To the Editor: We have read with great interest the articles by Llamas-Velasco et al1 and Marzano et al2 about the current controversy regarding coronavirus disease 2019 (COVID-19) vesicular exanthems and the role of herpesvirus in the etiology of these lesions. Llamas-Velasco et al1 report 3 cases of vesicular lesions in patients hospitalized with COVID-19, suggesting that complementary tests, such as Tzanck smear, virus culture, polymerase chain reaction (PCR), or skin biopsy should be performed to rule out other viral infections. Marzano and Genovese2 were not able to perform PCR tests in their previous study of varicella-like exanthem3 due to logistic reasons but also due to clinical presentation not being suggestive of varicella.
We previously conducted a prospective study of vesicular COVID-19 rashes, all with a positive nasopharyngeal swab for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), in our hospital from March 1 to April 20, 2020.4 Of a total of 53 patients, 15 were excluded because of an alternative herpes simplex/zoster clinical diagnosis (clinical data are summarized in Table I ). All 15 patients presented typical clinical lesions and symptoms of herpes simplex/zoster. Only 1 patient (6.7%) had a previous history of immunosuppression. Latency time between COVID-19 symptoms and herpetic lesions was variable (median, 16 days; range, 6-32 days). Despite performing PCR tests for SARS-CoV-2 from the content of the vesicles in only 3 patients, all of the results were negative.
Table I.
Summary of patient clinical data
| Patient | Sex | Age, y | Relevant medical history | Chest x-ray | Total number of days since onset of COVID-19 symptoms | Diagnosis | Multiplex herpes PCR/SARS-CoV-2 rt-PCR from the vesicles | Medication |
|---|---|---|---|---|---|---|---|---|
| 1 (Fig 1, A) | Male | 69 | None | Bilateral interstitial pneumonia (required ICU stay) | 16 | Recurrent herpes simplex (orolabial) | HSV1/negative | Hydroxychloroquine, azithromycin, ceftriaxone, acyclovir |
| 2 | Female | 96 | Hypertension, chronic kidney disease, hyperuricemia | Bilateral interstitial pneumonia | 27 | Recurrent herpes simplex (orolabial) | HSV1/negative | Hydroxychloroquine, azithromycin, prednisone |
| 3 | Female | 77 | Primary biliary cholangitis, Alzheimer disease | Bilateral interstitial pneumonia | 14 | Recurrent herpes simplex (orolabial) | HSV1/not done | Hydroxychloroquine, lopinavir/ritonavir, azithromycin, prednisone |
| 4 | Male | 65 | Hypertension, dyslipidemia | Bilateral interstitial pneumonia (required ICU stay) | 32 | Recurrent herpes simplex (orolabial) | HSV1/not done | Lopinavir/ritonavir, azithromycin, prednisone, tocilizumab, remdesivir, acyclovir |
| 5 | Male | 38 | Colorectal cancer (on chemotherapy treatment) | Bilateral interstitial pneumonia | 9 | Recurrent herpes simplex (orolabial) | HSV1/not done | Lopinavir/ritonavir, tocilizumab, remdesivir, prednisone, acyclovir |
| 6 | Male | 61 | None | Bilateral interstitial pneumonia (required ICU stay) | 15 | Recurrent herpes simplex (orolabial) | HSV1/not done | Hydroxychloroquine, lopinavir/ritonavir, tocilizumab, prednisone, acyclovir |
| 7 | Female | 45 | None | Bilateral interstitial pneumonia | 18 | Recurrent herpes simplex (orolabial) | Not done/not done | Hydroxychloroquine |
| 8 | Male | 76 | Hypertension, dyslipidemia | Bilateral interstitial pneumonia | 24 | Recurrent herpes simplex (orolabial) | Not done/not done | Hydroxychloroquine |
| 9 (Fig 1, B) | Female | 56 | None | Bilateral interstitial pneumonia | 22 | Localized herpes zoster | HSV3/negative | Hydroxychloroquine, valacyclovir |
| 11 | Male | 52 | None | Normal | 14 | Localized herpes zoster | HSV3/not done | Valacyclovir |
| 10 | Female | 63 | Hypertension | Normal | 26 | Localized herpes zoster (ophthalmic) | Not done/not done | Valacyclovir |
| 12 | Male | 56 | dyslipidemia | Normal | 26 | Localized herpes zoster (ophthalmic) | Not done/not done | Valacyclovir |
| 13 | Male | 82 | Hypertension, diabetes | Bilateral interstitial pneumonia | 7 | Localized herpes zoster | Not done/not done | Hydroxychloroquine, acyclovir |
| 14 | Female | 73 | Dyslipidemia | Bilateral interstitial pneumonia | 12 | Localized herpes zoster | Not done/not done | Hydroxychloroquine, prednisone, acyclovir |
| 15 | Male | 78 | Hypertension | Bilateral interstitial pneumonia | 6 | Localized herpes zoster | Not done/not done | Hydroxychloroquine, acyclovir |
COVID-19, Coronavirus disease 2016; HSV1, herpes simplex virus 1; HSV3, herpes simplex virus 3; ICU, intensive care unit; PCR, polymerase chain reaction; rt-PCR, reverse-transcriptase polymerase chain reaction; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Regarding vesicular rashes or varicella-like COVID-19 exanthems,3 we previously reported 4 cases in which we performed both PCR multiplex for herpesvirus and reverse-transcriptase PCR for SARS-CoV-2 directly from the content of the vesicles. Interestingly, results for both techniques were negative in all 4 cases.4 This reasonably rules out a role of herpes viruses3 and a potential infective ability of SARS-CoV-2 through the vesicles.
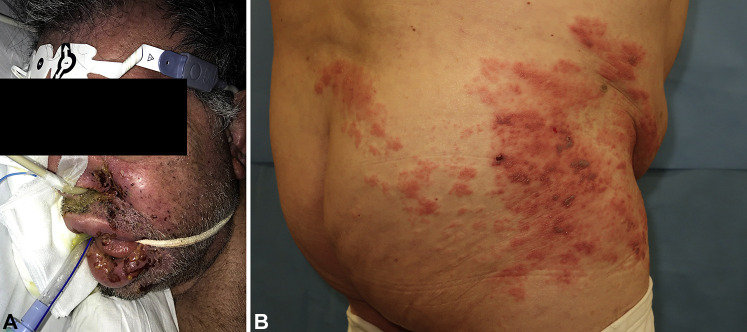
We agree with the authors that there is a potential role for herpetic viral infections and superinfections in patients with COVID-19. In fact, some presumed COVID-19 vesicular lesions have been later proven to be caused by herpetic infections.1 , 5 In our prospective study,4 from a total of 96 COVID-19 dermatologic consultations in the reported period, 15.6% corresponded to herpes simplex/zoster diagnoses. However, we cannot categorically affirm that there is an incidence increase of these diagnoses in patients with COVID-19 due to the lack of a control group. In our current experience, the diagnosis of herpesvirus infection in patients with COVID-19 does not usually involve diagnostic doubts, due to the clinical presentation and reported symptoms being typical of the disease, even when lesions are extensive (Fig 1 ).
Fig 1.
A, A 69-year-old man with COVID-19 pneumonia and extensive orolabial herpes simplex virus 1 reactivation. B, A 56-year-old woman with COVID-19 pneumonia and herpes zoster on the trunk.
In conclusion, complementary diagnostic tests for herpesvirus and even SARS-CoV-2 may prove useful for clinical research and should be encouraged if the necessary resources are available. However, we believe that regarding clinical practice, we should reserve these techniques for atypical clinical presentations or cases where therapeutic management would change significantly.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
IRB approval status: Not applicable.
Reprints not available from the authors.
References
- 1.Llamas-Velasco M., Rodríguez-Jiménez P., Chicharro P., et al. Reply to “Varicella-like exanthem as a specific COVID-19-associated skin manifestation: multicenter case series of 22 patients”: to consider varicella-like exanthem associated with COVID-19, virus varicella zoster and virus herpes simplex must be ruled out. J Am Acad Dermatol. 2020;83(3):e253–e254. doi: 10.1016/j.jaad.2020.04.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marzano A.V., Genovese G. Response to “Reply to ‘Varicella-like exanthem as a specific COVID-19-associated skin manifestation: multicenter case series of 22 patients’: to consider varicella-like exanthem associated with COVID-19, virus varicella zoster and virus herpes simplex must be ruled out.”. J Am Acad Dermatol. 2020;83(3):e255–e256. doi: 10.1016/j.jaad.2020.05.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marzano A.V., Genovese G., Fabbrocini G., et al. Varicella-like exanthem as a specific COVID-19-associated skin manifestation: multicenter case series of 22 patients. J Am Acad Dermatol. 2020;83(1):280–285. doi: 10.1016/j.jaad.2020.04.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fernandez-Nieto D, Ortega-Quijano D, Jimenez-Cauhe J, et al. Clinical and histological characterization of vesicular COVID-19 rashes: a prospective study in a tertiary care hospital [e-pub ahead of print]. Clin Exp Dermatol. https://doi.org/10.1111/ced.14277. Accessed May 27, 2020. [DOI] [PMC free article] [PubMed]
- 5.Galván Casas C, Català A, Carretero Hernández G, et al. Classification of the cutaneous manifestations of COVID-19: a rapid prospective nationwide consensus study in Spain with 375 cases [e-pub ahead of print]. Br J Dermatol. https://doi.org/10.1111/bjd.19163. Accessed May 27. 2020. [DOI] [PMC free article] [PubMed]