Abstract
Background
Various procedures have been described for patients undergoing a revision carpal tunnel release. These can include repeat open decompression with external or internal neurolysis, tenosynovectomy, endoscopic release, various flap techniques, saphenous vein wrapping and use of prosthetic implants. This study reports a case series of 30 consecutive patients who underwent revision carpal tunnel release at single institution from 2012 to 2018. Our surgical plan in all the patients involved a combination of these three techniques (triple therapy approach): neurolysis (external or internal) and tenosynovectomy, collagen matrix conduit wrap (NeuraWrap; Integra LifeSciences or Axoguard Nerve Protector, AxoGen Inc), and hypothenar fat flap.
Materials and methods
A total of 30 patient records were identified. The index surgery was performed by a variety of surgeons at varied private institutions as well as the VA hospital. However, all of the revision interventions in this series were performed by the senior author (Z.J.P.). Demographic data (age, sex, hand dominance, comorbidities, alcohol, and smoking history) were collected. Preoperative and postoperative symptoms were recorded for all patients, including: subjective outcomes, need for additional surgery and complications. Mean VAS preoperatively and postoperatively were compared using a paired t-test. All statistical analyses were performed with SPSS 20 (IBM, Chicago, IL).
Results
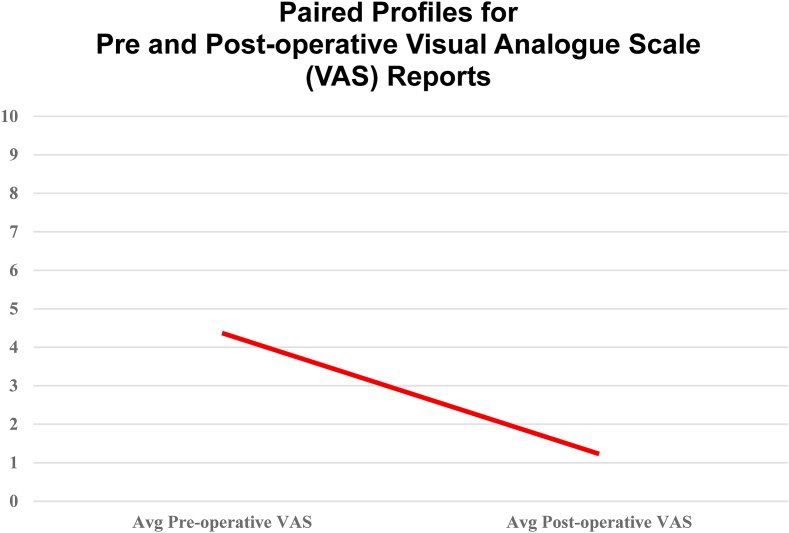
Patient reported measures of resolution of symptoms and VAS scores documented at 3 months. Of the 30 patients who underwent surgery for persistent or recurrent carpal tunnel syndrome, symptoms resolved completely in 25 patients. 2 patients were lost to follow up. 3 patients showed no improvement. The mean preoperative VAS score was 4.37 and declined to 1.23 after surgery (P < .0001).
Conclusion
Our study demonstrates that a combination of neurolysis and tenosynovectomy along with a nerve wrap and hypothenar fat flap should be considered in patients presenting with recurrent or persistent carpal tunnel syndrome.
Keywords: Hypothenar flap, Nerve wrap, Nerve conduit, Neurolysis, Median neuropathy, Recurrent and persistent carpal tunnel syndrome, Redo carpal tunnel release, Secondary procedure, Hand treatment
1. Introduction
Carpal tunnel syndrome (CTS) is the most common neuropathy of the upper extremity, affecting 3–7% of the general population.1,2 An open or endoscopic median nerve decompression procedure is done to relieve associated symptoms. Although most patients experience complete resolution of symptoms after surgical carpal tunnel release (CTR), there exists a percentage of patients who have persistent or recurrent symptoms despite or following intervention. The incidence of persistent or recurrent symptoms has ranged from 1% to 32%, however the rate of revision in large series is generally around 5%.1,2
Known factors affecting the rates of recurrence include incomplete release of the transverse carpal ligament, tenosynovitis, re-association of the transverse carpal ligament and intraneural fascicular scarring.3, 4, 5, 6
Various procedures have been described for those patients undergoing a revision carpal tunnel release. These can include repeat open decompression with external or internal neurolysis, tenosynovectomy, endoscopic release, various flap techniques, saphenous vein wrapping and use of prosthetic implants.7 Many experts advise that external or internal neurolysis is essential to address the neural fibrosis that is invariably present in these cases.8, 9, 10, 11, 12, 13, 14, 15
This study reports a case series of 30 consecutive patients who underwent revision carpal tunnel release at singular institution from 2012 to 2018. Our surgical plan in all the 30 patients involved a combination of these three techniques:
-
1)
Neurolysis (external or internal) and tenosynovectomy
-
2)
Collagen matrix conduit wrap (NeuraWrap; Integra LifeSciences, Plainsboro, NJ or Axoguard Nerve Protector, AxoGen Inc, Alachua, Florida, USA)
-
3)
Hypothenar fat pad flap
2. Methods
We retrospectively examined the records of the hand surgery service at the Miami Veterans Administration Healthcare System. We received pre-approval by the Miami VA Healthcare System Human Studies Subcommittee. The medical records of all patients with recurrent or persistent compression carpal tunnel syndrome after an index open or endoscopic carpal tunnel release from a 6-year period from 2012 to 2018 were retrieved from the electronic chart, Computerized Patient Records System (CPRS).
A total of 30 patient records were identified for this study purpose. There were no duplicate patients and each patient represented one procedure. In our series, primary operations were performed by a variety of surgeons at varied private institutions as well as at Veterans Administration facilities. However, all of the revision interventions in this series were completed using the triple-therapy approach performed by the senior author (Z.J.P.)
All 30 patients underwent a Nerve Conduction Study and Electromyogram to confirm the diagnosis of persistent or recurrent median nerve compression.
Demographic data (age, sex, hand dominance, comorbidities, alcohol, and smoking history) were collected from these records. Preoperative and postoperative symptoms were recorded for all patients, including subjective outcomes, need for additional surgery, and complications. Preoperative and postoperative pain levels were recorded using the ten-point visual analog scale (VAS) at a 3 month follow up. We compared the mean VAS preoperatively and postoperatively using a paired t-test. All statistical analyses were performed with SPSS 20 (IBM, Chicago, IL). In addition, all surgical findings of each revisional surgery were recorded, along with type and size of collagen conduit wrap used.
3. Operative technique
The patient was placed supine and the arm held in an arm table. Upper extremity was exsanguinated with an Esmarch bandage, and tourniquet inflated to 250 mm Hg pressure.
Standard palmar incision over the carpal tunnel area was used, incorporating the prior open palmar carpal tunnel scar (if present). Sharp incision was extended distally and proximally, taking care to obliquely cross the wrist crease (at a designed 45-degree angle to prevent any potential scar contracture). Dissection was performed using two Senn retractors for soft tissue distraction, and same #15 scalpel blade was used to cut through the skin, subcutaneous tissues and palmar fascia. Combination of tenotomy scissors for spreading and sharp scalpel dissection was used, with the median nerve identified, preserved and fully exposed. If any perineural fibrosis was noted, then external neurolysis was performed routinely. If there was significant intraneural fibrosis present, then an internal neurolysis was pursued, but this is not routinely done.
Median nerve exposure and release was carried throughout the length of the incision, and the entire area inspected for any neuromas. The described exposure of the median nerve was detailed in Fig. 1a. Nerve diameter was measured and a nerve wrap, approximately 1–2 mm larger, was selected. The nerve conduit wrap was wrapped around the compressed portion of nerve, and then secured with 8–0 prolene suture at each end to the epineurium as well as a single suture at the midpoint to close the collagen wrap. The placement and inset of the nerve conduit wrap around the median nerve is shown in Fig. 1b .
Fig. 1.
Figure 1a. Exposure of the median nerve. Note the hourglass deformity from chronic compression. Figure 1b. Placement and inset of the nerve conduit wrap around the median nerve. Figure 1c. Hypothenar fat pad flap. The vascularized flap is sutured to the cut end of the retinaculum with interrupted absorbable sutures.
At the conclusion of the tenosynovectomy and placement of the nerve conduit wrap, a 15 blade was used to sharply raise an ulnarly based adipose tissue flap over the hypothenar area of the palm. Adequate dissection was carried out to mobilize the flap in a tension free fashion up to the cut end of the retinaculum. The fat pad flap was then sutured to the cut end of the retinaculum with interrupted absorbable sutures (see Fig. 1c).
Tourniquet was released and hemostasis obtained. Perfused hand was verified. Skin routinely was closed with multiple interrupted non-absorbable sutures. Bulky soft dressing was applied. Patients were immobilized for 2 weeks with a resting volar splint until first post-operative appointment.
Patients were referred to occupational therapy once the wound was judged well healed.
Follow-up occurred at 3 months after the surgery and patient outcomes parameters were measured. If there was resolution of the patient symptoms at 3 months, patients were asked to follow-up as needed.
4. Results
Total of 30 patients were surgically treated with the nerve conduit wrap for recurrent or persistent revision carpal tunnel syndrome. Demographic factors were considered in the review of patient outcomes following surgery. The mean age at surgery was 67 years old and ranged from 47 to 85 years. Of note, 26 of the 30 patients were male and 4 cases were female.
Comorbid conditions are described in Table 1.6 (20%) patients admitted smoking tobacco at time of surgery, and 4 (13%) patients stated regular alcohol consumption. All the patients presented with recurrent or persistent symptoms of pain, numbness, and paresthesia.
Table 1.
Comorbidities of 30 patients Undergoing Revision Carpal Tunnel Surgery.
| Condition | Frequency, n (%) |
|---|---|
| Hypertension | 18 (60) |
| Psychologic disorders | 17 (57) |
| Diabetes mellitus | 9 (30) |
| Osteoarthritis | 9 (30) |
| Hyperlipidemia | 8 (27) |
| Gastroesophageal reflux disease | 7 (23) |
| Benign prostatic hyperplasia | 7 (23) |
| Chronic obstructive pulmonary disorder | 5 (16) |
| Coronary artery disease | 3 (10) |
| Hypercholesterolemia | 3 (10) |
| Asthma | 3 (10) |
| Obesity | 2 (7) |
All patients had EMG and NCS confirmed evidence of carpal tunnel syndrome. Patients with carpal tunnel syndrome had a mean motor latency of 5.5 milliseconds and a motor conduction velocity of 44.4 m/sec. The mean time period between index carpal tunnel surgery ranged from 1 to 25 years with a mean of 8 years.
The nature of the initial surgery and intraoperative findings are summarized in Table 2. 25 patients underwent initial open surgery and 25 presented with recurrent rather than persistence pain. 26 patients presented with flexor tenosynovitis and 18 presented with scarring. 4 patients also presented with hourglass deformities.
Table 2.
Summary of CTR procedures.
| Nature of Initial Surgery | Frequency, n (%) |
|---|---|
| Open | 25 (83) |
| Endoscopic | 5 (17) |
| Nature of CTS | 9 (30) |
| Recurrent | 25 (83) |
| Persistent | 5 (17) |
| Median, IQR | |
| Interval from Primary CTR | 6 |
| Intraoperative Findings | Frequency, n (%) |
| Flexor Tenosynovitis | 26 (87) |
| Scarring | 18 (60) |
| Hourglass Deformity | 4 |
| Clinical Outcomes | |
| Resolved | 25 (83) |
| Unchanged | 3 |
| Lost to follow-up | 2 |
Suture removal was performed at 2 weeks and patients were referred to occupational therapy. Patient reported measures of resolution of symptoms and VAS scores were documented at 3 months. These findings were utilized in the study.
Of the 30 patients who underwent surgery for persistent or recurrent carpal tunnel syndrome, 25 patients reported complete symptom resolution. 2 patients were lost to follow-up and 3 patients showed no improvement.
Of the 3 patients, 1 patient underwent a revision of the revision CTR with a nerve wrap and hypothenar fat pad which resulted in resolution of symptoms. 2 patients declined further surgery.
The mean preoperative VAS score was 4.37 and declined to 1.23 after surgery (P < .0001) (see Fig. 2).
Fig. 2.
Pre and post-operative visual analogue scale (VAS) reports.
5. Discussion
Carpal tunnel surgery generally results in excellent clinical outcomes and patient satisfaction. However a small percentage of patients undergoing carpal tunnel surgery do have persistent or recurrent carpal tunnel syndrome which can be multifactorial. There are many treatment options available for the management of persistent or recurrent carpal tunnel syndrome.
Kluemper et al. described flexor tenosynovectomy in 108 patients with recurrent or persistent carpal tunnel syndrome with favorable outcomes.16 Soltani et al. described the utilization of tenosynovectomy and collagen nerve wrap for the same condition with up to 89% success rate.17 Puckett et al. described 3 excellent and 1 good outcome in 5 patients undergoing neurolysis and nerve wrapping with tissue engineered biomatrix.18 The use of hypothenar fat pad has also been correlated with good outcomes.19, 20, 21, 22, 23, 24 Use of autologous vein grafting and nerve wrapping with collagen, polyglycolic acid, and caprolactone has also been described.25, 26, 27, 28
In their systematic review of 294 patients undergoing revision carpal tunnel surgery, Soltani et al. found a vast array of surgical techniques tried for this difficult condition.29 They concluded that decompression with flap interposition such a hypothenar flap had a higher success rate over simple repeated decompression.
In our study we performed a combination of three procedures in all patients:
-
1)
Neurolysis (external or internal) and tenosynovectomy
-
2)
Collagen matrix conduit wrap
-
3)
Hypothenar fat pad flap
We believe that each of these techniques has its own unique biomechanical and/or biological benefit to protect the nerve in the setting of revision carpal tunnel surgery. Neurolysis and tenosynovectomy release the involved nerve from connected scar tissue and increase the relative space available for the nerve in the carpal tunnel. A nerve wrap isolates the nerve segment from scarring by acting as a physical bio-barrier to deleterious fibrous ingrowth, restricting the egress of neurotrophic factors, and also promoting nerve gliding. The hypothenar fat pad flap further assists in preventing any reformation of the transverse carpal ligament. It also theoretically can help revascularize the ischaemic median nerve. We believe that as a combination, these unique properties in synergy contributed to overall success in re-operative surgery.
There are some limitations of the study. This is a short-term study with a follow-up period of 3 months after surgery. We assessed the resolution of patient symptoms and recorded VAS scores. Symptoms resolved in 25 patients (83%) at this time and they were asked to follow-up as needed or if their symptoms recurred.
The study was conducted at the Veterans Administration Hospital in Miami, Florida which is a referring tertiary institute for veterans. In the senior author's several years of experience working at the VA, the veteran patient population prefers to receive ongoing follow-up care at the same facility and has relatively easy access to the hand clinics. If patients did develop late symptoms following their revision carpal tunnel surgery, they would have likely returned back for additional follow-up care.
The fact that none of the patients returned back after 3 months is a very encouraging sign and there is a high likelihood that the symptoms resolved permanently in the patients. However, this is our speculation and further mid and long-term studies are needed to review sustained recovery and capture any recurrences at greater follow-up lengths.
Another limitation of the study is that only the resolution of symptoms and VAS scores were utilized as outcomes parameters. The retrospective nature of the study did not allow for use of other patient reported measure such as the DASH score. VAS was the best available measure to capture pain as it was used at each patient visit in the hand clinics and provided a standardized data set.
An economic consideration is the added cost involved in the utilization of the nerve wrap. However, we believe that the excellent outcomes obtained in our study justify the cost involved.
The patient demographic of the VA Hospital should also be considered. Our study only captured data from 4 female patients. National health data shows that in 2018, only 10% of veterans served at the Florida Veterans Affairs hospitals were female.30 Our technique was utilized at one-site and thus reflects the population that this healthcare system serves.
It is our belief that this study represents the largest number of patients undergoing a “triple therapy” approach to persistent or recurrent carpal tunnel syndrome. The strength of the study is the large number of patients involved and consistence of excellent results.
6. Conclusion
There are different individual techniques described in literature to address recurrent and persistent carpal tunnel syndrome. To our knowledge, this is the first time that a combination of three techniques has been utilized for the problem. Our study demonstrates that our triple-therapy approach involving the combination of neurolysis and tenosynovectomy along with a nerve wrap and hypothenar flap results in excellent outcomes in patients with recurrent or persistent carpal tunnel syndrome. We believe that each of the three individual techniques utilized works through a unique mechanism and together have an additive effect in addressing recurrent and persistent carpal tunnel syndrome.
Ethical approval statement
This was a retrospective review, pre-approved by the Institutional Review Board of the Subcommittee.
Author contributions
All authors contributed to this work.
Role of funding source
There are no funding sources to disclose.
Declaration of competing interest
None.
References
- 1.Ashworth N.L. Carpal tunnel syndrome. Clin Evid. 2007:1114. [PubMed] [Google Scholar]
- 2.Atroshi I., Gummesson C., Johnsson R., Ornstein E., Ranstam J., Rosen I. Prevalence of carpal tunnel syndrome in a general population. J Am Med Assoc. 1999;282:153–158. doi: 10.1001/jama.282.2.153. [DOI] [PubMed] [Google Scholar]
- 3.Kulick M.I., Gordillo G., Javidi T., Kilgore E.S., Jr., Newmayer W.L., III Long-term analysis of patients having surgical treatment for carpal tunnel syndrome. J Hand Surg. 1986;11:59–66. doi: 10.1016/s0363-5023(86)80104-6. [DOI] [PubMed] [Google Scholar]
- 4.Louis D.S., Greene T.L., Noellert R.C. Complications of carpal tunnel surgery. J Neurosurg. 1985;62:352–356. doi: 10.3171/jns.1985.62.3.0352. [DOI] [PubMed] [Google Scholar]
- 5.MacDonald R.I., Lichtman D.M., Hanlon J.J., Wilson J.N. Complications of surgical release for carpal tunnel syndrome. J Hand Surg. 1978;3:70–76. doi: 10.1016/s0363-5023(78)80118-x. [DOI] [PubMed] [Google Scholar]
- 6.Mackinnon S.E. Secondary carpal tunnel surgery. Neurosurg Clin N Am. 1991;2:75–91. [PubMed] [Google Scholar]
- 7.Teoh L.C., Tan P.L. Endoscopic carpal tunnel release for recurrent carpal tunnel syndrome after previous open release. Hand Surg. 2004;9:235–239. doi: 10.1142/s0218810404002327. [DOI] [PubMed] [Google Scholar]
- 8.Hulsizer D.L., Staebler M.P., Weiss A.C. The results of revision carpal tunnel release following previous open versus endoscopic surgery. J Hand Surg Am. 1998;23:865Y869. doi: 10.1016/S0363-5023(98)80164-0. [DOI] [PubMed] [Google Scholar]
- 9.Beck J.D., Brothers J.G., Maloney P.J. Predicting the outcome of revision carpal tunnel release. J Hand Surg Am. 2012;37:282Y287. doi: 10.1016/j.jhsa.2011.10.040. [DOI] [PubMed] [Google Scholar]
- 10.Duclos L., Sokolow C. Management of true recurrent carpal tunnel syndrome: is it worthwhile to bring vascularized tissue? Chir Main. 1998;17:113Y117. doi: 10.1016/s0753-9053(98)80003-3. discussion 118. [DOI] [PubMed] [Google Scholar]
- 11.Forman D.L., Watson H.K., Caulfield K.A. Persistent or recurrent carpal tunnel syndrome following prior endoscopic carpal tunnel release. J Hand Surg Am. 1998;23:1010Y1014. doi: 10.1016/s0363-5023(98)80008-7. [DOI] [PubMed] [Google Scholar]
- 12.Cobb T.K., Amadio P.C., Leatherwood D.F. Outcome of reoperation for carpal tunnel syndrome. J Hand Surg Am. 1996;21:347Y356. doi: 10.1016/S0363-5023(96)80341-8. [DOI] [PubMed] [Google Scholar]
- 13.Wadstroem J., Nigst H. Reoperation for carpal tunnel syndrome. A retrospective analysis of forty cases. Ann Chir Main. 1986;5:54Y58. doi: 10.1016/s0753-9053(86)80049-7. [DOI] [PubMed] [Google Scholar]
- 14.Chang B., Dellon A.L. Surgical management of recurrent carpal tunnel syndrome. J Hand Surg Br. 1993;18:467Y470. doi: 10.1016/0266-7681(93)90148-9. [DOI] [PubMed] [Google Scholar]
- 15.Bilasy A., Facca S., Gouzou S. Canaletto implant in revision surgery for carpal tunnel syndrome: 21 case series. J Hand Surg Eur. 2012;37:682Y689. doi: 10.1177/1753193411431051. [DOI] [PubMed] [Google Scholar]
- 16.Kluemper C.T., Swafford R.E., Hankins M.J., Davis C.M., Brzezienski M.A., Jemison M.D. Flexor tenosynovectomy for recurrent carpal tunnel syndrome: a retrospective case series of 108 hands. HAND. April 2019 doi: 10.1177/1558944719840735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Soltani A.M., Allan B.J., Best M.J., Mir H.S., Panthaki Z.J. Revision decompression and collagen nerve wrap for recurrent and persistent compression neuropathies of the upper extremity. Ann Plast Surg. 2014 May;72(5):572–578. doi: 10.1097/SAP.0b013e3182956475. PubMed PMID: 24322638. [DOI] [PubMed] [Google Scholar]
- 18.Puckett B.N., Gaston R.G., Lourie G.M. A novel technique for the treatment of recurrent cubital tunnel syndrome: ulnar nerve wrapping with a tissue engineered bioscaffold. J Hand Surg Eur. 2011;36(2):130–134. doi: 10.1177/1753193410384690. [DOI] [PubMed] [Google Scholar]
- 19.Strickland J.W., Idler R.S., Lourie G.M., Plancher K.D. The hypothenar fat pad flap for management of recalcitrant carpal tunnel syndrome. J Hand Surg. 1996;21:840–848. doi: 10.1016/S0363-5023(96)80201-2. [DOI] [PubMed] [Google Scholar]
- 20.Chrysopoulo M.T., Greenberg J.A., Kleinman W.B. The hypothenar fat pad transposition flap: a modified surgical technique. Tech Hand Up Extrem Surg. 2006;10:150–156. doi: 10.1097/01.bth.0000225004.56982.42. [DOI] [PubMed] [Google Scholar]
- 21.Craft R.O., Duncan S.F.M., Smith A.A. Management of recurrent carpal tunnel syndrome with microneurolysis and the hypothenar. Fat Pad Flap Hand. 2007;2:85–89. doi: 10.1007/s11552-007-9025-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mathoulin C., Bahm J., Roukoz S. Pedicled hypothenar fat flap for median nerve coverage in recalcitrant carpal tunnel syndrome. Hand Surg. 2000;5:33–40. doi: 10.1142/s0218810400000120. [DOI] [PubMed] [Google Scholar]
- 23.Strickland J.W., Idler R.S., Lourie G.M., Plancher K.D. The hypothenar fat pad flap for management of recalcitrant carpal tunnel syndrome. J Hand Surg Am. 1996;21:840–848. doi: 10.1016/S0363-5023(96)80201-2. [DOI] [PubMed] [Google Scholar]
- 24.Tollestrup T., Berg C., Netscher D. Management of distal traumatic median nerve painful neuromas and of recurrent carpal tunnel syndrome: hypothenar fat pad flap. J Hand Surg Am. 2010;35:1010–1014. doi: 10.1016/j.jhsa.2010.03.035. [DOI] [PubMed] [Google Scholar]
- 25.Sotereanos D.G., Giannakopoulos P.N., Mitsionis G.I., Xu J., Herndon J.H. Vein-graft wrapping for the treatment of recurrent compression of the median nerve. Microsurgery. 1995;16(11):752–756. doi: 10.1002/micr.1920161110. [DOI] [PubMed] [Google Scholar]
- 26.Varitimidis S.E., Vardakas D.G., Goebel F., Sotereanos D.G. Treatment of recurrent compressive neuropathy of peripheral nerves in the upper extremity with an autologous vein insulator. J Hand Surg Am. 2001;26(2):296–302. doi: 10.1053/jhsu.2001.22528. [DOI] [PubMed] [Google Scholar]
- 27.Kokkalis Z.T., Jain S., Sotereanos D.G. Vein wrapping at cubital tunnel for ulnar nerve problems. J Shoulder Elbow Surg. 2010;19(2 suppl):91–97. doi: 10.1016/j.jse.2009.12.019. [DOI] [PubMed] [Google Scholar]
- 28.Kokkalis Z.T., Mavrogenis A.F., Ballas E.G. Collagen nerve wrap for median nerve scarring. J Orthoped. 2015;38(2):117–121. doi: 10.3928/01477447-20150204-04. [DOI] [PubMed] [Google Scholar]
- 29.Soltani A.M., Allan B.J., Best M.J., Mir H.S., Panthaki Z.J. A systematic review of the literature on the outcomes of treatment for recurrent and persistent carpal tunnel syndrome. Plast Reconstr Surg. 2013 Jul;132(1):114–121. doi: 10.1097/PRS.0b013e318290faba. Review. PubMed PMID: 2380691. [DOI] [PubMed] [Google Scholar]
- 30.U.S. Department Of Veteran Affairs . 2020. National Center for Veterans Analysis and Statistics.https://www.va.gov/vetdata/Veteran_Population.asp Retrieved from. [Google Scholar]