Abstract
Background
The novel coronavirus (2019-nCOV) appeared in China and precipitously extended across the globe. As always, natural disasters or infectious disease outbreaks have the potential to cause emergency department (ED) volume changes.
Objective
We aimed to assess the influence of the Coronavirus Disease 2019 (COVID-19) pandemic on ED visits and the impact on the handling of patients requiring urgent revascularization.
Methods
We reviewed the charts of all patients presenting to the ED of Hospital Sainte Anne (Toulon, France) from March 23 to April 5, 2020 and compared them with those of the same period in 2019. Then we analyzed complementary data on acute coronary syndrome (ST-elevation myocardial infarction [STEMI] and non-ST-elevation myocardial infarction [NSTEMI]) and neurovascular emergencies (strokes and transient ischemic attacks).
Results
The total number of visits decreased by 47%. The number of people assessed as triage level 2 was 8% lower in 2020. There were five fewer cases of NSTEMI in 2020, but the same number of STEMI. The number of neurovascular emergencies increased (27 cases in 2019 compared with 30 in 2020). We observed a reduction in the delay between arrival at the ED and the beginning of coronary angiography for STEMI cases (27 min in 2019 and 22 min in 2020). In 2020, 7 more stroke patients were admitted.
Conclusion
The COVID-19 pandemic probably dissuaded “non-critical” patients from coming to the hospital, whereas the same number of patients with a critical illness attended the ED as attended prior to the pandemic. There does not seem to have been any effect of the pandemic on patients requiring reperfusion therapy (STEMI and stroke).
Keywords: COVID-19, emergency department, STEMI, NSTEMI, stroke, TIA
Introduction
A novel coronavirus (severe acute respiratory syndrome coronavirus 2, SARS-CoV-2) causing respiratory infections—Coronavirus Disease 2019 (COVID-19)—was first detected in Wuhan, China in December 2019 (1, 2, 3). Within weeks, the virus had spread to all provinces of China, and to a growing number of countries (4,5). On March 12, 2020, the World Health Organization declared the epidemic of COVID-19 as a pandemic (6). At the time of writing (May 11, 2020), there are over 3,925,815 confirmed COVID-19 cases and nearly 274,488 deaths around the world (7). The first three confirmed COVID-19 cases were detected on January 24, 2020 (8). In May 2020, France is now facing the COVID-19 wave, with more than 139,063 cases and 25,561 deaths (9). On March 16, 2020, an almost full lockdown was imposed, unprecedented in peace time in France, to limit daily human contact outside of the home.
As always, natural disasters or infectious disease outbreaks have the potential to cause emergency department (ED) volume changes (10, 11, 12). The effects on health care utilization for an infectious disease epidemic depend on the characteristics of the infection (13, 14, 15, 16). Evaluating the impact of the COVID-19 pandemic on emergency care could provide important information for epidemiology, medical services, and public health. Therefore, this information could be useful for the development of an effective strategy in the case of a future SARS-like outbreak. Indeed, the health consequences of a SARS epidemic are not limited to those people who have been infected (17,18).
Due to the potential impact of SARS on people's access to medical services, we decided to investigate the changes in emergency care utilization at the Sainte Anne “Army teaching hospital” (ATH), in Toulon, during the COVID-19 pandemic (19, 20, 21). We also wanted to assess whether the handling of patients requiring urgent revascularization (ST-elevation myocardial infarction [STEMI]/stroke) had been modified (22, 23, 24, 25).
Methods
Study Setting
This study was carried out in the ED of the Sainte Anne ATH in Toulon, France. This military hospital is an integral part of the local emergency health network. Due to its technical platform, it is the hospital of reference in this area of France for neurovascular emergencies and serious traumas. In the case of cardiac emergencies, the hospital also has equipment for coronary angiography available 24 h a day.
During the year 2019, we received 34,167 patients in the ED. This year (2020), the hospital department was reorganized to cope with the COVID-19 pandemic, and is now divided into two parts—one section for admitting suspected COVID-19 patients (the “COVID [Red] zone”) with 17 beds, and a conventional section (the “non-COVID [Green] zone”) comprising eight beds.
Population
This monocentric observational study was carried out retrospectively using computerized records (ResUrgences software). We have compared patients admitted during the COVID-19 pandemic (from March 23 to April 5, 2020) with those patients admitted into the ED the previous year (March 23 to April 5, 2019). We examined all the records from March 23 to April 5, 2019 (1197 files) and all of those from March 23 to April 5, 2020 (634 files), a total of 1831 files. The 2-week period was chosen because, this year, it corresponds to the peak in the number of arrivals with suspected COVID-19 in the EDs in France (26).
We have detailed the following epidemiological characteristics: age, gender, number of arrivals (in the non-COVID zone and in the designated COVID zone), the number of hospital admissions, the clinical severity of the patients according to their ED triage score (Classification Clinique des Maladies aux Urgences [CCMU]), and the length of time spent in the ED.
We re-examined the computerized records in the ED software (ResUrgences) together with those from the Neurology and Cardiology departments (using AMADEUS, the IT management software for patients at the Sainte Anne ATH). This approach enabled us to gather the complementary data on acute coronary syndromes (ACS; STEMI and non-ST-elevation myocardial infarction [NSTEMI], sex, age, duration of symptoms prior to consultation, and the time between consultation and coronary angiography) and the neurovascular emergencies (number of strokes, number of transient ischemic attacks [TIAs], sex, age, duration of symptoms prior to consultation, and the time between consultation and cerebral imaging).
First, we detailed the management of patients with cardiovascular diseases (STEMI and NSTEMI) and with neurological diseases (stroke and TIA). Next, we looked more closely at cases of STEMI and strokes requiring urgent revascularization.
Statistical Analyses
Analysis of the quantitative data was performed, depending on the parameters of the sample, using either the Student's t test (homogeneity of variance and normality) or the Mann–Whitney test. The outcome of these tests is shown in our results by an index of confidence, “p”, with a significance threshold of 5%.
All the statistical analyses were carried out using the Python language in a special data science environment on the Anaconda distribution (Anaconda, Inc., Austin TX).
Ethics Statement
This study has the support of the Ethical Committee of our hospital (0011873-2020-06).
Results
Description and Comparison of Populations
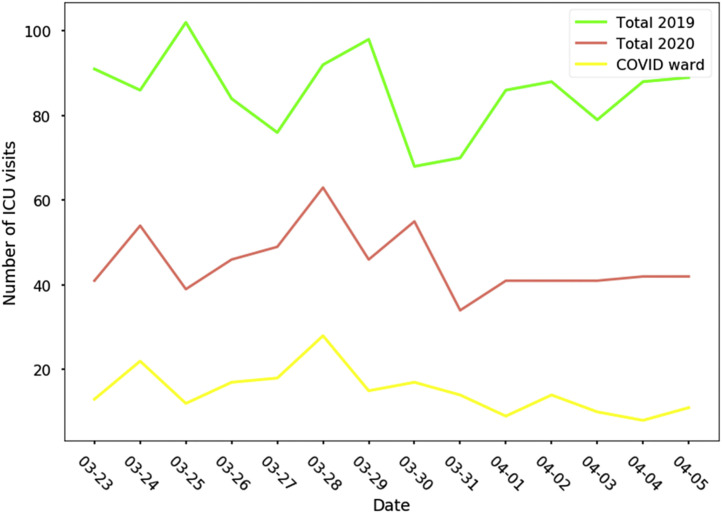
During our 2-week study period, the total number of patients decreased by 47%, from 1197 patients in 2019 to 634 in 2020. These results show an average of 85 admitted patients per day in 2019, but only 45 per day in 2020. The highest number of patients in 2020 was recorded on April 28, which corresponds to the peak in the “COVID zone” on the same day (Figure 1 ). The two cohorts are comparable as regards the intrinsic characteristics of the patients. On the other hand, the percentage of presenting patients requiring hospital admissions was significantly higher during the recent COVID-19 period, compared with 2019 (p < 0.001). The average length of time spent in the ED was lower in 2020 (5 h, 41 min) than in the previous year (7 h, 28 min), but this was not a significant difference (p = 0.086). The seriousness of the patient's condition was measured here using the ED triage score (CCMU). The proportion of patients assessed as being triage (CCMU) level 2 decreased by 8% in 2020 (p < 0.001); however, patients estimated to be at triage (CCMU) levels 3 or 4 increased by 4% (p = 0.014) and 3% (p = 0.005), respectively (Table 1 ).
Figure 1.
ICU admissions as a function of year and ICU admissions to the COVID ward. ICU = intensive care unit; COVID = Coronavirus Disease.
Table 1.
Details of Entries and Admissions in 2019 and 2020
| 2019 | 2020 | p-Value | |
|---|---|---|---|
| Population, total | 1197 | 634 | |
| Age | |||
| Mean | 54.9 | 56.7 | 0.092 |
| Min | 3 | 5 | |
| Max | 100 | 98 | |
| (0–20) | 87 (7%) | 17 (3%) | 0.295 |
| (20–40) | 293 (24%) | 147 (23%) | 0.851 |
| (40–60) | 289 (24%) | 181 (29%) | 0.096 |
| (60–80) | 338 (28%) | 190 (30%) | 0.528 |
| (80–100) | 190 (16%) | 99 (16%) | 0.776 |
| Gender, men | 617 (51.5%) | 348 (54.9%) | 0.184 |
| Admissions | |||
| Mean/d | 85 | 45 | 0.004 |
| Mean COVID ward/d | – | 15 | |
| Mean standard ward/d | 85 | 30 | 0.221 |
| Hospitalization | |||
| Total | 301 (25.1%) | 222 (35%) | < 0.001 |
| COVID ward | – | 102 | |
| Standard ward | 301 | 120 | 0.003 |
| Stay length, mean (hours:min) | 07:28 | 05:41 | 0.086 |
| CCMU∗ | |||
| 1 | 0 | 1 (<1%) | |
| 2 | 977 (82%) | 469 (74%) | < 0.001 |
| 3 | 189 (16%) | 129 (20%) | 0.014 |
| 4 | 28 (2%) | 30 (5%) | 0.005 |
| 5 | 3 (<1%) | 5 (1%) |
COVID = Coronavirus Disease; CCMU∗ = Classification Clinique des Maladies aux Urgences (emergency department triage score).
Description and Comparison of Different Diseases
Compared with 2019, the proportion of infectious diseases increased by 10% in 2020 (p < 0.01), whereas the proportion of trauma patients was 15% lower in 2020 (p < 0.01). The percentage of cardiac and neurological diseases was 4% and 3% lower, respectively, in 2020 (Table 2 ).
Table 2.
Classification of the Diagnoses in the ED by Medical Specialists
| 2019 | 2020 | p-Value | |
|---|---|---|---|
| Traumatology | 266 (22%) | 86 (7%) | < 0.01 |
| Cardiology | 147 (12%) | 90 (8%) | 0.246 |
| Gastroenterology | 114 (10%) | 50 (4%) | 0.243 |
| Neurology | 109 (9%) | 71 (6%) | 0.153 |
| ENT | 68 (6%) | 14 (1%) | 0.001 |
| Neurosurgery | 63 (5%) | 20 (2%) | 0.039 |
| Internal Medicine | 62 (5%) | 11 (1%) | < 0.01 |
| Dermatology | 55 (5%) | 11 (1%) | 0.002 |
| Nephrology | 53 (4%) | 27 (2%) | 0.866 |
| Rheumatology | 52 (4%) | 15 (1%) | 0.032 |
| Pulmonology | 45 (4%) | 30 (3%) | 0.318 |
| Ophthalmology | 44 (4%) | 8 (1%) | 0.003 |
| Surgery | 31 (3%) | 12 (1%) | 0.349 |
| Psychiatry | 31 (3%) | 21 (2%) | 0.376 |
| Infectiology | 31 (3%) | 152 (13%) | < 0.01 |
| Gynecology | 8 (1%) | 0 | 0.039 |
| Hyperbaric | 7 (1%) | 0 | 0.054 |
| Oncology | 6 (1%) | 2 (<1%) | 0.567 |
| Vascular | 5 (<1%) | 14 (1%) | < 0.01 |
ED = emergency department; ENT = ear, nose, and throat (Otolaryngology).
The number of hospital admissions in Cardiology and Neurology varies very little from one year to another, with around 27% hospitalizations in Cardiology. In 2020, the number of patient admissions in Neurology increased by 7% (Figure 2 ).
Figure 2.
Entries and hospitalizations for the Cardiology and Neurology specialties.
Cardiovascular Emergencies (ACS: STEMI and NSTEMI) and Neurological Emergencies (Stroke and TIA)
During the selected study period, there were five fewer cases of ACS in 2020, a reduction of 41.7% compared with 2019. In addition, in 2020 the patients experiencing an ACS were examined more quickly (4 h, 42 min) than in 2019 (10 h, 48 min) (Table 3 ).
Table 3.
Description of Patients Experiencing an ACS (STEMI or NSTEMI)
| 2019 | 2020 | p-Value | |
|---|---|---|---|
| Number of ACS | 12 | 7 | 0.331 |
| Men | 9 (75%) | 5 (71.4%) | 0.912 |
| Average age (years) | 72 | 67 | 0.478 |
| Duration of symptoms prior to ED arrival | 10 h 48 | 4 h 42 | 0.251 |
| NSTEMI | 9 (75%) | 4 (57.1%) | 0.463 |
| STEMI | |||
| Total | 3 (25%) | 3 (42.9%) | 0.463 |
| Time from ED arrival to coronarography (min) | 27 | 22 | 0.473 |
| Time (>2 h) from symptoms to ED arrival | 3 (100%) | 2 (66.7%) | 0.538 |
ACS = acute coronary syndrome; STEMI = ST-elevation myocardial infarction; NSTEMI = non-ST-elevation myocardial infarction; ED = emergency department.
In 2020, an increase was observed in the number of neurovascular emergencies (stroke and TIA), with 27 cases in 2019 as opposed to 30 in 2020. As for the patients with ACS, the average time interval between the first symptoms and the consultation was shorter in 2020. However, the average time lapse between the consultation and subsequent cerebral imaging increased in 2020 (3 h, 6 min) compared with 2019 (2 h, 36 min) (Table 4 ).
Table 4.
Description of Patients Experiencing a Stroke or a TIA
| 2019 | 2020 | p-Value | |
|---|---|---|---|
| Patients (stroke + TIA) | 27 | 30 | 0.811 |
| Average age (years) | 76 | 73 | 0.392 |
| Men | 15 (55.6%) | 21 (70%) | 0.267 |
| Duration of symptoms prior to consultation (mean) | 28 h 12 | 12 h 42 | 0.633 |
| Time between consultation and imagery (mean) | 2 h 36 | 3 h 06 | 0.093 |
| TIA | 9 (33.3%) | 5 (16.7%) | 0.15 |
| Stroke | 18 (66.7%) | 25 (83.3%) | 0.15 |
TIA = transient ischemic attack.
STEMI and Strokes Requiring Emergency Revascularization
An identical number of STEMI cases (n = 3) were seen in both years. Also, as regards STEMI patients, no significant difference was observed for the average delay between arrival at the ED and the beginning of the coronary angiography (27 min in 2019 and 22 min in 2020) (Table 3).
In 2020, 7 more stroke patients were admitted compared with 2019. Furthermore, the number of stroke patients dealt with after a delay of more than 5 h was reduced by 6% in 2020 (Table 4).
After statistical analysis, these results seem to be nonsignificant; however, this may be due to the relatively small patient numbers available during this period.
Discussion
Our study shows evidence of a 47% reduction in the number of ED consultations at the Sainte Anne ATH in 2020. As was seen in Taiwan during the SARS epidemic in 2003 and in South Korea with the Middle East respiratory syndrome epidemic of 2015, this COVID-19 pandemic has led to a drop in the number of arrivals at our ED (14,15). Two major hypotheses have been proposed to explain this phenomenon. The first is linked with the characteristics of the virus. Those hospitals that have been taking in patients suffering from the Coronavirus respiratory illness (which includes Sainte Anne ATH) are probable sites of contamination and, consequently, most people would be too anxious to go there. The other hypothesis is that this reduction in the number of patient entries is linked to the lockdown imposed on the general public.
The average age did not vary between the 2 years, and equally, there is no difference when comparing the age groups. In 2019, 44% of patients were aged 60 years or above, and this figure was 46% in 2020. Because age is known to be a risk factor in the severity of COVID-19 infections, we might have seen a reduction in the proportion of elderly people arriving at the ED, but this was not the case (27).
As regards the level of severity of patient cases, the number of people assessed as being at triage (CCMU) level 2 (not “critically” ill) was 8% lower in 2020. This reduction may be partly correlated with a smaller number of trauma cases. On the other hand, we observed an increase in patients presenting with triage (CCMU) level 3 and 4 symptoms. It is clear that the COVID-19 pandemic resulted in a reduction in consultations for noncritical conditions. However, as during the SARS epidemic in Taiwan in 2003, critically ill patients were examined at the ED despite the COVID-19 pandemic (12).
The relative percentages of different illnesses seen in the ED have changed during this pandemic phase. In 2020, infectious diseases accounted for 13% of the people who presented at the ED, compared with 3% in 2019, and the majority were patients suspected of having COVID-19. The effect of the arrivals in the separate “COVID zone” on the total number of patient entries in 2020 can be seen in Figure 1. The early creation of a specific “COVID zone” was essential for better management of the patients concerned and to limit contamination of patients in the “non-COVID zone.” The other important change that we observed was that trauma patients accounted for only 7% of entries in 2020, compared with 22% in 2019. This reduction can partly be explained by the lockdown measures that were in place (e.g., fewer activities with a risk of trauma, a reduction in traffic circulation). When we consider the percentages of cardiac and neurological illnesses, we see a reduction of 4% and 3%, respectively. This nonsignificant drop in numbers is surprising. COVID-19 is not simply a respiratory infection, and there may also be complications, either neurological (anosmia, encephalitis, stroke) or cardiac (myocardial injury, pulmonary embolism) (28,29). It is probable that certain patients did not go to the ED when necessary, which can lead to serious consequences in the short or medium term. In fact, the number of deaths at home increased by 29.6% in France from April 1 to April 20, 2020 (30).
The overall fall in the number of emergency consultations is accompanied by a 41.7% drop in ACS (STEMI and NSTEMI) over the same time period. However, this reduction concerned only the cases of NSTEMI. The clinical signs of NSTEMI are less clear and more intermittent, compared with STEMI, and so almost certainly went unnoticed. These symptoms were probably less worrying for the patients than a potential COVID-19 infection in the ED. During the COVID-19 pandemic in Hong Kong, the delay between the onset of symptoms and consultation in the ED seemed to increase, whereas we observed the opposite in our study (31). Despite the nonsignificant difference in our study, due to low experimental numbers, we have shown a reduction in the time lapse between the onset of symptoms and examination in the ED. During the pandemic, patients were advised to call the emergency number “15” if they experienced respiratory problems that could be concomitant with the thoracic pain of an ACS. This handling of cases by the “15” call center led, perhaps, to patients being examined more promptly in the ED.
Like these ACS patients, stroke or TIA victims were also examined more quickly in the ED in 2020. However, we observed, during our study period, the tendency for a longer delay between consultation and subsequent cerebral imagery. The radiology service also had to be reorganized during the COVID-19 pandemic, which possibly had an impact on the rapidity of diagnostic imaging.
With regards to those illnesses requiring urgent revascularization (STEMI and stroke), we have seen the same number of STEMI cases in both years. In addition, in 2020 we observed a slight reduction in the delay between arrival at the ED and the beginning of coronary angiography for STEMI cases. This could be explained by a fall in the workload at the ED, due to the drop in patient numbers. In the United States, for a large cohort study, there was a 39% drop in cerebral imaging for suspected strokes during the pandemic (32). Other research teams seem to highlight an increase in the incidence of strokes in patients infected with COVID-19, as observed in our study (33). There could be an interaction between the stroke's conventional risk factor, infection, systemic inflammatory response, and plaque destabilization (34). This rise in the number of strokes among our patients is perhaps linked to co-infections with COVID-19, a percentage of strokes with considerable clinical consequences (e.g., hemiplegia, aphasia), or some shortcomings in our study.
To conclude, the COVID-19 pandemic does not seem to have had an effect on patients needing emergency revascularization (STEMI and stroke) and, equally, we have observed an increase in the number of stroke patients. There is no evidence of any major impact of this pandemic on dealing with these patients.
Limitations
Due to the monocentric nature of our study, we cannot conclude that it is representative of all regions of France, because the impact of the COVID-19 pandemic has varied geographically. In addition, the study period selected is only 2 weeks, which does not cover the entire period of the pandemic. Finally, the number of arrivals at our ED during the study periods, and particularly the number of stroke and STEMI victims, is low and, consequently, our data are not robust enough to highlight any significant differences.
Conclusion
The COVID-19 pandemic led to a 47% fall in attendance at our ED. The lockdown and the fear of catching COVID-19 probably dissuaded the “non-critical” patients from coming to the hospital, whereas the same number of those with a critical illness attended the ED as prior to the pandemic period. There does not seem to have been any effect of the pandemic on patients requiring reperfusion therapy (STEMI and stroke). Furthermore, the COVID-19 pandemic had no impact on the delivery of health care to these emergency cases. The only impact concerned illnesses with less clear or self-limiting symptoms, such as TIA or NSTEMI.
Article Summary
1. Why is this topic important?
To date, there is a paucity of documentation outlining the impact of the Coronavirus Disease 2019 (COVID-19) pandemic on emergency department (ED) use.
2. What does this study attempt to show?
We aimed to assess the influence of the COVID-19 pandemic on ED visits and the impact on the handling of patients requiring urgent revascularization.
3. What are the key findings?
The COVID-19 pandemic led to a 47% fall in attendance at our ED and resulted in a reduction in consultations for noncritical conditions. The COVID-19 pandemic does not seem to have had an effect on patients needing emergency revascularization (ST-elevation myocardial infarction [STEMI] and stroke). The only impact concerned illnesses with less clear or self-limiting symptoms, such as transient ischemic attack or non-STEMI.
4. How is patient care impacted?
Evaluating the impact of the COVID-19 pandemic on emergency care could provide important information for epidemiology, medical services, and public health. Therefore, this information could be useful for the development of an effective strategy in the case of a future severe acute respiratory syndrome-like outbreak.
References
- 1.Zhu N., Zhang D., Wang W. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li Q., Guan X., Wu P. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu J.T., Leung K., Leung G.M. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020;395:689–697. doi: 10.1016/S0140-6736(20)30260-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization (WHO) COVID-19 situation reports. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports Available at:
- 5.European Centre for Disease Prevention and Control (ECDC) Situation update worldwide, as of 26 April 2020. https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases Available at:
- 6.World Health Organization (WHO) WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 Available at:
- 7.World Health Organization (WHO) WHO COVID-19 dashboard. https://covid19.who.int/ Available at:
- 8.Bernard Stoecklin S., Rolland P., Silue Y. First cases of Coronavirus Disease 2019 (COVID-19) in France: surveillance, investigations and control measures, January 2020. Euro Surveill. 2020;25:2000094. doi: 10.2807/1560-7917.ES.2020.25.6.2000094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chene G., Desenclos J.-C. Santé publique france; Saint-Maurice, France: 2020. COVID-19 Point épidémiologique hebdomadaire du 23 Avril 2020. [in French] [Google Scholar]
- 10.Miroballi Y., Baird J.S., Zackai S. Novel influenza A (H1N1) in a pediatric health care facility in New York City during the first wave of the 2009 pandemic. Arch Pediatr Adolesc Med. 2010;164:24–30. doi: 10.1001/archpediatrics.2009.259. [DOI] [PubMed] [Google Scholar]
- 11.Fagbuyi D.B., Brown K.M., Mathison D.J. A rapid medical screening process improves emergency department patient flow during surge associated with novel H1N1 influenza virus. Ann Emerg Med. 2011;57:52–59. doi: 10.1016/j.annemergmed.2010.08.026. [DOI] [PubMed] [Google Scholar]
- 12.Huang C.C., Yen D.H., Huang H.H. Impact of severe acute respiratory syndrome (SARS) outbreaks on the use of emergency department medical resources. J Chin Med Assoc. 2005;68:254–259. doi: 10.1016/S1726-4901(09)70146-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Choi J.Y. An outbreak of Middle East respiratory syndrome coronavirus infection in South Korea, 2015. Yonsei Med J. 2015;56:1174–1176. doi: 10.3349/ymj.2015.56.5.1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lu T.H., Chou Y.J., Liou C.S. Impact of SARS on healthcare utilization by disease categories: implications for delivery of healthcare services. Health Policy. 2007;83:375–381. doi: 10.1016/j.healthpol.2007.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chang H.-J., Huang N., Lee C.-H., Hsu Y.-J., Hsieh C.-J., Chou Y.-J. The impact of the SARS epidemic on the utilization of medical services: SARS and the fear of SARS. Am J Public Health. 2004;94:562–564. doi: 10.2105/ajph.94.4.562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cho S.Y., Kang J.M., Ha Y.E. MERS-CoV outbreak following a single patient exposure in an emergency room in South Korea: an epidemiological outbreak study. Lancet. 2016;388:994–1001. doi: 10.1016/S0140-6736(16)30623-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee S.Y., Khang Y.H., Lim H.K. Impact of the 2015 Middle East respiratory syndrome outbreak on emergency care utilization and mortality in South Korea. Yonsei Med J. 2019;60:796–803. doi: 10.3349/ymj.2019.60.8.796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Emanuel E.J. The lessons of SARS. Ann Intern Med. 2003;139:589–591. doi: 10.7326/0003-4819-139-7-200310070-00011. [DOI] [PubMed] [Google Scholar]
- 19.Yeoh S.C., Lee E., Lee B.W., Goh D.L. Severe acute respiratory syndrome: private hospital in Singapore took effective control measures. BMJ. 2003;326:1394. doi: 10.1136/bmj.326.7403.1394-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Haines C.J., Chu Y.W., Chung T.K. The effect of severe acute respiratory syndrome on a hospital obstetrics and gynaecology service. BJOG. 2003;110:643–645. doi: 10.1016/S1470-0328(03)03007-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Clark J. Fear of SARS thwarts medical education in Toronto. BMJ. 2003;326:784. doi: 10.1136/bmj.326.7393.784/c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995;333:1581–1587. doi: 10.1056/NEJM199512143332401. [DOI] [PubMed] [Google Scholar]
- 23.Generalized efficacy of t-PA for acute stroke. Subgroup analysis of the NINDS t-PA stroke trial. Stroke. 1997;28:2119–2125. doi: 10.1161/01.str.28.11.2119. [DOI] [PubMed] [Google Scholar]
- 24.Effect of intravenous recombinant tissue plasminogen activator on ischemic stroke lesion size measured by computed tomography. NINDS; The National Institute of Neurological Disorders and Stroke (NINDS) rt-PA Stroke Study Group. Stroke. 2000;31:2912–2919. doi: 10.1161/01.str.31.12.2912. [DOI] [PubMed] [Google Scholar]
- 25.Nallamothu B.K., Bradley E.H., Krumholz H.M. Time to treatment in primary percutaneous coronary intervention. N Engl J Med. 2007;357:1631–1638. doi: 10.1056/NEJMra065985. [DOI] [PubMed] [Google Scholar]
- 26.Santé publique France (SPF) Bulletin National d’Information OSCOUR du 12 Mai 2020. http://surveillance-syndromique-sursaud-R/documents/bulletin-national/2020/bulletin-national-d-information-oscour-du-12-mai-2020 Available at: [in French]
- 27.Zhou F., Yu T., Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Carod-Artal F.J. Neurological complications of coronavirus and COVID-19. Complicaciones Neurológicas por Coronavirus y COVID-19. Rev Neurol. 2020;70:311–322. doi: 10.33588/rn.7009.2020179. [in English, Spanish] [DOI] [PubMed] [Google Scholar]
- 29.Clerkin K.J., Fried J.A., Raikhelkar J. COVID-19 and cardiovascular disease. Circulation. 2020;141:1648–1655. doi: 10.1161/CIRCULATIONAHA.120.046941. [DOI] [PubMed] [Google Scholar]
- 30.Institut national de la statistique et des études économiques (Insee). Nombre de Décès Quotidiens par Département. https://www.insee.fr/fr/information/4470857#graphique-figure1_radio3 Available at: [in French]
- 31.Tam C.-C.F., Cheung K.-S., Lam S. Impact of Coronavirus Disease 2019 (COVID-19) outbreak on ST-segment-elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13:e006631. doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kansagra A.P., Goyal M.S., Hamilton S., Albers G.W. Collateral effect of Covid-19 on stroke evaluation in the United States [published online ahead of print, 2020 May 8] N Engl J Med. 2020;383:400–401. doi: 10.1056/NEJMc2014816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mao L., Jin H., Wang M. Neurologic manifestations of hospitalized patients with Coronavirus Disease 2019 in Wuhan, China. JAMA Neurol. 2020;77:683–690. doi: 10.1001/jamaneurol.2020.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bhatia R., Srivastava M.V.P. COVID-19 and stroke: incidental, triggered or causative. Ann Indian Acad Neurol. 2020;23:318–324. doi: 10.4103/aian.AIAN_380_20. [DOI] [PMC free article] [PubMed] [Google Scholar]