] [Google Scholar]
- 17.Harrison B, Wood MB, Keats TE. The grooves of the distal articular surface of the femur – a normal variant. AJR. American Journal of Roentgenology. 1976;126:751–754. doi: 10.2214/ajr.126.4.751. [DOI] [PubMed] [Google Scholar]