Abstract
Prescription drug spending and other financial factors (e.g., out-of-pocket costs) partially explain variation in cost-related medication nonadherence (CRN). Indicators of social capital such as neighborhood factors and social support may influence the health and well-being of older adults as they may rely on community resources and support from family and peers to manage conditions. Previous research on the relationship of social capital and CRN has limited evidence and contradictory findings. Hence, our objective is to assess the relationship of social capital indicators (neighborhood social cohesion, neighborhood physical disorder, positive social support, and negative social support) and CRN using a longitudinal design, 2006 to 2016, in a nationally representative sample of older adults in the United States (US). The Health and Retirement Study is a prospective panel study of US adults aged ≥ 50 years evaluated every two years. Data was pooled to create three waves and fitted using Generalized Estimating Equation modelling adjusting for both baseline and timevarying covariates (age, sex, education, race, total household income, and perceived health status). The three waves consisted of 11,791, 12,336, and 9,491 participants. Higher levels of neighborhood social cohesion and positive social support were related with lower CRN (OR 0.92, 95% CI 0.88-0.95 and OR 0.77, 95% CI 0.70-0.84, p<0.01). In contrast, higher levels of neighborhood physical disorder and negative social support were related to higher CRN (OR 1.07, 95% CI 1.03-1.11 and OR 1.46, 95% CI 1.32-1.62, p<0.01). Interventions targeting social capital are needed, reinforcing positive social support and neighborhood social cohesion and diminishing neighborhood physical disorder and negative social support for older adults.
Keywords: Social capital, Cost-related medication nonadherence, Neighborhood social cohesion, Neighborhood physical disorder, Positive social support, Negative social support
Highlights
-
•
To our knowledge, the first study assessing social capital and CRN over time.
-
•
Risk of CRN was abated by neighborhood social cohesion and positive social support.
-
•
Risk of CRN was reinforced by neighborhood physical disorder and negative support.
-
•
Age, gender, and race were non-modifiable factors associated with CRN.
-
•
Education and health status were modifiable risk factors associated with CRN.
Introduction
The behavior of taking medications is a widely researched topic especially among older adults. In the United States, a study revealed that 41% of older adults, aged 65 years or older (n = 17,569), reported taking five or more prescribed medications (Wilson et al., 2007). Interestingly, approximately half of the sample disclosed being nonadherent to prescribed medications, and slightly more than a quarter of the sample was affected by any cost-related nonadherence (Wilson et al., 2007). This phenomenon is known as cost-related medication non-adherence (CRN) impacting vulnerable populations such as older adults (Briesacher, Gurwitz, & Soumerai, 2007; Lee, Jiang, Dowdy, Hong, & Ory, 2018). With the rising cost of drugs, individuals are forgoing treatment (skipping doses, splitting pills, delaying or stopping fills, etc.) as they are unable to afford needed medications (Lee et al., 2018). As medications are a cornerstone of condition management, medication nonadherence may exacerbate conditions and lead to poor health outcomes with increased risk of downstream complications. Furthermore, economic consequences include higher health care utilization and higher health care costs. For example, a systematic review by Cutler et al. found the annual costs attributed to medication nonadherence across conditions to range from $949 to $44,190 per person (Cutler, Fernandez-Llimos, Frommer, Benrimoj, & Garcia-Cardenas, 2018). Consequently, at the collective level, this costs the US health care system between $100 billion and $289 bllion annually (Viswanathan et al., 2012).
Prescription drug spending and other financial factors (e.g. out-of-pocket expenses, prescription drug coverage) partially explain variation in CRN behavior (Briesacher et al., 2007; Kurlander, Kerr, Krein, Heisler, & Piette, 2009; Zivin, Ratliff, Heisler, Langa, & Piette, 2011). Findings suggest non-modifiable factors such as younger age among the older adult population and female gender as drivers of CRN (Briesacher et al., 2007; Kang, Lobo, Kim, & Sohn, 2018; Zivin et al., 2011). In fact, additional drivers play a vital role in CRN with complex relationships. For example, Piette et al. developed a conceptual model for CRN behaviors, with an adaptation of the framework by Briesacher et al. both highlighting financial factors as main effects for CRN, but acknowledging secondary effects (e.g., sociodemographics, perceived risks/benefits, health literacy, mental/physical health, side effects, etc.) and potential mediators (trust, accessibility, coordination of care, etc.) as factors associated with the difference in response to medication costs despite similar financial resources (Briesacher et al., 2007; Piette, Heisler, Horne, & Caleb Alexander, 2006). Indicators of social capital may be regarded as potential determinants by cultivating access to support and resources as well as fostering trust in the community. This emphasizes the need to explore and develop strategies and initiatives to hone efforts on addressing the factors of an individual's environment that are inhibiting individuals of achieving their best health, especially considering different factors instead of financial factors alone (August & Billimek, 2016; Briesacher et al., 2007; Donkin, Goldblatt, Allen, Nathanson, & Marmot, 2018; Piette et al., 2006).
Older adults often rely on the community for support and resources. They are especially susceptible because of reduced mobility, adverse health conditions, and increased health needs. Contextual factors that impact the health of older adults are related to residing in areas lacking accessible or reliable transportation making access to preventive health care services difficult, residing in healthy food priority areas lacking access to affordable healthy food options, or residing in areas lacking walkable public spaces for physical and social activity. Social capital has been defined as trust, reciprocity, social cohesion, social support, mutual accountability, and associated resources that are aspects of social structure that fosters participation for communal benefit (Baum, 2003; Coleman, 1988; Portes, 1998; Putnam, Leonardi, & Nanetti, 1993). For example, an individual's neighborhood environment, an indicator of social capital, has been reported to influence health and health behaviors of older adults in several studies (Billimek & Sorkin, 2012; de Vries McClintock et al., 2015; S. Kim, Spilman, Liao, Sacco, & Moore, 2018; Rouxel et al., 2015; Schmitz et al., 2012; Smalls, Gregory, Zoller, & Egede, 2014, 2015; Sun & Yuan, 2019; Warner et al., 2013). Specifically, neighborhood social cohesion and neighborhood physical disorder may be indicators of interest. For example, Kim and Kawachi manifested that increased levels of neighborhood social cohesion was beneficial with regards to preventive healthcare use in obtaining vaccinations, testing, and screenings in older adults (E. S. Kim & Kawachi, 2017). Additionally, findings from studies utilizing the Health and Retirement Study data, indicated individuals with higher levels of neighborhood social cohesion were less likely to develop cardiometabolic conditions (Robinette, Charles, & Gruenewald, 2018), had lower risk of stroke (E. S. Kim, Park, & Peterson, 2013), and lower likelihood of insomnia (Chen-Edinboro et al., 2014), respectively. In contrast, increased levels of neighborhood physical disorder may exhibit an opposite effect. Previous studies have shown a negative relationship between high levels of neighborhood physical disorder (dilapidated or vacant properties and presence of graffiti, vandalism, or garbage) and health (Population Reference Bureau, n.d.; Skogan, 1992) with this relationship extending to older adults. For example, Clarke et al. found individuals living in neighborhoods with a higher level of physical disorder experienced a faster rate of cognitive decline compared with individuals living in neighborhoods with lower levels of physical disorder (Clarke, Weuve, Barnes, Evans, & Mendes de Leon, 2015). Aside from neighborhood indicators, social support may be an indicator of significance in assessing social capital. Based upon the glossary definition of social capital published by Moore and Kawachi, “social capital refers to the resources to which individuals and groups have access through their social networks” (Moore & Kawachi, 2017). Accordingly, social support could be considered to be an aspect of social resources that contribute to social capital. This includes the exchange of social support and information within social networks with levels of trust influencing these exchanges (Kawachi & Berkman, 2000). Social support is crucial since it has been suggested to be a protective factor later in life preserving positive health status. Social support has been widely studied regarding its relationship with health outcomes (DiMatteo, 2004) as well. Social support in older adults may promote adherence by several mechanisms such as increased self-esteem and relieving stress, thereby positively impacting health outcomes (Peggy A. Thoits, 2011). In a meta-analysis conducted by DiMatteo, results suggest a relationship between family social support and adherence (DiMatteo, 2004). Individuals with low family cohesiveness had 1.74 times higher risk of nonadherence compared to individuals with high family cohesiveness (DiMatteo, 2004).
The aforementioned findings from studies investigating the impact of social capital indicators in various contexts could be considered of notable evidence highlighting the importance of social capital on health and overall wellbeing. However, a gap exists as literature is lacking concerning the relationship of social capital and CRN among older adults. To date, a Brazilian study using cross-sectional data conducted by Luz et al. examined aspects of social capital (neighborhood trust, perception of physical environment, and perception of attachment to the neighborhood) and CRN among adults aged 60 years or older. The authors found an inverse relationship between both perception of attachment to the neighborhood and perception of help with CRN based on the Greater Metropolitan Belo Horizonte Health Survey (Luz, Loyola Filho, & Lima-Costa, 2011). In contrast, a cohort study published by Oksanen et al. with participants with an age range of 22–66 years, linked a workplace social capital survey to pharmacy records based upon the Finnish healthcare system and did not find an association between workplace social capital and adherence to antihypertensive medications for employees (Oksanen et al., 2011). The study implemented a year of follow up after completion of the survey, with multiple assessments for the outcome to account for time variation in social capital as it relates to adherence behavior. The results of this study, however, are not generalizable to the population in the United States as the study was based on a national health insurance system. Based on the study design of this previous work, analyzing this relationship with longitudinal data taking into account a life course perspective and the investigation of several social capital indicators simultaneously with data from the United States would importantly contribute to this body of knowledge.
To gain a better understanding of the relationship between CRN and social capital in older adults, our aim is to assess the relationship of social capital indicators (neighborhood social cohesion, neighborhood physical disorder, positive social support, and negative social support) and CRN in older adults using the Health and Retirement Study data. To our knowledge, our study will be the first to assess this relationship using a longitudinal study design in a national representative sample of older adults in the United States over time. The richness of the data resulting from the inclusion of the diverse social capital indicators will allow us to investigate on aspects of deeper meaning in the realm of attitudes, behavior, identity, and values of the individuals and community. We hypothesize individuals with higher levels of social cohesion, lower levels of physical disorder, more exposure to positive social support and less exposure to negative social support will be less likely to report CRN.
Methods
Study design and data source
We conducted a retrospective longitudinal cohort study using the Health and Retirement Study (HRS) dataset. The HRS is a nationally representative and prospective panel study of U.S. adults aged 50 years, conducted by the University of Michigan's Institute for Social Research. Since 1992, the data are collected every two years and utilizes a multi-stage area probability sampling of households. Detailed information regarding the HRS protocol, instrumentation, and complex sampling strategy is reported elsewhere (http://hrsonline.isr.umich.edu/). Response rates for the core interview are considerably high, with the baseline response rate ranging from 47.4% to 81.3% across study entry cohorts and an average of 73.0% and re-interview response rates ranging from 68.8% to 92.3% (Health and Retirement Study, 2017).
Study sample
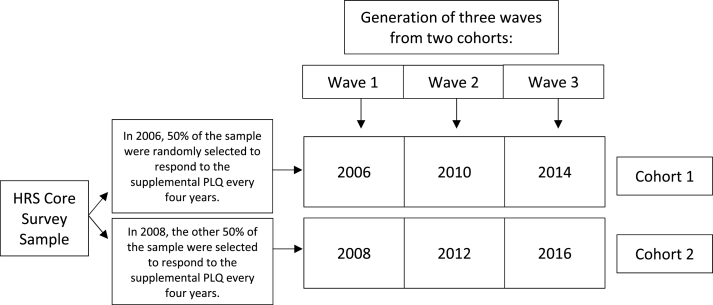
The study sample was derived using six waves of panel data from 2006 to 2016; each wave is surveyed every 2 years as part of the core survey. The Psychosocial and Lifestyle Questionnaire (PLQ) is a supplemental questionnaire administered to complement the in-person core surveys. The focus of this study relates to the lifestyle (neighborhood evaluation) and social relationships (positive and negative support). Starting in 2006, a random 50% of HRS respondents were selected as the first cohort to receive a supplemental Psychosocial and Lifestyle questionnaire that was self-reported every other wave (every four years). The remaining 50% were selected as the second cohort and followed the same process starting in 2008 (Fig. 1).
Fig. 1.
Creation of the study sample into three waves utilizing two cohorts formed from the administration of the supplemental Psychosocial and Lifestyle Questionnaire (PLQ). HRS: Health and Retirement Study.
The first PLQ cohort had three waves of assessments in 2006, 2010, and 2014 and the second PLQ cohort had three waves of assessments in 2008, 2012, and 2016 (Fig. 1). Data was pooled from the first and second PLQ cohorts to create three waves. Therefore, wave 1 includes the initial PLQ measurements in years 2006 and 2008, wave 2 includes measurements in years 2010 and 2012, and wave 3 includes measurements in years 2014 and 2016. Respondents of the mail-in Psychosocial and Lifestyle questionnaire module have sample weights to account for the complex sampling design. The weights are a product of three factors: 1) The core of nursing home weights for the given wave, 2) A non-response adjustment factor obtained from a propensity score model predicting Psychosocial and Lifestyle responses, and 3) A post-stratification adjustment to the weighted HRS sample. HRS is sponsored by the National Institute on Aging (grant number NIA U01AG009740) and has been approved by several ethics committees, including University of Michigan IRB (IRB protocol HUM00061128) (Health and Retirement Study, 2018). Informed consent was obtained from all HRS respondents.
Our analysis was restricted to a final sample of 16,521 HRS participants. The inclusion/exclusion criteria was applied to the starting sample of n = 31,102 HRS participants from 2006 to 2016 with the sample size remaining as follows: who were eligible for the PLQ survey (n = 27,237), did not move their residence (n = 24,178), did not reside in a nursing home (n = 23,153), had complete data for the cost-related medication non-adherence (CRN) item from the core survey (n = 23,052) as well as the social capital indicators from the PQL survey (n = 18,848), and were aged 50 years or older (n = 18,446). In addition, complete data regarding covariates (age, sex, race, education, total household income, perceived health status) were required to be included in the analysis (n = 16,521). The analysis resulted in approximately 11% loss of participants, ranging from 3 to 17% loss of observations by wave.
A total of 8,964 and 7,557 HRS participants were included from the first (years 2006, 2010, and 2014) and second (years 2008, 2012, and 2016) cohorts, respectively. Moreover, the pooling of the data from the two cohorts distributed participants across three waves as follows: n = 11,791 participants in wave 1 (2006 & 2008), n = 12,336 participants in wave 2 (2010 & 2012), and n = 9,491 participants in wave 3 (2014 & 2016). Individuals are followed over time and may be represented in more than one wave. Similarly, individuals may be considered new cohort participants and thus, may have representation beginning in waves 2 or 3.
Variables and measurements
Cost-related medication non-adherence
Cost-related medication non-adherence (CRN) was measured in the core survey with the question, “Sometimes people delay taking medication or filling prescriptions because of the cost. At any time have you ended up taking less medication than was prescribed for you because of the cost?“. CRN was assessed by a yes/no response within the corresponding years for the two distinct cohorts. Measures of CRN (i.e., did not fill a prescription because it was too expensive, skipped doses to make medication last longer, took less medicine than prescribed to make the medicine last longer) have been widely used, previously validated, and are similar to measures of CRN in other studies in older adults (Burcu, Alexander, Ng, & Harrington, 2015; Gellad, Haas, & Safran, 2007; Pierre-Jacques et al., 2008; Safran et al., 2005; Soumerai et al., 2006; Warth et al., 2019; Zivin et al., 2011). Based upon CRN data from the HRS Prescription Drug Study, Zivin et al. confirmed results are similar when using CRN as a global measure or as behaviors separately (e.g., not filling prescriptions because of cost and delaying taking medication) (Zivin et al., 2011).
Social capital indicators
Perceived neighborhood social cohesion and neighborhood physical disorder
Perceived neighborhood social cohesion was assessed using a four-item scale that was developed and tested for use in two nationally representative studies of older adults using data from the Chicago Neighborhood and Disability Study (CNDS) which was integrated into the Chicago Health and Aging Project (CHAP) (Cagney et al., 2009; Mendes De Leon et al., 2009). The survey items for CNDS/CHAP were derived from previous research (Balfour & Kaplan, 2002; K. J.; Fisher, Li, Michael, & Cleveland, 2004; Jencks & Mayer, 1990; R J; Sampson, Raudenbush, & Earls, 1997; Robert J.; Sampson, Morenoff, & Gannon-Rowley, 2002). The scale assesses the respondent's perceived level of social cohesion and social trust in his or her neighborhood. Using a 7-point Likert scale, respondents indicated the degree to which they endorsed the following four items: “I really feel part of this area”, “If you were in trouble, there are lots of people in this area who would help you”, “Most people in this area can be trusted”, and “Most people in this area are friendly”. The score was calculated as missing if more than two items contained missing values. The index was created by reverse coding all four items and averaging the scores across all items. Higher scores reflected higher perceived neighborhood social cohesion. Cronbach α has been evaluated in previous studies ranging from 0.60 to 0.86 (Cagney et al., 2009; Mendes De Leon et al., 2009; Smith, Ryan, Fisher, Sonnega, & Weir, 2017). Our results were similar across waves ranging from 0.84 to 0.87.
Perceived Neighborhood physical disorder was assessed using a four-item scale that was developed and tested for use in two nationally representative studies of older adults using data from the Chicago Neighborhood and Disability Study (CNDS) which was integrated into the Chicago Health and Aging Project (CHAP) (Cagney et al., 2009; Mendes De Leon et al., 2009). The survey items for CNDS/CHAP were derived from previous research (Balfour & Kaplan, 2002; K. J.; Fisher et al., 2004; Jencks & Mayer, 1990; R J; Sampson et al., 1997; Robert J.; Sampson et al., 2002). The scale assesses the respondent's perceived level of physical disorder in the neighborhood using a 7-point Likert scale. The four items comprising the scale include: “Vandalism and graffiti are a big problem in this area”, “People would be afraid to walk alone in this area after dark”, “This area is always full of litter and rubbish”, and “There are many vacant or deserted houses or storefronts in this area”. In 2006, the index was created by reverse coding all four items due to the change in coding in the subsequent years. The index was created by averaging the scores across all items. The score was calculated as missing if more than two items contained missing values. Higher scores reflected higher perceived neighborhood physical disorder. Cronbach α has been evaluated in previous studies ranging from 0.64 to 0.88 (Cagney et al., 2009; Mendes De Leon et al., 2009; Smith et al., 2017). Our results were similar across waves ranging from 0.75 to 0.85.
In some studies, neighborhood social cohesion and neighborhood physical disorder are examined at the aggregated neighborhood level using multilevel modeling (Murayama, Fujiwara, & Kawachi, 2012) However, this requires a nested study design with many residents clustered in many neighborhoods, which was not available in this sample. Therefore, this study focuses on people's perceptions of neighborhood social cohesion and neighborhood physical disorder at the individual level.
Perceived social support
Positive social support was examined for different relationship categories (spouse/partner, children, other family, and friends) separately using the following three questions based on a 4-point Likert scale (1 = A lot, 4 = Not at all): “How much do they really understand the way you feel about things?“, “How much can you rely on them if you have a serious problem?“, and “How much can you open up to them if you need to talk about your worries?“. The positive social support index was created by reverse coding all three items and averaging the scores across all items within each relationship category. The scores within each relationship category were combined as an overall average. The score was calculated as missing if more than one item contained missing values. Higher scores reflected higher perceived positive social support. This measure has been widely used and validated. The social support measure was derived from previous measures of affective support (Turner, Frankel, & Levin, 1983). Cronbach α has been evaluated in previous studies ranging from 0.80 to 0.88 (Ha, Kahng, & Choi, 2017; Schuster, Kessler, & Aseltine, 1990; Smith et al., 2017; Walen & Lachman, 2000). Our results were similar across waves ranging from 0.81 to 0.86.
Negative social support was examined for different relationship categories (spouse/partner, children, other family, and friends) separately using the following four questions based on a 4-point Like scale (1 = A lot, 4 = Not at all): “How often do they make too many demands on you?“, “How much do they criticize you?“, and “How much do they let you down when you are counting on them?“. The negative social support index was created by reverse coding all four items and averaging the scores across all items within each relationship category. The scores within each relationship category were combined as an overall average. The score was calculated as missing if more than two items contained missing values. Higher scores reflected higher negative social support. This measure has been widely used and validated. The social support measure was derived from previous measures of affective support (Turner et al., 1983). Cronbach α has been evaluated in previous studies ranging from 0.73 to 0.81 (Ha et al., 2017; Schuster et al., 1990; Smith et al., 2017; Walen & Lachman, 2000). Our results were similar across waves ranging from 0.75 to 0.80.
Sociodemographic and health characteristics
The following sociodemographic factors were assessed for all waves: age (numerical mean), sex (male, female), educational attainment (no degree, high school or general educational development (GED), some college or college degree, Masters and Professional degrees), total household income (<$25,000, $25,000-$49,999, $50,000-$74,999, $75,000-$99,999, ≥$100,000), and perceived health status (poor, fair, good, very good, excellent). As described in the RAND HRS Detailed Imputations File 2016 (V2) Documentation, “the HRS public release provide imputations for many asset and income types in earlier waves, but the imputation method is not consistent across all waves, and there are no imputations in more recent waves” (Bugliari et al., 2019). As a result, total household income was based on consistent imputation methods by RAND across waves including the following underlying covariates: (transformations of) husband and wife's employment status, education, health status, age, race, marital status, occupation class, cognition, and bequest expectations (Bugliari et al., 2019). The race variable was created by combining information from race (White, African American or other) and from Hispanic origin (Mexican, Hispanic or Other). Final categories were White, African American, Hispanic, and Other).
Statistical analysis
Individuals with complete information by wave were included, n = 11,791, 12,336, and 9,491 observations across three waves, respectively. Before pooling data from the first and second cohorts, we quantitatively examined whether there were differences between the individuals from these cohorts across waves. No differences were found allowing the data to be pooled, and thereby creating three waves. Descriptive statistics were performed for the comparisons between the sample characteristics of the three waves via frequencies and percentages or means and standard errors for categorical and continuous variables, respectively. Following, we used a Generalized Estimating Equation modeling approach (GEE) to investigate the relationship between each social capital indicator (neighborhood social cohesion and neighborhood physical disorder, positive social support and negative social support) and CRN accounting for both baseline and time-varying covariates (age, total household income, perceived health status, and social capital indicators) with four separate models. The model specification included a logit link and binomial family, with an exchangeable correlation structure. Due to the limitations in conducting a GEE in SAS with complex survey data, two modeling approaches were analyzed. One approach considered the survey weights and repeated observations (e.g., respondent ID) while the second modeling approach considered the complex survey design variables and survey weights. The complex sampling design was taken into account in order to obtain more reliable standard deviations and standard errors (G. G. Fisher & Ryan, 2018). The individuals were clustered within primary stage units defined by U.S. Metropolitan Statistical Areas (Heeringa & Connor, 1995). Results from the two approaches were similar, and therefore, we proceeded with the approach recognizing survey weights and repeated observations to prioritize adjustment for correlation between the repeated measures for the same respondent. It is important to note, as the weights for the 2016 data were unavailable, weights of the individuals present in the previous wave were utilized, therefore, excluding new individuals entering in 2016. As the results of wave 3 were aligned with waves 1 and 2, we felt this does not impact the interpretation of our results. Lastly, since previous literature observed important sex differences in social trust, neighborhood closeness, and neighborhood safety (Chuang & Chuang, 2008; Kavanagh, Bentley, Turrell, Broom, & Subramanian, 2006), we explored sex differences by assessing the interaction between sex and social capital indicators. None of the interaction terms, however, were statistically significant, and therefore, we deleted the interaction term of the final models (Vyncke et al., 2014; Zivin et al., 2011). SAS 9.4 (SAS Institute Inc., Cary, NC, USA) software was used to build the analytical file and conduct analyses.
Results
Using data from 2006 to 2016, Table 1 shows the descriptive characteristics of the HRS participants (n = 11,791, n = 12,336, and n = 9,491) across the three waves. Among the participants, 8.5%, 10%, and 7.9% had experienced CRN within the last two years. Participants had an average age at baseline of 66.4 years (wave 1), 65.5 years (wave 2), and 68 years (wave 3). The majority of participants were White (81.5%, 79.5%, 80.2%, respectively) across the three waves. Approximately half of the participants attained a GED or high school diploma as the most frequent level of education. Likewise, approximately half of the participants had a total household income less than $50,000. Over time, the trend of perceived health status and social capital indicators remained stable. For example, participants reported higher levels of perceived neighborhood cohesion and lower levels of perceived neighborhood physical disorder across waves. Similarly, the sample reported having higher positive social support in contrast to negative social support.
Table 1.
Descriptive statistics of cost-related medication nonadherence, social capital indicators and covariates by wave in the United States, the Health and Retirement Study data from 2006 to 2016.
|
Characteristics |
Wave 1 (n = 11,791) |
Wave 2 (n = 12,336) |
Wave 3 (n = 9,491) |
|||
|---|---|---|---|---|---|---|
| n | %/Mean (SE) | n | %/Mean (SE) | n | %/Mean (SE) | |
| Cost-Related Medication Nonadherence | ||||||
| No | 10,828 | 91.55 | 11,151 | 90.00 | 8,714 | 92.11 |
| Yes | 963 | 8.45 | 1,185 | 10.00 | 777 | 7.89 |
| Age | 66.39 (0.17) | 65.45 (0.26) | 68.04 (0.27) | |||
| Sex | ||||||
| Male | 5,062 | 46.73 | 5,262 | 46.59 | 3,922 | 45.99 |
| Female | 6,729 | 53.27 | 7,074 | 53.40 | 5,569 | 54.01 |
| Race | ||||||
| White | 9,203 | 81.52 | 8,929 | 79.53 | 6,799 | 80.19 |
| African American | 1,441 | 8.90 | 1,820 | 9.18 | 1,414 | 8.77 |
| Hispanic | 895 | 7.28 | 1,239 | 8.19 | 1,004 | 7.97 |
| Other | 252 | 2.29 | 348 | 3.10 | 274 | 3.07 |
| Education | ||||||
| No degree | 2,205 | 16.50 | 1,958 | 13.17 | 1,378 | 11.71 |
| GED/High School | 6,461 | 53.72 | 6,671 | 52.23 | 5,117 | 51.74 |
| Some college/College degree | 2,030 | 19.31 | 2,466 | 22.82 | 1,955 | 23.50 |
| Master/Professional | 1,095 | 10.46 | 1,241 | 11.78 | 1,041 | 13.06 |
| Perceived Health Status | ||||||
| Poor | 824 | 7.45 | 786 | 6.44 | 545 | 5.51 |
| Fair | 2,363 | 19.00 | 2,315 | 17.39 | 1,917 | 18.16 |
| Good | 3,736 | 30.25 | 4,006 | 30.59 | 3,311 | 33.26 |
| Very Good | 3,612 | 31.41 | 3,994 | 33.77 | 2,958 | 33.86 |
| Excellent | 1,256 | 11.88 | 1,236 | 11.80 | 760 | 9.21 |
| Total Household Incomeb | ||||||
| <$25,000 | 3,498 | 26.59 | 3,517 | 24.65 | 2,565 | 22.25 |
| $25,000 - $49,999 | 3,419 | 26.68 | 3,423 | 24.18 | 2,516 | 23.02 |
| $50,000 - $74,999 | 1,885 | 16.36 | 2,002 | 16.72 | 1,569 | 16.81 |
| $75,000–99,999 | 1,037 | 9.76 | 1,187 | 10.83 | 935 | 11.06 |
| ≥$100,000 | 1,952 | 20.62 | 2,207 | 23.63 | 1,906 | 26.87 |
| Social Capital Indicatorsa | ||||||
| Neighborhood Social Cohesion | 5.52 (0.02) | 5.50 (0.02) | 5.46 (0.02) | |||
| Neighborhood Physical Disorder | 2.43 (0.02) | 2.48 (0.02) | 2.42 (0.03) | |||
| Positive Social Support | 3.13 (0.01) | 3.13 (0.01) | 3.13 (0.01) | |||
| Negative Social Support | 1.66 (0.01) | 1.65 (0.01) | 1.62 (0.01) | |||
Note: Individuals may be represented across waves or may be considered new cohort participants by having representation beginning in waves 2 or 3.
Reversed scale; Higher scores indicate higher values for Neighborhood Social Cohesion, Positive Social Support, and Negative Social Support.
Total Household Income was based on consistent imputation methods by RAND across waves.
After adjusting for both baseline and time-varying covariates (age, sex, education, race, total household income, and perceived health status) in the four GEE models (neighborhood social cohesion, neighborhood physical disorder, positive social support, and negative social support; social capital indicators modeled separately), neighborhood social cohesion and positive social support were suggested as protective factors for CRN (Table 2). Each one-unit increase in neighborhood social cohesion and positive social support was associated with a multivariate-adjusted odds ratio (OR) for CRN of 0.92 (95% CI, 0.88–0.95, p < 0.01) and 0.77 (95% CI, 0.70–0.84, p < 0.01), respectively. This suggests that overall higher levels of neighborhood social cohesion and positive social support promotes overall lower CRN across all waves. In contrast, risk of CRN was reinforced by higher levels of neighborhood physical disorder and negative social support. Each one-unit increase in neighborhood physical disorder and negative social support was associated with a multivariate-adjusted OR of 1.07 (95% CI, 1.03–1.11) and OR 1.46 (95% CI, 1.32–1.62) (p < 0.01) indicating that overall higher levels of neighborhood physical disorder and negative social support influence overall higher CRN across all waves.
Table 2.
Results from the Generalized Estimated Equation models to test the association between social capital indicators and cost-related medication nonadherence in the United States, the Health and Retirement Study data from 2006 to 2016.
| Social Capital Indicator Models: |
Neighborhood Social Cohesion |
Neighborhood Physical Disorder |
Positive Social Support |
Negative Social Support |
||||
|---|---|---|---|---|---|---|---|---|
| Covariates | OR (95% CI) | p-valuea | OR (95% CI) | p-valuea | OR (95% CI) | p-valuea | OR (95% CI) | p-valuea |
| Wave Number | ||||||||
| Wave 1 (Reference) | 1.00 | – | 1.00 | – | 1.00 | – | 1.00 | – |
| Wave 2 | 1.22 (1.10–1.36) | <0.01a | 1.22 (1.10–1.35) | <0.01a | 1.23 (1.11–1.36) | <0.01a | 1.23 (1.11–1.37) | <0.01a |
| Wave 3 | 1.10 (0.98–1.24) | 0.11 | 1.11 (0.99–1.25) | 0.08 | 1.11 (0.99–1.25) | 0.09 | 1.12 (1.00–1.27) | 0.06 |
| Age | 0.94 (0.94–0.95) | <0.01a | 0.94 (0.93–0.95) | <0.01a | 0.94 (0.94–0.95) | <0.01a | 0.94 (0.94–0.95) | <0.01a |
| Sex | ||||||||
| Male (Reference) | 1.00 | – | 1.00 | – | 1.00 | – | 1.00 | – |
| Female | 1.55 (1.38–1.74) | <0.01a | 1.54 (1.37–1.73) | <0.01a | 1.60 (1.43–1.80) | <0.01a | 1.52 (1.35–1.71) | <0.01a |
| Race | ||||||||
| White (Reference) | 1.00 | – | 1.00 | – | 1.00 | – | 1.00 | – |
| African American | 1.28 (1.11–1.48) | <0.01a | 1.28 (1.11–1.47) | <0.01a | 1.37 (1.19–1.58) | <0.01a | 1.29 (1.12–1.49) | <0.01a |
| Hispanic | 0.89 (0.74–1.09) | 0.26 | 0.90 (0.74–1.09) | 0.26 | 0.94 (0.78–1.14) | 0.54 | 0.92 (0.76–1.11) | 0.39 |
| Other | 1.30 (0.96–1.75) | 0.09 | 1.31 (0.97–1.76) | 0.08 | 1.31 (0.97–1.77) | 0.08 | 1.25 (0.92–1.68) | 0.15 |
| Education | ||||||||
| No degree (Reference) | 1.00 | – | 1.00 | – | 1.00 | – | 1.00 | – |
| GED/High School | 0.94 (0.81–1.10) | 0.43 | 0.94 (0.81–1.10) | 0.44 | 0.93 (0.80–1.08) | 0.32 | 0.93 (0.80–1.09) | 0.37 |
| Some college/College degree | 0.90 (0.74–1.10) | 0.29 | 0.91 (0.74–1.11) | 0.33 | 0.88 (0.72–1.07) | 0.20 | 0.88 (0.72–1.07) | 0.20 |
| Master/Professional | 0.93 (0.70–1.24) | 0.62 | 0.94 (0.71–1.25) | 0.68 | 0.91 (0.68–1.21) | 0.51 | 0.91 (0.69–1.21) | 0.52 |
| Total Household Incomec | ||||||||
| <$25,000 (Reference) | 1.00 | – | 1.00 | – | 1.00 | – | 1.00 | – |
| $25,000 - $49,999 | 0.81 (0.71–0.92) | <0.01a | 0.81 (0.71–0.92) | <0.01a | 0.82 (0.72–0.93) | <0.01a | 0.81 (0.71–0.92) | <0.01a |
| $50,000 - $74,999 | 0.63 (0.53–0.74) | <0.01a | 0.63 (0.53–0.74) | <0.01a | 0.63 (0.54–0.74) | <0.01a | 0.63 (0.53–0.74) | <0.01a |
| $75,000–99,999 | 0.48 (0.39–0.59) | <0.01a | 0.48 (0.39–0.59) | <0.01a | 0.48 (0.39–0.59) | <0.01a | 0.47 (0.38–0.58) | <0.01a |
| ≥$100,000 | 0.30 (0.24–0.37) | <0.01a | 0.30 (0.24–0.37) | <0.01a | 0.30 (0.24–0.37) | <0.01a | 0.29 (0.24–0.37) | <0.01a |
| Perceived Health Status | ||||||||
| Poor (Reference) | 1.00 | – | 1.00 | – | 1.00 | – | 1.00 | – |
| Fair | 0.75 (0.63–0.88) | <0.01a | 0.74 (0.63–0.87) | <0.01a | 0.76 (0.64–0.89) | <0.01a | 0.76 (0.64–0.90) | <0.01a |
| Good | 0.43 (0.36–0.51) | <0.01a | 0.42 (0.36–0.50) | <0.01a | 0.43 (0.36–0.51) | <0.01a | 0.44 (0.37–0.52) | <0.01a |
| Very Good | 0.23 (0.19–0.28) | <0.01a | 0.23 (0.19–0.27) | <0.01a | 0.24 (0.19–0.29) | <0.01a | 0.24 (0.20–0.29) | <0.01a |
| Excellent | 0.13 (0.10–0.18) | <0.01a | 0.13 (0.19–0.27) | <0.01a | 0.13 (0.10–0.18) | <0.01a | 0.14 (0.10–0.18) | <0.01a |
| Social Capital Indicator Estimateb | 0.92 (0.88–0.95) | <0.01a | 1.07 (1.03–1.11) | <0.01a | 0.77 (0.70–0.84) | <0.01a | 1.46 (1.32–1.62) | <0.01a |
Denotes statistically significant p < 0.05.
Reversed scale; Higher scores indicate higher values for Neighborhood Social Cohesion, Positive Social Support, and Negative Social Support, respectively. Models included covariates and one social capital indicator.
Total Household Income was based on consistent imputation methods by RAND across waves.
Discussion
In a nationally representative sample of older adults in the United States, we found the risk of CRN abated by higher levels of neighborhood social cohesion and positive social support. In contrast, risk of CRN was reinforced by higher levels of neighborhood physical disorder and negative social support. Social capital was measured at the individual level using perceived indicators of neighborhood social environment and social support. To our knowledge, this study represents the first consideration of assessing the relationship of social capital and CRN over time.
The results of the present study confirm our hypothesis of the possible influence of neighborhood and social environment on CRN. Moreover, the results are aligned with the findings from Luz et al. the only other study directly assessing the relationship between social capital and CRN as far as we know (Luz et al., 2011). The study utilized similar measures of social capital compared to our study and found lower levels of perception of attachment to the neighborhood and perception of help to be associated with CRN in Brazil (Luz et al., 2011). The work by Oksanen et al. evaluated workplace social capital and the effect on adherence to antihypertensive therapies (Oksanen et al., 2011). The authors did not find an association between the variables under study and a potential explanation for this finding may be due the measurement of social capital being limited to the workplace (not inclusive of neighborhood or social support factors outside the workplace) as well as the identification of individuals with hypertension based on entitlement to special reimbursement; chronic and severe hypertension with submission of required documentation. Additionally, the study only included the assessment of antihypertensive medications, whereas our study included assessments of CRN more broadly (e.g. any medication). As a result, social capital may affect conditions differently as certain conditions may be more at risk of CRN (Zivin et al., 2011).
Social capital may be a facet of an individual's environment stemming from a variety of settings. In the context of older adults, neighborhood factors and social support may influence the health and well-being of older adults as they spend more time within the home environment compared to their younger counterparts (Cramm, van Dijk, & Nieboer, 2013). Our results are in accordance with a theoretical model developed by August and Billimek, highlighting the importance of social and physical factors on shaping an individual's environment and health (August & Billimek, 2016). Moreover, our study emphasizes how multiple factors contribute to CRN suggesting shifting the culture of focusing on one aspect of an individual's life, to a multi-faceted approach to managing health, e.g. CRN. Needless to say, our social indicators, e.g., observing lack of neighborhood social cohesion or increased neighborhood physical disorder, extend beyond the surface of the physical attributes (e.g., perceived friendliness of people or observing vandalism and graffiti) of the measure. The image portrayed translates into a deeper meaning of attitudes, behavior, identity, and values of the individuals and community. The lack of safety, publicly available green space or community centers, and pedestrian infrastructure hinders participation in physical activity, the practice of health-seeking behaviors, social interaction via social gatherings deterring sense of community, mobility, and neighborly support (Adler & Newman, 2002; Cramm et al., 2013; Hirsch et al., 2016; Michael, Green, & Farquhar, 2006). It is important for older adults to have a sense of community to provide social integration, a sense of purpose, and emotional support (S. Cohen, 2004; P A Thoits, 1995; Peggy A. Thoits, 2011).
Accordingly, an individual living in an affluent neighborhood may have advantages that may not be available to another individual living in a less affluent neighborhood (Adler & Newman, 2002). An affluent neighborhood attracts affluent individuals with investment in increasing safety, access to leisure space, access to health promotion efforts and other public health and social services, and social networks. In contrast, less affluent neighborhoods are disadvantaged with lack of investment and maintenance, and thereby suffers from an increase in physical disorder, crime, poor health behaviors, instability, and lack of access to the aforementioned resources (Peterson & Krivo, 2009; Solari, 2012) creating stressors for the community (August & Billimek, 2016). Neighborhood stressors may be detrimental to an individual's self-care and health as these stressors warrant priority and immediate need distracting from sustaining positive health behaviors, and as a result, discounting health such as maintaining adherence to prescribed therapeutic regimens, and relevant to our study, the risk of CRN (August & Billimek, 2016). Furthermore, neighborhood physical disorder is commonly accompanied by low social cohesion resulting in diminished social interaction and support (August & Billimek, 2016).
Positive social support exists within social networks with higher levels of trust influencing these exchanges (Kawachi & Berkman, 2000). Moreover, positive social support has been shown to facilitate the motivation to take control over one's self, self-efficacy, and the reduction of stress (Mirowsky & Ross, 2003; Peggy A; Thoits, 2006). Consequently, this produces a positive effect on health (Uchino, 2006) with the likelihood of positive support being reciprocated (Fredrickson, 2001). Conversely, exposure to negative social support in the form of additional stress and demands of relationships triggers the absence of the feeling of belonging and acceptance by peers, thus diminishing sense of control and mental wellbeing (Mirowsky & Ross, 2003). Berglund et al. found negative social support to be related to nonadherence (Berglund, Lytsy, & Westerling, 2019). Similarly, another study found a higher risk of mortality among older women with lack of emotional support (Lyyra & Heikkinen, 2006). These findings provide support in explaining our findings of the relationship between higher levels of positive support and the decreased risk of CRN with the inverse relationship for negative social support and CRN.
Interestingly, our model yielded younger age, female gender, lower levels of income, lower levels of perceived health status, and being African American were associated with CRN; these findings are consistent with a literature review on CRN factors conducted by Briesacher et al. (Briesacher et al., 2007). Insurance coverage, a variable we did not include in our study due to low response rate, may explain the risk effect of younger ages and risk of CRN (Gu & Shen, 2019; Kang et al., 2018; Piette, Heisler, & Wagner, 2004). The Medicare benefit provides coverage for older adults when they reach 65 years old whereas younger individuals may not be eligible for experience the same prescription coverage benefits from their respective plans, if insured. Also, a healthcare providers’ intrinsic sense of their professional responsibility to address medication management may place an emphasis on managing older adults based upon the belief of greater importance with age (M. J. Cohen et al., 2012; Gu & Shen, 2019).
In addition, we found evidence of higher risk for CRN among African Americans when compared to Whites. This result ties well with previous studies wherein African Americans were factors more likely to report CRN compared to Whites driven by income and higher out-of-pocket prescription costs. (Gellad et al., 2007; Tseng et al., 2008). African Americans are inclined to live in deprived neighborhoods with less racial heterogeneity, lower socioeconomic status, and less education with smaller and less diverse networks when compared to the social networks of Whites, thereby impacting access to resources (Ajrouch, Antonucci, & Janevic, 2001; Mays, Cochran, & Barnes, 2007; McPherson, Smith-Lovin, & Brashears, 2006). The network may be comprised of a larger proportion of family members as it is hypothesized that family members may be more trusted compared to individuals outside of the family. The reliance on family may be a limiting factor in access to resources beyond the family if African American families are prone to have similar less affluent social networks and connections. The difference between affluent and poor neighborhoods has been shown to be steadily increasing over time on factors related to income, unemployment, race, proportion of female-headed households, and education (Solari, 2012). Furthermore, cultural differences in lifestyle, beliefs, and discrepancies in health care may be contributing factors (August & Billimek, 2016; Mays et al., 2007).
In essence, risk factors for CRN may be viewed as modifiable or non-modifiable with more effective adherence interventions encompassing multiple risk factors (De et al., 2016; Haynes, Ackloo, Sahota, McDonald, & Yao, 2008; van Eijken, Tsang, Wensing, de Smet, & Grol, 2003). The modifiable risk factors may include but are not limited to neighborhood conditions, education and poor perceived health status. Expansion of government programs (e.g., public school funding, safety initiatives, housing programs/policies, additional employment support services) to improve neighborhood conditions may be considered. Pre-existing community organizations may be leveraged to enhance communication and build trust within the community. Members of the community should be encouraged to participate in decision-making, thereby, allowing the community to feel empowered and have an increased sense of belonging by having their voices heard. It is of the utmost importance to strategize and develop initiatives through influenceable pathways and adapt interventions to an individual's social and physical environment. Therefore, programs to help individuals seek treatment or access resources as well as educate the importance of compliance with annual health and lifestyle recommendations should be adopted. This may be supported by healthy lifestyle policies and social support that address neighborhood factors, thereby improving CRN. On the other hand, for factors that are non-modifiable such as gender and age, CRN may be mitigated with viable solutions indirectly affecting these factors. For example, with the assistance of health care providers by prescribing less costly versions of medications (e.g., generics when available) or by providing additional resources for patients to utilize. This effort may be facilitated with the development of screening tools or prediction models via the use of big data to identify those at risk of CRN and should be considered as a priority (Zhang & Meltzer, 2016).
It is important to note that this study has several limitations. The survey data may be subjected to gaps in participant knowledge subjecting the study to recall bias. However, due to the nature of the outcome and specific covariates included in the model, the likelihood of recall bias is low. In addition, reverse causation may be of concern in the event the participants’ health conditions and/or CRN influenced the perceived level of neighborhood social cohesion, neighborhood physical disorder, or positive and negative social support. We explored the inclusion of additional variables in the model (e.g., comorbidities, alcohol use, smoking status, and marital status), however, to avoid overfitting the model, the variables were deleted as they did not provide additional information concerning the interpretation of our results. There is debate about whether social support is considered a part of social capital. However, according to the commonly accepted definition of social capital, i.e., resources available through social networks, social support could be considered to be an aspect of social capital (Moore & Kawachi, 2017). Notwithstanding the recommendation to measure social capital at the individual and at the community level, this data was not available in the Health and Retirement Study. As community-level indicators were not available, social capital was measured at the individual level using both perceived neighborhood measures and social support measures based upon validated scales as well as similarly reported measures in literature (Chen-Edinboro et al., 2014; Kawachi, Kennedy, Lochner, & Prothrow-Stith, 1997; E. S.; Kim, Hawes, & Smith, 2014; E. S.; Kim et al., 2013; E. S.; Kim & Kawachi, 2017; Luz et al., 2011; Robinette et al., 2018). As for the analysis, the rationale for assessing social capital via four separate models in place of consolidating the indicators to produce an overall score was deemed appropriate for two reasons. First, to avoid combining positive and negative scales, and second, to preserve information from each indicator. If the indicators were condensed to an overall score, the richness of information in understanding the contribution of each indicator would be lost, and our objective was to understand how these indicators affect CRN individually. For example, testing the hypothesis that higher levels neighborhood social cohesion and neighborhood physical disorder affect the risk of CRN differently; assume a similar effect for positive social support and negative social support.
Despite these limitations, the analysis has several strengths. This is one of two studies addressing the gap of assessing how social capital indicators impact CRN. Moreover, we measured the relationship of CRN and social capital with multiple time points utilizing all time periods of data available as well as accounting for time-varying factors. The pooling of survey data across individuals reduces the effect of “same source bias”. Utilizing information from one individual may create spurious associations based on an individual's perception and personal experience. Furthermore, due to the large sample size and oversampling features for race, this allowed us to generalize to the population of the U.S. of older adults. The data employs best practices for developing and administering surveys, therefore, providing quality data for the research community.
Overall, social capital may affect the well-being of older adults of whom rely heavily on their neighborhood, community resources and support from family and peers to manage medications for their conditions (Cramm et al., 2013). The lack of social capital deters sense of community, mobility, and neighborly support (Adler & Newman, 2002; Cramm et al., 2013; Hirsch et al., 2016; Michael et al., 2006). It is important for older adults to have a sense of community to provide social integration, a sense of purpose, and emotional support as social isolation and loneliness is highly prevalent among this population (S. Cohen, 2004; Fakoya, McCorry, & Donnelly, 2020; P A Thoits, 1995; Peggy A. Thoits, 2011).
As the size of the older adult population continues to grow, future research should aim to assess factors allowing individuals to continue adhering to medications with increases in cost to see if practices could be implemented or adopted among individuals experiencing CRN. Additionally, utilizing both qualitative and quantitative studies as well as subjective and objective measures to address this gap would be useful to complement existing knowledge. Identification of conditions that may be having the greatest impact on the relationship between social capital and CRN may shed insight where to focus efforts as well. Moreover, effective interventions targeting social capital are needed, reinforcing positive social support and neighborhood social cohesion and diminishing neighborhood physical disorder and negative social support of older adults.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethics statement
We acknowledge the ethical standards in publishing our research regarding authorship, originality and plagiarism, data access and retention, multiple, redundant or concurrent publications, acknowledgement of sources, disclosure and conflicts of interest, fundamental errors in published work, and reporting standards.
CRediT authorship contribution statement
Kayleigh R. Majercak: Conceptualization, Methodology, Software, Formal analysis, Validation, Data curation, Writing - original draft, Visualization. Laurence S. Magder: Methodology, Validation, Writing - review & editing. Ester Villalonga-Olives: Conceptualization, Methodology, Validation, Writing - review & editing.
Declaration of competing interest
None.
Acknowledgments
We acknowledge the support of the University of Maryland, Baltimore, Institute for Clinical & Translational Research (ICTR) and the National Center for Advancing Translational Sciences (NCATS) Clinical Translational Science Award (CTSA) grant number 1UL1TR003098. Partial funding for open access was provided by the University of Maryland Health Sciences and Human Services Library's Open Access Fund.
Contributor Information
Kayleigh R. Majercak, Email: kmajercak@umaryland.edu.
Laurence S. Magder, Email: lmagder@som.umaryland.edu.
Ester Villalonga-Olives, Email: ester.villalonga@rx.umaryland.edu.
References
- Adler N.E., Newman K. Socioeconomic disparities in health: Pathways and policies. Health Affairs. 2002;21(2):60–76. doi: 10.1377/hlthaff.21.2.60. [DOI] [PubMed] [Google Scholar]
- Ajrouch K.J., Antonucci T.C., Janevic M.R. Social networks among blacks and Whites: The interaction between race and age. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2001;56(2):S112–S118. doi: 10.1093/geronb/56.2.S112. [DOI] [PubMed] [Google Scholar]
- August K.J., Billimek J. A theoretical model of how neighborhood factors contribute to medication nonadherence among disadvantaged chronically ill adults. Journal of Health Psychology. 2016;21(12):2923–2933. doi: 10.1177/1359105315589391. [DOI] [PubMed] [Google Scholar]
- Balfour J.L., Kaplan G.A. Neighborhood environment and loss of physical function in older adults: Evidence from the alameda county study. American Journal of Epidemiology. 2002;155(6):507–515. doi: 10.1093/aje/155.6.507. [DOI] [PubMed] [Google Scholar]
- Baum F.E. Social capital. Journal of Epidemiology & Community Health. 2003;57:320–323. doi: 10.1136/jech.57.5.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berglund E., Lytsy P., Westerling R. Living environment, social support, and informal caregiving are associated with healthcare seeking behaviour and adherence to medication treatment: A cross‐sectional population study. Health and Social Care in the Community. 2019 doi: 10.1111/hsc.12758. hsc.12758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Billimek J., Sorkin D.H. Self-reported neighborhood safety and nonadherence to treatment regimens among patients with type 2 diabetes. Journal of General Internal Medicine. 2012;27(3):292–296. doi: 10.1007/s11606-011-1882-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briesacher B.A., Gurwitz J.H., Soumerai S.B. Patients at-risk for cost-related medication nonadherence: A review of the literature. Medicine. 2007;22:864–871. doi: 10.1007/s11606-007-0180-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bugliari D., Campbell N., Chan C., Hayden O., Hayes J., Hurd M. 2019. RAND HRS longitudinal file 2016 (V1) documentation.www.rand.org/well-being/social-and-behavioral-policy/centers/aging.html Retrieved from. [Google Scholar]
- Burcu M., Alexander G.C., Ng X., Harrington D. Construct validity and factor structure of survey-based assessment of cost-related medication burden. Medical Care. 2015;53(2):199–206. doi: 10.1097/MLR.0000000000000286. [DOI] [PubMed] [Google Scholar]
- Cagney K.A., Glass T.A., Skarupski K.A., Barnes L.L., Schwartz B.S., Mendes de Leon C.F. Neighborhood-level cohesion and disorder: Measurement and validation in two older adult urban populations. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2009;64(3):415–424. doi: 10.1093/geronb/gbn041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen-Edinboro L.P., Kaufmann C.N., Augustinavicius J.L., Mojtabai R., Parisi J.M., Wennberg A.M.V. Neighborhood physical disorder, social cohesion, and insomnia: Results from participants over age 50 in the health and retirement study. International Psychogeriatrics. 2014:1–8. doi: 10.1017/S1041610214001823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chuang Y.-C., Chuang K.-Y. Gender differences in relationships between social capital and individual smoking and drinking behavior in Taiwan. Social Science & Medicine. 2008;67(8):1321–1330. doi: 10.1016/j.socscimed.2008.06.033. [DOI] [PubMed] [Google Scholar]
- Clarke P.J., Weuve J., Barnes L., Evans D.A., Mendes de Leon C.F. Cognitive decline and the neighborhood environment. Annals of Epidemiology. 2015;25(11):849–854. doi: 10.1016/j.annepidem.2015.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S. Social relationships and health. American Psychologist. 2004;59(8):676–684. doi: 10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- Cohen M.J., Shaykevich S., Cawthon C., Kripalani S., Paasche-Orlow M.K., Schnipper J.L. Predictors of medication adherence postdischarge: The impact of patient age, insurance status, and prior adherence. Journal of Hospital Medicine. 2012;7(6):470–475. doi: 10.1002/jhm.1940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman J.S. American journal of sociology. The University of Chicago Press; 1988. Social capital in the creation of human capital. [DOI] [Google Scholar]
- Cramm J.M., van Dijk H.M., Nieboer A.P. The importance of neighborhood social cohesion and social capital for the well being of older adults in the community. The Gerontologist. 2013;53(1):142–152. doi: 10.1093/geront/gns052. [DOI] [PubMed] [Google Scholar]
- Cutler R.L., Fernandez-Llimos F., Frommer M., Benrimoj C., Garcia-Cardenas V. Economic impact of medication non-adherence by disease groups: A systematic review. BMJ Open. 2018;8(1) doi: 10.1136/bmjopen-2017-016982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De H.F., Mcclintock V., Morales K.H., Small D.S., Bogner H.R., Morales H.F. Patterns of adherence to oral hypoglycemic agents and glucose control among primary care patients with type 2 diabetes. Behavioral Medicine. 2016;42(2):63. doi: 10.1080/08964289.2014.904767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiMatteo M.R. Social support and patient Adherence to medical treatment: A meta-analysis. Health Psychology. 2004;23(2):207–218. doi: 10.1037/0278-6133.23.2.207. [DOI] [PubMed] [Google Scholar]
- Donkin A., Goldblatt P., Allen J., Nathanson V., Marmot M. Global action on the social determinants of health. BMJ Global Health. 2018;3(Suppl 1) doi: 10.1136/bmjgh-2017-000603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Eijken M., Tsang S., Wensing M., de Smet P.A.G.M., Grol R.P.T.M. Interventions to improve medication compliance in older patients living in the community. Drugs & Aging. 2003;20(3):229–240. doi: 10.2165/00002512-200320030-00006. [DOI] [PubMed] [Google Scholar]
- Fakoya O.A., McCorry N.K., Donnelly M. Loneliness and social isolation interventions for older adults: A scoping review of reviews. BMC Public Health. 2020;20(1):129. doi: 10.1186/s12889-020-8251-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher K.J., Li F., Michael Y., Cleveland M. Neighborhood-level influences on physical activity among older adults: A multilevel analysis. Journal of Aging and Physical Activity. 2004;12(1):45–63. doi: 10.1123/japa.12.1.45. [DOI] [PubMed] [Google Scholar]
- Fisher G.G., Ryan L.H. Overview of the health and retirement study and introduction to the special issue. Work, Aging and Retirement. 2018;4(1):1–9. doi: 10.1093/workar/wax032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson B.L. The role of positive emotions in positive psychology. The broaden-and-build theory of positive emotions. American Psychologist. 2001;56(3):218–226. doi: 10.1037//0003-066x.56.3.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gellad W.F., Haas J.S., Safran D.G. Race/ethnicity and nonadherence to prescription medications among seniors: Results of a national study. Journal of General Internal Medicine. 2007;22(11):1572–1578. doi: 10.1007/s11606-007-0385-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu D., Shen C. Assessing the importance of factors associated with cost-related nonadherence to medication for older US medicare beneficiaries. Drugs & Aging. 2019;36(12):1111–1121. doi: 10.1007/s40266-019-00715-3. [DOI] [PubMed] [Google Scholar]
- Ha J.-H., Kahng S.K., Choi N. Reciprocal effects between health and social support in older adults' relationships with their children and friends. Research on Aging. 2017;39(2):300–321. doi: 10.1177/0164027515611182. [DOI] [PubMed] [Google Scholar]
- Haynes R.B., Ackloo E., Sahota N., McDonald H.P., Yao X. Interventions for enhancing medication adherence. Cochrane Database of Systematic Reviews. 2008;(2) doi: 10.1002/14651858.CD000011.pub3. [DOI] [PubMed] [Google Scholar]
- Health, Retirement S. 2017. Sample sizes and response rates.https://hrs.isr.umich.edu/sites/default/files/biblio/ResponseRates_2017.pdf Retrieved from. [Google Scholar]
- Health, Retirement S. 2018. Institutional review board information.http://hrsonline.isr.umich.edu/ Retrieved from. [Google Scholar]
- Heeringa S.G., Connor J.H. 1995. Technical description of the health and retirement survey sample design technical description health and retirement study sample design.https://hrs.isr.umich.edu/sites/default/files/biblio/HRSSAMP.pdf Retrieved from. [Google Scholar]
- Hirsch J.A., Grengs J., Schulz A., Adar S.D., Rodriguez D.A., Brines S.J. How much are built environments changing, and where?: Patterns of change by neighborhood sociodemographic characteristics across seven U.S. metropolitan areas. Social Science & Medicine. 2016;169:97–105. doi: 10.1016/j.socscimed.2016.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jencks C., Mayer S.E. The social consequences of growing up in a poor neighborhood. In: Laurence J., Lynn E., McGeary M., editors. Inner-city poverty in the United States. National Academy Press; Washington, DC: 1990. pp. 111–186. [Google Scholar]
- Kang H., Lobo J.M., Kim S., Sohn M.-W. Cost-related medication non-adherence among U.S. adults with diabetes HHS Public Access. Diabetes Research and Clinical Practice. 2018;143:24–33. doi: 10.1016/j.diabres.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kavanagh A.M., Bentley R., Turrell G., Broom D.H., Subramanian S.V. Does gender modify associations between self rated health and the social and economic characteristics of local environments? Journal of Epidemiology & Community Health. 2006;60(6):490–495. doi: 10.1136/jech.2005.043562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I., Berkman L. Social capital, social cohesion, and health. In: Berkman L.F., Kawachi I., editors. Social epidemiology. Oxford University Press; New York: 2000. pp. 174–190. [Google Scholar]
- Kawachi I., Kennedy B.P., Lochner K., Prothrow-Stith D. Social capital, income inequality, and mortality. American Journal of Public Health. 1997;87(9):1491–1498. doi: 10.2105/ajph.87.9.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim E.S., Hawes A.M., Smith J. Perceived neighbourhood social cohesion and myocardial infarction. Journal of Epidemiology & Community Health. 2014;68(11):1020–1026. doi: 10.1136/jech-2014-204009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim E.S., Kawachi I. Perceived neighborhood social cohesion and preventive healthcare use. American Journal of Preventive Medicine. 2017;53(2):35–40. doi: 10.1016/j.amepre.2017.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim E.S., Park N., Peterson C. Perceived neighborhood social cohesion and stroke. Social Science & Medicine. 2013;97:49–55. doi: 10.1016/j.socscimed.2013.08.001. [DOI] [PubMed] [Google Scholar]
- Kim S., Spilman S.L., Liao D.H., Sacco P., Moore A.A. Social networks and alcohol use among older adults: A comparison with middle-aged adults. Aging & Mental Health. 2018;22(4):550–557. doi: 10.1080/13607863.2016.1268095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurlander J.E., Kerr E.A., Krein S., Heisler M., Piette J.D. 2009. Cost-related nonadherence to medications among patients with diabetes and chronic pain factors beyond finances. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S., Jiang L., Dowdy D., Hong Y.A., Ory M.G. Attitudes, beliefs, and cost-related medication nonadherence among adults aged 65 or older with chronic diseases. Preventing Chronic Disease. 2018;15:180190. doi: 10.5888/pcd15.180190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luz T.C.B., Loyola Filho A. I. de, Lima-Costa M.F. Perceptions of social capital and cost-related non-adherence to medication among the elderly. Cadernos de Saúde Pública. 2011;27(2):269–276. doi: 10.1590/S0102-311X2011000200008. [DOI] [PubMed] [Google Scholar]
- Lyyra T.-M., Heikkinen R.-L. Perceived social support and mortality in older people. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2006;61(3):S147–S152. doi: 10.1093/geronb/61.3.S147. [DOI] [PubMed] [Google Scholar]
- Mays V.M., Cochran S.D., Barnes N.W. Race, race-based discrimination, and health outcomes among African Americans. Annual Review of Psychology. 2007;58:201–225. doi: 10.1146/annurev.psych.57.102904.190212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McPherson M., Smith-Lovin L., Brashears M.E. Social isolation in America: Changes in core discussion networks over two decades. American Sociological Review. 2006;71(3):353–375. doi: 10.1177/000312240607100301. [DOI] [Google Scholar]
- Mendes De Leon C.F., Cagney K.A., Bienias J.L., Barnes L.L., Skarupski K.A., Scherr P.A. Neighborhood social cohesion and disorder in relation to walking in community-dwelling older adults A multilevel analysis. Journal of Aging and Health. 2009;21:155–171. doi: 10.1177/0898264308328650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michael Y.L., Green M.K., Farquhar S.A. Neighborhood design and active aging. Health & Place. 2006;12(4):734–740. doi: 10.1016/j.healthplace.2005.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirowsky J., Ross C.E. New York NY by aldine de Gruyter. Aldine de Gruyter; 2003. Social causes of psychological distress. Published in 2003.https://lib.ugent.be/catalog/rug01:000783165 Retrieved from. [Google Scholar]
- Moore S., Kawachi I. Twenty years of social capital and health research: A glossary. Journal of Epidemiology & Community Health. 2017;71(5):513–517. doi: 10.1136/jech-2016-208313. [DOI] [PubMed] [Google Scholar]
- Murayama H., Fujiwara Y., Kawachi I. 2012. Social capital and health: A review of prospective multilevel studies. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oksanen T., Kawachi I., Kouvonen A., Suzuki E., Takao S., Sjösten N. Workplace social capital and adherence to antihypertensive medication: A cohort study. PloS One. 2011;6(9) doi: 10.1371/journal.pone.0024732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson R.D., Krivo L.J. Segregated spatial locations, race-ethnic composition, and neighborhood violent crime. The Annals of the American Academy of Political and Social Science. 2009;623(1):93–107. doi: 10.1177/0002716208330490. [DOI] [Google Scholar]
- Pierre-Jacques M., Safran D.G., Zhang F., Ross-Degnan D., Adams A.S., Gurwitz J. Vol. 46. 2008. https://www.jstor.org/stable/pdf/40221681.pdf?refreqid=excelsior%3A81998e46d2bcfff0ad56842886d9701e (Reliability of new measures of cost-related medication nonadherence). Retrieved from. [DOI] [PubMed] [Google Scholar]
- Piette J.D., Heisler M., Horne R., Caleb Alexander G. A conceptually based approach to understanding chronically ill patients' responses to medication cost pressures. Social Science & Medicine. 2006;62(4):846–857. doi: 10.1016/J.SOCSCIMED.2005.06.045. [DOI] [PubMed] [Google Scholar]
- Piette J.D., Heisler M., Wagner T.H. Cost-related medication underuse among chronically ill adults: The treatments people forgo, how often, and who is at risk. American Journal of Public Health. 2004;94(10):1782–1787. doi: 10.2105/ajph.94.10.1782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Population Reference Bureau. (n.d.). Research on aging: How neighborhoods affect the health and well-being. Retrieved July 1, 2019, from https://www.prb.org/todays-research-aging-neighborhoods-health/.
- Portes A. Social capital: Its origins and applications in modern sociology. Annual Review of Sociology. 1998;24 Retrieved from www.annualreviews.org. [Google Scholar]
- Putnam R.D., Leonardi R., Nanetti R. Princeton University Press; 1993. Making democracy work : Civic traditions in modern Italy.https://press.princeton.edu/titles/5105.html Retrieved from. [Google Scholar]
- Robinette J.W., Charles S.T., Gruenewald T.L. Neighborhood cohesion, neighborhood disorder, and cardiometabolic risk. Social Science & Medicine. 2018;198:70–76. doi: 10.1016/j.socscimed.2017.12.025. 1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rouxel P., Tsakos G., Demakakos P., Zaninotto P., Chandola T., Watt R.G. Is social capital a determinant of oral health among older adults? Findings from the English longitudinal study of ageing. PloS One. 2015;10(5) doi: 10.1371/journal.pone.0125557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safran D.G., Neuman P., Schoen C., Kitchman M.S., Wilson I.B., Cooper B. Prescription drug coverage and seniors: Findings from A 2003 national survey. Health Affairs. 2005;24(Suppl1) doi: 10.1377/hlthaff.W5.152. W5-W152-W5-166. [DOI] [PubMed] [Google Scholar]
- Sampson R.J., Morenoff J.D., Gannon-Rowley T. Assessing “neighborhood effects”: Social processes and new directions in research. Annual Review of Sociology. 2002;28(1):443–478. doi: 10.1146/annurev.soc.28.110601.141114. [DOI] [Google Scholar]
- Sampson R.J., Raudenbush S.W., Earls F. Neighborhoods and violent crime: A multilevel study of collective efficacy. Science (New York, N.Y.) 1997;277(5328):918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- Schmitz M.F., Giunta N., Parikh N.S., Chen K.K., Fahs M.C., Gallo W.T. The association between neighbourhood social cohesion and hypertension management strategies in older adults. Age and Ageing. 2012;41(3):388–392. doi: 10.1093/ageing/afr163. [DOI] [PubMed] [Google Scholar]
- Schuster T.L., Kessler R.C., Aseltine R.H. Supportive interactions, negative interactions, and depressed mood. American Journal of Community Psychology. 1990;18(3):423–438. doi: 10.1007/BF00938116. [DOI] [PubMed] [Google Scholar]
- Skogan W.G. University of California Press; 1992. Disorder and decline : Crime and the spiral of decay in American neighborhoods.https://www.ucpress.edu/book/9780520076938/disorder-and-decline Retrieved from. [Google Scholar]
- Smalls B.L., Gregory C.M., Zoller J.S., Egede L.E. Effect of neighborhood factors on diabetes self-care behaviors in adults with type 2 diabetes. Diabetes Research and Clinical Practice. 2014;106(3):435–442. doi: 10.1016/j.diabres.2014.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smalls B.L., Gregory C.M., Zoller J.S., Egede L.E. Direct and indirect effects of neighborhood factors and self-care on glycemic control in adults with type 2 diabetes. Journal of Diabetes and its Complications. 2015;29(2):186–191. doi: 10.1016/J.JDIACOMP.2014.10.008. [DOI] [PubMed] [Google Scholar]
- Smith J., Ryan L., Fisher G.G., Sonnega A., Weir D. 2017. Psychosocial and lifestyle questionnaire 2006-2016 documentation report core section LB.https://hrs.isr.umich.edu/sites/default/files/biblio/HRS 2006-2016 SAQ Documentation_07.06.17_0.pdf Retrieved from. [Google Scholar]
- Solari C.D. Affluent neighborhood persistence and change in U.S. Cities. City & Community. 2012;11(4):370–388. doi: 10.1111/j.1540-6040.2012.01422.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soumerai S.B., Pierre-Jacques M., Zhang F., Ross-Degnan D., Adams A.S., Gurwitz J. Cost-related medication nonadherence among elderly and disabled medicare beneficiaries: A national survey 1 year before the medicare drug benefit. Archives of Internal Medicine. 2006;166(17):1829–1835. doi: 10.1001/archinte.166.17.1829. [DOI] [PubMed] [Google Scholar]
- Sun X., Yuan L. Analysis OF the effects OF social capital ON smoking behavior among older adults IN China. Innovation in Aging. 2019;3(Supplement_1):S900–S901. doi: 10.1093/geroni/igz038.3290. [DOI] [Google Scholar]
- Thoits P.A. Stress, coping, and social support processes: Where are we? What next? Journal of Health and Social Behavior, Spec No, 53–79. 1995 http://www.ncbi.nlm.nih.gov/pubmed/7560850 Retrieved from. [PubMed] [Google Scholar]
- Thoits P.A. Personal agency in the stress process. Journal of Health and Social Behavior. 2006;47(4):309–323. doi: 10.1177/002214650604700401. [DOI] [PubMed] [Google Scholar]
- Thoits P.A. Mechanisms linking social ties and support to physical and mental health. Journal of Health and Social Behavior. 2011;52(2):145–161. doi: 10.1177/0022146510395592. [DOI] [PubMed] [Google Scholar]
- Tseng C.-W., Tierney E.F., Gerzoff R.B., Dudley R.A., Waitzfelder B., Ackermann R.T. Race/Ethnicity and economic differences in cost-related medication underuse among insured adults with diabetes: The translating research into action for diabetes study. Diabetes Care. 2008;31(2):261–266. doi: 10.2337/dc07-1341. [DOI] [PubMed] [Google Scholar]
- Turner J., Frankel G., Levin D. Vol. 3. 1983. Social support: Conceptualization, measurement, and implications for mental health; pp. 67–111.https://psycnet.apa.org/record/1984-20538-001 (Research in community & mental health). Retrieved from. [Google Scholar]
- Uchino B.N. Social support and health: A review of physiological processes potentially underlying links to disease outcomes. Journal of Behavioral Medicine. 2006;29(4):377–387. doi: 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- Viswanathan M., Golin C.E., Jones C.D., Ashok M., Blalock S.J., Wines R.C.M. Interventions to improve adherence to self-administered medications for chronic diseases in the United States. Annals of Internal Medicine. 2012;157(11):785. doi: 10.7326/0003-4819-157-11-201212040-00538. [DOI] [PubMed] [Google Scholar]
- de Vries McClintock H.F., Wiebe D.J., OʼDonnell A.J., Morales K.H., Small D.S., Bogner H.R. Neighborhood social environment and patterns of adherence to oral hypoglycemic agents among patients with type 2 diabetes mellitus. Family & Community Health. 2015;38(2):169–179. doi: 10.1097/FCH.0000000000000069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vyncke V., Hardyns W., Peersman W., Pauwels L., Groenewegen P., Willems S. How equal is the relationship between individual social capital and psychological distress? A gendered analysis using cross-sectional data from ghent (Belgium) BMC Public Health. 2014;14(1):960. doi: 10.1186/1471-2458-14-960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walen H.R., Lachman M.E. Social support and strain from partner, family, and friends: Costs and benefits for men and women in adulthood. Journal of Social and Personal Relationships. 2000;17(1):5–30. doi: 10.1177/0265407500171001. [DOI] [Google Scholar]
- Warner L.M., Schüz B., Aiken L., Ziegelmann J.P., Wurm S., Tesch-Römer C. Interactive effects of social support and social conflict on medication adherence in multimorbid older adults. Social Science & Medicine. 2013;87:23–30. doi: 10.1016/J.SOCSCIMED.2013.03.012. [DOI] [PubMed] [Google Scholar]
- Warth J., Puth M.-T., Tillmann J., Beckmann N., Porz J., Zier U. Cost-related medication nonadherence among over-indebted individuals enrolled in statutory health insurance in Germany: A cross-sectional population study. BMC Health Services Research. 2019;19(1):887. doi: 10.1186/s12913-019-4710-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson I.B., Schoen C., Neuman P., Strollo M.K., Rogers W.H., Chang H. Physician-Patient communication about prescription medication nonadherence: A 50-state study of America's seniors. Medicine. 2007;22:6–12. doi: 10.1007/s11606-006-0093-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J.X., Meltzer D.O. Identifying patients with cost-related medication non-adherence: A big-data approach. Journal of Medical Economics. 2016;19(8):806–811. doi: 10.1080/13696998.2016.1176031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zivin K., Ratliff S., Heisler M.M., Langa K.M., Piette J.D. Factors influencing cost-related nonadherence to medication in older adults: A conceptually based approach. Value in Health. 2011;13(4):338–345. doi: 10.1111/j.1524-4733.2009.00679.x. [DOI] [PMC free article] [PubMed] [Google Scholar]