Abstract
Objectives
To identify the shared research priorities of patients, caregivers and multidisciplinary renal health and social care professionals across Wales for integrated renal health and social care in Wales.
Design
Research priority setting exercise adapted from the James Lind Alliance national priority setting partnership framework in UK healthcare.
Setting
Two workshops: one in North Wales with patients, caregivers and multidisciplinary renal health and social care professionals and one in South Wales with the Welsh Renal Clinical Network (commissioners of renal services in Wales). Additional input provided from stakeholders via email correspondence and face to face communications.
Participants
Academics n=14, patients n=16, family/carers n=6, multidisciplinary renal healthcare professionals n=40, local authority councils n=3, renal charities n=6 wider third sector organisations n=8, renal industries n=4, Welsh government social care n=3, renal service commissioners n=8.
Results
38 research priority questions grouped into 10 themes were agreed. The themes included: (1) integrating health and social care, (2) education, (3) acute kidney injury, (4) chronic kidney disease and cardiovascular disease, (5) transplantation, (6) dialysis, (7) personalised medicines, (8) cross-cutting priorities, (9) specific social contexts and (10) transitional services and children. Research questions were broad and covered a range of health and social care topics. Patient and professional perspectives broadly overlapped. Research priority setting activities revealed gaps in knowledge in overall service provision and potential areas for service improvement.
Conclusions
Mapping priorities in health services and social care highlighted the research needed to support renal health services delivery and commissioning in Wales.
Keywords: nephrology, social medicine, health services administration & management
Strengths and limitations of this study.
First pan Wales priority setting exercise with a focus on renal health services and social care.
Views and perspectives collated from over 120 participants across Wales.
Views and perspectives of people living with kidney disease, family members and the wider social care sector were included.
The focus was limited to health services and social care research in renal disease and did not include biomedical priorities.
Background
Chronic kidney disease (CKD) affects 6%–8% of the Welsh population (around 200 000 people).1 More than 3000 people are currently being treated for kidney failure in Wales with this number increasing year on year,2 and one in five people admitted to a hospital in Wales will have a serious problem with their kidneys as part of their illness.3
Wales is part of the UK with a devolved healthcare system and a population of around 3 million. In Wales multidisciplinary teams (MDTs) provide health and social care to patients with CKD (table 1). Multidisciplinary renal teams are involved in all aspects of patient health and social care from decision making about treatment options to lifestyle adjustments and ongoing social services support.
Table 1.
Members of multidisciplinary renal health and social care teams
| Specialist multidisciplinary renal healthcare professionals | Social care and community professionals |
|
|
Cross-cutting
| |
NHS, National Health Service.
CKD has no cure and can have a considerable impact on patients health (eg, multiple comorbidities, greater risks of infection and frailty), well-being (eg, depression, anxiety, isolation), quality of life (eg, frequent dialysis sessions, reduced mobility, unemployment) and family relationships (eg, perceptions of burden, guilt, shame, intimacy).4 5 Years of living with CKD have different burdens depending on the person, for example, age, socioeconomic status, gender and care and support at home.6 7 In Wales, health policies are integrated with social care and recent policy agendas are seeking to address the social contexts of chronic conditions first in order to reduce and relieve burdens on healthcare systems.8 Yet research in these areas is overall lacking in the context of a Welsh health and social care system, and as a consequence patient and family involvement in research priority setting for health services and the social contexts of kidney disease has yet to be established. Therefore, current research may not be addressing questions that are meaningful and important to patients and their families. In addition, we do not yet know which health services and social care contexts of living with kidney disease matter the most to patients and family members.
Recent research priority setting in chronic conditions in children recognises a real gap in the priorities of the healthcare providers and patients and family9 and a 2015 systematic review of research priority setting in kidney disease found that only 4/16 studies (25%) explicitly involved patients and inconsistencies in reporting and transparency of engagement with patients, the public and healthcare professionals.10 At the same time priority setting exercises with patients with CKD in Canada around predialysis successfully identified top research priorities for health professionals and patients11 and in a 2-year follow-up found that patients still agreed with the overall priorities and were able to see past individual needs and balance these with greater research potential impacts.12
Welsh renal health, social care and research context
Since 2015, researchers from the Wales Kidney Research Unit (WKRU) have been developing an integrated portfolio of research in health services and social care.13 A part of the development established greater links with the Welsh Renal Clinical Network who are responsible for planning and monitoring adult renal services in Wales on behalf of the Welsh population and National Health Service (NHS) Wales.14 Figure 1 lists the main responsibilities of the Welsh Renal Clinical Network (figure 1).
Figure 1.
Welsh Renal Clinical Network roles and responsibilities. NHS, National Health Service.
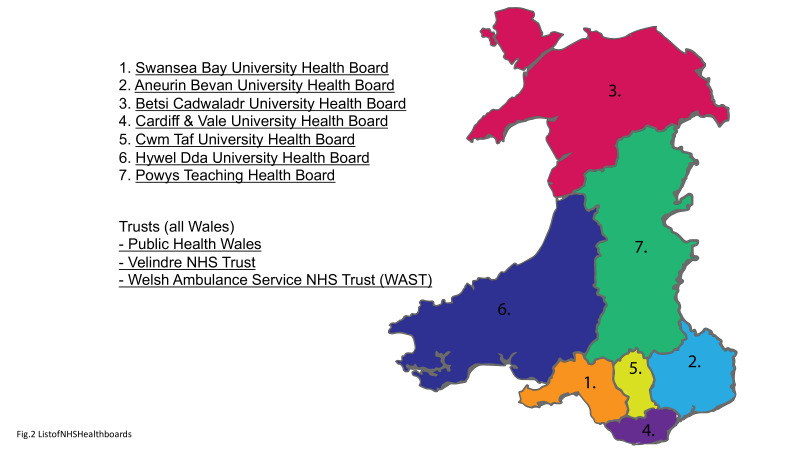
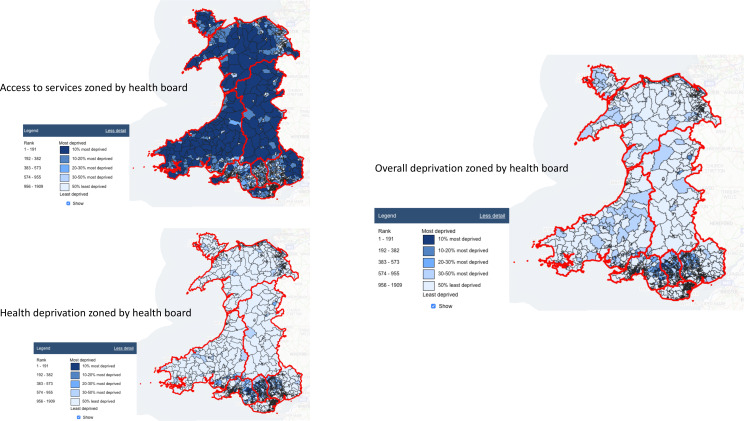
Wales devolved healthcare system is made up of seven health boards and three trusts (figure 2). Wales has higher levels of deprivation than England and the population is older and sicker than the rest of the UK.15 16 The majority of the population reside in areas in North and South Wales17 with overall deprivation higher in these areas18 (figure 3). In Wales, overall deprivation is measured by; employment, health, education, access to services, community safety, physical environment and housing. On the whole these individual measures generally map onto the overall deprivation score accept for ‘access to services’ which appears as the mirror opposite of deprivation (figure 4).
Figure 2.
List of NHS health boards. NHS, National Health Service.
Figure 3.
Wales population and deprivation mapping.
Figure 4.
Deprivation map (overall and health) and access to services map zoned by health board.
Looking at the landscape of Wales as a whole we wanted to best capture the views and opinions of people living with kidney disease on health services and social care research. Rather than focus on a stage of CKD, or a type of kidney disease or dialysis modality, we wanted to frame the initial discussions around the categories of deprivation and the recent policy contexts and agendas in Wales in social care, for example, The Social Services and Well-being (Wales) Act19 and Care and support at home in Wales strategic plan 2017–2022.8
In addition to learning from people living with kidney disease and family members we wanted to establish greater links with the Wales Renal Clinical Network, as the commissioners of renal services in Wales, to learn about the ways research could support their agenda in the short, medium and long term. We specifically wanted to align where appropriate the networks strategic service improvement plan with the WKRU priority social care agenda.
In this paper, we report on the outcomes from the first national research priority setting exercise in renal health services and social care in Wales.
Aim
To establish an agreed list of research priorities in integrated renal health and social care research in Wales (2020–2025).
In undertaking this research priority setting exercise we also wanted to:
Capture the priorities of the multiple MDTs in particular professionals allied to medicine (Allied Health Professionals, AHPs) and the social care sector. These perspectives tend to be overshadowed or missed completely in favour of health-related outcomes in published research.
Avoid any potential mismatch between the multiple MDTs and patients and family members. As there are so many MDTs each with a distinct focus on patient care, it was critical that we were able to align professional priorities with patients and family members.
Produce priorities that had a distinct focus on health services commissioning and social care research. We felt this was an important match, to connect where possible the views of the Welsh Renal Clinical Network with patients and family members to jointly benefit research and health services planning and delivery.20
Encourage wider and greater patient involvement in research from across Wales. We wanted to use this exercise to stimulate interest and increase capacity in non-clinical renal research.
Methods
We adapted the James Lind Alliance (JLA) processes21 for our local Welsh context (see table 2). We facilitated two innovative and bespoke workshops, engaged in face-to-face consultations and email correspondence with professionals, patients, family members and wider social care services in North and South Wales. The first modified priority setting workshop was hosted in North Wales with the South Wales workshop arranged after outcomes from North Wales had been analysed.
Table 2.
Mapping the James Lind priority setting partnership against workshop 1 and workshop two activities
| James lind priority setting partnership activity | Interpreted for workshop 1: the ‘Social Care Innovation Lab’ SCIL north wales | Interpreted for workshop 2: setting priorities with the Welsh Renal Clinical Network. | |
| 1. | Create a Steering Group. Composed with equal representation of patients, carers and clinicians, this group agrees the plan of action or ‘protocol’ and takes responsibility for the Priority Setting Partnership (PSP). | Summer 2017, began planning an ‘Innovation Research Ideas in Kidney Health and Social Care’ event with; the Wales Kidney Research Unit (WKRU), Wales School for Social Care Research (WSSCR) and the National Centre for Population Health and Well-being Research (NCPHWR) in partnership with the Centre for Ageing and Dementia Research (CADR). Organisations have a wealth of experience, expertise and diverse representation (including patients) from various background with various health conditions. We agreed to host an SCIL as part of the event developed by WSSCR and CADR to best capture the range of views, professions and expertise and to deliver the exercise within time and resource constraints.27 | The WKRU has an executive board with core representatives from patients, clinicians, academics and independent advisors. The network manager and lead nurse for Wales after attending the SCIL were invited to the annual Wales Kidney Research Unit executive meeting where it was agreed to host a priority setting workshop with the Wales Renal Clinical Network. The Wales Kidney Research Unit would take responsibility for the priority setting exercise. |
| 2. | Gather evidence uncertainties. By asking patients, carers and clinicians to respond to a survey asking what questions they have for research, and by searching existing literature to find evidence gaps | SCIL: 2 hours repeat afternoon sessions where an interdisciplinary group of patients, family members, renal health and social care professionals and wider third sector organisations and industry (n=20×2) were asked to identify and agree the key social care research priorities in kidney disease in Wales. SCILs were structured in such a way to make discussing social care easy and accessible for all and to find novel solutions to the complex problems and puzzles that social care services present. Presentations, small group work, posit notes and flip charts, and feedback were used to elicit responses. The purpose of the labs was to bring together the kidney health and social care sector, including the wider social care sector to identify shared research priorities. | A review of the current research priorities in key documents in renal healthcare in the UK were undertaken, including National Institute for Health and Care Excellence (NICE), The UK renal research strategy, outcomes from the SCIL and additional consultation work with stakeholders (including patients) undertaken by the authors as part of the WKRU. |
| 3. | Summarising the responses gathered. With the help of an Information Specialist, the PSP sorts all the responses and creates summary questions. This becomes the long list of summary questions. | SCI divided into three parts:
|
A long list of research priorities was drawn up taken from key documents in renal health and social care and shared prior to the meeting. five worksheets were prepared and shared:
The worksheets also included reminders taken from the Welsh Renal Clinical Network Renal Services in Wales 2016–2020 delivery plan and Health and Care Research Wales commitments to integrating research into clinical provision and building research capacity in the field. 106 research questions, topics, themes and areas were identified. |
| 4. | Evidence checking. The long list of summary questions is checked against existing research evidence to ensure they are true uncertainties. Any questions that have already been answered by research are removed. | Previous research undertaken by the Wales Kidney Research Unit, revealed almost no published research from social care perspectives in the UK and none in Wales. Priorities identified were not always in the form of a research question and rather indicated overall research areas. Wales Kidney Unit Researchers undertook minor edits to develop research questions out of the top priorities. A summary of the SCIL including detailed outcomes in tables and word clouds were sent to all the delegates following the meeting. We asked for any additional feedback and explained that we intended to use outcomes from the SCIL in an additional workshop. A copy of the full report and outcomes from the workshop is available in online supplementary file 1. At this point we turned our attention to organising a workshop with the Wales Clinical Renal Network in order to complete the exercise. |
4.5.6. were undertaken via a workshop with the Welsh Renal Clinical Network.
|
| 5. | Interim priority setting. To reduce the remaining long list of summary questions to a shorter list so they can be discussed at a workshop, a wide range of patients, carers and clinicians are asked to vote on the most important questions in an interim priority setting survey. This is usually via an online ranking survey. | n/a | |
| 6. | Workshop. The highest ranked 25–30 questions from the interim priority setting survey are discussed in a workshop of patients, carers and clinicians who together agree the ‘top 10’ list of priorities. | n/a | |
| 7. | Publish and promote top 10 research priorities top 10 is announced and published on the JLA website and promoted to researchers and funders. The Priority Setting Partnership works with researchers and funders to further develop the priorities into specific research questions. | n/a | 7. Following journal publication we will publish the results on the website and promote at Wales Kidney Research Unit and partner events across Wales. |
JLA, James Lind Alliance; n/a, not applicable.
bmjopen-2020-036872supp001.pdf (13.9MB, pdf)
Workshop 1: the ‘Social Care Innovation Lab’ North Wales
In March 2018 the WKRU, Wales School for Social Care Research and the National Centre for Population Health and Well-being Research jointly hosted an ‘Innovating Research in Kidney Health and Social Care’ event in North Wales. In preparation, we reviewed the ways the JLA model had been adapted and applied in various contexts including a national CKD priority setting workshop in Australia which was able to identify and agree priorities in a single workshop saving on resources, costs and feasibility.22 While Tong et al acknowledged the potential limitations of this largely quantitative approach compared with prolonged stakeholder engagement designed to extract more nuanced results and higher quality of questions, they deemed it necessary in order to extract priorities that represent national priorities in a diverse population and in a vast landscape. We explain our adapted and modified JLA priority setting exercise and map it against the original JLA priority setting exercises in table 2.
Sampling
Delegates were purposively sampled from WKRU contacts and invited from across Wales to reach maximum variation. Our target was 80 participants based on venue capacity and resources. Box 1 summaries the sample.
Box 1. A summary of the sample for the social care innovation laboratory workshops.
Health professionals (clinicians and nurses).
Professionals allied to medicine (renal dietician, renal occupational therapist, renal psychologists).
Renal social workers.
Renal charities (Kidney Wales, Paul Popham Fun, Polycystic Kidney Disease Charity, Kidney Care UK).
Wider Social care sector (eg, Diabetes Cymru, Shelter Cymru, Age Connect).
Local council representatives (eg, Gwynedd Council, Conwy Council, Flintshire Council).
Welsh government.
Welsh Renal Clinical Network, lead Nurse and Network manager.
Academics.
People living with kidney disease, family and friends.
We offered to pay expenses for travel to all participants and stopped inviting participants when the guest list reached 100. Of the 100 registered 81 attended the conference, 62% were female and 38% male, all were adults. Of 81, 14 (17.3%) were people living with kidney disease and family members. A detailed list of attendees is available in table 3.
Table 3.
Full list of participants involved in stages of the priority setting
| List of attendees for North Wales conference and innovation lab | ||
| Occupation | Region | N |
| University staff | ||
| Academics (exercise psychology, health psychology, sociology, child health, methodologies, biomedical sciences, nursing and rehabilitation, cognitive functioning and ageing, social care, healthcare, ageing and dementia, national centre for population health and well-being research, primary care research) | North Wales | 10 |
| Academics: immunology, fundamental disease mechanisms | South Wales | 2 |
| Academic knowledge exchange affiliate mapping the psycho/social renal workforce | UK | 1 |
| NHS engagement officer | North Wales | 1 |
| Patients, family members and friends | ||
| People living with kidney disease | North Wales | 11 |
| Family and friends of people living with kidney disease | North Wales | 3 |
| Multidisciplinary renal teams North Wales | ||
| Renal social worker | North Wales | 3 |
| Renal clinical psychologists | North Wales | 2 |
| Renal nurses; ward nurses (3), predialysis clinical nurse specialists (5), research nurse (1), renal nurses (2), home therapies specialist nurses (1) | North Wales | 12 |
| Renal pharmacist | North Wales | 1 |
| Renal service manager | North Wales | 1 |
| Renal consultants and registrars | North Wales | 5 |
| Renal unit managers (Bbraun) | North Wales | 1 |
| Renal dietician | North Wales | 1 |
| Multidisciplinary renal teams South Wales | ||
| Renal social worker | South Wales | 1 |
| Renal youth worker | South Wales | 1 |
| Lead renal nurse managers | South Wales | 2 |
| Renal Physiotherapist | South Wales | 1 |
| Anaemia lead nurse | South Wales | 1 |
| Renal registrars | South Wales | 1 |
| Renal technical services and analysts | South Wales | 2 |
| Local authorities | ||
| Community Health Council (Conwy) | North Wales | 1 |
| Local County Councils (Flintshire, Denbighshire) | North Wales | 2 |
| Renal charity providers | ||
| Renal charities; Kidney Wales, Paul Popham Renal Fund, Kidney Care UK, Polycystic Kidney Disease, | Pan Wales | 4 |
| Wider third sector | ||
| Wider third sector, for example, Age Connect North Wales Central, Holistic Therapies, Citizens Advice Bureau, Carers Wales, Sign-Sight and Sound, Alternative Futures Innovation Labs, local council authorities | North Wales | 8 |
| Industry | ||
| Industry, for example, Renal Services, Bbraun, Baxter, Fresenius | UK | 4 |
| Welsh Government and commissioners | ||
| Welsh Government Health and Care Research Wales Representatives | Pan Wales | 1 |
| Welsh Government, Wales Renal Clinical Network Commissioners | Pan Wales | 2 |
| Wales Renal Clinical Network (WRCN) Priority Setting Workshop | ||
| Welsh Renal Clinical Network Commissioners | Pan Wales | 8 |
| Additional consultation via email and face to face | ||
| People living with kidney disease | South Wales | 5 |
| Family and friends of people living with kidney disease | South Wales | 3 |
| Renal charity professionals | South Wales | 2 |
| Multidisciplinary renal professionals | South Wales | 5 |
Invites were sent out via emails, telephone calls and face-to-face communications. We focused patient and family member recruitment to the North Wales area due to travel restrictions experienced by many people living with kidney disease. We also targeted the local wider third sector organisations via google map searchers and follow-up telephone calls. The multidisciplinary renal teams were however invited from across Wales. We felt it important to aim to get as many of the professionals in one room and they are more familiar with commuting for joint meetings and events. The venue selected was in a neutral location not associated with the NHS or the University (Venue Cymru in Llandudno) but very familiar to the local communities.23
The complete summary report of the Social Care Innovation Lab is available in online supplementary file 1.
Workshop 2: setting priorities with the Welsh Renal Clinical Network
Following the focus of the North Wales workshops to extract relevant social care issues and people living with kidney disease, family and carer perspectives, we needed to put these outcomes and priorities back to the Welsh Renal Clinical Network, while at the same time establish what their priorities were in terms of health services research, as commissioners of renal services in Wales.
Although the network manager and the lead nurse for Wales attended workshop 1, the network board membership comprises many more clinical and non-clinical representatives. All of the network ‘leads’ are practising renal healthcare specialists across all of the multi-disciplinary renal care pathways and advocate on behalf of their speciality across Wales. The board also has representatives from all Wales NHS management, charity providers, patient representatives, renal research, Welsh government and wider specialist networks supporting the delivery of renal health and social care to people in Wales. Currently there are around 22 board members with individuals co-opted as necessary to provide specialist knowledge and skills. Board meetings are usually held every 3 months with additional all Wales quarterly meetings coordinated with specific specialities, for example, specialist nurses (education and home therapies) and AHPs. The network also brings all of renal health and social care together for an annual audit day, networking and opportunities to share learning and clinical practice.
In preparation, a review of the current research priorities in renal healthcare in the UK were undertaken. Five worksheets were shared prior to the meeting with a total of 106 questions identified (this included the list of priorities identified in workshop 1).
Due to conflicting schedules the decision was taken to proceed with the workshop on a date when the most people could attend. Eight people attended the workshop held in the Lifesciences hub at Cardiff Bay.24 The group included; the Deputy All Wales Clinical Lead, The Network Manager, The Lead Nurse for Wales, The Welsh Renal Information Analyst, The Project Manager, The Network Coordinator, Lead Consultants and the Lead Pharmacist for Wales. The exercise took just over 2 hours and included some time to discuss anything that the group felt was missing from the lists and ways to improve patient and public involvement in renal research in Wales. The session was facilitated by a member of the research team and opened with a presentation and summary of workshop 1. Details are provided in table 2 and the full worksheets are available in online supplementary file 2.
bmjopen-2020-036872supp002.pdf (239.6KB, pdf)
Following the workshop, a list was compiled of all the areas the Welsh Renal Clinical Network listed as green (via a traffic light voting system explained in detail in table 2, workshop 2, section 5). This list was shared via email and face-to-face meetings with a selection of multidisciplinary renal professionals, renal charity representatives and patients who were unable to attend either workshop. We asked them to review the list, make comments and add anything they felt was missing. A final list was drafted and shared with the executive board of the WKRU. The full list of people who had input into the complete research priority setting exercise is listed in table 3. The complete research priority setting exercise was reported using the REPRISE checklist and guidelines.25
Patient and public involvement
Patients, family members and the wider social care sector were involved in every aspect of the priority setting exercise. We had input at a strategic level from two patient representatives on the WKRU executive board who supported the idea of an All Wales priority setting exercise in health services and social care. The number of patients at the first workshop in North Wales exceeded all other specialities. The Welsh Renal Clinical Network has 2 patient representatives on their board as well as lay representatives all of whom feed into the Networks agenda. We also involved every renal charity in Wales, wider third sector representatives and industries.*
*Paul Popham Renal Fund, Kidney Care UK, Kidney Wales, Polycystic Kidney Disease, Age Connect North Wales Central, Holistic Therapies, Citizens Advice Bureau, Carers Wales, Sign-Sight and Sound, Alternative Futures Innovation Labs, local council authorities, Renal Services, Bbraun, Baxter and Fresenius.
Results
The top priorities identified from workshop 1 the Social Care Innovation Lab were:
What support do patients want and how could it best be integrated into routine care (eg, social prescribing and what is the role of social prescribing)?
How can we best support patients with decision making?
What are the different groups knowledge, needs and understandings and how can we make better education programmes?
How best to integrate health promotion into routine care pathways?
What works best and how best to integrate best care into clinical care pathways.
When these were presented as part of the long list in workshop 2, we were able to identify 38 individual research questions broadly grouped into 10 research themes: (1) integrating health and social care, (2) education, (3) acute kidney injury, (4) CKD and cardiovascular disease, (5) transplantation, (6) dialysis, (7) personalised medicines, (8) cross-cutting priorities, (9) specific social contexts and (10) transitional services and children (box 2).
Box 2. Results of the research priority setting exercise in health services and social care research in Wales.
Integrated health and social care
What is the best clinical and most cost-effective frequency of review for people on peritoneal dialysis, haemodiafiltration, haemodialysis or conservative management? What are patients’ and carers’ views on and experiences of the frequency of review for people on peritoneal dialysis, haemodiafiltration, haemodialysis or conservative management?
What is the optimum timing of laparoscopic and percutaneous peritoneal dialysis access creation? What are patients’ and carers’ views on and experiences of the optimum timing of laparoscopic and percutaneous peritoneal dialysis access creation?
What is the clinical and cost-effectiveness of having a keyworker (interpreted as ‘named nurse’) present in the context of renal replacement therapy? What support do patients want and how could it best be integrated into routine care (eg, social prescribing and what is the role of social prescribing)?
What are the adverse health and social care effects of haemoglobin levels in older people with kidney disease?
What works best in MDT care and how best to integrate MDT renal care into clinical care pathways?
What are the health and social care outcomes of living with obesity and kidney disease?
What are the health and social care outcomes of living with diabetes and kidney disease?
Education
Does the provision of education and supportive interventions to people with CKD by healthcare professionals increase patients’ skills and confidence in managing their conditions and improve clinical outcomes? What are patients’ and carers’ views on and experiences of the provision of education and supportive interventions and how can we best support patients with decision making?
What are different groups (women, minority, disadvantaged, special needs, deprivation, young people, etc) knowledge, needs and understandings and how can we make better education programmes for these groups?
Acute kidney injury
How do we develop and implement suitable markers for early detection of acute kidney injury (AKI)?
How do we improve ways to identify people at risk of AKI?
Chronic kidney disease and cardiovascular disease.
What is the clinical and cost-effectiveness of cardiac assessment before transplantation? What are patients’ and carers’ views on and experiences of cardiac assessment before transplantation?
How do we reduce cardiovascular risk in the renal population?
What are the views and experiences of people with cardiovascular disease while on dialysis?
Transplantation
What is the best clinical and most cost-effective strategy for timing of pre-emptive transplantation? What are patients’ and carers’ views on and experiences of strategies for timing of pre-emptive transplantation?
What are the health and social care outcomes of older/frailer people who have had a transplant?
What is the optimal BMI cut-off for renal transplant from the multiple (patient, carer, clinical) perspectives?
What are the patient and carer views and experiences of post-transplant psycho/social support post-transplant across Wales?
Dialysis
What are the biological and psychosocial effects of being on dialysis?
What are the health and social care benefits of exercise while on dialysis?
What are the health and social care benefits of diet while on dialysis?
What are the best ways to reduce complications of peritoneal dialysis? What are patients views and experiences of the complications of peritoneal dialysis?
How do we preserve vascular access in people with kidney disease?
What are patients, carers and family members views, experiences and understandings of new technological innovations in dialysis?
What are patients, carers and professionals’ views and experiences of ‘extended’ dialysis on their health and social care?
Personalised medicines
What are the patients, cares and professionals’ views and experiences of personalised medicine?
What are the best medicines for palliative care and people with CKD?
Cross-cutting
What are the value of patient peer support groups?
How do we maximise the use of the Rare Renal Disease Registry (RADAR) and increase the opportunity for people to participate in RADAR?
What are the best ways to treat people with cognitive impairments, and undiagnosed impairments for example, dementia?
How do we improve the use and effectiveness of frailty scores in Vital Data (the All Wales Renal Audit data) in patient care?
How do we improve the translation of renal audit data into high quality research publications?
Specific social contexts
How best to integrate health promotion into routine care pathways?
What is the role of the renal social worker in renal care in Wales?
What are the social care needs of older people with CKD?
Transitional services and children
What are patients, carers views and experiences of transition services across Wales?
Children and renal disease—the research priorities can be adjusted to include children where appropriate.
Service evaluation and improvement questions
What does the renal patient pathway look like in Wales from the multiple perspectives?
BMI, body mass index; CKD, chronic kidney disease; MDT, multidisciplinary team.
We also identified a priority for the Welsh Renal Clinical Network was to better understand the renal patient pathways across Wales and what these look like from the multiple perspectives (including patients) in order to undertake pan Wales service evaluations and improve renal health and social care services (Box 2).
Many of the identified priorities of the professionals, people living with kidney disease and family members and wider social care sector overlapped. Many of the priorities identified by the Welsh Renal Clinical Network mapped onto those identified by patients, and the network identified all of the questions identified in the Social Care Innovation Lab as a priority.
The Welsh Renal Clinical Network noted that some questions in particular those identified by National Institute for Health and Care Excellence were important but many were unrealistic or impossible to study and in some cases the treatment under investigation were not always offered in Wales, for example, diafiltration. Other questions the Welsh Renal Clinical Network felt were important but could not easily be answered within the 5-year time frame set for this exercise and that others were more important to address first.
Bringing people together to discuss integrated health and social care research priorities supported many of the multidisciplinary renal professionals in particular AHPs to view their practice in a research context. For many this was the first time they had opportunity to think about research and how their role could support further integrated health and social care research.
The Welsh Renal Clinical Network noted that many recent Randomised Controlled Trials in renal research showed negative or inclusive results, and therefore, were having little impact on clinical practice.
Discussion
Over 12 months, two workshops and consultations with the renal health and social care community including patients and family members, and the wider social care sector identified 38 research questions as a priority to health services and social care research in Wales. As we did not specify a stage of CKD, mode of dialysis or treatment stage many of the priorities identified could be mapped across early to late stage renal failure and specific treatment modalities.
As with other recent priority setting partnerships, logistics and resources made it impossible to undertake the priority setting exercise in the detail specified on the JLA website.26 However, through working in close partnership with the Welsh Clinical Renal Network and the unique ways in which it is configured, we felt we were able to successfully undertake evidence checking (stage 4), interim priorities (stage 5), and agreed list (stage 6) into a single workshop (table 2). This was largely due to having all the expertise and perspectives of the network in one room, as well as building up good partnerships and working relationships through a variety of research activities under the WKRU.
While it was encouraging to see that overall there was a broad agreement with renal healthcare professionals and patients in their priorities, initially it was not always clear to the Welsh Renal Clinical Network what role social care could potentially have on health service delivery. For example, ‘social prescribing’ was not well understood or the role it could have to improve services. In future workshops additional time and attention could be dedicated to social care contexts of kidney disease with real-life examples and cases to support understanding and help contextualise the potential integration of social care and health services research.
In order to produce a list of integrated health services and social care research priorities the authors where appropriate added an additional question to include the patient and care perspective. Future research could take this into account when setting up their research designs and potentially include mixed method and qualitative tools and measures to evaluate findings and future interventions, to take account of the patient perspective as well as improve health services.
Strengths and limitations of this study
This priority setting exercise was the first to be undertaken in Wales and to account for the population landscape of Wales and the Welsh renal health and social care services. Compared with other health systems and countries Wales is small (7 health boards, 3 trusts and 3.1 million population). MDT renal teams in Wales are beginning to work more cohesively, while at the same time accounting for the landscape of Wales (high deprivation, pockets of high population density coupled with rural and isolated communities). There is, therefore, capacity for high quality, Wales wide initiatives to address integrated health and social care priorities across the population and to map findings onto similar populations and demographics. It is also possible to undertake future (well planned) research priority setting partnerships with representative samples from the professional and patient perspectives in short time frames and with limited resources.
The noticeable difference of this priority setting exercise compared with others is the lack of treatment specific questions. The priorities listed here do not always seek to create new treatments and interventions but evaluate the impact of current treatments and interventions from the multiple perspectives. The focus of the priority setting was on integrating health and social care research. By enlarge this was achieved although the investigators were surprised by the initial lack of understanding of the social care needs of people living with kidney disease, and the ways social care could potentially support the health services agenda. Including methods to capture the patient and carers perspective in future studies and interventions could support the further alignment of professional and patient outcomes in research.
We were unable to undertake a full review of the field to examine in depth which research questions have or are already being undertaken outside of those identified in the Welsh Renal Clinical Network workshop. Further research is needed, alongside systematic reviews in order to move many of the research priorities forward. Finally we acknowledge the need to continually and systematically revisit and update research priorities with multiple key stakeholder input.
Conclusion
A modified version of the JLA priority setting partnership was effective in establishing shared research priorities across Wales. Research priorities identified by patients, caregivers and health professionals emphasise a broad integrated health and social care priority agenda. Future research should seek to further integrate the patient perspective into research study designs. These priorities can be used by commissioners to help shape future policies and service commissioning.
Supplementary Material
Acknowledgments
Thank you to all of the delegates who attended the North Wales conference and the Social Care Innovation Lab for attending and sharing their views. Thank you to the Welsh Renal Clinical Network for supporting a research priority setting exercise and to those members of the network who attended to share their views and perspectives. Thank you to the National Centre for Population Health and Wellbeing Research (NCPHWR) and the Wales School for Social Care Research (WSSCR) for cohosting the North Wales meeting. Thank you to Diane Seddon and the Centre for Aging and Dementia Research for producing the SCIL template and to Gill Toms and Steven Baker for hosting the Social Care Innovation Lab. A special thank you to all of the people living with kidney disease, family members and friends for coming to the various meetings and sharing your views and helping to shape these priorities. Thank you to the Wales Kidney Research Unit for supporting this work.
Footnotes
Twitter: @leahmclaughiln, @janenoyes
Contributors: LML: codesigned the approach with JN, prepared content for both workshops and facilitated the Welsh Renal Clinical Network workshops. Prepared and drafted manuscript. JN: codesigned the approach with LML, oversaw the preparations of both workshops, provided overall contextual input. Reviewed and drafted manuscript. SS: supported and set up the Welsh Renal Clinical Network workshop, provided policy and commissioning contexts.
Funding: This work was supported by the Wales Kidney Research Unit (WKRU) funded by Health and Care Research Wales (HCRW).
Map disclaimer: The depiction of boundaries on this map does not imply the expression of any opinion whatsoever on the part of BMJ (or any member of its group) concerning the legal status of any country, territory, jurisdiction or area or of its authorities. This map is provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article or uploaded as online supplementary information.
References
- 1.Network WRC Renal services in Wales 2016 – 2020 delivery plan, 2016. Available: http://www.wales.nhs.uk/sites3/Documents/773/RenalDiseaseQualityDeliveryPlan1.pdf [Accessed 11 Oct 2019].
- 2.Registry R. Audit Portal - UK Renal Registry. Available: https://www.renalreg.org/datasets/audit-portal/ [Accessed 11 Oct 2019].
- 3.Kidney Research UK As kidney failure rates grow in Wales, Kidney Research UK challenges lack of awareness on World Kidney Day - Kidney Research UK. Available: https://kidneyresearchuk.org/2017/03/09/as-kidney-failure-rates-grow-in-wales-kidney-research-uk-challenges-lack-of-awareness-on-world-kidney-day/ [Accessed 11 Oct 2019].
- 4.Abdel-Kader K, Unruh ML, Weisbord SD. Symptom burden, depression, and quality of life in chronic and end-stage kidney disease. Clin J Am Soc Nephrol 2009;4:1057–64. 10.2215/CJN.00430109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nguyen NTQ, Cockwell P, Maxwell AP, et al. Chronic kidney disease, health-related quality of life and their associated economic burden among a nationally representative sample of community dwelling adults in England. PLoS One 2018;13:e0207960. 10.1371/journal.pone.0207960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Crews DC, Bello AK, Saadi G. Burden, access, and disparities in kidney disease. Braz J Med Biol Res 2019;52 10.1590/1414-431x20198338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Luyckx VA, Tonelli M, Stanifer JW. The global burden of kidney disease and the sustainable development goals. Bull World Health Organ 2018;96:414–22. 10.2471/BLT.17.206441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Welsh Government Care and support at home, a summary of the five year strategic plan 2017-2022, 2017. Available: https://socialcare.wales/cms_assets/file-uploads/Plan-on-a-page-English.pdf [Accessed 31 Oct 2019].
- 9.Odgers HL, Tong A, Lopez-Vargas P, et al. Research priority setting in childhood chronic disease: a systematic review. Arch Dis Child 2018;103:942–51. 10.1136/archdischild-2017-314631 [DOI] [PubMed] [Google Scholar]
- 10.Tong A, Chando S, Crowe S, et al. Research priority setting in kidney disease: a systematic review. Am J Kidney Dis 2015;65:674–83. 10.1053/j.ajkd.2014.11.011 [DOI] [PubMed] [Google Scholar]
- 11.Hemmelgarn BR, Pannu N, Ahmed SB, et al. Determining the research priorities for patients with chronic kidney disease not on dialysis. Nephrol Dial Transplant 2017;32:847–54. 10.1093/ndt/gfw065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Elliott MJ, Sale JEM, Goodarzi Z, et al. Long-Term views on chronic kidney disease research priorities among stakeholders engaged in a priority-setting partnership: a qualitative study. Health Expect 2018;21:1142–9. 10.1111/hex.12818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wales kidney research unit. Available: http://www.kidneyresearchunit.wales/ [Accessed 31 Oct 2019].
- 14.Networks WR Welsh Renal Networks - an Official NHS Wales website.
- 15.Nigel Edwards The challenge of change in the NHS in Wales | the Nuffield trust. Available: https://www.nuffieldtrust.org.uk/resource/the-challenge-of-change-in-the-nhs-in-wales#cause-and-effect [Accessed 18 Oct 2019].
- 16.Abel GA, Barclay ME, Payne RA. Adjusted indices of multiple deprivation to enable comparisons within and between constituent countries of the UK including an illustration using mortality rates. BMJ Open 2016;6:e012750. 10.1136/bmjopen-2016-012750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Welsh Government Stats Wales. Available: https://statswales.gov.wales/Catalogue/Population-and-Migration/Population/Estimates/Local-Authority/populationestimates-by-localauthority-year [Accessed 18 Oct 2019].
- 18.Welsh Government Welsh index of multiple deprivation 2014 the official measure of relative deprivation for small areas in Wales. Available: http://wimd.wales.gov.uk/ [Accessed 18 Oct 2019].
- 19.Welsh Government Social services and wellbeing (Wales) act 2014, 2014. Available: http://www.legislation.gov.uk/anaw/2014/4/pdfs/anaw_20140004_en.pdf [Accessed 31 Oct 2019].
- 20.Davies -Director EM. The UK renal research strategy, 2016. Available: https://www.kidneyresearchuk.org/wp-content/uploads/2019/02/KR9501-UKRRS-Booklet-V8-WEB.pdf [Accessed 11 Oct 2019].
- 21.The James Lind alliance | James Lind alliance, 2004. Available: http://www.jla.nihr.ac.uk/ [Accessed 17 Oct 2019].
- 22.Tong A, Crowe S, Chando S, et al. Research priorities in CKD: report of a national workshop conducted in Australia. Am J Kidney Dis 2015;66:212–22. 10.1053/j.ajkd.2015.02.341 [DOI] [PubMed] [Google Scholar]
- 23.Conferences | venue Cymru. Available: https://venuecymru.co.uk/conferences [Accessed 31 Oct 2019].
- 24.Life sciences hub Wales | life sciences. Available: https://lshubwales.com/ [Accessed 4 Nov 2019].
- 25.Tong A, Synnot A, Crowe S, et al. Reporting guideline for priority setting of health research (Reprise). BMC Med Res Methodol 2019;19:243. 10.1186/s12874-019-0889-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Priority setting partnership (PSPs) flowchart.. Available: http://www.jla.nihr.ac.uk/about-the-james-lind-alliance/downloads/JLA-PSP-process-final.pdf [Accessed 5 Nov 2019].
- 27.Social Care Innovation Lab | Centre For Ageing & Dementia Research. Available: http://www.cadr.cymru/en/social-care-innovation-lab.htm [Accessed 31 Oct 2019].
- 28.National Institute for health and care excellence (NICE), renal research recommendations. Available: https://www.nice.org.uk/search?om=[%7B%22ndt%22:[%22Researchrecommendations%22]%7D]&ps=50&q=renal&sp=on [Accessed 21 Oct 2019].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-036872supp001.pdf (13.9MB, pdf)
bmjopen-2020-036872supp002.pdf (239.6KB, pdf)