Abstract
Papillary muscle rupture is an infrequent and highly morbid mechanical complication of acute myocardial infarction. Surgical repair or replacement is traditionally considered first-line therapy. However, many of these patients present in extremis with prohibitively high surgical risk. Repair of mitral regurgitation with the MitraClip device (Abbot Vascular, Menlo Park, CA, USA) is an established therapy to treat degenerative and functional mitral regurgitation. We present a case of successful repair of severe mitral regurgitation due to papillary muscle rupture in the setting of acute myocardial infarction. A two-clip strategy resulted in mild residual mitral regurgitation with resolution of cardiogenic shock and refractory hypoxemia requiring veno-venous extracorporeal membrane oxygenation. Six-month follow-up echocardiogram identified durable results with mild mitral regurgitation and left ventricular ejection fraction of 63 %. Our case demonstrates that percutaneous mitral valve repair with MitraClip is a well-tolerated procedure that can provide acute and long-term benefit for patients with acute mitral regurgitation due to papillary muscle rupture who are at prohibitively high surgical risk.
<Learning Objective: Our case illustrates the role of MitraClip in acute mitral regurgitation due to papillary muscle rupture in cardiogenic shock as an alternative to surgical intervention in extremely high-risk patients.>
Keywords: Cardiogenic shock, Myocardial infarction, Mitral valve disease, Structural heart disease, Percutaneous, Intervention
Introduction
Mitral regurgitation (MR) due to papillary muscle rupture occurs in 1 to 3% of patients with acute myocardial infarction and carries a mortality of 80 % without surgical correction [1], [2]. Emergency surgical intervention is traditionally considered first-line therapy. However, in-hospital surgical mortality remains high at 40 % despite exclusion of over half of severe MR patients due to prohibitively high surgical risk. Percutaneous mitral valve repair with MitraClip (Abbot Vascular, Menlo Park, CA, USA) is an established therapy for treatment of degenerative MR and functional MR [3], [4]. Early reports have demonstrated that percutaneous mitral repair with the MitraClip device is safe in patients with cardiogenic shock and associated with decreased inotrope requirements after intervention [5], [6]. Here we present a case of successful repair of severe MR due to papillary muscle rupture in the setting of acute myocardial infarction.
Case report
A 51-year-old man presented to another hospital with a ST-segment elevation myocardial infarction (STEMI) complicated by cardiogenic shock and hypoxemic respiratory failure. He underwent emergent intubation and coronary intervention with drug-eluting stents placed in first obtuse marginal, atrioventricular groove circumflex, and posterolateral branch of the left circumflex artery. An intra-aortic balloon pump (IABP) was inserted for cardiogenic shock. On hospital day #4, the patient developed worsening hypoxemic respiratory failure. Repeat transthoracic echocardiography identified severe MR due to anterolateral papillary muscle rupture. On hospital day #6, he was transferred to our hospital for higher level of care. He arrived intubated on multiple inotropes and IABP. An Impella CP (Abiomed, Inc. Danvers, Massachusetts, U.S) was placed on arrival to improve his hemodynamics. The cardiothoracic surgery department was consulted and deemed the patient to be at prohibitive risk for mitral valve surgery (Society of Thoracic Surgeons (STS) Risk Score Mortality: 57 %, STS Morbidity or Mortality: 99 %). He was therefore referred for emergent percutaneous mitral valve repair using the MitraClip device on hospital day #7.
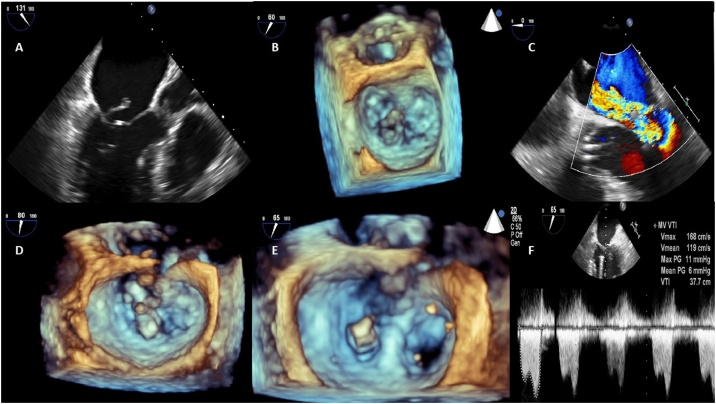
Upon arrival at the cardiac catheterization laboratory, the patient rapidly deteriorated due to worsening hypoxemic respiratory failure despite maximum ventilatory support. He was placed emergently onto veno-venous extracorporeal membrane oxygenation (VV ECMO) prior to mitral valve intervention. The first MitraClip XTR was implanted at the A2-P2 scallop. A MitraClip XTR clip was chosen to address the large flail gap and to minimize the procedural time in this critically ill patient. Due to significant remaining regurgitation, a second MitraClip XTR was placed on the lateral aspect of the A2-P2 leaflets with reduction in regurgitation from severe to mild and improvement in pulmonary vein systolic flow from systolic reversal to diastolic dominance (Fig. 1 and Movie 1, 2). Due to concern of paradoxical right to left shunt during VV ECMO support, an iatrogenic atrial septal defect was closed with a 20 mm Gore Cardioform Septal Occluder (Gore Medical, Flagstaff, Arizona, U.S) with no residual shunt. On hospital day #9 (Postoperative Day (POD) #2), the Impella CP was removed. On hospital day #10 (POD#3), he was decannulated from VV ECMO and extubated to nasal cannula the following day. He was discharged to an acute rehabilitation care facility on hospital day #23. At six-month follow-up, he remained in a stable condition in New York Heart Association class I. Six-month echocardiography revealed mild mitral valve regurgitation (Movie 3,4), a mean transmitral gradient of 5 mmHg and left ventricular ejection fraction of 63 %.
Fig. 1.
(A) Long-axis view identifying the ruptured anterolateral (AL) papillary muscle head. (B) 3-D reconstruction demonstrating ruptured AL papillary muscle and associated posterior leaflet (P2) flail. (C) Mid-esophageal view showing severe mitral regurgitation and Impella CP placed across the aortic valve. (D) Orienting the first MitraClip over the A2-P2 segment of the mitral valve. (E) Orienting the second MitraClip along the A2-P2 segment of the mitral valve, lateral to the previously placed first MitraClip. (F) Continuous wave Doppler through the mitral valve following MitraClip × 2 placement with a mean gradient of 6 mmHg.
Discussion
Acute MR due to papillary muscle rupture can occur in STEMI, non-STEMI, and less commonly due to chordal rupture. The majority of patients with papillary muscle rupture have a relatively small infarct with poor collateral flow [7]. Although small case series of emergency surgical intervention suggest an operative mortality rate of 20 to 25 %, a large observational study of a minimally selected cohort of patients with cardiogenic shock due to acute severe MR suggests surgical mortality is closer to 40 % [2], [7]. Earlier case reports have described successful treatment with MitraClip of acute severe MR due to papillary rupture [8], [9], [10]. Our case highlights that even a patient in extremis requiring both Impella CP and VV ECMO support can derive immediate and long-term benefit with percutaneous treatment. Importantly, increased operator and institutional experience with MitraClip are associated with improved procedural success and decreased complication rates with an inflection point seen at approximately 50 cases [11]. The Society of Thoracic Surgeons-American College of Cardiology Transcatheter Valve Therapies (STS-ACC TVT) Registry and multicenter collaboration is necessary to further develop best practices for this infrequent but highly morbid mechanical complication of acute myocardial infarction.
Conclusion
This case demonstrates that percutaneous mitral valve repair with MitraClip is a relatively safe and well tolerated intervention that can provide a significant and durable benefit for extremely high surgical risk patients with acute mitral regurgitation due to papillary muscle rupture.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.jccase.2020.07.001.
Appendix A. Supplementary data
The following are Supplementary data to this article:
References
- 1.Lavie C.J., Gersh B.J. Mechanical and electrical complications of acute myocardial infarction. Mayo Clin Proc. 1990;65:709–730. doi: 10.1016/s0025-6196(12)65133-7. [DOI] [PubMed] [Google Scholar]
- 2.Thompson C.R., Buller C.E., Sleeper L.A., Antonelli T.A., Webb J.G., Jaber W.A. Cardiogenic shock due to acute severe mitral regurgitation complicating acute myocardial infarction: a report from the SHOCK Trial Registry. SHould we use emergently revascularize Occluded Coronaries in cardiogenic shocK? J Am Coll Cardiol. 2000;36(3 Suppl. A):1104–1109. doi: 10.1016/s0735-1097(00)00846-9. [DOI] [PubMed] [Google Scholar]
- 3.Feldman T., Kar S., Rinaldi M., Fail P., Hermiller J., Smalling R. EVEREST Investigators. Percutaneous mitral repair with the MitraClip system: safety and midterm durability in the initial EVEREST (Endovascular Valve Edge-to-Edge REpair Study) cohort. J Am Coll Cardiol. 2009;54:686–694. doi: 10.1016/j.jacc.2009.03.077. [DOI] [PubMed] [Google Scholar]
- 4.Stone G.W., Lindenfeld J., Abraham W.T., Kar S., Lim D.S., Mishell J.M. Transcatheter mitral-valve repair in patients with heart failure. N Engl J Med. 2018;379:2307–2318. doi: 10.1056/NEJMoa1806640. [DOI] [PubMed] [Google Scholar]
- 5.Dawkins S., Cheng R., Makar M., Hamilton M., Makkar R., Kar S. 600.55 Percutaneous mitral valve repair for patients in severe cardiogenic shock is safe and is associated with improved renal function. JACC Cardiovasc Interv. 2019;12(4 Suppl):S57. doi: 10.1016/j.jcin.2019.05.042. [DOI] [PubMed] [Google Scholar]
- 6.Dawkins S., Cheng R., Tso J., Makar M., Hamilton M., Makkar R. 600.52 What is the impact of percutaneous mitral valve repair on inotrope use in cardiogenic shock? JACC Cardiovasc Interv. 2019;12(4 Suppl):S55–S56. doi: 10.1016/j.jcin.2019.05.042. [DOI] [PubMed] [Google Scholar]
- 7.Reeder G.S. Identification and treatment of complications of myocardial infarction. Mayo Clin Proc. 1995;70:880–884. doi: 10.1016/S0025-6196(11)63946-3. [DOI] [PubMed] [Google Scholar]
- 8.Bahlmann E., Frerker C., Kreidel F., Thielsen T., Ghanem A., van der Schalk H. MitraClip implantation after acute ischemic papillary muscle rupture in a patient with prolonged cardiogenic shock. Ann Thorac Surg. 2015;99:e41–e42. doi: 10.1016/j.athoracsur.2014.09.075. [DOI] [PubMed] [Google Scholar]
- 9.Valle J.A., Miyasaka R.L., Carroll J.D. Acute mitral regurgitation secondary to papillary muscle tear: is transcatheter edge-to-edge mitral valve repair a new paradigm? Circ Cardiovasc Interv. 2017;10 doi: 10.1161/CIRCINTERVENTIONS.117.005050. [DOI] [PubMed] [Google Scholar]
- 10.Wolff R., Cohen G., Peterson C., Wong S., Hockman E., Lo J. MitraClip for papillary muscle rupture in patient with cardiogenic shock. Can J Cardiol. 2014;30:1461.e13–1461.e14. doi: 10.1016/j.cjca.2014.07.015. [DOI] [PubMed] [Google Scholar]
- 11.Chhatriwalla A.K., Vemulapalli S., Holmes D.R., Dai D., Li Z., Ailawadi G. Institutional experience with transcatheter mitral valve repair and clinical outcomes: insights from the TVT Registry. JACC Cardiovasc Interv. 2019;12:1342–1352. doi: 10.1016/j.jcin.2019.02.039. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.