Abstract
Historically, one of the most common graft choices for anterior cruciate ligament (ACL) reconstruction in the pediatric population has been the hamstring autograft. Although pediatric ACL reconstructions with a hamstring autograft have allowed a majority of children and adolescents to return to athletics, it has been reported that anywhere between 6% and 38% of these patients will go on to experience subsequent graft rupture. The quadriceps tendon autograft is an alternative to the hamstring tendon autograft that demonstrates superior preliminary outcomes, and we currently recommend it for skeletally immature patients undergoing primary and revision ACL reconstruction. This paper aims to describe our technique for an open full-thickness quadriceps tendon harvest with repair.
Anterior cruciate ligament (ACL) tears in the pediatric and adolescent population are being recognized and treated with increasing frequency.1,2 Surgical techniques specific for this skeletally immature population have rapidly evolved to minimize the risk of growth disturbance and retear.3 However, incidence of graft failure is still high, with reported rates of retear ranging anywhere from 6% to 38%, largely dependent on the age and level of competition within the pediatric and young adolescent cohort as well as the type of graft used.4,5 When performing anterior cruciate ligament reconstruction (ACLR) in a growing adolescent athlete, the common graft options include hamstring tendon autograft versus quadriceps tendon autograft. The hamstring tendon autograft is more frequently used in the skeletally immature adolescent population, but recent investigations have focused on the quadriceps tendon as a potential superior alternative.6, 7, 8, 9, 10
Numerous quad tendon graft harvest approaches have been described. Techniques include using either an open or minimally invasive approach, taking partial- or full-thickness graft, with or without a bone plug from the patella, and with or without quadriceps defect repair.11,12 A 2018 systematic review found that partial-thickness quadriceps tendon autograft with a bone plug for single-bundle reconstruction was the most used form of the quadriceps autograft.13
Although the use of a quadriceps tendon autograft shows promising preliminary results, recently published data mainly involve ACLR using a quadriceps tendon autograft with a patellar bone block.14, 15, 16, 17, 18 In the skeletally immature patient, growth arrest following ACLR is more likely to occur when 3% to 5% of the physis is violated.19 For this reason, soft-tissue grafts are generally recommended over grafts that contain bone plug in patients with open physis.17,19, 20, 21, 22 Literature describing harvest techniques of a soft-tissue quadriceps tendon autograft is limited to minimally invasive approaches and partial-thickness harvests.12,23, 24, 25, 26 This paper describes a technique for an open approach to full-thickness soft-tissue quadriceps tendon harvest with subsequent defect repair for use in single-bundle ACLR.
Surgical Technique (With Video Illustration)
Patient Prep
The patient is placed in the supine position upon the operating room table. Following successful regional anesthesia, all bony prominences are well padded to avoid skin and neurovascular compromise. After performing an examination under anesthesia, the lower extremity is prepped and draped in the usual sterile fashion with the knee flexed to 90°.
Graft Harvest
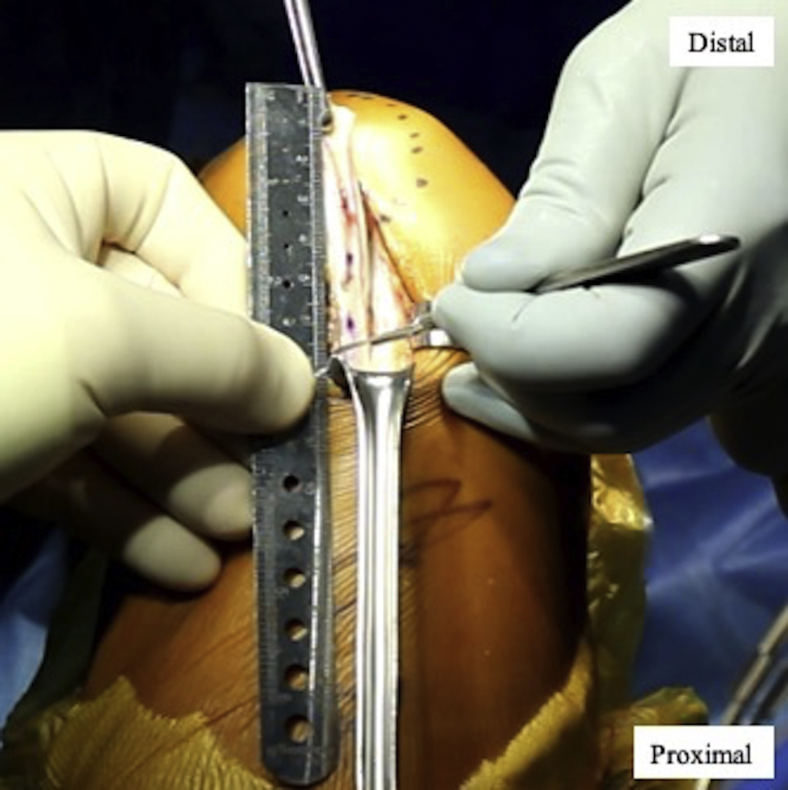
Following Esmarch exsanguination of the lower extremity, the tourniquet is inflated, and a 5-cm incision is made longitudinally overlying the quadriceps insertion beginning 1 cm proximal to the superior pole of the patella and extending proximally (Fig 1). The incision is taken through the subcutaneous tissue to the level of the extensor mechanism. Once the quadriceps tendon is visualized, a surgical marker should be used to mark the proximal and central aspect of the quadriceps tendon where there is often an apex as the quadriceps musculature converges. The mark is carried distally to the superior pole of the patella (Fig 2). We typically will use either a double-bladed 11-mm or 10-mm scalpel (Parallel Graft Knife; Arthrex, Naples, FL) depending upon the size of the patient. The double-bladed scalpel is used to incise the tendon beginning at the superior pole of the patella extending proximally, straddling the previously marked central portion of the quadriceps tendon (Fig 3). Using a #15 blade scalpel, the graft is released directly from its insertion on the superior pole of the patella, freed from attachments along its length (Fig 4), and then amputated proximally (Fig 5) for a final length of either 60 to 65 mm for all-epiphyseal ACLR or 70 to 75 mm for complete transphyseal ACLR (Fig 6). A full-thickness graft is obtained including the rectus femoris and rectus intermedius components of the quadriceps tendon, leaving the synovial capsular layer intact if it is substantive (Fig 7). As stated previously, we prefer a full-thickness, all soft-tissue graft (without a bone plug from the superior pole of the patella) in this population of children and young adolescents. Particular care is necessary to avoid injury to the rectus femoris muscle tendon junction at the proximal aspect of the harvest.
Fig 1.
Lateral view of the right knee. A 5-cm incision is shown over the quadriceps tendon extending to the superior pole of the patella.
Fig 2.
Right knee. Central portion of the quadriceps tendon marked with a surgical pen to the superior pole of the patella.
Fig 3.
Right knee. Double-bladed scalpel is used to incise the central portion of the quadriceps tendon straddling the previously placed markings.
Fig 4.
Right knee. The quadriceps tendon is freed from remaining surrounding tissue attachments with a #15 blade.
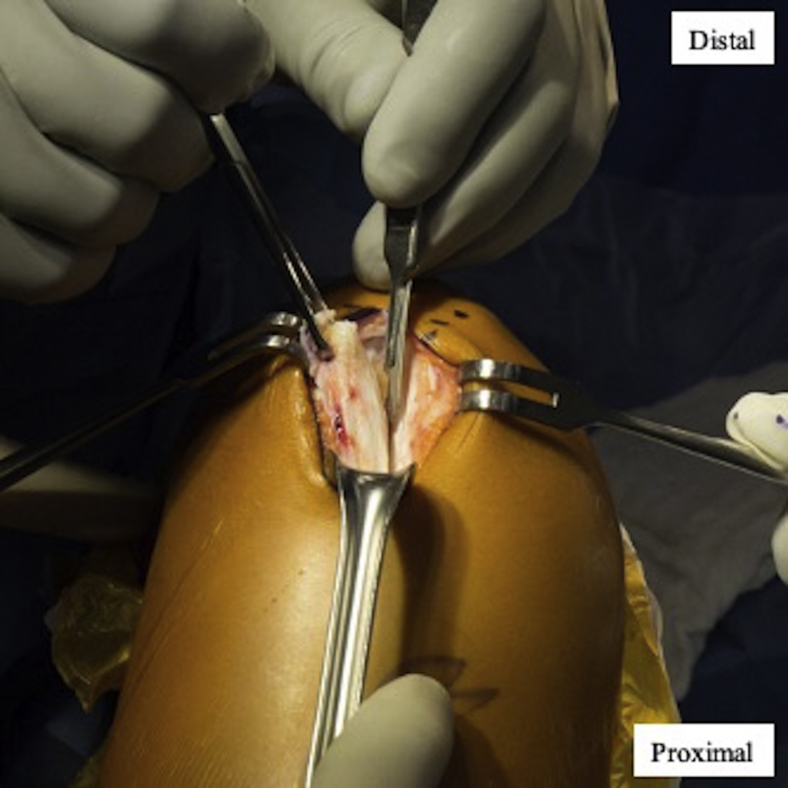
Fig 5.
Right knee. Once proper length is obtained, the proximal end of the graft is amputated with a #15 blade.
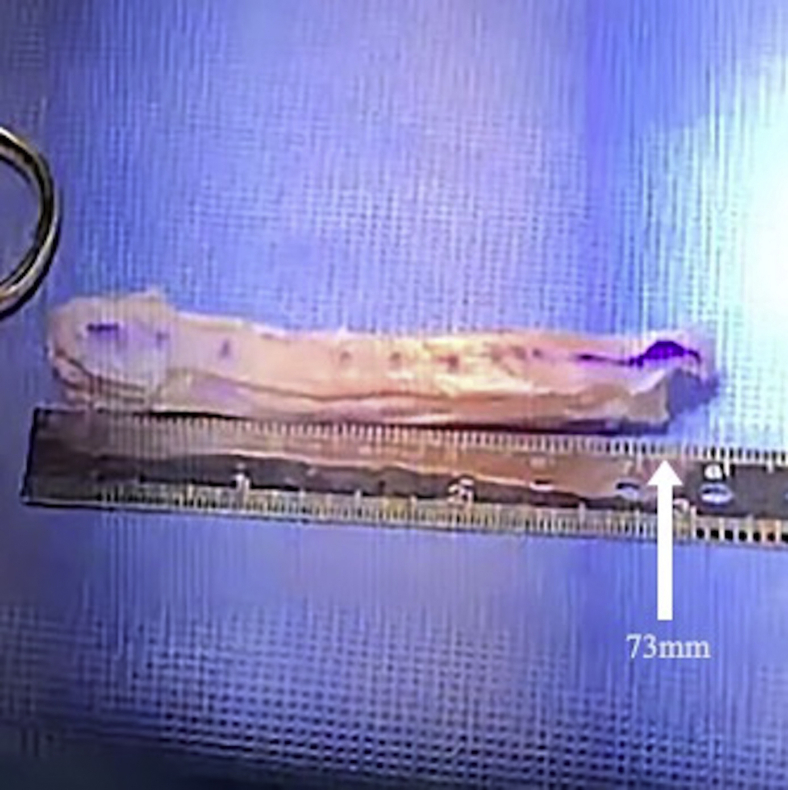
Fig 6.
Harvested 73-mm quadriceps tendon autograft for use in complete transphyseal anterior cruciate ligament reconstruction.
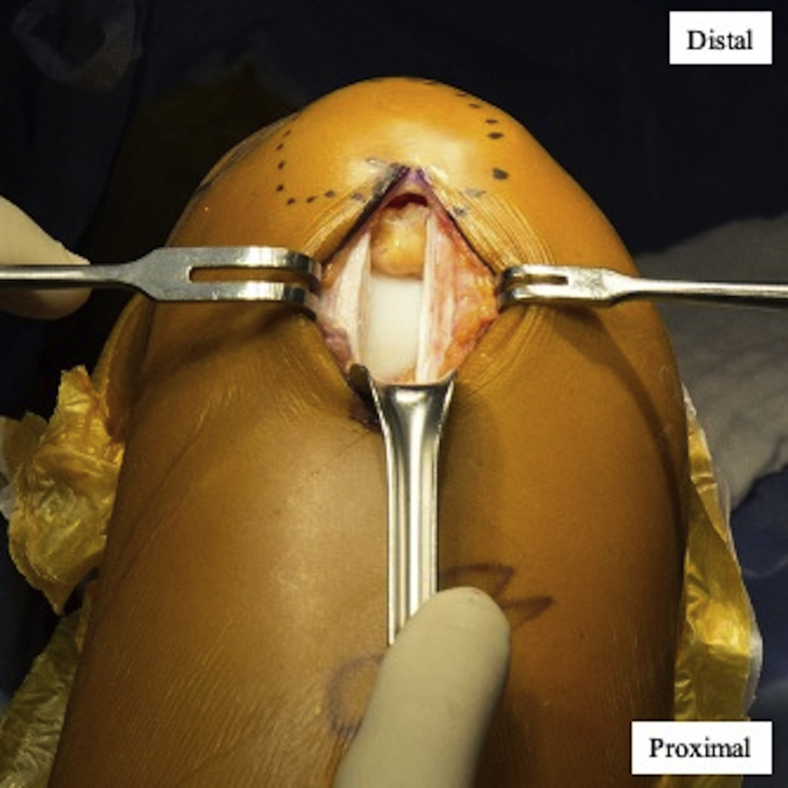
Fig 7.
Right knee. View of the quadriceps tendon defect after completion of full-thickness graft harvest.
Defect Repair
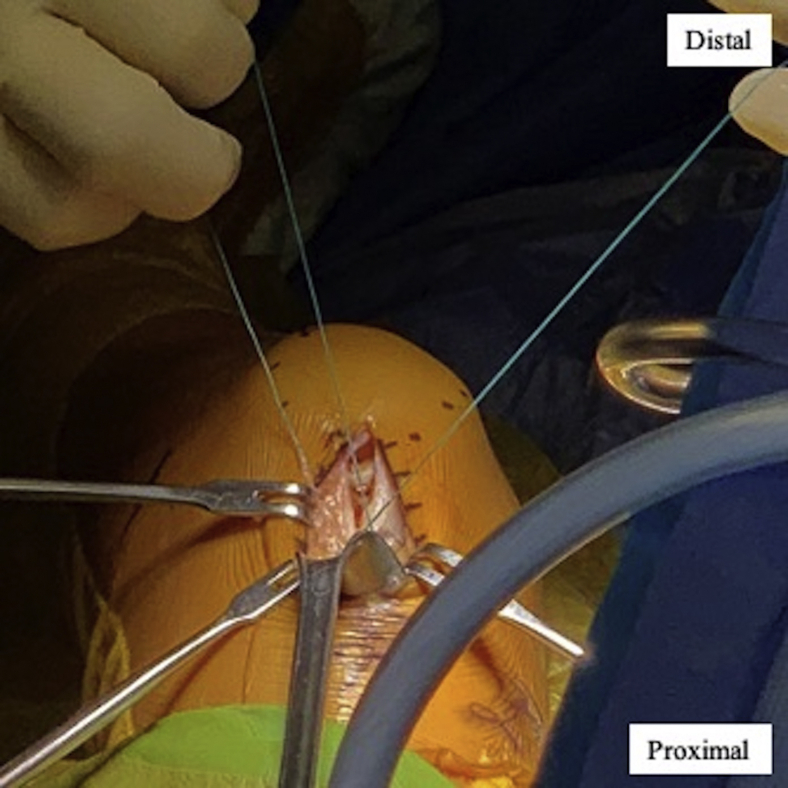
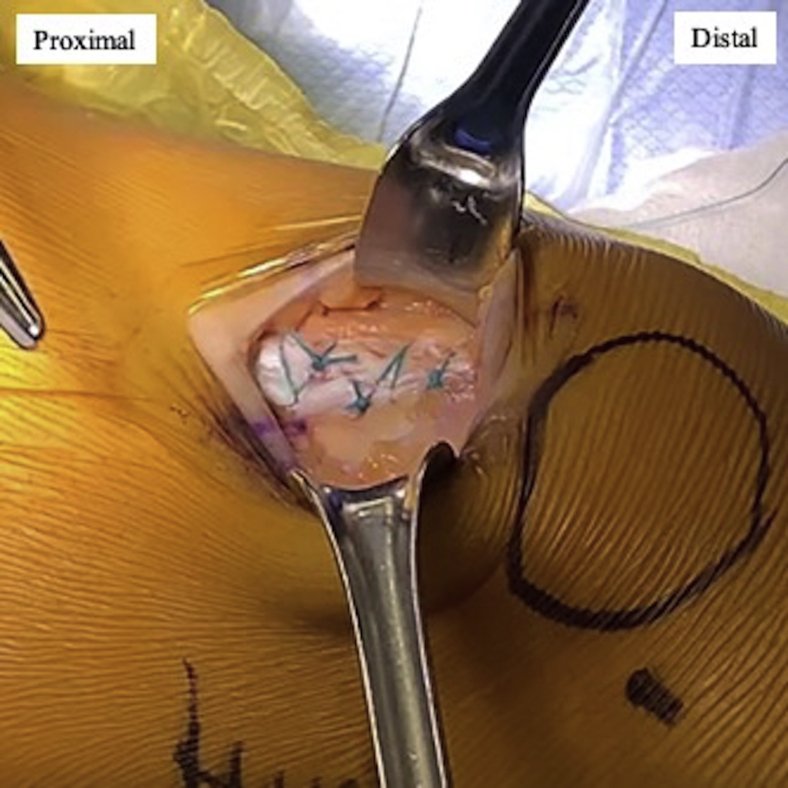
To begin, a #2 ETHIBOND suture (Ethicon, Somerville, NJ) is placed at the most proximal aspect of the defect and left long to provide traction and exposure by delivering the most proximal end of the defect for complete repair (Fig 8). Then, using #2 ETHIBOND sutures in an interrupted simple fashion, the remainder of the quadriceps defect is closed down to the superior pole of the patella. The repair included the synovial and capsular layers as well. The stitch used to close the distal most aspect of the quadriceps tendon defect may be placed in a buried fashion and in smaller patients, a #1 or #0 VICRYL may be used. The repair should be complete to limit extravasation of arthroscopy fluid for the remainder of the case (Fig 9). The tourniquet is released, and careful hemostasis is established.
Fig 8.
Right knee. Repair of the remaining quadriceps defect using #2 ETHIBOND sutures in an interrupted simple fashion.
Fig 9.
Lateral view of the right knee. Finished quadriceps tendon repair extending to the superior pole of the patella.
Graft Preparation
Once passed to the back table, the quadriceps tendon should be prepared by first trimming nontendon or mechanically incompetent tissue. Using a modified Krakow technique, a combination of locking and running nonabsorbable #2 sutures should be passed through the distal 20 mm of the graft on both ends. Then, BTB TightRopes (Arthrex) must be secured to the graft proximally and distally. We prefer using FiberLink and TigerLink sutures (Arthrex) in a modified Krakow technique to secure the BTB TightRope to the graft (Fig 10). Other techniques are available as well; however, this has been an efficient and secure construct in our experience. The graft should then be passed using an all-inside technique (sockets not tunnels) with BTB TightRopes on both the femoral and tibial sides as previously described by McCarthy et al.27
Fig 10.
Quadriceps tendon autograft prepared with a modified Krakow technique and BTB TightRopes on both the femoral and tibial ends.
Closure
At the conclusion of the procedure, the wound is copiously irrigated with antibiotic solution. The subcutaneous tissues of the quadriceps incision are closed with 2-0 VICRYL in an interrupted simple fashion and the skin is closed with a running 3-0 PROLENE or 3-0 MONOCRYL in a subcuticular fashion depending on patient factors and surgeon preferences. Steri strips and padding should be applied over the closed wound before wrap and brace application.
A video detailing the technique is shown in Video 1. Pearls and pitfalls and advantages and disadvantages of this technique for ACLR with a soft tissue quadriceps autograft are described in Tables 1 and 2, respectively.
Table 1.
Pearls and Pitfalls of ACL Reconstruction Using a Quadriceps Tendon Autograft
| Harvest a Full-thickness Graft including Both the Rectus Femoris and Rectus Intermedius. |
| Avoid compromise of the proximal muscle tendon junction during the harvest by limiting the proximal extent to avoid injury of the muscle and proximal migration. |
| We prefer using link sutures with a modified Krakow technique on the 2 sides of the graft to secure the BTB TightRope constructs proximally and distally. |
| Ensure the quadriceps tendon defect is fully repaired after autograft harvest to inhibit extravasation of arthroscopy fluid. |
ACL, anterior cruciate ligament.
Table 2.
Advantages and Disadvantages of a Using a Quadriceps Tendon Autograft for ACL Reconstruction
| Advantages | Disadvantages |
|---|---|
|
|
ACL, anterior cruciate ligament.
Discussion
The quadriceps tendon autograft is an excellent alternative to the hamstring tendon autograft, as cadaveric studies have reported comparable or superior load to failure strength.28,29 In addition, the quadriceps tendon is able to consistently provide a graft of robust size. In an anatomic study by Lippe et al.,30 the size of the native quadriceps tendon was found to be 88.3 ± 8.4 mm in length (range, 78.3-99.7 mm) and 43.3 ± 5.8 mm in width (range, 34.3-54.1 mm). The large size of the native tendon allows for a dependable harvest from the center third to yield a graft size of 10 to 11 mm in width and 70 to 75 mm in length. Contrary to hamstring tendon harvest, which requires harvesting the entire tendon and detaching the muscle, harvesting only the central portion of the quadriceps tendon does not disrupt the insertion of the quadriceps femoris muscles. In addition, the use of a quadriceps tendon autograft eliminates the risk of saphenous nerve injury associated with hamstring tendon harvest.31 However, care must be taken to avoid violation of the proximal muscle tendon junction as mentioned previously.
In preliminary studies, the quadriceps tendon autograft has shown superior outcomes over the hamstring tendon autograft.32, 33, 34 In a retrospective study with 81 patients who underwent ACLR with a quadriceps tendon–patellar bone block autograft, the incidence of graft failure was 1.2% at 3 years' follow-up.32 A meta-analysis compared outcomes after randomized controlled trials of graft choice for ACL reconstruction including bone–patellar tendon–bone, double-bundle and 4-strand hamstring tendon, and quadriceps tendon with bone block autografts. The authors found superior satisfaction based on subjective International Knee Documentation Committee scores in patients who underwent ACL reconstruction with a quadriceps tendon autograft.35 Another recent study comparing soft-tissue quadriceps tendon autograft and hamstring tendon autograft found a significantly lower retear rate 2.8 years after ACL reconstruction with a soft-tissue quadriceps tendon autograft (4% vs 21%, P = .03).33
In addition to superior patient-reported outcomes and decreased rates of graft retear, the quadriceps tendon autograft confers lower complication rates and donor-site morbidity than the hamstring tendon autograft.36,37 A study looking at 1638 revision ACLR cases found the quadriceps autograft group to have significantly lower incidence of postoperative septic arthritis of than the hamstring group (0.16% vs 1.29%, P = .013).38 A different study reported on donor-site morbidity by evaluating sensory loss and found the mean measured area of hypoesthesia was significantly lower in the quadriceps group compared with the hamstring group (70.3 ± 77.1 cm2 vs 8.7 ± 5.1 cm2; P < .0001).39 Although there are reports of patellar fracture and quadriceps tendon rupture after harvest of a quadriceps tendon with a bone block, no major complications after soft-tissue quadriceps tendon harvest have been reported.40,41
Our experience with this technique has shown promising results thus far. To date, a consecutive series of 101 patients younger than 20 years of age have undergone ACL reconstruction with a soft-tissue quadriceps tendon autograft. None of our patients have experienced ipsilateral graft tear or other significant complications. Fifty-one patients have undergone 1-year postoperative magnetic resonance imaging, all of which demonstrate an intact graft with proper healing (Fig 11).
Fig 11.
One-year postoperative sagittal magnetic resonance imaging of the right knee after all epiphyseal anterior cruciate ligament reconstruction with a quadriceps tendon autograft (white circle).
There are several technical aspects of harvesting and graft preparation regarding the use of the quadriceps autograft that must be mentioned. The first is the potential for injury at the muscle tendon junction during the proximal aspect of the quadriceps harvest. Although we have not noted any evidence of complications related to this potential in our patient population, surgeons should be cognizant of this risk. Second, the quadriceps autograft preparation is technically demanding and does require specific training. It is different from a hamstring autograft preparation as the hamstring loops provide for a more familiar adaptation to suspensory fixation. The quadriceps autograft is a solid piece of collagen (which we believe is a significant benefit of this graft choice) and as such requires an innovative technique, which we have described, to manage the secure fixation of the suspensory mechanism construct. Third, there is some variability of the proximal aspect of the quadriceps autograft where the rectus femoris and rectus intermedius begin to separate. An interval of adipose tissue between these tendon layers is noted on occasion and requires care in securing the suspensory fixation mechanism. Fourth, in smaller patients who are undergoing a complete transphyseal reconstruction, obtaining 70 mm of an all-soft tissue quadriceps autograft can be challenging. Some investigators have incorporated a portion of the superior pole of the patellar to address this. We have not found this to be necessary, as a 65-mm autograft length will suffice in these unusual circumstances. Fifth, theoretically there is the potential for quadriceps weakness in the early phases of rehabilitation. We have not found this to be of clinical significance, as these patients develop the ability to perform a straight leg raise on par with our patellar tendon autograft patients. Finally, this experience and series represents the patient population of the 2 senior authors and therefore may not be generalizable.
As growing literature supports the use of a quadriceps tendon autograft, this article describes a technique that can be used in younger patients undergoing ACLR that produces superior short-term outcomes. We currently recommend the use of a soft-tissue quadriceps tendon autograft in adolescents undergoing primary or revision ACLR.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: D.W.G. reports personal fees from Arthrex and Pega Medical, outside the submitted work. F.A.C. reports other from Arthrex, outside the submitted work. In addition, he has a patent (Arthrex) with royalties paid, a patent (Wolters Kluwer) with royalties paid, and a patent (Mosby/Saunders) with royalties paid and is on the JSES Board of Trustees and ASES Executive Board. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
With the patient in supine position and the right knee in 90° of flexion, a 5-cm incision is made longitudinally over the quadriceps tendon, 1 cm proximal to the superior pole of the patella, and taken down through subcutaneous tissues to the level of the extensor mechanism. After visualizing the quadriceps tendon, a surgical marker is used to identify the central, proximal part of the quadriceps tendon. A double-bladed scalpel is used to incise the tendon beginning at the superior pole of the patella, straddling the previously placed central markings. Using a #15 blade, the graft is released from its insertion on the superior pole of the patella. The full-thickness graft is then freed from any remaining attachments along its length. Before the proximal end of the graft is amputated, it should be measured to ensure adequate length. Once proper length is obtained, the proximal end of the graft should be amputated carefully to avoid injury to the rectus femoris muscle tendon junction. The remaining quadriceps tendon defect should be repaired using a #2 ETHIBOND suture in an interrupted simple fashion. The repair should include the synovial and capsular layers and extend to the superior pole of the patella. Successful repair of the defect allows for subsequent arthroscopy without extravasation of fluid.
.
References
- 1.Tepolt F.A., Feldman L., Kocher M.S. Trends in pediatric ACL reconstruction from the PHIS database. J Pediatr Orthop. 2018;38:e490–e494. doi: 10.1097/BPO.0000000000001222. [DOI] [PubMed] [Google Scholar]
- 2.Dodwell E.R., LaMont L.E., Green D.W., Pan T.J., Marx R.G., Lyman S. 20 Years of pediatric anterior cruciate ligament reconstruction in New York State. Am J Sports Med. 2014;42(3):675–680. doi: 10.1177/0363546513518412. [DOI] [PubMed] [Google Scholar]
- 3.Popkin C.A., Wright M.L., Pennock A.T. Trends in management and complications of anterior cruciate ligament injuries in pediatric patients. J Pediatr Orthop. 2018;38:e61–e65. doi: 10.1097/BPO.0000000000001098. [DOI] [PubMed] [Google Scholar]
- 4.Cordasco F.A., Black S.R., Price M. Return to sport and reoperation rates in patients under the age of 20 after primary anterior cruciate ligament reconstruction: Risk profile comparing 3 patient groups predicated upon skeletal age. Am J Sports Med. 2019;47:628–639. doi: 10.1177/0363546518819217. [DOI] [PubMed] [Google Scholar]
- 5.Larson C.M., Heikes C.S., Ellingson C.I. Allograft and autograft transphyseal anterior cruciate ligament reconstruction in skeletally immature patients: Outcomes and complications. Arthroscopy. 2016;32:860–867. doi: 10.1016/j.arthro.2015.10.014. [DOI] [PubMed] [Google Scholar]
- 6.Andrews M., Noyes F.R., Barber-Westin S.D. Anterior cruciate ligament allograft reconstruction in the skeletally immature athlete. Am J Sports Med. 1994;22:48–54. doi: 10.1177/036354659402200109. [DOI] [PubMed] [Google Scholar]
- 7.Longo U.G., Ciuffreda M., Casciaro C. Anterior cruciate ligament reconstruction in skeletally immature patients. Bone Joint J. 2017;99-B:1053–1060. doi: 10.1302/0301-620X.99B8.BJJ-2016-1150.R1. [DOI] [PubMed] [Google Scholar]
- 8.Shelton W.R., Fagan B.C. Autografts commonly used in anterior cruciate ligament reconstruction. Am Acad Orthop Surg. 2011;19:259–264. doi: 10.5435/00124635-201105000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Yucens M., Aydemir A.N. Trends in anterior cruciate ligament reconstruction in the last decade: A web-based analysis. J Knee Surg. 2019;32:519–524. doi: 10.1055/s-0038-1655764. [DOI] [PubMed] [Google Scholar]
- 10.Ho B., Edmonds E.W., Chambers H.G., Bastrom T.P., Pennock A.T. Risk factors for early ACL reconstruction failure in pediatric and adolescent patients: A review of 561 cases. J Pediatr Orthop. 2018;38:388–392. doi: 10.1097/BPO.0000000000000831. [DOI] [PubMed] [Google Scholar]
- 11.Diermeier T, Tisherman R, Hughes J, et al. Quadriceps tendon anterior cruciate ligament reconstruction [pubished online February 18, 2020]. Knee Surg Sport Traumatol Arthrosc https://doi.org/10.1007/s00167-020-05902-z. [DOI] [PubMed]
- 12.Slone H.S., Ashford W.B., Xerogeanes J.W. Minimally invasive quadriceps tendon harvest and graft preparation for all-inside anterior cruciate ligament reconstruction. Arthrosc Tech. 2016;5:e1049–e1056. doi: 10.1016/j.eats.2016.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kanakamedala A.C., de SA D., Obioha O.A. No difference between full thickness and partial thickness quadriceps tendon autografts in anterior cruciate ligament reconstruction: A systematic review. Knee Surg Sport Traumatol Arthrosc. 2019;27:105–116. doi: 10.1007/s00167-018-5042-z. [DOI] [PubMed] [Google Scholar]
- 14.Chen C.H., Chuang T.Y., Wang K.C., Chen W.J., Shih C.H. Arthroscopic anterior cruciate ligament reconstruction with quadriceps tendon autograft: Clinical outcome in 4-7 years. Knee Surg Sport Traumatol Arthrosc. 2006;14:1077–1085. doi: 10.1007/s00167-006-0111-0. [DOI] [PubMed] [Google Scholar]
- 15.Howe J.G., Johnson R.J., Kaplan M.J., Fleming B., Jarvinen M. Anterior cruciate ligament reconstruction using quadriceps patellar tendon graft. Part I. Long-term followup. Am J Sports Med. 1991;19:447–457. doi: 10.1177/036354659101900505. [DOI] [PubMed] [Google Scholar]
- 16.Albright J., Lepon A.K., Mayer S. Anterior cruciate ligament reconstruction in pediatric and adolescent patients using quadriceps tendon autograft. Sports Med Arthrosc. 2016;24:159–169. doi: 10.1097/JSA.0000000000000128. [DOI] [PubMed] [Google Scholar]
- 17.Mauch C., Arnold M.P., Wirries A., Mayer R.R., Friederich N.F., Hirschmann M.T. Anterior cruciate ligament reconstruction using quadriceps tendon autograft for adolescents with open physes—a technical note. Sport Med Arthrosc Rehabil Ther Technol. 2011;3:7. doi: 10.1186/1758-2555-3-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Todor A., Caterev S., Nistor D.V., Khallouki Y. Free bone plug quadriceps tendon harvest and suspensory button attachment for anterior cruciate ligament reconstruction. Arthrosc Tech. 2016;5:e541–e544. doi: 10.1016/j.eats.2016.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Houle J.B., Letts M., Yang J. Effects of a tensioned tendon graft in a bone tunnel across the rabbit physis. Clin Orthop Relat Res. 2001;391:275–281. doi: 10.1097/00003086-200110000-00032. [DOI] [PubMed] [Google Scholar]
- 20.Nottage W.M., Matsuura P.A. Management of complete traumatic anterior cruciate ligament tears in the skeletally immature patient: Current concepts and review of the literature. Arthroscopy. 1994;10:569–573. doi: 10.1016/s0749-8063(05)80016-7. [DOI] [PubMed] [Google Scholar]
- 21.Seil R., Pape D., Kohn D. The risk of growth changes during transphyseal drilling in sheep with open physes. Arthroscopy. 2008;24:824–833. doi: 10.1016/j.arthro.2008.02.007. [DOI] [PubMed] [Google Scholar]
- 22.Meller R., Kendoff D., Hankemeier S. Hindlimb growth after a transphyseal reconstruction of the anterior cruciate ligament: A study in skeletally immature sheep with wide-open physes. Am J Sports Med. 2008;36:2437–2443. doi: 10.1177/0363546508322884. [DOI] [PubMed] [Google Scholar]
- 23.Sprowls G.R., Robin B.N. The quad link technique for an all-soft-tissue quadriceps graft in minimally invasive, all-inside anterior cruciate ligament reconstruction. Arthrosc Tech. 2018;7:e845–e852. doi: 10.1016/j.eats.2018.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Andrish J. Recurrent patellar dislocation. In: Fulkerson J.P., editor. AAOS Monograph: Common Patellofemoral Problems. American Academy of Orthopaedic Surgeons; Rosemont, IL: 2005. pp. 43–55. [Google Scholar]
- 25.DeAngelis J.P., Fulkerson J.P. Quadriceps tendon—a reliable alternative for reconstruction of the anterior cruciate ligament. Clin Sports Med. 2007;26:587–596. doi: 10.1016/j.csm.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 26.Fulkerson J.P., Langeland R. An alternative cruciate reconstruction graft: The central quadriceps tendon. Arthroscopy. 1995;11:252–254. doi: 10.1016/0749-8063(95)90078-0. [DOI] [PubMed] [Google Scholar]
- 27.McCarthy M.M., Graziano J., Green D.W., Cordasco F.A. All-epiphyseal, all-inside anterior cruciate ligament reconstruction technique for skeletally immature patients. Arthrosc Tech. 2012;1:e231–e239. doi: 10.1016/j.eats.2012.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sasaki N., Farraro K.F., Kim K.E., Woo S.L.Y. Biomechanical evaluation of the quadriceps tendon autograft for anterior cruciate ligament reconstruction: A cadaveric study. Am J Sports Med. 2014;42:723–730. doi: 10.1177/0363546513516603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Harris N.L., Smith D.A.B., Lamoreaux L., Purnell M. Central quadriceps tendon for anterior cruciate ligament reconstruction. Part I: Morphometric and biomechanical evaluation. Am J Sports Med. 1997;25:23–28. doi: 10.1177/036354659702500105. [DOI] [PubMed] [Google Scholar]
- 30.Lippe J., Armstrong A., Fulkerson J.P. Anatomic guidelines for harvesting a quadriceps free tendon autograft for anterior cruciate ligament reconstruction. Arthroscopy. 2012;28:980–984. doi: 10.1016/j.arthro.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 31.Wittstein J.R., Wilson J.B., Moorman C.T. Complications related to hamstring tendon harvest. Oper Tech Sports Med. 2006;14:15–19. [Google Scholar]
- 32.Gagliardi A.G., Carry P.M., Parikh H.B., Albright J.C. Outcomes of quadriceps tendon with patellar bone block anterior cruciate ligament reconstruction in adolescent patients with a minimum 2-year follow-up. Am J Sports Med. 2020;48:93–98. doi: 10.1177/0363546519885371. [DOI] [PubMed] [Google Scholar]
- 33.Pennock A.T., Johnson K.P., Turk R.D. Transphyseal anterior cruciate ligament reconstruction in the skeletally immature: Quadriceps tendon autograft versus hamstring tendon autograft. Orthop J Sport Med. 2019;7(9) doi: 10.1177/2325967119872450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hurley E.T., Calvo-Gurry M., Withers D., Farrington S.K., Moran R., Moran C.J. Quadriceps tendon autograft in anterior cruciate ligament reconstruction: A systematic review. Arthroscopy. 2018;34:1690–1698. doi: 10.1016/j.arthro.2018.01.046. [DOI] [PubMed] [Google Scholar]
- 35.Yang X gang, Wang F., He X. Network meta-analysis of knee outcomes following anterior cruciate ligament reconstruction with various types of tendon grafts. Int Orthop. 2019;44:365–380. doi: 10.1007/s00264-019-04417-8. [DOI] [PubMed] [Google Scholar]
- 36.Lind M., Nielsen T.G., Soerensen O.G., Mygind-Klavsen B., Faunø P. Quadriceps tendon grafts does not cause patients to have inferior subjective outcome after anterior cruciate ligament (ACL) reconstruction than do hamstring grafts: A 2-year prospective randomised controlled trial. Br J Sports Med. 2020;54:183–187. doi: 10.1136/bjsports-2019-101000. [DOI] [PubMed] [Google Scholar]
- 37.Ajrawat P, Dwyer T, Whelan D, et al. A comparison of quadriceps tendon autograft with bone-patellar tendon-bone autograft and hamstring tendon autograft for primary anterior cruciate ligament reconstruction: A systematic review and quantitative synthesis [published online June 19, 2019]. Clin J sport med. https://doi.org/10.1097/JSM.0000000000000765. [DOI] [PubMed]
- 38.Schuster P, Schlumberger M, Mayer P, et al. Lower incidence of post-operative septic arthritis following revision anterior cruciate ligament reconstruction with quadriceps tendon compared to hamstring tendons [published online February 4, 2020]. Knee Surg Sport Traumatol Arthrosc https://doi.org/10.1007/s00167-020-05878-w. [DOI] [PubMed]
- 39.Mouarbes D, Dagneaux L, Olivier M, et al. Lower donor-site morbidity using QT autografts for ACL reconstruction [published online February 4, 2020]. Knee Surg Sport Traumatol Arthrosc https://doi.org/10.1007/s00167-020-05873-1. [DOI] [PubMed]
- 40.Fu F.H., Rabuck S.J., West R.V., Tashman S., Irrgang J.J. Patellar fractures after the harvest of a quadriceps tendon autograft with a bone block: A case series. Orthop J Sport Med. 2019;7(3) doi: 10.1177/2325967119829051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pandey V., Madi S., Joseph A., Acharya K. Late quadriceps tendon rupture at the donor site following cruciate ligament reconstruction using central quadriceps tendon graft. BMJ Case Rep. 2015;2015 doi: 10.1136/bcr-2015-212621. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
With the patient in supine position and the right knee in 90° of flexion, a 5-cm incision is made longitudinally over the quadriceps tendon, 1 cm proximal to the superior pole of the patella, and taken down through subcutaneous tissues to the level of the extensor mechanism. After visualizing the quadriceps tendon, a surgical marker is used to identify the central, proximal part of the quadriceps tendon. A double-bladed scalpel is used to incise the tendon beginning at the superior pole of the patella, straddling the previously placed central markings. Using a #15 blade, the graft is released from its insertion on the superior pole of the patella. The full-thickness graft is then freed from any remaining attachments along its length. Before the proximal end of the graft is amputated, it should be measured to ensure adequate length. Once proper length is obtained, the proximal end of the graft should be amputated carefully to avoid injury to the rectus femoris muscle tendon junction. The remaining quadriceps tendon defect should be repaired using a #2 ETHIBOND suture in an interrupted simple fashion. The repair should include the synovial and capsular layers and extend to the superior pole of the patella. Successful repair of the defect allows for subsequent arthroscopy without extravasation of fluid.