Abstract
Arthroscopic shoulder stabilization offers a safe and effective means for restoring glenohumeral mechanics in the setting of shoulder instability. Modern arthroscopic techniques have allowed improved access and efficiency when treating patients with shoulder instability. However, access to certain areas of the labrum and the creation of safe accessory portals can still prove difficult for the arthroscopic surgeon. Currently, there is debate as to the ideal patient position, portal location, equipment, and technique for addressing anterior–inferior labral pathology. The following article presents a safe and effective approach to accessing the labrum for treatment of shoulder instability in the lateral decubitus position. In addition, this paper highlights the use of accessory portals, including a percutaneous “7-o’clock” portal for suture anchor placement, along with multiple types of suture anchor and suture shuttling techniques.
Introduction (With Video Illustration)
Chronic glenohumeral instability and shoulder dislocation are common injuries that affect 1% to 2% of the general population.1, 2, 3, 4 In addition, there is a very high rate of shoulder dislocation in the youth athletic population.5 Risks of treating shoulder instability nonoperatively include recurrent instability episodes that may result in further damage to the labrum as well as bone and cartilage loss.6 Thus, some patients afflicted with shoulder dislocation and instability injuries stand to benefit from surgical stabilization through open or arthroscopic procedures.7,8
Arthroscopic shoulder-stabilization procedures have increased in popularity over the past 20 years as arthroscopic repair techniques have improved. Data from 2009 indicate that arthroscopic stabilization is performed in approximately 90% of shoulder-stabilization surgeries.9,10 Benefits of arthroscopic stabilization include limited disruption to the subscapularis, increased ability to address concomitant intra-articular shoulder pathology, improved postprocedural external rotation, minimized postoperative pain, and decreased morbidity.11, 12, 13, 14, 15, 16, 17, 18
When considering arthroscopic stabilization, there are 2 main patient positioning options: “beach chair” and lateral decubitus. It is our preference to address shoulder instability in the lateral decubitus position when treating it arthroscopically. This positioning allows for circumferential access to the glenoid labrum, thus allowing easy and safe instrumentation to the inferior and posteroinferior labrum, as chronic instability often affects these regions. Moreover, the traction applied to the joint allows for ample space to safely insert suture anchors, cannulas, and shuttling devices. Recent research has supported use of lateral decubitus over beach chair for these reasons.19
Additional principles of arthroscopic shoulder stabilization include maintaining oblique angles for suture anchor insertion, using at least 3 points of fixation, and minimizing the interference of sutures and suture knots on the chondral surfaces of the humeral head.19 This technique paper discusses our technique for safe and effective arthroscopic shoulder stabilization. A detailed description of our technique can be viewed in Video 1.
Surgical Technique
Preoperative Evaluation, Imaging, and Surgical Indications
Patients presenting with a history of shoulder instability require initial workup, including a comprehensive history and physical examination. Details surrounding dislocation events such as mechanism, number of dislocations, and ease of dislocation are important in determining proper treatment. Physical examination should be performed on both the injured and healthy shoulder and should include the apprehension test, sulcus test, anterior release test, and the relocation test. Conventional radiography, computed tomography, and magnetic resonance imaging arthrography can be used to help evaluate the shoulder. Indications for surgical intervention include patients with a high risk of recurrent instability (such as young athletes) or those who have not responded to nonoperative management.
Anesthesia and Patient Positioning
Surgical consent is obtained from all patients per standard protocol at our hospital. A preoperative, ultrasound-guided supraclavicular brachial plexus block is administered by the anesthesiologist. The patient is then transported to the operating room, and general anesthesia is administered along with preoperative antibiotics. The patient is then positioned into the lateral decubitus position with the use of a bean bag (Fig 1). Care is taken to position the superior extent of the bean bag at the level of the nipples and to keep the bean bag leaflets below the level of the patient. These considerations minimize impingement of the bean bag on the arthroscopic camera or instruments during the procedure.
Fig 1.
The patient is positioned into the lateral decubitus position using a bean bag. We also use a Lateral Jack device to provide upwards force on the humeral head, which is positioned just opposite and distal to the axilla of the patient. Positioning of the portals (high lateral posterior, 7-o’clock and traditional posterior) also can be visualized.
Two different arm positioners are used in our technique. A pneumatic arm holder (Spider; Smith & Nephew, Wixom, MA) is positioned on the contralateral bed rail, approximately one foot proximal to the end of the rail. We also use an additional device to provide upwards force on the humeral head. This device (Lateral Jack; Smith & Nephew) is positioned just opposite and distal to the axilla of the patient (Table 1, Fig 1). An axillary roll is also used. Following an examination of the patient while he or she is under anesthesia, the operative side is prepped, draped, and positioned into the respective arm holders before skin marking. Our prep consists of a prewash using chlorhexidine/peroxide, followed by chlorhexidine paint brushes.
Table 1.
Pearls and Pitfalls of Arthroscopic Shoulder Stabilization
| Pearls | Pitfalls |
|---|---|
| Addition of Lateral Jack device creates additional glenohumeral joint distraction | Multiple positioning devices can add to OR time and is highly depending on OR staff experience |
| Percutaneous 7-o’clock anchor placement allows for improved access to inferior glenohumeral joint | Backing out of spinal needle or switching stick during dilation for cannula placement adds surgical time |
| Knotless fixation through single cannula technique improves efficiency for anchors at 3-o’clock position | Establishment of percutaneous portals must be done with care to avoid iatrogenic nerve injury |
OR, operating room.
Portal Placement
Our posterior viewing portal is made in line with the posterolateral edge of the acromion, rather than the traditional posterior viewing portal medial and distal to the posterolateral edge of the acromion (Fig 1). This modified portal will facilitate oblique and safe anchor trajectory into the posterior glenoid if needed. It is positioned superiorly so that suture anchors can be placed percutaneously at the 7-o’clock portal position.20
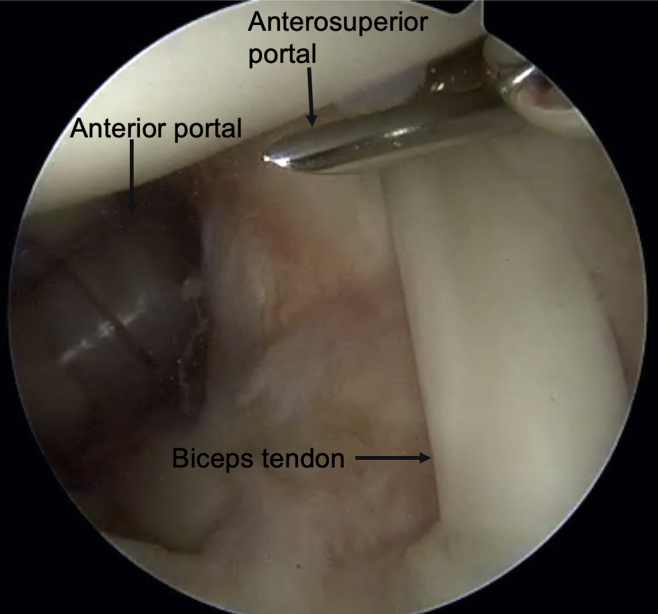
The posterior portal is established with a #11 blade, and a blunt trochar is used to introduce the camera and perform an initial diagnostic examination of the shoulder. Care is taken to visualize the biceps tendon, entirety of the labrum, subscapularis tendon and insertion, rotator cuff footprint, and axillary pouch. The anterior portal is then established, which is positioned just superior to the subscapularis (Fig 2). A spinal needle from a hip arthroscopy access kit (Stryker, Kalamazoo, MI) is used to create a precise and accurate trajectory for the portal (Table 2). A skin incision is then made, followed by insertion of a guidewire through the access needle. A cannulated switching stick is then placed over the guidewire, followed by sequential dilation using metal dilators (we dilate to accommodate an 8.25-mm cannula) and finally the cannula (7-mm clear twist in cannula; Arthrex, Naples, FL). We repeat this step for the anterosuperior cannula, which is positioned just superior to the biceps tendon, to insert our second cannula (Fig 3).
Fig 2.

Arthroscopic view of the left shoulder from the posterior viewing portal. With the patient positioned in the lateral decubitus position, the anterior portal is established, which is positioned just superior to the subscapularis.
Table 2.
Advantages and Disadvantages of Arthroscopic Shoulder Stabilization
| Advantages | Disadvantages |
|---|---|
| High lateral posterior viewing portal provides more panoramic view of glenoid | Conversion to potential open procedure is limited in the lateral decubitus position |
| Hip arthroscopy instruments ensure proper location and trajectory for cannula placement and help avoid overcrowding | Additional instrumentation required for cannula placement as well as single cannula passing technique |
| Percutaneous 7-o’clock portal allows proper inferior anchor placement | Accessory portal placement closer to neurovascular structures then traditional portals |
Fig 3.
Arthroscopic view of the left shoulder from the posterior viewing portal. The anterosuperior canula is established and positioned just superior to the biceps tendon.
At this point, the camera is removed from the posterior viewing portal while keeping the sheath in the posterior portal. The camera is inserted in the anterosuperior portal and a switching stick is placed through the sheath of the arthroscope into the posterior portal. The cannula is again sequentially dilated until a 7-mm clear twist-in cannula can be inserted. At this point, 3 portals with cannulas have been created in the shoulder. With the camera in the anterosuperior portal, the integrity of the posterior labrum can be fully evaluated, and Hill–Sachs defects can be assessed as well. The entirety of the diagnostic examination includes assessment of the labrum and glenoid cartilage circumferentially, humeral head cartilage, rotator cuff, biceps tendon, and presence of Hill–Sachs defects. The initial goal is to determine the extent of the capsulolabral injury. While many Bankart injuries consist of labral disruption of the anteroinferior labrum (3-o’clock to 5-o’clock), these injuries can often extend inferior and posterior, as is seen in this case example.
Labral Preparation
The anterior labral damage is first assessed, with the arthroscope in the posterior viewing cannula. A Bankart elevator is introduced from an anterior portal and is used to release and mobilize any medialized/healed labrum (Fig 4). A low-profile arthroscopic shaver is used to debride nonviable labral tissue and synovium. Then, a low-profile hooded burr is used to abrade the glenoid neck to prepare a bleeding surface for soft-tissue healing. At this point, the camera is moved into the anterosuperior viewing cannula so that similar preparation can be performed on the posteroinferior and inferior glenoid labrum.
Fig 4.

Arthroscopic view of the left shoulder from the posterior viewing portal. A Bankart elevator is introduced from the anterior portal and is used to release and mobilize any torn labrum.
Suture anchor Insertion
After the labrum has been fully mobilized and prepared, planning of suture anchor insertion can begin. In general, if the labral tear extends past the 5-o’clock position, the first anchors will be placed at the posteroinferior and inferior labrum using a percutaneous “7-o’clock” portal (Fig 5, Tables 1 and 2).20 With the camera viewing from anterosuperior portal, a hip-access spinal needle is inserted in the 6:30/7-o’clock position in preparation for percutaneous suture anchor placement. Once the spinal needle confirms the appropriate position and trajectory, the inner trocar will be removed, and a guidewire will be placed through the spinal needle. A small nick incision is be made, and the suture anchor (Suture Fix; Smith & Nephew) drill guide will then be placed over the guide wire in a cannulated fashion. Occasionally, the anchor will be lightly impacted onto the edge of the glenoid so that it firmly seats. The pilot hole is then drilled, and the anchor is inserted at the posterior extent of the tear. After insertion, the labrum and capsule will then be plicated in a posterior to anterior direction, with a suture shuttling lasso device (SutureLasso 90°; Arthrex) entering through the posterior cannula (or occasionally percutaneously at the 7-o’clock position). At this point, a single pass can be performed for a simple stitch repair configuration, or both limbs of the anchor can be shuttled for a mattress stitch. Care is taken to avoid tying the knot onto the glenoid face. This step can be repeated if additional posterior fixation is required, as was done in this example, working progressively anterior.
Fig 5.
Arthroscopic view of the left shoulder from the anterosuperior portal. A percutaneous accessory “7-o’clock” portal is used to place the first anchors at the posteroinferior and inferior labrum.
After the posteroinferior and inferior labrum is secured, the anteroinferior anchor is then addressed. Typically, the camera is then switched back to the posterior portal. A curved suture anchor (Suture Fix; Smith & Nephew) is then selected for anteroinferior anchor placement. The anchor is inserted through the anterior cannula and allows for anteroinferior anchor placement at the 5:30 or 5-o’clock position (Fig 6). One may alternatively use a straight suture anchor in a percutaneous technique through the subscapularis tendon. After the anchor is inserted, suture shuttling is performed using the curved suture lasso from either the same portal or from the 7-o’clock portal (Fig 5). Again, care is taken to avoid tying the knot on the glenoid face. This step can be repeating using an additional anchor (curved or straight) as progression is made up the anterior glenoid (Fig 7).
Fig 6.
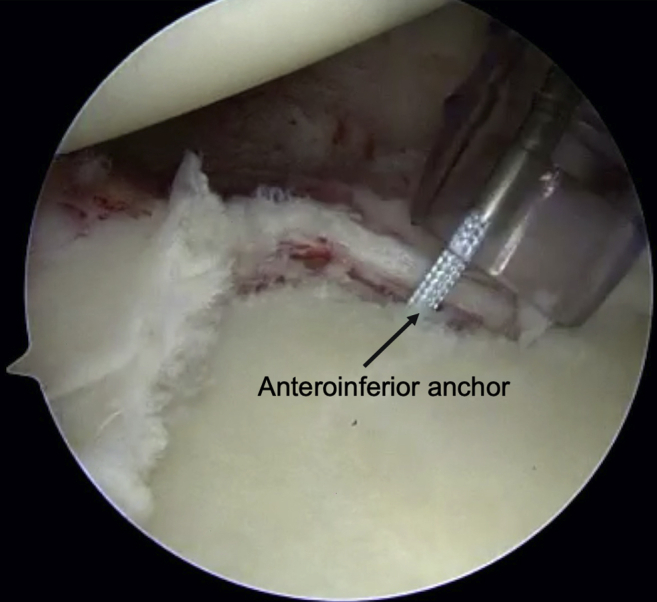
Arthroscopic view of the left shoulder from the posterior viewing portal. The anteroinferior anchor is inserted through the anterior cannula.
Fig 7.
Arthroscopic view of the left shoulder from the anterosuperior portal. This image demonstrates the final repair constructs, with labral fixation beginning at the posteroinferior labrum and continuing anteriorly. Note the low-profile nature of the mattress repair configuration of the labral fixation points.
If performing labral repair at the 3-o’clock position or 2-o’clock position, it is our preference to use low-profile knotless fixation with a single cannula technique (Table 1). A labral suture (LabralTape; Arthrex) is loaded into a self-capturing suture lasso device (Champion Slingshot; Stryker), which is then used to shuttle the suture around the labrum at the desired position. The device can then retrieve the tape in the same maneuver, withdrawing the passed tape through the cannula. The knotless anchor (2.4-mm PushLock; Arthrex) is then loaded and inserted in the standard fashion after drilling of the pilot hole.
Rehabilitation
The patient is immediately placed in an immobilization sling for 4 to 6 weeks postoperatively. During this time, the patient is progressed gradually through passive range of motion and active assist range of motion. After the immobilization sling is removed at the appropriate clinic visit (6 weeks’ postoperatively), active range-of-motion exercises can begin, which are aimed at strengthening the rotator cuff. Strengthening may begin 3 months’ postoperatively, with a return to sport approximately 5 to 6 months’ postoperatively.
Discussion
In recent decades, arthroscopic shoulder-stabilization surgeries have become an increasingly common intervention in treating shoulder instability in young, active individuals.9,10 Successful arthroscopic shoulder stabilization depends on obtaining both excellent visualization of the glenohumeral joint as well as proper access for labral preparation and anchor placement. The technique discussed presents a systematic and reproducible technique for improving visualization as well as ensuring accurate and useful placement of portals.
Our preferred positioning for addressing labral pathology is in the lateral decubitus position. Studies have consistently demonstrated that access to the entirety of the glenoid face and labrum can be more easily accomplished in the lateral decubitus position.21,22 In addition, recurrent shoulder instability following arthroscopic labral repair has shown to be lower when using the lateral decubitus versus beach chair position.23 To further improve visualization, our technique includes use of a lateral jack to add additional distraction of the glenohumeral joint in conjunction with a traditional traction device (Table 1). This allows for improved access of the inferior and posterior labrum, which can be crucial in successfully treating instability.
Access to traditional Bankart lesions of the anterior–inferior labrum has been well described for many years.24 While traditional portal placement allows for adequate visualization, access to the inferior and posterior glenoid for anchor placement can be difficult. Moving the posterior viewing portal into a high, lateral position just off the tip of the acromion can provide a more comprehensive view of the glenoid (Table 2) as well as option for safe instrumentation of the posterior and posterosuperior labrum. The use of a percutaneous 7-o’clock portal was introduced in early cadaver studies demonstrating its utility in reaching the inferior glenoid.25 Over the years, it has become accepted as a safe and reliable method of placing inferior glenoid anchors, with anatomic studies confirming safe distances from nearby neurovascular structures.25,26 Establishing the 7-o’clock portal in cadavers revealed an average distance of 39 mm and 28 mm from the axillary and suprascapular nerves, respectively.25 Our described technique adds the use of hip arthroscopy instruments to obtain and maintain proper trajectory for safe dilation and instrumentation.
In conclusion, positioning of the patient in the lateral decubitus position with an in-line and superiorly directed traction device with use of a high, lateral posterior viewing portal allows for excellent visualization for addressing labral pathology. Furthermore, the addition of a percutaneous 7-o’clock portal and use of hip arthroscopy access techniques for cannula placement creates an efficient, accurate, and reproducible technique.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: E.C.M. reports other from Smith & Nephew and Springer, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Arthroscopic shoulder stabilization is shown in the lateral decubitus position. The patient is placed in the lateral decubitus position, landmarks are marked, and the left shoulder is prepped and draped in standard fashion. The posterior viewing portal is established to perform an initial diagnostic examination of the shoulder, Preparation of the labrum is then accomplished through the anterior portal. The posteroinferior and inferior labrum are repaired by viewing from the anterosuperior portal and percutaneous suture anchor placement is achieved through an accessory 7-o’clock portal. After the labrum and glenoid are plicated in a posterior to anterior fashion, simple stich configuration is used for fixation. This method has provided an efficient, accurate and reproducible technique in cases of shoulder instability.
References
- 1.Best M.J., Tanaka M.J. Multidirectional instability of the shoulder: Treatment options and considerations. Sports Med Arthrosc Rev. 2018;26:113–119. doi: 10.1097/JSA.0000000000000199. [DOI] [PubMed] [Google Scholar]
- 2.Kane P., Bifano S.M., Dodson C.C., Freedman K.B. Approach to the treatment of primary anterior shoulder dislocation: A review. Phys Sportsmed. 2015;43:54–64. doi: 10.1080/00913847.2015.1001713. [DOI] [PubMed] [Google Scholar]
- 3.Kazar B., Relovszky E. Prognosis of primary dislocation of the shoulder. Acta Orthop Scand. 1969;40:216–224. doi: 10.3109/17453676908989501. [DOI] [PubMed] [Google Scholar]
- 4.Kroner K., Lind T., Jensen J. The epidemiology of shoulder dislocations. Arch Orthop Trauma Surg. 1989;108:288–290. doi: 10.1007/BF00932317. [DOI] [PubMed] [Google Scholar]
- 5.Good C.R., MacGillivray J.D. Traumatic shoulder dislocation in the adolescent athlete: Advances in surgical treatment. Curr Opin Pediatr. 2005;17:25–29. doi: 10.1097/01.mop.0000147905.92602.bb. [DOI] [PubMed] [Google Scholar]
- 6.Tokish J.M., McBratney C.M., Solomon D.J., Leclere L., Dewing C.B., Provencher M.T. Arthroscopic repair of circumferential lesions of the glenoid labrum. J Bone Joint Surg Am. 2009;91:2795–2802. doi: 10.2106/JBJS.H.01241. [DOI] [PubMed] [Google Scholar]
- 7.Gottschalk LJt, Walia P., Patel R.M. Stability of the glenohumeral joint with combined humeral head and glenoid defects: A cadaveric study. Am J Sports Med. 2016;44:933–940. doi: 10.1177/0363546515624914. [DOI] [PubMed] [Google Scholar]
- 8.Longo U.G., Rizzello G., Loppini M. Multidirectional instability of the shoulder: A systematic review. Arthroscopy. 2015;31:2431–2443. doi: 10.1016/j.arthro.2015.06.006. [DOI] [PubMed] [Google Scholar]
- 9.Zhang A.L., Montgomery S.R., Ngo S.S., Hame S.L., Wang J.C., Gamradt S.C. Arthroscopic versus open shoulder stabilization: Current practice patterns in the United States. Arthroscopy. 2014;30:436–443. doi: 10.1016/j.arthro.2013.12.013. [DOI] [PubMed] [Google Scholar]
- 10.Abrams J.S. Innovations in arthroscopic surgery of the shoulder: Advances in arthroscopic shoulder stabilization. Arthroscopy. 2003;19(suppl 1):106–108. doi: 10.1016/j.arthro.2003.09.034. [DOI] [PubMed] [Google Scholar]
- 11.Millett P.J., Clavert P., Warner J.J. Open operative treatment for anterior shoulder instability: When and why? J Bone Joint Surg Am. 2005;87:419–432. doi: 10.2106/JBJS.D.01921. [DOI] [PubMed] [Google Scholar]
- 12.Wang C., Ghalambor N., Zarins B., Warner J.J. Arthroscopic versus open Bankart repair: Analysis of patient subjective outcome and cost. Arthroscopy. 2005;21:1219–1222. doi: 10.1016/j.arthro.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 13.Green M.R., Christensen K.P. Arthroscopic versus open Bankart procedures: A comparison of early morbidity and complications. Arthroscopy. 1993;9:371–374. doi: 10.1016/s0749-8063(05)80308-1. [DOI] [PubMed] [Google Scholar]
- 14.Fabbriciani C., Milano G., Demontis A., Fadda S., Ziranu F., Mulas P.D. Arthroscopic versus open treatment of Bankart lesion of the shoulder: A prospective randomized study. Arthroscopy. 2004;20:456–462. doi: 10.1016/j.arthro.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 15.Cole B.J., L'Insalata J., Irrgang J., Warner J.J. Comparison of arthroscopic and open anterior shoulder stabilization. A two to six-year follow-up study. J Bone Joint Surg Am. 2000;82:1108–1114. doi: 10.2106/00004623-200008000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Cooper D.E., Arnoczky S.P., O'Brien S.J., Warren R.F., DiCarlo E., Allen A.A. Anatomy, histology, and vascularity of the glenoid labrum. An anatomical study. J Bone Joint Surg Am. 1992;74:46–52. [PubMed] [Google Scholar]
- 17.Nebelung W., Jaeger A., Wiedemann E. Rationales of arthroscopic shoulder stabilization. Arch Orthop Trauma Surg. 2002;122:472–487. doi: 10.1007/s00402-002-0423-6. [DOI] [PubMed] [Google Scholar]
- 18.Makhni E.C., Lamba N., Swart E. Revision arthroscopic repair versus latarjet procedure in patients with recurrent instability after initial repair attempt: A cost-effectiveness model. Arthroscopy. 2016;32:1764–1770. doi: 10.1016/j.arthro.2016.01.062. [DOI] [PubMed] [Google Scholar]
- 19.Leroux T.S., Saltzman B.M., Meyer M. The influence of evidence-based surgical indications and techniques on failure rates after arthroscopic shoulder stabilization in the contact or collision athlete with anterior shoulder instability. Am J Sports Med. 2017;45:1218–1225. doi: 10.1177/0363546516663716. [DOI] [PubMed] [Google Scholar]
- 20.Cvetanovich G.L., McCormick F., Erickson B.J. The posterolateral portal: Optimizing anchor placement and labral repair at the inferior glenoid. Arthrosc Tech. 2013;2:e201–e204. doi: 10.1016/j.eats.2013.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hamamoto J.T., Frank R.M., Higgins J.D., Provencher M.T., Romeo A.A., Verma N.N. Shoulder arthroscopy in the lateral decubitus position. Arthrosc Tech. 2017;6:e1169–e1175. doi: 10.1016/j.eats.2017.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peruto C.M., Ciccotti M.G., Cohen S.B. Shoulder arthroscopy positioning: Lateral decubitus versus beach chair. Arthroscopy. 2009;25:891–896. doi: 10.1016/j.arthro.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 23.Frank R.M., Saccomanno M.F., McDonald L.S., Moric M., Romeo A.A., Provencher M.T. Outcomes of arthroscopic anterior shoulder instability in the beach chair versus lateral decubitus position: A systematic review and meta-regression analysis. Arthroscopy. 2014;30:1349–1365. doi: 10.1016/j.arthro.2014.05.008. [DOI] [PubMed] [Google Scholar]
- 24.Paxton E.S., Backus J., Keener J., Brophy R.H. Shoulder arthroscopy: Basic principles of positioning, anesthesia, and portal anatomy. J Am Acad Orthop Surg. 2013;21:332–342. doi: 10.5435/JAAOS-21-06-332. [DOI] [PubMed] [Google Scholar]
- 25.Davidson P.A., Rivenburgh D.W. The 7-o'clock posteroinferior portal for shoulder arthroscopy. Am J Sports Med. 2002;30:693–696. doi: 10.1177/03635465020300051101. [DOI] [PubMed] [Google Scholar]
- 26.Difelice G.S., Williams R.J., 3rd, Cohen M.S., Warren R.F. The accessory posterior portal for shoulder arthroscopy: Description of technique and cadaveric study. Arthroscopy. 2001;17:888–891. doi: 10.1016/s0749-8063(01)90015-5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic shoulder stabilization is shown in the lateral decubitus position. The patient is placed in the lateral decubitus position, landmarks are marked, and the left shoulder is prepped and draped in standard fashion. The posterior viewing portal is established to perform an initial diagnostic examination of the shoulder, Preparation of the labrum is then accomplished through the anterior portal. The posteroinferior and inferior labrum are repaired by viewing from the anterosuperior portal and percutaneous suture anchor placement is achieved through an accessory 7-o’clock portal. After the labrum and glenoid are plicated in a posterior to anterior fashion, simple stich configuration is used for fixation. This method has provided an efficient, accurate and reproducible technique in cases of shoulder instability.