Abstract
Rationale & Objective
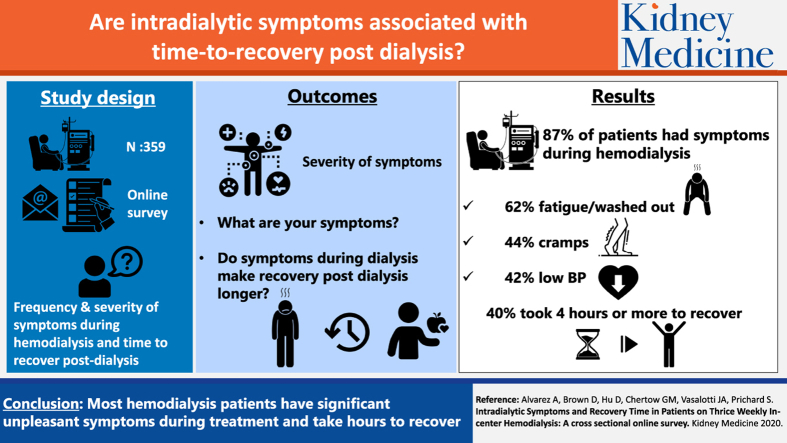
Patients experience various symptoms during hemodialysis. We aimed to assess the frequency and severity of symptoms during hemodialysis and whether intradialytic symptoms are associated with recovery time postdialysis.
Study Design
An online questionnaire was sent to 10,000 patients in a National Kidney Foundation database.
Setting & Participants
Adult patients receiving in-center hemodialysis 3 times weekly for 3 or more months.
Exposure
Online questionnaire.
Analytic Approach
Tabulation of frequency and severity of events and recovery time as percent of respondents, construction of a total symptom score, followed by rank correlation analysis of symptom characteristics with total recovery time.
Outcomes
Patient-reported intradialytic symptoms and recovery time postdialysis.
Results
359 patients met screening criteria and completed the questionnaire. Mean age was 62.5 ± 13.8 years, 207 (58%) were men, 74 (21%) were black/African American, 132 (37%) had diabetes, 252 (70%) had hypertension, and 102 (28%) had a history of myocardial infarction, heart surgery, or stent placement. 311 (87%) patients had symptoms during dialysis in the previous week, with mean severity of 2.7 (range for each symptom, 1-5). The most common symptoms were fatigue/feeling washed out (62%), cramps (44%), and symptoms of low blood pressure (42%). Median time to recovery was 3 (range, 0-24) hours, and this correlated with the incidence and severity of intradialytic symptoms (P < 0.0001). 40% of patients had time to recovery times of 4 hours or longer. 1 in 3 patients reported having stopped dialysis early for intradialytic symptoms and 6% reported skipping dialysis at least once because of intradialytic symptoms.
Limitations
Recall-based self-reported data with a relatively low response rate.
Conclusions
A majority of patients receiving in-center hemodialysis experience symptoms such as feeling washed out, fatigue, and cramping; these may be severe and are correlated with longer recovery time following hemodialysis, as well as shortened and skipped hemodialysis sessions.
Index Words: hemodialysis, symptoms, recovery time
Graphical abstract
Editorial, p. 98
The quality of care of the patient receiving dialysis is largely defined in current practice by the achievement of quantifiable laboratory-based test results, including those related to urea kinetics, anemia, and bone and mineral metabolism, as well as mortality rates and hospitalizations.1,2 Although reflective of the dialysis procedure and outcomes, these metrics are generally unrelated or minimally related to how a patient feels and functions. In recent years, more interest has focused on patient-centered outcomes, including data based on direct feedback from patients.3
During hemodialysis, there are important changes in the concentration of small- and middle-molecular-weight substances, pH, and electrolytes. Moreover, ultrafiltration is often rapid, exceeding rates of vascular refilling.4 Given these rapid changes in biochemistry and volume during dialysis, it is not surprising that patients experience a number of symptoms during and in the period immediately after and a number of hours after hemodialysis.5 Furthermore, treating teams are frequently not aware of the extent of symptoms experienced by their patients during treatments.6
Common intradialytic symptoms include muscle cramps, pruritus, headaches, nausea, and fatigue. Symptomatic hypotension occurs in up to 30% of patients during hemodialysis and patients may cut short their dialysis sessions because of intradialytic symptoms.7, 8, 9, 10, 11 Thus, although hemodialysis is a life-sustaining therapy, adverse effects increase its burden and can materially reduce health-related quality of life, not only during but also after hemodialysis. Understanding the degree to which intradialytic symptoms result in lengthened time to recovery after dialysis or shortening or even skipping dialysis, which can increase the risk for hospitalization and deaths, can clarify the extent of the problem and allow targets for improvement to be set.
The purpose of this study was to assess recovery time postdialysis and the frequency and severity of intradialytic symptoms and determine the association between the presence and severity of intradialytic symptoms with recovery time and the shortening or skipping of hemodialysis.
Methods
An online questionnaire was sent by e-mail to 10,000 patients in a National Kidney Foundation database of patients who have agreed to participate in surveys. The questionnaire was re-sent once to any patients who did not open their e-mails in the first wave. No personal identifying information was collected. The study used the Tonic web-based platform, which is compliant with the Health Insurance Portability and Accountability Act of 1996 (HIPAA).
The questionnaire screened for patients who were 18 years or older, were prescribed in-center hemodialysis 3 days a week, and who had been receiving dialysis for 3 months or more. Self-reported demographic and basic clinical data were collected, including age, sex, race/ethnicity, presence of diabetes, hypertension, and whether taking antihypertensive medication. Dialysis-related data collected included the number of hemodialysis sessions attended in the past week, the prescribed length of the hemodialysis session, hemodialysis vintage or time on dialysis therapy, and the geographic location of the dialysis center. Only patients who reported that they had attended 3 dialysis sessions in the last week and who completed the entire questionnaire were included in the analysis.
A 12-item symptom questionnaire, modified from the Kidney Disease Quality of Life Symptoms and Problems With Kidney Disease scale, addressed the type and severity of symptoms during hemodialysis sessions in the previous week. The symptoms included were fatigue/feeling washed out or drained, low blood pressure/hypotension, cramps, faintness or dizziness, headache, itchy skin, nausea or upset stomach, vomiting, shortness of breath, irregular or “fast/racing” heartbeat, chest pain, and difficulty concentrating/“foggy in the head”.
The number of dialysis sessions with symptoms was calculated. If the patient experienced a symptom during dialysis in the past week, the patient was asked to rate the severity of each of those symptoms during dialysis on a 5-point Likert scale, from 1 being “not severe” to 5 being “very severe.” Respondents who did not report experiencing a particular symptom during dialysis were assigned a symptom level of 0.
A total symptom score was calculated for each patient as the number of symptoms multiplied by the average of the severity of those reported symptoms, meaning that higher scores indicate that the patient had more frequent and/or more severe symptoms than those with a low total symptom score. The presence and severity of symptoms were also cross-classified and analyzed based on 3 dialysis vintage groups: 3 months to 1 year, 1 to 3 years, and longer than 3 years. Chi-square tests were applied to assess the relationship between these variables and dialysis vintage.
In addition, the following questions were asked. (1) “Over the last week, how long did it take you on average to recover from your dialysis sessions and resume your normal, usual activities?” The answer to this question was open ended, meaning that the patient could answer any number of hours up to 24 hours. (2) “Have you ever stopped dialysis early because of symptoms DURING your treatment?” This question offered a yes or no option for the answer. (3) “Please check all symptoms that have caused you to stop dialysis early.” This was followed by the 12 symptoms from the first part of the questionnaire, and the patient ticked off each that had caused him or her to stop dialysis early.
Two hundred fifty patients included in the study responded to the following questions. “Have you ever skipped a dialysis treatment because of symptoms you felt during previous treatments?” This question offered a yes or no option for the answer. “Which symptoms have caused you to skip a dialysis treatment?” This was followed by the 12 symptoms from the first part of the questionnaire and the patient ticked off each that had caused him or her to stop dialysis early.
We used Kendall tau-b coefficient to describe correlations. We conducted all analyses using SAS software, version 9.4, of the SAS system for Windows (SAS Institute, Inc).
Results
Four hundred sixty-four patients responded to the questionnaire. Of those, 393 (85%) patients met the screening inclusion criteria to complete the questionnaire. There were 9 partial responses and 25 patients who were not dialyzed 3 times in the previous week, leaving 359 (77%) completed questionnaires to be included in the analysis.
Average age of the respondents included was 62.5 ± 13.8 years, with a range of 20 to 90 years. Two hundred seven (58%) were men, 238 (66%) were white, and 74 (21%) were black/African American. One hundred thirty-two (37%) reported that they had diabetes, 252 (70%) had hypertension, and 102 (28%) had a history of myocardial infarction, heart surgery, or percutaneous coronary intervention with stent placement. Additional demographic data are shown in Table 1. Overall, the patient population was broadly representative of the US dialysis patient population as reported in the US Renal Data System. The subgroup of 250 patients who answered the additional questions and the groups divided based on recovery time are similar to the overall group.
Table 1.
Patient Demographics and Characteristics
| Full Response Group | Respondents to Additional Questions | Recovery Time 0-3 h | Recovery Time 3-6 h | Recovery Time 6-12 h | Recovery Time 12+ h | |
|---|---|---|---|---|---|---|
| Age, y (mean ± SD) [range] | 62.5 ± 13.8 [20-90] | 62.3 ± 13.8 [22-90] | 61.8 ± 14.2 [22-90] | 63.9 ± 13.6 [20-89] | 60.9 ± 12.8 [34-89] | 63.8 ± 13.0 [27-88] |
| Count (%) | Count (%) | Count (%) | Count (%) | Count (%) | Count (%) | |
|---|---|---|---|---|---|---|
| Sex (women) | 152 (42.3%) | 112 (44.8%) | 83 (42.8%) | 30 (40.0%) | 21 (42.9%) | 18 (43.9%) |
| Diabetic | 132 (36.8%) | 84 (33.6%) | 76 (39.2%) | 23 (30.7%) | 13 (26.5%) | 20 (48.8%) |
| Heart attack surgery or stent | 102 (28.4%) | 65 (26.0%) | 59 (30.4%) | 17 (22.7%) | 14 (28.6%) | 12 (29.3%) |
| HBP | 252 (70.2%) | 158 (63.2%) | 141 (72.7%) | 48 (64.0%) | 32 (65.3%) | 31 (75.6%) |
| If yes, % on HBP medication | 247 (98.0%) | 153 (96.8%) | 140 (99.3%) | 47 (97.9%) | 30 (93.8%) | 30 (96.8%) |
| Time on dialysis | ||||||
| 3 mo-1 y | 62 (17.3%) | 35 (14.0%) | 39 (20.1%) | 7 (9.3%) | 7 (14.3%) | 9 (22.0%) |
| 1-3 y | 153 (42.6%) | 105 (42.0%) | 87 (44.8%) | 33 (44.0%) | 21 (42.9%) | 12 (29.3%) |
| >3 y | 144 (40.1%) | 110 (44.0%) | 68 (35.1%) | 35 (46.7%) | 21 (42.9%) | 20 (48.8%) |
| Racea | ||||||
| Black/African American | 77 (21.5%) | 48 (19.2%) | 46 (23.7%) | 12 (16.0%) | 8 (16.3%) | 11 (26.8%) |
| White | 244 (68.0%) | 172 (68.8%) | 129 (66.5%) | 53 (70.7%) | 34 (69.4%) | 28 (68.3%) |
| Other | 49 (13.7%) | 40 (16.0%) | 23 (11.9%) | 14 (18.7%) | 9 (18.4%) | 3 (7.3%) |
| Machine | ||||||
| Fresenius | 203 (56.6%) | 142 (56.8%) | 117 (60.3%) | 42 (56.0%) | 30 (61.2%) | 14 (34.1%) |
| Phoenix | 1 (0.3%) | 1 (0.4%) | 0 (0.0%) | 0 (0.0%) | 1 (2.0%) | 0 (0.0%) |
| I do not know | 136 (37.9%) | 94 (37.6%) | 69 (35.6%) | 29 (38.7%) | 15 (30.6%) | 23 (56.1%) |
| Other | 19 (5.3%) | 13 (5.2%) | 8 (4.1%) | 4 (5.3%) | 3 (6.1%) | 4 (9.8%) |
| Region | ||||||
| Northeast | 56 (15.6%) | 45 (18.0%) | 23 (11.9%) | 16 (21.3%) | 7 (14.3%) | 10 (24.4%) |
| Midwest | 122 (34.0%) | 90 (36.0%) | 66 (34.0%) | 27 (36.0%) | 17 (34.7%) | 12 (29.3%) |
| South | 103 (28.7%) | 63 (25.2%) | 64 (33.0%) | 15 (20.0%) | 15 (30.6%) | 9 (22.0%) |
| West | 78 (21.7%) | 52 (20.8%) | 41 (21.1%) | 17 (22.7%) | 10 (20.4%) | 10 (24.4%) |
Note: Full response group, n = 359; respondents to additional questions, n = 250; recovery time 0-3 hours, n = 194; recovery time 3-6 hours, n = 75; recovery time 6-12 hours, n = 49; recovery time 12+ hours, n = 41. Values given as number (percent) unless otherwise noted.
Abbreviations: HBP, high blood pressure; SD, standard deviation.
Survey allowed more than 1 selection.
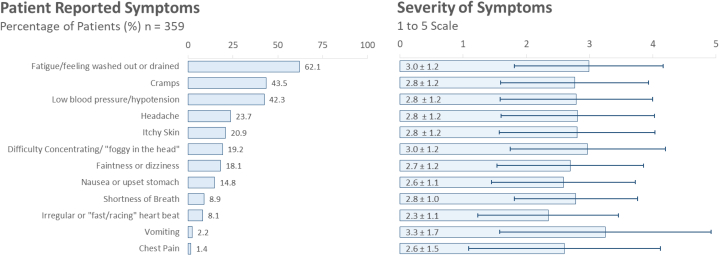
Three hundred eleven (87%) patients had symptoms during hemodialysis in the previous week. Figure 1 shows the frequency of occurrence and severity for each of the 12 symptoms included in the questionnaire. The most common symptoms are fatigue/washed out or drained (62%), cramps (44%), and low blood pressure (42%). The overall average severity of reported symptoms was rated as 2.7 ± 2.0. Chi-square tests showed no relationship between these variables and dialysis vintage.
Figure 1.
Prevalence and severity of reported symptoms. (Left panel) Percent of patients who report having each of the 12 symptoms in the questionnaire during their 3 dialysis sessions in the previous week. (Right panel) Mean severity reported for each of the 12 symptoms.
Thirty-three percent of patients reported stopping dialysis at some time because of symptoms they experienced during treatment. Cramps (19%) and low blood pressure (14%) were the 2 most common reasons for terminating dialysis early.
The number of symptoms reported by patients is shown in Figure 2. Almost 30% reported having 4 or more symptoms during dialysis. Of those reporting symptoms, 73% had symptoms on 2 or more treatment days in the week and 53% had symptoms on all 3 treatment days.
Figure 2.
Percent of patients by number of symptoms per patient.
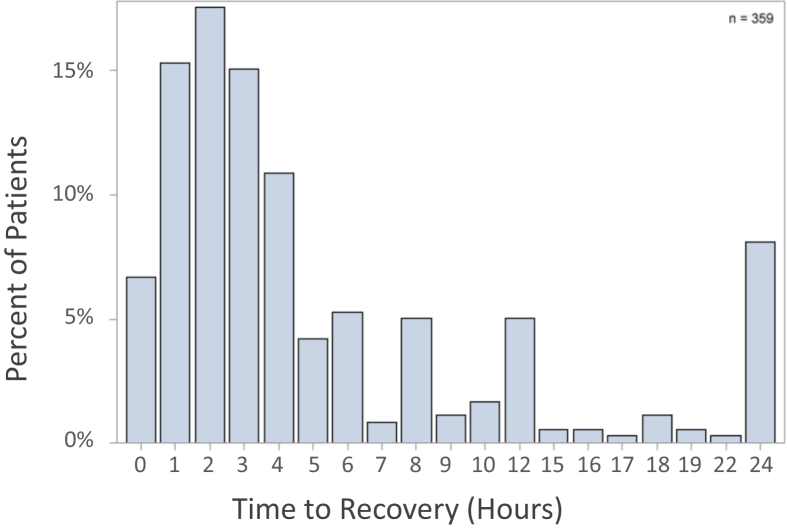
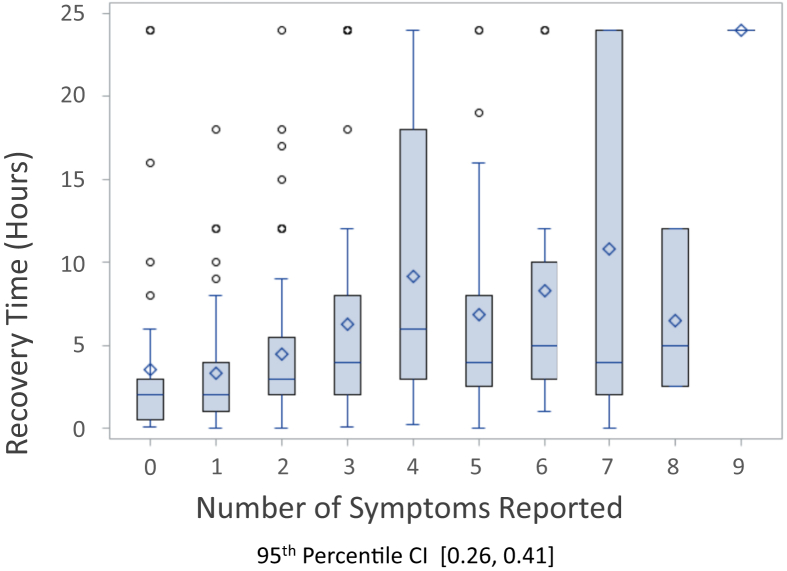
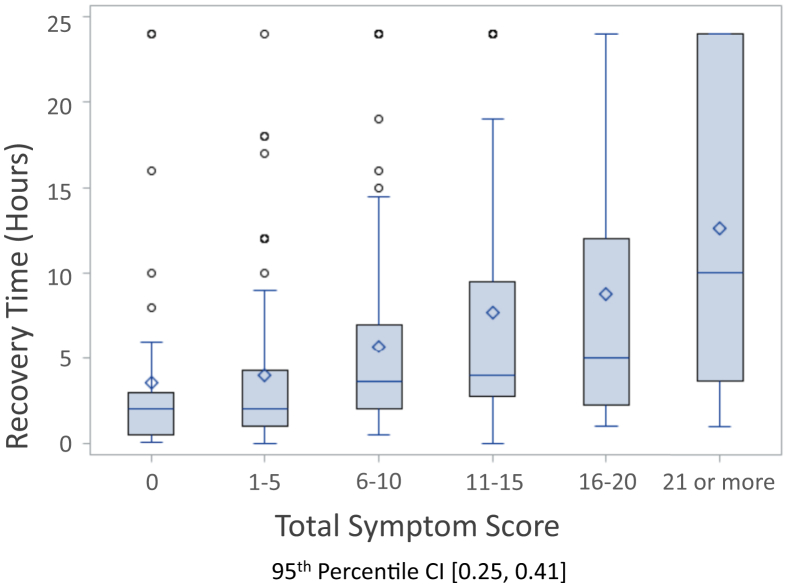
Figure 3 shows the distribution of time to recovery. Median recovery time was 3 hours, with a range of 0 to 24 hours. Recovery time was 4 hours or longer in 40% of patients. Figure 4 shows the association of recovery time to the number of intradialytic symptoms, and Figure 5 shows the association of time to recovery to the total symptom score. There were moderate correlations between recovery time and number of symptoms during dialysis. The 95% confidence interval (CI) is 0.26 to 0.41 for recovery time versus number of symptoms, and the 95% CI range is 0.25 to 0.41 for the recovery time versus total symptom score. No symptom exhibited a statistically stronger relationship to recovery time.
Figure 3.
Recovery time postdialysis.
Figure 4.
Relationship of recovery time versus number of symptoms. The correlation coefficient of recovery time as a function of number of symptoms per patient is 0.275 (P < 0.0001). Abbreviation: CI, confidence interval.
Figure 5.
Relationship of recovery time versus total symptom score. Total symptom score for each patient was calculated by number of symptoms multiplied by the average severity of the symptoms. The correlation coefficient of recovery time as a function of the total symptom score is 0.279 (P < 0.0001). Abbreviation: CI, confidence interval.
Two hundred fifty respondents also answered the question “Have you ever skipped a dialysis treatment because of symptoms you felt during previous treatments?” Sixteen patients (6%) reported having skipped dialysis at some point because of symptoms during dialysis.
Discussion
A majority of patients receiving in-center hemodialysis experience symptoms such as feeling washed out, fatigue, and cramping. These may be severe and are correlated with longer recovery time following hemodialysis, as well as shortened and skipped hemodialysis sessions. This study details the frequency and severity of self-reported symptoms during hemodialysis in a current broad-based group of patients in the United States. In the same patients, we report recovery time postdialysis and the association of frequency and severity of symptoms with recovery time.
The high frequency of symptoms during hemodialysis is not surprising given the rapid flux of solutes and rapid ultrafiltration that take place during the therapy. The results highlight some of the challenges faced by this patient population. The literature on dialysis outcomes is dominated by mortality and hospitalization rates, vascular access issues, infectious complications, and cardiovascular events.1 This study highlights that the burden of symptoms during dialysis itself should be considered an important outcome to measure and should be a target for further innovation. As improvements in dialysis technology are introduced, a measurement of success can reasonably be expected to include an improvement in intradialytic syndrome.
Recovery time postdialysis has been found to be a simple health-related quality-of-life question that is reliable and valid.12 It is also a measure of overall quality of life in dialysis patients that is associated with mortality rates.13 In this study, there is a direct correlation between the number of symptoms during hemodialysis and total symptom score and recovery time. Improving the dialysis experience for patients should be targeted at reducing these symptoms, which could be expected to also reduce recovery time postdialysis.
Observational and randomized trial data have shown that longer session length or more frequent or nocturnal hemodialysis prescriptions are associated with shortened recovery time and fewer symptoms during treatments.14, 15, 16 Strategies to reduce the incidence of intradialytic symptoms and reduce recovery time need to be developed for conventional thrice-weekly hemodialysis. These strategies might include modest extension of dialysis time, limits on ultrafiltration rates, alterations in dialysate composition or flow rates, slower blood flow rates, changes in dialysate temperature, and changes in diet or medications. Further studies to assess such interventions should be undertaken. The effect of these modifications on other important end points such as hospitalization and other health events should also be assessed.
Notably, patients indicate that symptoms experienced during hemodialysis can lead to shortened and skipped therapies, which can lead to many adverse consequences and events. Nonadherence among dialysis patients has been documented in dialysis17 and previous studies indicate that shortened and skipped therapies are associated with higher mortality and hospitalization rates.18,19 The reasons for skipped dialysis include transportation issues, concurrent illness, and conflicting social events. Although dialysis symptoms are reported to account for a relatively modest 6% of skipped dialysis sessions, when added to the other causes, the effect of dialysis symptoms on adherence is important. Therefore, if improving the dialysis experience could reduce skipped or shortened dialysis treatments, it has the potential to improve outcomes. Overall in this group of patients, the rate of skipping or shortening dialysis is low. This may reflect that they are generally more motivated to be adherent and also accounts for their willingness to participate in studies such as this one. The data do not allow one to draw conclusions in this regard.
There are several important limitations to this study. The low response rate to the e-mail request to complete the questionnaire, together with the need to eliminate a number of respondents because of screening criteria and incomplete answers, resulted in an overall rate of survey completion <5%. It is possible that respondents were more likely to have symptoms they wished to report and emphasize. That noted, the sample included a broad range of patients by age, sex, race/ethnicity, and comorbid conditions, consistent with the general US in-center hemodialysis population. This study may not be generalizable to the populations treated with in-center hemodialysis more or less frequently than thrice weekly or to those treated with home hemodialysis. Although the questionnaire certainly has face validity, neither the questionnaire itself nor the method of administration (web-based) has been formally validated. However, it is noteworthy that the frequency with which the symptoms are reported in this study is consistent with previously reported data,6 which gives additional credibility to these results.
In summary, conventional thrice-weekly in-center hemodialysis is associated with a number of adverse intradialytic symptoms in a vast majority of patients. Recovery time postdialysis can be prolonged and is directly correlated with the incidence and severity of intradialytic symptoms. Intradialytic symptoms can be associated with shortened or skipped dialysis sessions. Adequacy of dialysis could be expanded to include the severity of intradialytic symptoms, and improvement in intradialytic symptoms should be a target of innovation in hemodialysis care.
Article Information
Authors’ Full Names and Academic Degrees
Luis Alvarez, MD, PhD, Deborah Brown, BA, Dean Hu, MSc, Glenn M. Chertow, MD, Joseph A. Vasalotti, MD, and Sarah Prichard, MD.
Authors’ Contributions
Research idea and study design: DB, SP; data acquisition: DB; data analysis/interpretation: DH, SP; supervision or mentorship: GMC, JAV, SP. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Support
This study was supported by Outset Medical. The funder, Outset Medical, played a role in the study design, data collection, analysis, and decision to publish in consultation with National Kidney Foundation representatives.
Financial Disclosure
Dr Alvarez and Mr Hu are employees of Outset Medical. Dr Prichard is an advisor to Outset Medical.
Acknowledgements
The authors thank Anthony Gucciardo and Gail Torres, RN, of the National Kidney Foundation for working with the investigators to develop the questionnaire and for sending the e-mails with the questionnaire to patients in their database; Ashley Wu and Logan Rivas for technical support of the platform and analysis of the responses; STATKING for their support and expertise in doing the statistical analyses; and all the patients who took the time to reply to the questionnaire.
Peer Review
Received April 14, 2019. Evaluated by 2 external peer reviewers, with direct editorial input from the Statistical Editor, an Associate Editor, and the Editor-in-Chief. Accepted in revised form October 19, 2019.
Footnotes
Complete author and article information provided before references.
References
- 1.Saran R., Robinson B., Abbott K.C. US Renal Data System 2017 Annual Data Report: epidemiology of kidney disease in the United States. Am J Kidney Dis. 2018;71(3 suppl 1) doi: 10.1053/j.ajkd.2018.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Danquah F.V.N., Zimmerman L., Diamond P.M. Frequency, severity, and distress of dialysis-related symptoms reported by patients on hemodialysis. Nephrol Nurs J. 2010;37:627–638. [PubMed] [Google Scholar]
- 3.Caplin B., Kumar S., Davenport A. Patients’ perspective of haemodialysis-associated symptoms. Nephrol Dial Transplant. 2011;26:2656–2663. doi: 10.1093/ndt/gfq763. [DOI] [PubMed] [Google Scholar]
- 4.Nissenson A. Improving outcomes for ESRD patients: shifting the quality paradigm. Clin J Am Soc Nephrol. 2014;9(2):430–434. doi: 10.2215/CJN.05980613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Flythe J.E., Assimon M.M., Wenger J.B., Wang L. Ultrafiltration rates and the quality incentive program: proposed measure definitions and their potential dialysis facility implications. Clin J Am Soc Nephrol. 2016;11(8):1422–1433. doi: 10.2215/CJN.13441215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weisbord S.D., Fried L.F., Mor M.K. Renal provider recognition of symptoms in patients on maintenance hemodialysis. Clin J Am Soc Nephrol. 2007;2:960–967. doi: 10.2215/CJN.00990207. [DOI] [PubMed] [Google Scholar]
- 7.Assimon M.M., Flythe J.E. Intradialytic blood pressure abnormalities: the highs, the lows and all that lies between. Am J Nephrol. 2015;42:337–350. doi: 10.1159/000441982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dinesh K., Kunaparaju S., Cape K. A model of systolic blood pressure during the course of dialysis and clinical factors associated with various blood pressure behaviors. Am J Kidney Dis. 2011;58(5):794–803. doi: 10.1053/j.ajkd.2011.05.028. [DOI] [PubMed] [Google Scholar]
- 9.Shoji T., Tsubakihara Y., Fujii M., Imai E. Hemodialysis-associated hypotension as an independent risk factor for two-year mortality in hemodialysis patients. Kidney Int. 2004;66:1212–1220. doi: 10.1111/j.1523-1755.2004.00812.x. [DOI] [PubMed] [Google Scholar]
- 10.Sands J.J., Usvyat L.A., Sullivan T. Intradialytic hypotension: frequency, sources of variation and correlation with clinical outcome. Hemodial Int. 2014;18:415–422. doi: 10.1111/hdi.12138. [DOI] [PubMed] [Google Scholar]
- 11.Kuipers J., Oosterhuis J.K., Krijnen W.P. Prevalence of intradialytic hypotension, clinical symptoms and nursing interventions - a three-months, prospective study of 3818 haemodialysis sessions. BMC Nephrol. 2016;17:21. doi: 10.1186/s12882-016-0231-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lindsay R.M., Heidenheim P.A., Nesrallah G. Minutes to recovery after a hemodialysis session: a simple health-related quality of life question that is reliable, valid, and sensitive to change. Clin J Am Soc Nephrol. 2006;1:952–959. doi: 10.2215/CJN.00040106. [DOI] [PubMed] [Google Scholar]
- 13.Rayner H.C., Zepel L., Fuller D.S. Recovery time, quality of life, and mortality in hemodialysis patients: the Dialysis Outcomes and Practice Patterns Study (DOPPS) Am J Kidney Dis. 2014;64(1):86–94. doi: 10.1053/j.ajkd.2014.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Garg A.X., Suri R.S., Eggers P. Patients receiving frequent hemodialysis have better health-related quality of life compared to patients receiving conventional hemodialysis. Kidney Int. 2017;91:746–754. doi: 10.1016/j.kint.2016.10.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jaber B.L., Lee Y., Collins A.J. Effect of daily hemodialysis on depressive symptoms and postdialysis recovery time: interim report from the FREEDOM (Following Rehabilitation, Economics and Everyday-Dialysis Outcome Measurements) Study. Am J Kidney Dis. 2010;56(3):531–539. doi: 10.1053/j.ajkd.2010.04.019. [DOI] [PubMed] [Google Scholar]
- 16.Morfin J.A., Fluck R.J., Weinhandl D.E. Intensive hemodialysis and treatment complications and tolerability. Am J Kidney Dis. 2016;68(5 suppl 1):S43–S50. doi: 10.1053/j.ajkd.2016.05.021. [DOI] [PubMed] [Google Scholar]
- 17.Chan K.E., Thadhani R.I., Maddux F.W. Adherence barriers to chronic dialysis in the United States. J Am Soc Nephrol. 2014;25:2642–2648. doi: 10.1681/ASN.2013111160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Obialo C.I., Hunt W.C., Bashir K., Zager P.G. Relationship of missed and shortened hemodialysis treatments to hospitalization and mortality: observations from a US dialysis network. Clin Kidney J. 2012;5:315–319. doi: 10.1093/ckj/sfs071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Saran R., Bragg-Gresham J.L., Rayner H.C. Nonadherence in hemodialysis: associations with mortality, hospitalization, and practice patterns in the DOPPS Kidney. Int. 2003;64:254–262. doi: 10.1046/j.1523-1755.2003.00064.x. [DOI] [PubMed] [Google Scholar]