Prehabilitation involves health-optimizing interventions aimed at enhancing patients’ ability to tolerate an upcoming stressor. Surgical prehabilitation is typically multimodal and has been shown to enhance health and treatment outcomes.1 In the setting of the novel COVID-19 pandemic, prehabilitation may counteract the unintended sequelae of “social distancing” that may result in decreased cardiopulmonary fitness arising from increased sedentary behavior, theoretically leading to increased morbidity and mortality, particularly in patients with advanced age or medical frailty.2 Notably, among a subgroup of Italian fatalities, approximately 20% of patients infected with COVID-19 had active cancer.3 In addition, guidance related to nutrition and maintenance of psychologic health is impacted due to reduced availability of in-person visits with oncologic providers. Before the COVID-19 pandemic, our group was conducting a registered phase II clinical trial (NCT0386587) on the feasibility and benefits of prehabilitation during neoadjuvant therapy before surgical resection in patients with pancreatic ductal adenocarcinoma. Since pausing the trial, we turned our attention to supporting patients through telemedicine platforms. Here, we report our adaptive response to pandemic-related prehabilitation barriers using a virtual platform.
NEOADJUVANT THERAPY DURING THE PANDEMIC
In addition to the aforementioned cardiopulmonary deconditioning that may occur with social distancing, other complicating factors that have arisen in the setting of COVID-19 include changes to neoadjuvant protocols that are extended to keep patients out of the hospital for their own safety and to preserve valuable hospital resources. Changes to neoadjuvant therapy implemented at our institution include, but are not limited to, increased number of cycles of neoadjuvant chemotherapy over an extended duration and increased referrals for neoadjuvant therapy rather an upfront surgery in cases of upfront resectable tumors. By delaying “elective” operations and increasing the neoadjuvant treatment period, patients may encounter additional physiologic deterioration as a result of prolonged cytotoxic therapy.
Neoadjuvant therapy is known to be associated with a reduction in physical activity and increase in sarcopenia. Sarcopenia itself may result in decreased overall survival.4 Specifically, among patients with gastrointestinal cancers, the risk of malnutrition due to the disease process and side-effects of treatment poses a real danger.5 In a pandemic, however, malnutrition may be compounded by reduced access to healthful foods, which can further complicate patients’ nutritional status.
A TELEMEDICINE HOME-BASED PREHABILITATION PROGRAM
In response to the COVID-19 pandemic, we have developed a home-based prehabilitation program following evaluation of our preliminary trial results. The program we describe here may be considered for patients who are undergoing neoadjuvant therapy while awaiting surgery during the current pandemic. The proposed multimodal intervention, consisting of a standardized fitness program, nutrition supplementation, smoking cessation, and mindfulness practice, could be extrapolated for all oncologic patients awaiting eventual surgical intervention following the COVID-19 pandemic.
Our multidisciplinary team at the Massachusetts General Hospital (MGH) consists of physicians in the oncologic disciplines and physical medicine and rehabilitation. In addition, the team includes providers specializing in physical therapy and cancer nutrition.
Exercise Intervention
Patients receiving neoadjuvant treatment before surgery are screened by a physician to determine whether it is safe and feasible to participate in home-based training. Safety considerations are based on established exercise-oncology guidelines.6,7 If a patient is deemed appropriate for referral to the prehabilitation program, patients complete a virtual baseline assessment for placement into a fitness tier (basic, intermediate, or advanced) that informs the exercise prescription (Fig. 1). Evidence on the validity and reliability of virtual fitness testing is limited. However, under COVID-19 circumstances whereon patients would not otherwise receive care, we have employed the well-validated and simple 30-second Sit-to-Stand (30StS)8 test for home-based self-assessment to triage patients into the fitness tiers. The established tiers in Figure 1 were constructed from preliminary data from our clinical trial that demonstrated variance in patient fitness capacity based on these cut-offs. Participants in each tier are encouraged to complete 3 sessions per week for as long as the social distancing restrictions apply.
FIGURE 1.
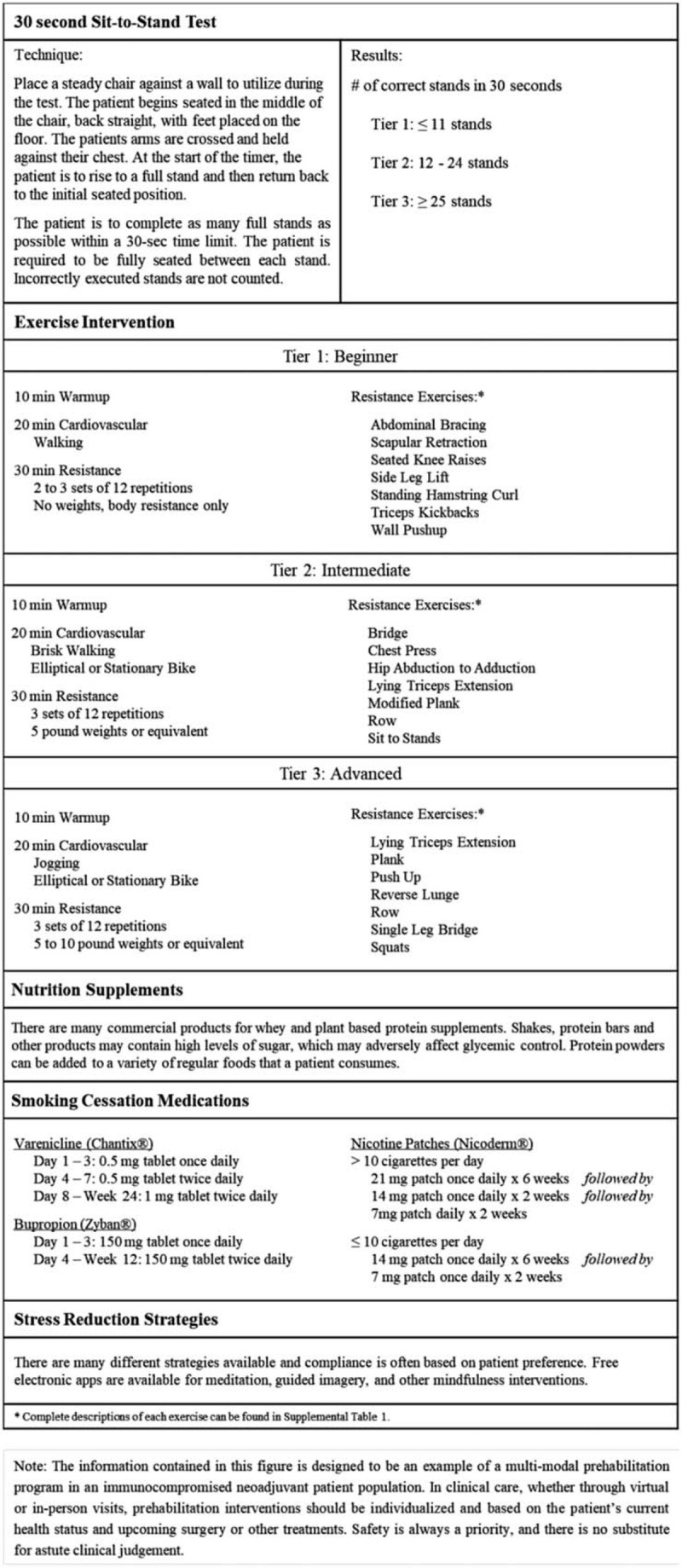
Example of a multimodal prehabilitation program for oncology patients undergoing neoadjuvant therapy.
Using the 30StS scores, the patient is provided a “whole body” exercise prescription developed by a licensed cancer exercise specialist. This whole body approach is critical in the setting of inactivity and during neoadjuvant therapy to mitigate the effects of muscle wasting on core muscle groups. Each exercise tier is comprised of a 10 minute cardiovascular warm-up, followed by 20 minutes of cardiovascular endurance training, and ending with 30 minutes of resistance and flexibility exercises. Clinicians should use their judgment, based on patient symptoms, comorbidities, and home-settings, to modify aspects of this suggested regimen for individual patients. Cardiovascular endurance exercises are modified according to patients’ needs and living situation, and outdoor exercise (eg, walking) is encouraged for added psychological benefit, provided social distancing criteria are met. Target intensity of exercise is based on the American College of Sports Medicine (ACSM) recommendations for cancer survivors.6 The ACSM guidelines recommend cancer patients exercise to 60% to 85% HR reserve for cardiovascular endurance exercises and a HR of 60% to 70% per repetition for resistance exercises. The exercise prescriptions are intended to require minimal or no fitness equipment, but can be included if available to the patient without attending a public/shared fitness facility.
Resistance training includes body weight, resistance band, or free-weights exercises that target the large upper and lower body muscle groups, as well as core stability (Supplemental Table 1). In the absence of free-weights, different objects in the home may be used if they can be safely held and provide the requisite training stimulus (eg, full water bottles, cans, or cloth bags with sufficiently heavy contents). Flexibility exercises such as stretching target major muscle groups activated during the exercise. If available, participants are encouraged to use their physical activity trackers and associated health apps. Smartphones are nearly ubiquitous and often have built-in technology that can track steps and/or heart rate, as well as support apps to log the details of exercise bouts.
Nutrition Intervention
In addition to a nutritious diet, it is important for patients to account for glycemic control and enhance protein intake.2 Glycemic control is important in mitigating infections, whereas increased protein intake provides the building blocks during muscle conditioning. Prehabilitation research suggests that whey and/or plant-based protein supplementation may be helpful, and assuming there are no contraindications, we suggest that patients consume a daily supplemental protein intake of 30 g in addition to their normal dietary intake.9 Although daily consumption is optimal, our trial data demonstrated that daily compliance may have been an issue based on preliminary reports. Therefore, a more realistic goal to be sustained over months is to consume this supplement 4 times per week rather than daily. The specific supplement of use can be determined on an individual basis by the treating physician or licensed dietitian/nutritionist to meet the unique needs of each patient and to promote compliance.
Smoking Cessation
Substance abuse can undermine conditioning, tolerance of therapy, and prehabilitation at a time of increased anxiety and heightened stress. Social distancing can be either a positive or negative influence in the attempt to help patients quit smoking in the setting of a newly diagnosed illness.10 One can anticipate that a pandemic may result in reduced access to and income for cigarette purchasing, and it is likely that some patients may increase their smoking, whereas others may aim to decrease it or even be amenable to cessation altogether. Therefore, virtual oversight of the use of tobacco products (and also alcohol as well as other substances) with individualized health advice (eg, smoking cessation or alcohol reduction) from the treating physician at each telemedicine oncology visit is paramount at this time. Smoking cessation is imperative for optimal surgical outcomes. Therefore, appropriate advice and medical intervention (including medications that can be e-prescribed and symptoms monitored virtually) may be helpful.
Mindfulness
Increased stress is common in cancer patients under usual circumstances. However, in this global pandemic, patients now have the added uncertainty of how their cancer and overall health will fair and whether delays in care may result in detrimental outcomes. Encouraging stress reduction interventions is best practices in general, and may provide an added benefit during this particularly challenging time. There are many types of interventions such as meditation, guided imagery, yoga, and so on. Many mindfulness platforms exist free-of-charge online and can be tailored to individual patient preferences.
Risks to Participants
As noted, physicians should provide initial evaluations and appropriate follow-up for all oncology patients throughout the pandemic. Although many studies have documented that exercise in cancer survivors,6 even those undergoing neoadjuvant therapy, is safe, caution is still warranted, particularly given the reduction in direct supervision. Before commencing exercise sessions, patients should be instructed to be mindful of any significant changes in symptoms (eg, excessive shortness of breath) or the presence of new symptoms (e.g. chest pain), to determine whether patients should engage in exercise on a given day. Common side-effects include muscular fatigue and soreness, as well as transient increases in treatment-related symptoms. Rarer risks include the possibility of injury due to unknown bone metastases or acute cardiac events in conjunction with cytotoxic therapy. Intensity and acute changes in symptoms should be closely monitored and reported.
In conclusion, a structured multimodal virtual prehabilitation program for cancer patients during the COVID-19 pandemic may help promote optimal outcomes during neoadjuvant therapy and better prepare them for future surgery. The unique availability of time and social distancing provides a distinct opportunity to improve patients’ health by optimizing cardiopulmonary reserve, skeletal muscle mass, nutritional status, and mental well-being. A virtual prehabilitation intervention would focus on modifiable predictors of outcomes and empower patients to regain control of their cancer.
Supplementary Material
Footnotes
NMS was supported by the NIH T32 Research Training in Aging grant 5T32AG023480-14. The NIH had no involvement in study design; collection, analysis, or interpretation of data; writing of the report; or decision to submit the article for publication.
The authors report no conflicts of interest.
REFERENCES
- 1.Carli F, Silver JK, Feldman LS, et al. Surgical prehabilitation in patients with cancer: state-of-the-science and recommendations for future research from a panel of subject matter experts. Phys Med Rehabil Clin N Am 2017; 28:49–64. [DOI] [PubMed] [Google Scholar]
- 2. Silver JK. Prehabilitation Could Save Lives In A Pandemic - The BMJ. [online] The BMJ. Available at: https://blogs.bmj.com/bmj/2020/03/19/julie-k-silver-prehabilitation-could-save-lives-in-a-pandemic/2020 Mar 19. [Accessed March 22, 2020]. [Google Scholar]
- 3.Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA 2020; doi: 10.1001/jama.2020.4683. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 4.Okuno M, Goumard C, Kopetz S, et al. Loss of muscle mass during preoperative chemotherapy as a prognosticator for poor survival in patients with colorectal liver metastases. Surgery 2019; 165:329–336. [DOI] [PubMed] [Google Scholar]
- 5.Gärtner S, Krüger J, Aghdassi AA, et al. Nutrition in pancreatic cancer: a review. Gastrointest Tumors 2016; 2:195–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Campbell KL, Winters-Stone KM, Wiskemann J, et al. Exercise guidelines for cancer survivors: consensus statement from International Multidisciplinary Roundtable. Med Sci Sports Exerc 2019; 51:2375–2390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maltser S, Cristian A, Silver JK, et al. A focused review of safety considerations in cancer rehabilitation. PMR 2017; 9:S415–S428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jones CJ, Rikli RE, Beam WC. A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Research quarterly for exercise and sport. Res Q Exerc Sport 1999; 70:113–119. [DOI] [PubMed] [Google Scholar]
- 9.Minnella EM, Awasthi R, Loiselle SE, et al. Effect of exercise and nutrition prehabilitation on functional capacity in esophagogastric cancer surgery: a randomized clinical trial. JAMA Surg 2018; 153:1081–1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Choi NG, DiNitto DM. Role of new diagnosis, social isolation, and depression in older adults’ smoking cessation. Gerontologist 2015; 55:793–801. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


