Abstract
Background
The aim of the study was to compare the clinical and radiographic evaluation of pulpotomy using mineral trioxide aggregate (MTA), calcium silicate-based cement (Biodentine), and Er,Cr:YSGG laser in primary molars.
Materials and methods
Fifty-four primary teeth were selected for this study as per the inclusion and exclusion criteria in the age group of 4–9 years and then randomly allocated to three groups A, B & C. In group A, after removal of coronal pulp, MTA was placed at the floor of pulp chamber. In group B, calcium silicate-based cement (Biodentine) was placed at the floor of pulp chamber. In group C, decontamination of the cavity was done with Er,Cr:YSGG laser. This was followed by placement of permanent restorative material in all the groups. Clinical and radiographic success was evaluated at 3, 6 and 9 months. Data analysis was performed using Statistical Package for the Social Science-21 (SPSS-21).
Results
At the end of 9 months, overall success rate of pulpotomy was 85.5%. There was no significant difference among the three groups (p > 0.05).
Conclusion
The study showed that the success of pulpotomy procedure is independent of the type of medicament used for pulpotomy. Moreover, the study also shows that Er,Cr:YSGG laser can be effectively used for pulpotomy procedures.
Keywords: Pulpotomy; MTA; Biodentine; Er,Cr:YSGG laser
Introduction
Pulp therapy in pediatric dentistry involves treatment of both primary as well as young permanent teeth with the use of medicaments favorable for the pulpal tissue. There are various modalities under this broader therapy which can be used on the basis of pulpal involvement and symptoms given by the patient. 1) Thus, it is very essential to have apt knowledge for the clinician regarding these therapeutic methods.
The purpose of dental pulp therapy is to maintain the vitality of a decayed tooth to secure its presence in the dental arch. Depending on the extent of pulpal involvement, vital pulp therapy may include pulp capping and pulpotomy procedures. In the present study emphasis on pulpotomy procedure has been put forth. According to American Association of Pediatric Dentistry (2014), pulpotomy can be defined as the complete removal of coronal portion of the dental pulp followed by placement of suitable dressing or medicament that will promote healing and preserve vitality of the tooth. Various materials have been recommended for this purpose, such as formocresol, glutaraldehyde, ferric sulphate, calcium hydroxide, mineral trioxide aggregate (MTA), Biodentine and laser therapy. 2)
In the present study, pulpotomy was performed using MTA, Biodentine and Er,Cr:YSGG laser. Among these methods, MTA has been established as gold standard medicament for pulpotomy, however other medicaments such as Biodentine and various lasers are still under research. MTA was first introduced in the dental literature in 1993, however it received FDA approval in 1998. 3) It has several desirable properties such as biocompatibility, bioactivity, hydrophilicity, radiopacity, sealing ability and low solubility, but due to its poor handling characteristics and high cost new calcium silicate-based material with improved properties were introduced.
Biodentine was first commercially available in 2009 and was specifically designed as a ‘dentine replacement’ material. The material is actually formulated using the MTA-based cement technology with the improvement of some properties such as physical qualities and handling. Biodentine resists microleakage and also has an antimicrobial effect. It is relatively more user-friendly material as compared to MTA. 4)
The applications of lasers to dental tissues also have shown their potential to increase healing, stimulate dentinogenesis and preserve vitality of the dental pulp. Different types of lasers are being used in dentistry such as CO2 lasers, diode lasers, Nd:YAG, Er:YAG lasers and Er,Cr:YSGG laser. 5) As Er,Cr:YSGG laser involves water coolant, it causes less thermal damage of pulpal tissues. 6) The aim of present study is comparative evaluation of radiological and clinical outcome of pulpotomy with MTA, Biodentine and Er,Cr:YSGG laser.
Materials and methodology
A total of 54 primary teeth in 45 children aged 4–9 years participated in the study in the Department of Pedodontics & Preventive Dentistry at Maulana Azad Institute of Dental Sciences, New Delhi. The present study was a randomized controlled trial carried out after obtaining prior approval from the Ethical Committee of the Institution and registered with Clinical trials registry of India (CTRI/2018/06/014414). The sample size was estimated based on the previous literature 7) findings and by consulting a biostatistician. The teeth were divided equally into the following three groups of 18 primary teeth each by simple random allocation as in Chart 1 and Table 1 based on inclusion and exclusion criteria.
Chart 1:

Teeth were divided equally into the following three groups of 18 primary teeth each by simple random allocation
Table 1: Group wise distribution.
| S.No. | Group | Description | No. of teeth |
|---|---|---|---|
| 1 | Group A | MTA | 18 |
| 2 | Group B | Biodentine | 18 |
| 3 | Group C | Er,Cr:YSGG laser | 18 |
Table 1: Depicts group wise distribution of total number of patients among all the groups.
Inclusion criteria
Pediatric patients aged 4–9 years.
Deep carious lesion present in primary molars.
Absence of clinical signs and symptoms of pulpal exposure.
Absence of radiographic signs and symptoms of pulpal degeneration.
Positive parental informed consent.
Exclusion criteria
Un co-operative children.
Children with medically compromised disease.
Presence of clinical signs and symptoms of pulpal exposure.
Presence of radiographical signs and symptoms of pulpal degeneration.
Physiologic root resorption more than one-third.
Group A- MTA (MTA Angelus, Londina, PR, Brazil) paste was prepared as per the manufacturers' instructions to obtain a putty-like consistency and carried into the prepared cavity and uniformly placed over the floor of pulp chamber.
Group B- Biodentine (Septodont Biodentine™, St. Maur-des-Foss'es, France) was mixed according to the manufacturer's instructions and carried into the prepared cavity and uniformly placed over the floor of pulp chamber.
Group C- The floor of the pulp chamber was radiated with Er,Cr:YSGG laser (Waterlase iPlus, Biolase) at 75 -100 mJ (1–1.5 W)6 for 60 sec to ensure complete decontamination as in Figures 1 and 2. While approaching canal orifices, the power [100 to 120 mJ, 1.0 to 1.8 W] and frequency [10 to 15 Hz] set and water spray was maintained. Laser tips of diameter 600 µm were used. The procedure was repeated three to four times for 15 to 20 seconds in 30 seconds intervals in order to obtain full vaporization of the coronal pulp tissue and cessation of the bleeding. Then, the access cavity filled with a thick mix of zinc oxide eugenol cement followed by cermet restoration.
Figure 1:

Rubber dam application over deep carious tooth
Figure 2:

Decontamination using Er,Cr:YSGG laser
After 24 hours, the teeth in all three groups were restored with preformed stainless -steel crowns (3M™ ESPE™). The participants were recalled for clinical and radiographic evaluations after 3, 6 and 9 months as depicted in Figure 3.
Figure 3:

Representative radiographic observations in all the three groups over different follow-up periods. (a) MTA; (b) Biodentine; (c) Er,Cr:YSGG laser pulpotomies in primary molars.
At the end of 3, 6 and 9 months, all teeth were evaluated clinically and radiographically based on AAPD criteria8): (1) absence of spontaneous pain and/or sensitivity to pressure; (2) absence of sinus, fistula, edema, and/or abnormal mobility; (3) absence of radiolucency at the interradicular and/or periapical regions; (4) absence of internal or external root resorption.
Data analysis was performed using Statistical Package for the Social Science-21 (SPSS-21). The data was analyzed on the basis of categorical scores given to clinical and radiographic analysis of the three groups using chisquare (χ2) analysis and p-values < 0.05 were considered statistically significant.
Results
After three months, 54 teeth were available for follow-up. At the end of 3 months, clinically two teeth exhibited mild gingival inflammation due to poor oral hygiene in both MTA and Er,Cr:YSGG laser group. At the end of 6 and 9 months, 50 teeth were available for follow-up. There were 17 teeth available for follow-up in Group A (MTA), 17 teeth available for follow-up in Group B (Biodentine) and 16 teeth available for follow-up in Group C (Er,Cr:YSGG laser).
Thus at 3 months, no tooth had any sign of pulpal inflammation or periapical pathologies as shown in Table 2. At the end of 6 and 9 months, one tooth in Group B and three teeth in Group A and C presented with gingival swelling clinically and inter-radicular radiolucency radiographically as shown in Graph 1 and Table 2. Chi square value was 2.19 and the p-value at the end of 9 months was 0.33. The difference among the three groups was not statistically significant as p > 0.05.
Table 2: Clinical and radiographic evaluation of Group A, B, C after 3, 6 and 9 months.
| 3 months | 6 months | 9 months | TOTAL | Total failures | ||
|---|---|---|---|---|---|---|
|
Group A (MTA) |
Clinical | 0/18 | 3/17 | 3/17 | 3/17 | 3/17 |
| Radiographic Periapical lesion | 0/18 | 3/17 | 3/17 | 3/17 | ||
| Radiographic Pathologic resorption | 0/18 | 3/17 | 3/17 | 3/17 | ||
|
Group B (BIODENTINE) |
Clinical | 0/18 | 0/17 | 0/17 | 0/17 | 1/17 |
| Radiographic Periapical lesion | 0/18 | 1/17 | 1/17 | 1/17 | ||
| Radiographic Pathologic resorption | 0/18 | 1/17 | 1/17 | 1/17 | ||
|
Group C (Er,Cr:YSGG laser) |
Clinical | 0/18 | 3/16 | 3/16 | 3/16 | 3/16 |
| Radiographic Periapical lesion | 0/18 | 3/16 | 3/16 | 3/16 | ||
| Radiographic Pathologic resorption | 0/18 | 3/16 | 3/16 | 3/16 |
Graph 1:
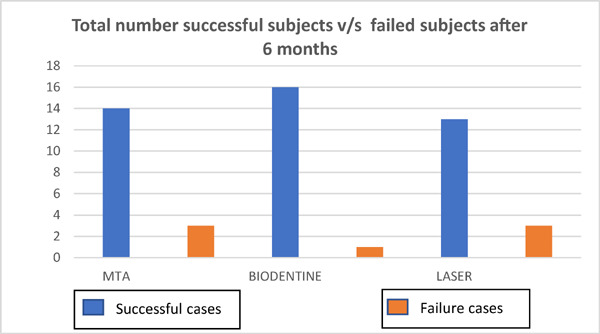
Comparison of successful cases v/s failed cases after 6 months
Discussion
Dental caries is one of the most frequent chronic conditions in childhood mainly affecting primary teeth. When compared to the permanent teeth, primary teeth have thinner enamel and dentin, wider dentinal tubules and higher and larger pulp chamber. This leads to early involvement of pulp in primary teeth than in permanent teeth. 9) When pulpal inflammation is restricted to coronal portion of the pulp, the treatment of choice is pulpotomy. 10) Pulpotomy is a procedure performed in a tooth with deep carious lesion adjacent to pulp, where coronal pulp is amputated to preserve the vitality of radicular pulp. 11)
Ranly (1994) in reviewing the rationale and various medicaments, provided three categories of treatment approaches: 1) Devitalization - which intended to destroy or mummify the vital tissue. 12) 2) Preservation - approach involved medicaments and techniques that provide minimal insult to the orifice tissue and maintains the vitality and normal histologic appearance of the entire radicular pulp. 13) 3) Regeneration - approach includes pulpotomy agents that have cell-inductive capacity to either replace lost cells or induce existent cells to differentiate into hard tissue–forming elements. 14)
In all the three groups, stainless steel crown was placed as the final restorative material. Soxman JA (2000) 15) conducted a study to determine the performance of stainless-steel crown after pulpotomy procedures in primary teeth and concluded that stainless steel crown (SSC) provide a more durable and reliable final restoration for primary molars. Another similar study was conducted by Holan G et al (2002). 16)
The final clinical follow up was conducted at the end of 9 months. In our study, the overall success of the pulpotomy procedure was 85.5%. The similar results were in accordance with the study conducted by Rolling I and Thylstrup A (1975) 17), Aminabadi NA et al (1993) 18), Farooq NS et al (2000) 19) and Caicedo R et al (2006). 20)
The overall success rate at the end of 3 months was 88.2% for MTA, 100% for Biodentine and 87.5% for Er,Cr:YSGG laser which reduced to 82% for MTA, 94% for Biodentine and 78.5% for Er,Cr:YSGG laser at the end of 6 and 9 months. This result was also similar to a study conducted by Kusum B et al (2015) 7) and Niranjani K et al (2015) 21) on pulpotomy treatment on primary molars.
After 6 and 9 months, 82% success rate of pulpotomy treatment was found in MTA group. The good clinical success rates of pulpotomy are related to the thickness of the newly formed dentin. The result was also similar in accordance with a study conducted by Odabas ME et al (2012) 22) and Olatosi OO et al (2014). 23) Three failures were observed in Group A due to known disadvantages of gradual disintegration and tunnel defects in the newly formed dentin.
The success rate of pulpotomy treatment in Biodentine group was 100% at 3 months and 94% at the end of 6 and 9 months. This result was also similar to a study conducted by Togaru H et al (2016) 24) and Akhtar M et al (2016). 25) There was only one failure in Biodentine group after 6 months follow up. This might have occurred due to poor case selection or improper manipulation and improper coverage of the permanent restorative material.
In Er,Cr:YSGG group, the success rate of pulpotomy treatment was 87.5% at 3 months and 78.5% at the end of 6 and 9 months. Our result was in accordance with the study conducted by Olivi G et al (2007). 6)
Due to the decontamination property of Er,Cr:YSGG laser, the bactericidal action is achieved and thus Er,Cr:YSGG can be effectively used for pulpotomy procedures. Three failures were observed in Group C. This might have occurred due to poor case selection or improper coverage of the permanent restorative material. Incomplete decontamination with laser may also have resulted in failure of pulpotomy treatment. 26)
Clinically and radiographically, the overall success rate of the three pulpotomy groups were 85.5% with no statistical difference among the groups for the observation period of 3, 6 and 9 months. The common clinical failure in the present study was pain, percussion sensitivity and gingival abscess. The radiographic failure was attributed to interradicular radiolucency and periodontal ligament widening or any procedural errors that included manipulation of material, delay in placement of material into the pulp chamber and improper coverage of the permanent restorative material.
Conclusion
In the present study, pulpotomy of primary molars using MTA, calcium silicate based cement (Biodentine) and Er,Cr:YSGG laser showed high clinical and radiographic success (85.5%) at the end of 9 months. These findings suggest the potential of Biodentine for being used as a pulpotomy medicament in primary teeth. On the other hand, Er,Cr:YSGG laser showed good success rate in both clinical and radiographic outcomes as well as MTA. Pulpotomy treatment was successful independent of bactericidal liner if adequate decontamination can be achieved as in case of Er,Cr:YSGG laser. Pulpotomy procedures done in the present study have given successful results with different types of pulp capping agents. It is suggested that more studies with longer follow up be carried out in order to establish a standard protocol for the management of deep carious lesions with pulpotomy procedures.
References
- 1: Asgary S, Fazlyab M, Sabbagh S, Eghbal MJ. Outcomes of different vital pulp therapy techniques on symptomatic permanent teeth: a case series. Iran Endod J. 2014. October; 9(4):295-300. [PMC free article] [PubMed] [Google Scholar]
- 2: Parirokh M, Torabinejad M. Mineral trioxide aggregate: a comprehensive literature review—part III: clinical applications, drawbacks, and mechanism of action. J Endod. 2010. March 1;36(3):400-13. [DOI] [PubMed] [Google Scholar]
- 3: Tawil PZ, Duggan DJ, Galicia JC. Mineral trioxide aggregate (MTA): its history, composition, and clinical applications. Compendium of continuing education in dentistry (Jamesburg, NJ: 1995). 2015. April;36(4):247-52. [PMC free article] [PubMed] [Google Scholar]
- 4: Neelagiri NK, Geeta IB, Narayanaswamy S, Vinay CR, Aniketh TN. Direct pulp capping with a new material biodentine: a case report. J Evolution Med Dent Sci. 2015. April 27;4(34):5990-5. [Google Scholar]
- 5: Davoudi A, Sanei M, Badrian H. Application of laser irradiation for restorative treatments. Open Dent J. 2016; 10: 636-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6: Olivi G, Genovese MD, Maturo P, Docimo R. Pulp capping: advantages of using laser technology. Eur J Paediatr Dent. 2007. June;8(2):89-95. [PubMed] [Google Scholar]
- 7: Kusum B, Rakesh K, Richa K. Clinical and radiographical evaluation of mineral trioxide aggregate, biodentine and propolis as pulpotomy medicaments in primary teeth. Restor Dent Endod. 2015. November;40(4):276-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8: American Academy of Pediatric Dentistry. Guideline on pulp therapy for primary and immature permanent teeth. Pediatr Dent. 2009;31:179-86. [Google Scholar]
- 9: Havale R, Anegundi RT, Indushekar K, Sudha P. Clinical and radiographic evaluation of pulpotomies in primary molars with formocresol, glutaraldehyde and ferric sulphate. Oral Health Dent Manag 2013; 12(1): 24-31. [PubMed] [Google Scholar]
- 10: Ounsi HF, Debaybo D, Salameh Z, Chebaro A, Bassam H. Endodontic considerations in pediatric dentistry: a clinical perspective. Int Dent 2009;11(2); 40-50. [Google Scholar]
- 11: Godhi B, Sood PB, Sharma A. Effects of mineral trioxide aggregate and formocresol on vital pulp after pulpotomy of primary molars: An in vivo study. Contemp Clin Dent. 2011. October;2(4):296-301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12: Dummett CO, Kopel HM. Pediatric Endodontics. In. Ingle, editor. Endodontics. 5th edition, Elsevier publication; 864. [Google Scholar]
- 13: Dummett CO, Kopel HM. Pediatric Endodontics. In. Ingle, editor. Endodontics. 5th edition, Elsevier publication; 864-76. [Google Scholar]
- 14: Ranly DM. Pulpotomy therapy in primary teeth: New modalities for old rationales. Pediatr Dent 1994; 16:403-9. [PubMed] [Google Scholar]
- 15: Soxman JA. Stainless steel crown and pulpotomy: procedure and technique for primary molars. Gen Dent. 2000. May-Jun;48(3):294-7. [PubMed] [Google Scholar]
- 16: Holan G, Fuks AB, Ketlz N. Success rate of formocresol pulpotomy in primary molars restored with stainless steel crown vs amalgam. Pediatr Dent. 2002;24(3):212-6. [PubMed] [Google Scholar]
- 17: Rolling I, Thylstrup A. A 3-year clinical follow-up study of pulpotomized primary molars treated with the formocresol technique. Scand J Dent Res. 1975. March;83(2):47-53. [DOI] [PubMed] [Google Scholar]
- 18: Aminabadi NA, Zadeh Farahani RM, Gajan EB. A clinical study of formocresol pulpotomy versus root canal therapy of vital primary incisors. J Clin Pediatr Dent. 2008. Spring;32(3):211-4. [DOI] [PubMed] [Google Scholar]
- 19: Farooq NS, Coll JA, Kuwabara A, Shelton P. Success rates of formocresol pulpotomy and indirect pulp therapy in the treatment of deep dentinal caries in primary teeth. Pediatr Dent. 2000. Jul-Aug;22(4):278-86. [PubMed] [Google Scholar]
- 20: Caicedo R, Abbott PV, Alongi DJ, Alarcon MY. Clinical, radiographic and histological analysis of the effects of mineral trioxide aggregate used in direct pulp capping and pulpotomies of primary teeth. Aust Dent J. 2006. December;51(4):297-305. [DOI] [PubMed] [Google Scholar]
- 21: Niranjani K, Prasad MG, Vasa AA, Divya G, Thakur MS, Saujanya K. Clinical evaluation of success of primary teeth pulpotomy using mineral trioxide aggregate, laser and Biodentine™-an in vivo study. J Clin Diagn Res. 2015. April;9(4):35-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22: Odabaş ME, Alaçam A, Sillelioğlu H, Deveci C. Clinical and radiographic success rates of mineral trioxide aggregate and ferric sulphate pulpotomies performed by dental students. Eur J Paediatr Dent. 2012. June;13(2):118-22. [PubMed] [Google Scholar]
- 23: Olatosi OO, Sote EO, Orenuga OO. Effect of mineral trioxide aggregate and formocresol pulpotomy on vital primary teeth: A clinical and radiographic study. Niger J Clin Pract. 2015. Mar-Apr;18(2):292-6. [DOI] [PubMed] [Google Scholar]
- 24: Togaru H, Muppa R, Srinivas N, Naveen K, Reddy VK, Rebecca VC. Clinical and radiographic evaluation of success of two commercially available pulpotomy agents in primary teeth: An in vivo study. J Contemp Dent Pract. 2016. July 1;17(7):557-63. [PubMed] [Google Scholar]
- 25: Akhtar M, Rana SA, Rana MJ, Parveen N, Kashif M. Clinical and radiological success rates of Biodentine for pulpotomy in children. IJCMR 2016;3(8):2300-2. [Google Scholar]
- 26: Yadav P, KR I, BG S, Sheoran N, Sardana D. Comparative evaluation of ferric sulfate, electrosurgical and diode laser on human primary molars pulpotomy: an “in-vivo” study. Laser Ther. 2014. March 27;23(1):41-7. [DOI] [PMC free article] [PubMed] [Google Scholar]


