Summary
We report the case of a 95-year-old man with soft tissue deficiency associated with a pubic abscess that occurred 30 years after prostate cancer surgery and radiation therapy. A fistula with purulent discharge without any obvious cause appeared in the midline of the lower abdomen and progressed to a soft tissue defect in which several calcium phosphate stones of 5-8 mm in diameter were found. Computed tomography showed calcium deposits on the surface of the pubis and irregular zonal calcifications extending from the pubis to the medial region of both thighs.
Conservative treatment did not improve the patient's condition; thus, surgical treatment was performed. The pedicled rectus femoris muscle flap was elevated from the left thigh and transferred to fill the tissue defect, then a split thickness skin graft was applied on it. The tissue defect was successfully repaired, and the patient was able to regain ambulation ability.
In the present case, it was presumed that urine exudation around the bladder due to radiation cystitis was involved in the formation of ectopic calculi and subsequent infection. In reconstructing a complex defect associated with infection, using muscle flaps to fill the dead space with well vascularized tissue is considered to be appropriate. In our case, we chose a rectus femoris muscle flap, which has advantages in volume and versatility of transposition owing to long vascular pedicle and requires no microsurgical vascular anastomosis. As a result, the preoperative activity was maintained, the infection was treated, and a good course was obtained.
Keywords: Rectus femoris muscle flap, Prostate cancer, Ectopic calculi, Radiotherapy, Pubis
Introduction
Radiotherapy is a common treatment modality for the management of pelvic malignancies. As complications, inflammation of the pubis and bladder1 and infectious disease, such as osteomyelitis and vesical fistula,2 have been reported. In this report we present a case of reconstruction of massive soft tissue loss complicated by an abscess secondary to the infection of ectopic stones formed around the pubis after prostate cancer surgery and radiation therapy. Various pedicled or free flaps are used to reconstruct complex defects in the abdominal wall.3 In our case, pedicled rectus femoris muscle flap transfer was performed and a satisfactory result was obtained.
Case report
The patient in the present case was a 95-year-old man with a history of prostate cancer who had undergone radical prostatectomy and radiation therapy approximately 30 years previously.
A fistula with purulent discharge appeared without any obvious cause in the midline of the lower abdomen, and he visited a nearby urology clinic. Although he received wound treatment and oral antibiotic treatment, his symptoms gradually deteriorated without improvement, and he was referred to our hospital.
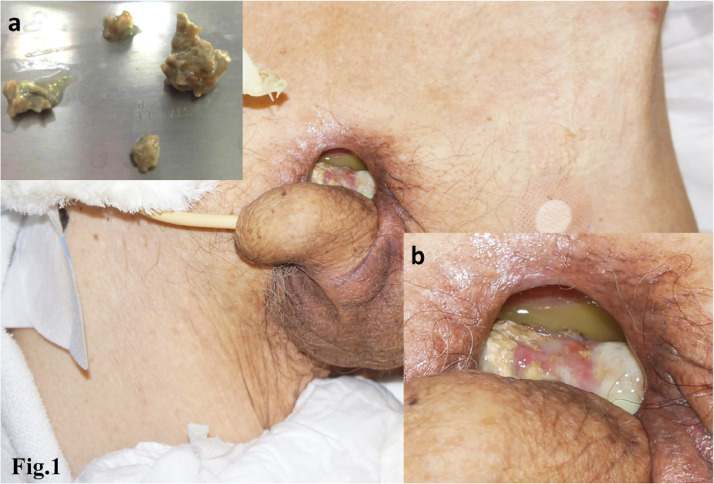
Incision and drainage of the abscess to the fistula was performed and an old silk suture thread and several 5-8 mm diameter stones were found in the wound and removed. A component analysis of the excised stones revealed they were composed of calcium phosphate. The exposed pubic bone was denatured white by calcium deposits that had adhered to the surface (Figure 1).
Figure 1.
The appearance of the wound on admission. (a) Removed ectopic stones. (b) The pubic bone was exposed and denatured white by calcium deposits that adhered to the surface. Pus was observed to have accumulated around the pubic bone.
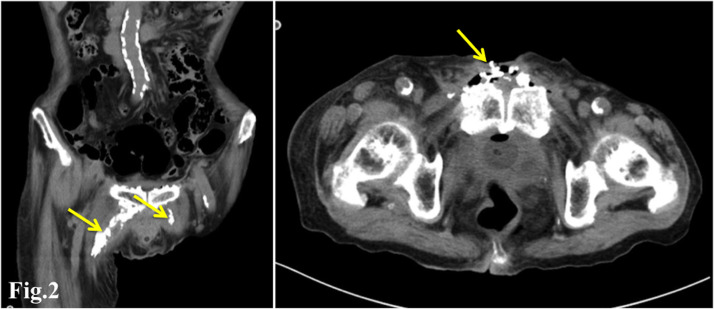
Computed tomography showed irregular calcium deposits on the entire surface of the pubis and irregular zonal calcifications extending from the pubis to the medial region of both thighs (Figure 2).
Figure 2.
Computed tomography showed irregular calcium deposits on the entire pubic bone surface and a calcified mass in a beaded shape from the anterior pubic symphysis to the medial sides of both proximal thighs.
MRI showed edematous changes in the peripubic tissue but no intensity change in the pubic bone marrow.
Cystography was performed, but no vesical fistula was found, and a bacterial examination of the wound detected multiple organisms.
Although cleaning and curettage of the pubic surface at the bed side was performed daily, the infection did not improve and the drainage of pus persisted. Thus, surgical treatment was performed.
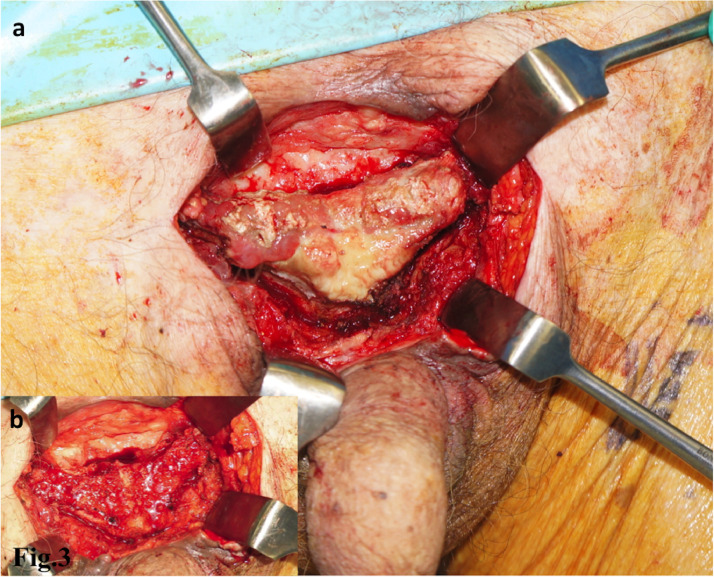
The exposed and degenerated portion of the pubic bone was excised with a bone chisel. The cancellous bone on the resected surface was normal with no findings of necrosis or infection (Figure 3).
Figure 3.
Intraoperative findings. (a) The exposed and degenerated portion of the pubic bone was excised. (b) The cancellous bone on the resected surface was normal, with no findings of necrosis or infection.
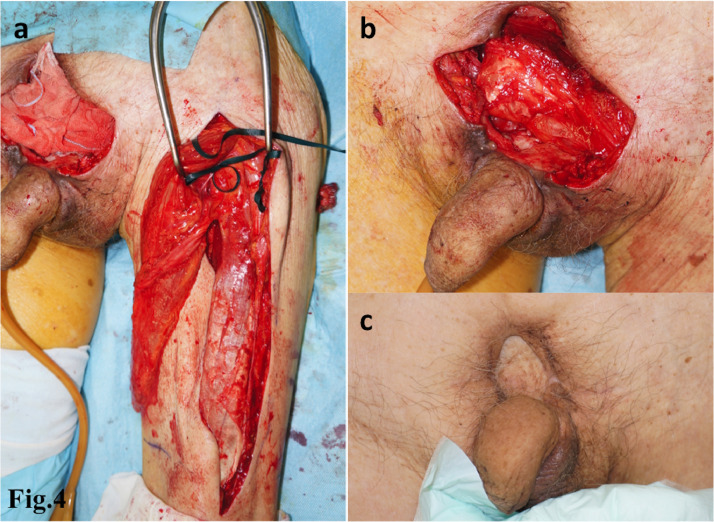
The pedicled rectus femoris muscle flap was elevated from the left thigh. Initially, we planned to use a combined flap including the anterolateral thigh (ALT) flap, but the perforator to the ALT flap was found to be extremely thin and passed through the vastus lateralis muscle. Only a muscle flap was used due to the potential for an adverse effect on ambulation due to further damage to the vastus lateralis muscle, as well as the sacrifice of the rectus femoris muscles.
The muscle flap was passed through a subcutaneous tunnel formed in the groin region to the tissue defect, which was filled in as two folds, and the split thickness skin graft was applied on the flap (Figure 4).
Figure 4.
(a) The pedicled rectus femoris muscle flap that was elevated from the left thigh. (b) The tissue defect was filled with the muscle flap, and a split thickness skin graft was applied on the flap. (c) Seventeen months after the operation.
Pathological findings of the resected pubis showed fibroplastic lesions in the bone marrow tissue, some of which are accompanied by osteonecrotic lesions, granulation tissue, osteoclasts, and osteoblasts.
The tissue defect was successfully repaired, and the patient was discharged to return home at 6 weeks after the operation, and was able to regain his ambulation ability at home. His activity gradually decreased as his cognitive symptoms progressed; however, at 17 months after the operation, the pubic area was in good condition with no relapse of symptoms of infection.
Discussion
Definitive radiation therapy for prostate cancer has become a standard treatment, and is associated with several complications, including inflammation of the bladder and rectum resulting in stenosis and fistula formation,1 and pubic bone osteomyelitis.2
Among these complications, radiation cystitis often manifests as hemorrhagic cystitis with difficult hemostasis4 and spontaneous rupture of the bladder5 has been reported after a long course of radiation therapy.
In addition to overt bleeding cystitis, there is a possibility that subclinical vesical fistula associated with bladder wall degeneration may occur. In our case, we could not confirm the presence of a vesical fistula; however, bead-like continuous urinary calculus was observed from the anterior pubic symphysis to the medial sides of both proximal thighs. MRI showed a change in intensity along the adductor muscle, where ectopic stones were observed on the CT image. It is known that the loose connective tissue that continues from the prevesical space into the adductor muscle is a path through which fluid, such as pus and urine, flows down. Ennaciri and Bitard6 reported a case of vesical fistula after radical prostatectomy and radiation treatment, in which large fluid collection originating from the urethrovesical junction developed in the thigh. Yoshida et al.7 reported a case with abscess formation in the prevesical space to the bilateral thigh muscles that occurred secondarily to osteomyelitis of the pubis, and described the anatomy between the prevesical space and femoral sheath.
The pathogenesis of the present case was considered to be as follows: the urine that exuded from fibrosed and degenerated bladder wall due to radiation treatment collected around the pubic bone into the adductor muscles of both thighs formed ectopic urinary stones, and urinary tract infection also spread to the surface of the pubis and nearby stones and formed an abscess.
Various pedicled or free flaps are used to reconstruct complex abdominal wall defects that develop in association with infection or resection of a malignant tumor.3 Muscle flaps are considered superior to fasciocutaneous flaps when it comes to treating an infected wound because they can fill the dead space with well vascularized tissue.8,9
Local muscle flaps, represented by the rectus abdominal muscle flap are the optimal choice for an abdominal wall defect.10 However, orthopedic surgeons are not familiar with their use. In our case, we chose the rectus femoris muscle flap, which has advantages in muscle volume and versatility of transposition due to the long vascular pedicle. This flap was selected because it was located well away from the area of irradiation and required no microsurgical vascular anastomosis. Although the muscle belly was atrophic due to old age, an appropriate volume was obtained by folding it in two. The preoperative activity was maintained, the infection was treated, and a good course was obtained.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Declaration of Competing Interest
We have no conflicts of interest to disclose.
References
- 1.Mallick S, Madan R, Julka PK, Rath GK. Radiation Induced Cystitis and Proctitis - Prediction. Assessment and Management. Asian Pac J Cancer Prev. 2015;16:5589–5594. doi: 10.7314/apjcp.2015.16.14.5589. [DOI] [PubMed] [Google Scholar]
- 2.Madden-Fuentes RJ, Osteomyelitis Peterson AC.Pubic Bone, Fistula Pubosymphyseal Urinary. A Poorly RecognizedComplication in Prostate Cancer Survivors. Oncology. 2017;31:169–173. [PubMed] [Google Scholar]
- 3.Rohrich RJ, Lowe JB, Hackney FL, Bowman JL, Hobar PC. An algorithm for abdominal wall reconstruction. Plast Reconstr Surg. 2000;105:202–216. doi: 10.1097/00006534-200001000-00036. [DOI] [PubMed] [Google Scholar]
- 4.Ma JL, Hennessey DB, Newell BP, Bolton DM, Lawrentschuk N. Radiotherapy-related complications presenting to a urology department: a more common problem than previously thought? BJU Int. 2018;121(Suppl 3):28–32. doi: 10.1111/bju.14145. [DOI] [PubMed] [Google Scholar]
- 5.Fujikawa K, Yamamichi F, Nonomura M, Soeda A, Takeuchi H. Spontaneous rupture of the urinary bladder is not a rare complication of radiotherapy for cervical cancer: report of six cases. Gynecol Oncol. 1999;73:439–442. doi: 10.1006/gyno.1999.5347. [DOI] [PubMed] [Google Scholar]
- 6.Ennaciri S, Bitard TM. Collection in the thigh revealing bladder fistula after radiotherapy for prostate cancer. Pan Afr Med J doi: 10.11604/pamj.2018.30.197.16037. http://www.panafrican-med-journal.com/content/article/30/197/full/ [Accessibility verified June 8, 2020]. [DOI] [PMC free article] [PubMed]
- 7.Yoshida S, Nakagomi K, Goto S. Abscess formation in the prevesical space and bilateral thigh muscles secondary to osteomyelitis of the pubis–basis of the anatomy between the prevesical space and femoral sheath. Scand J Urol Nephrol. 2004;38:440–441. doi: 10.1080/00365590410031652. [DOI] [PubMed] [Google Scholar]
- 8.Smith IM, Austin OM, Batchelor AG. The treatment of chronic osteornyellitis:a10 years audit. Jplast Reconstr Aesthet surg. 2006;59:11–15. doi: 10.1016/j.bjps.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 9.Russell RC, Graham DR, Feller AM, Zook EG, Mathur A. Experimental evaluation of the antibiotic carrying capacity of a muscle flap into a fibrotic cavity. Plast Recon Surg. 1988;81:162–170. doi: 10.1097/00006534-198802000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Kaufman DA, Browne BM, Zinman LN, Vanni AJ. Management of Radiation Anterior Prostato-symphyseal Fistulas With Interposition Rectus Abdominis Muscle Flap. Urology. 2016;92:122–126. doi: 10.1016/j.urology.2016.01.029. [DOI] [PubMed] [Google Scholar]