Abstract
Objectives
Although cardiovascular disease (CVD) risk has lessened in Korea, it is unclear whether older adults in all socioeconomic strata have benefited equally. This study explored trends in income disparities in CVD risk among older adults in Korea.
Methods
This was a secondary analysis of Korean National Health and Nutrition Examination Survey data (2008–2017), targeting 14,836 older adults (≥65 years). Socioeconomic position, defined as income and use of welfare benefits, was the primary indicator. The outcome was binary for predicted CVD risk (<90th vs. ≥ 90th). The Slope Index of Inequality (SII) and Relative Index of Inequality (RII) were used to assess trends in disparities.
Results
The percentage of older adults with a predicted CVD risk of 90% or more declined over time, but this was due to a decrease among the more affluent. Disparities have persisted since 2012, with a worsening trend seen for Medicaid recipients. We found significant absolute and relative disparities among men over 75 years of age in recent years (SII > 0.19, RII > 7).
Conclusions
These results may inform and improve policies regarding income disparity reduction and cardiovascular health.
Keywords: Korea, Income, Trends, Cardiovascular health, Older adults
Abbreviations: CVD, cardiovascular disease; GLM, generalized linear model; KCDC, Korean centers for disease control and prevention; KNHANES, Korean national health and nutrition examination survey; KNHI, Korean national health insurance; MAR, missing at random; OECD, organization for economic cooperation and development; RD, risk difference; RII, relative index of inequality; RR, relative risk; SEP, socioeconomic position; SII, slope index of inequality
Highlights
-
•
Income disparities in CVD risk have persisted since 2012, with a worsening trend seen for Medicaid recipients.
-
•
Our results highlight the need to improve CVD risk management services offered to the economically disadvantaged.
-
•
It is important to consider both the absolute and relative terms when examining the disparity trends.
1. Introduction
Cardiovascular diseases (CVDs) are among the most serious public health problems in many countries. Despite overall improvements in cardiovascular health, studies consistently report widening income-related disparities in CVD outcomes (Coke, 2018; Mills et al., 2016). As such, tracking these disparities has become an important component of the global health policy agenda (Office of Disease Prevention and Health Promotion, 2020). Importantly, this monitoring has impacted the government's plans and has led to a lessening of burden of health problems among economically disadvantaged populations (Pahigiannis et al., 2019).
South Korea (hereafter “Korea”) is no exception. Although change patterns vary both among and within different age and gender groups, most studies demonstrate that income-related disparities in cardiovascular health are evident and that a widening gap exists over time in Korea (Kim et al., 2017; Lee & Im, 2020). Based upon the surveillance data, government policies have been consistently targeted toward reducing disparities. For instance, the Korean government has expanded health promotion social policies, welfare programs, and care services related to CVD risk factors, targeting populations with low incomes (Lee et al., 2015). However, older adults have not been a major focus of these efforts.
It is critical to examine trend data in disparities in CVD among older adults so that future social policies for the health of the older population with lower income take into account the unique circumstances experienced by this population (Khang & Lee, 2012). The current Korean older adult generation has lived through major politico-economic changes in the society over the past decades such as rapid economic growth, economic crisis, neoliberal structural reforms and increased income disparity (Lee et al., 2017). Such income disparities have remained relatively constant since the early 2000s, which has led to widening health disparities and deepening health problems (Park et al., 2012).
In addition, in recent years, the limitations of the current public health insurance system have left a growing number of medically-eligible older adults abstaining from social and health benefits. In Korea, enrollment in health insurance is compulsory, with most of the population covered by Korean national health insurance (KNHI). An estimated 3–5% of people below the poverty line who cannot afford health insurance premiums are covered by Medicaid. Although KNHI and Medicaid together virtually guarantee universal access to health insurance coverage, low benefit levels and high out-of-pocket costs impose limits to the health services received by some beneficiaries, notably those in lower income brackets (Jeon & Kwon, 2017; Kwon, 2009). Moreover, the efficacy of Medicaid is continuously questioned for its health support for those covered by the program (Jang et al., 2015). Indeed, research has revealed that increased CVD prevalence could be largely explained by income status among older adults (Choi et al., 2015; Kim et al., 2014).
One of the major roles of the public health insurance system is to reduce the widening health gap between socioeconomic groups. Further, with increasing life expectancy, Korean older adults are affected by more diverse CVD risk factors. Studies of the persistence or worsening of income-driven disparities in cardiovascular health, therefore, would be of substantial interest to policymakers in Korea and in other nations facing disparities in cardiovascular care.
The present study thus aimed to explore trends in income disparities in cardiovascular health among older adults in Korea. In particular, we aimed to explain cardiovascular disparities with the trends in the prevalence and disparities of CVD risk conditions. This approach will inform health policies for reducing future burden of CVD and responses to future disparities in CVD morbidity and mortality (Martinson et al., 2016).
2. Methods
2.1. Design
This is a secondary analysis of data from the Korean National Health and Nutrition Examination Survey (KNHANES) conducted by Korea Centers for Disease Control and Prevention (KCDC). KNHANES is a nationwide survey composed of an ongoing series of cross-sectional surveys that provides comprehensive information on the health status, health behavior, nutritional status, and socio-demographics of people living across the 600 national districts in Korea. Beginning with KNHANES IV (2007–2009), the survey became an annual rolling survey that used a stratified, multi-stage, clustered sampling method to allow for annual analysis of national representative sample data. Sampling units were based on geographical area, gender, and age using household registries. KNHANES is composed of three distinct sections: a health interview survey, a health examination survey, and a nutrition survey for dietary assessment. The present study uses the health interview and health examination survey.
The KNHANES's overall response rate is targeted at 75%. The response rate of participants was approximately 77.8% in KNHANES IV, 80% in KNHANES V (2010–2012), 78.4% in KNHANES VI (2013–2015), and 76.6% in KNHANES 2016–2017 on average. Further details of KNHANES can be found elsewhere (Kweon, 2014).
2.2. Ethical considerations
KNHANES is a free public data set which does not include personal information. The study was exempted by the institutional review board of the university where authors are affiliated. The KCDC and related academic societies have managed external quality control programs for all steps (including survey administration, data collection, laboratory analysis and data processing) as well as internal quality assurance and control procedures. The survey staff members were required to complete an intensive training course and to conduct supervised practice before working in the survey field for the control of the survey. The interviewer was not given any information about specific participants before conducting the interviews, and all the surveys are conducted with the participants’ consent using a consent form that described the purpose of the study as well as the potential benefits and dangers.
2.3. Analysis sample
Trend analyses were conducted with the data from 2008 to 2017 using five two-year time periods: 2008–2009, 2010–2011, 2012–2013, 2014–2015, and 2016–2017. Questionnaire variables related to each measurement item indicated in this study remained consistent across the relevant survey years (2008–2017). From the initial total of 15,730 participants, 708 were excluded for incomplete anthropometric data. In addition, 186 people with a preexisting diagnosis of CVD were excluded to prevent reverse causality; respondents were considered to have a pre-existing diagnosis if they had ever been told by the doctor that they had angina pectoris, stroke, or myocardial infarction. A final total of 14,836 older adults (57.94% female) were included in the analyses.
2.4. Measures
2.3.1. Cardiovascular health
We operationalize the term “cardiovascular health” as the risk of developing CVD over a 10-year period. We determined the individual risk for CVD, using a health risk appraisal model for coronary heart disease based on data collected nationwide from the Korean Heart Study (Jee, Batty, et al., 2014). This model was developed based on a multivariate Cox proportional hazard model using data from a retrospective cohort in alignment with the Framingham equation model (Anderson et al., 1991). The proposed model was later validated in another random sample representative of the Korean population enrolled in the national insurance system (Jee, Jang, et al., 2014).
Risk assessment for this study was based on the summation of categorical values for the following major CVD risk factors: a) sex, b) age, c) total cholesterol, d) high-density lipoprotein cholesterol, e) systolic blood pressure, f) smoking, and g) diabetes (Supplement). This generates a continuous risk score, with lower scores representing better cardiovascular health. We used the score to identify binary levels of CVD risk, defined as low-level and high-level risk groups. As suggested in the literature (Kang & Hong, 2017; Lee et al., 2016), we defined cases as belonging to the high-risk group when each risk was ≥90 percentile for each sex, as the model was validated by comparing actual events and prediction of events according to the decile of predicted risk for each sex (Jee, Jang, et al., 2014).
2.3.2. Socioeconomic position measures
Income was used as the indicator of SEP. Equivalized income (the household monthly income divided by the square root of the household size, “OECD,” n.d.) and welfare benefits were used to define five income groups. The target population was first divided into KNHI beneficiaries and Medicaid beneficiaries. The former was subdivided into quartiles based on equivalized income (quartile 1, highest; quartile 4, lowest), and this determination was based on the Korean national household income quartile criteria. Next, older adults belonging to the Medicaid beneficiary group were classified separately and ranked in a bottom group.
2.3.3. Covariates
We included the following covariates, which showed a significant association (p-value < .05) with the main outcome of this study (i.e. binarized CVD risk) in the univariate analysis: (a) initial health status including activity limitation (yes/no); (b) behavioral factors including weight control (yes/no), regular physical activity (yes/no), and regular health check-up (yes/no); and (c) geographical location (urban/rural). Activity limitation was evaluated by a single question: “Have you experienced restrictions in your daily life and social activities due to current health problems?” Weight control was assessed by a single question: “Have you ever tried to control your weight on your own over the past few years?” Regular health check-ups were measured by a single question: “'Have you had a regular general health check-up or a comprehensive medical check-up over the past few years?” Lastly, regular physical activity was defined by the fulfillment of “sufficient activity” by the Korean version of the International Physical Activity Questionnaire standard (Oh et al., 2007).
2.5. Statistical analysis
Given the importance of the age-specific analysis in disparities research (Khang et al., 2004), all analyses were conducted by 10-year birth cohorts (i.e. younger-old group: 65–74 years, older-old group: ≥ 75 years). Stratification was also done by gender as the ways in which income contributes to poorer cardiovascular health status in women compared with men vary (Backholer et al., 2017).
Sample characteristics were reported for each of the two-year five time period using descriptive statistics. The prevalence of older adults with predicted CVD risk of 90% or greater (i.e. high CVD risk) was estimated for different gender and age groups in each time period. To test the statistical significance of a trend in prevalence over time, we computed p-values for the linear effect of the survey year variable representing five time periods on the outcome variable (i.e. binary levels of CVD risk), as estimated by logistic regression.
Disparities in high CVD risk were assessed using both absolute (the risk difference [RD] and the slope index of inequality [SII]) and relative inequality measures (the relative risk [RR] and the relative index of inequality [RII]). The RD and RR involve pair-wise comparisons of different socioeconomic groups. The RII and SII are regression-based summary measures of inequalities calculated across the entire socioeconomic distribution (Moreno-Betancur et al., 2015).
To estimate the SII and RII, the grouped income data are transformed into cumulative rank probabilities (ridit scores; Donaldson, 1998) ranging from 0 (highest income) to 1 (lowest income), with values reflecting the midpoint of the cumulative proportion of the population in each income group (Eq. (1)). This score was then used in generalized linear models (GLMs) with an identity link function to calculate SIIs, and with a logarithmic link function to model RIIs (Eq. (2)). Each analysis using a GLM regression included the following covariates – initial health status, behavioral factors, and rural/urban residence – for ridit score.
| (1) |
| (2) |
β1 is the coefficient of interest and expresses SII when the identity link is used and RII when the log link is used. Y = 1 is for the high-risk group, and Y = 0 is for the low risk group under our study. Ridit is the ridit score, which replaces income level. β2, β3 corresponds to relevant regression coefficients. The error term has a binomial distribution.
SII, the β1 under binomial regression, represents the risk difference (i.e., the absolute health gap) between the person of the lowest SEP rank and the person of the highest rank. RII, the exponential of the slope, exp (β1) under log-binomial regression, indicates the proportionate difference in outcome between the extreme bottom versus the extreme top of the SEP hierarchy. In this analysis, the highest (i.e., most advantaged) income group was set as the reference group. A positive SII and an RII that is larger than 1 represent inequality in favor of the highest income group.
The linear trend of RR and PD for high CVD risk was conducted by obtaining the p-value for an interaction term (income by survey year) in GLMs. To assess trends in RII and SII, we used the methods outlined by Ernstsen et al. (2012) using pooled survey data (with survey-specific ridit scores) and included covariates for ridit score described earlier and a interaction term (ridit score by survey year). A p value of < .05 for the interaction is indicative of significant change in the inequality measure over time. To accommodate a possible nonlinear quadratic trend, a second order polynomial trend was also included in the main effect model by adding the time2 variable along with the interaction of the independent variable and the polynomial trends.
All analyses were performed with SAS software (SAS Institute, Inc., Cary North Carolina) after accounting for the complex sample designs including primary sampling units, stratification, and sample weights. For the merged data, we calculated an integrated weight in proportion to the total number of primary sample units of each year based on the methods recommended by the KCDC. The number of samples with missing outcome measures was minimal (<6% for all variables) thus the maximum number of available samples was retained by single imputation. Missingness of continuous variables were missing at random (MAR) thus imputed with the expectation-maximization method. Missing values on categorical variables, which are also MAR, were replaced with the most common category for each variable.
3. Results
3.1. Characteristics of the study population by survey year (Table 1)
Table 1.
Characteristics of the study population by survey year.
| 2008–2009 | 2010–2011 | 2012–2013 | 2014–2015 | 2016–2017 | |
|---|---|---|---|---|---|
| Gender, n (%) | |||||
| Men | 1236 (39.9) | 1230 (42.7) | 1181 (42.1) | 1276 (43.1) | 1317 (42.7) |
| Women | 1866 (60.1) | 1651 (57.3) | 1625 (57.9) | 1683 (56.9) | 1771 (57.3) |
| Age, years | |||||
| Mean ± SD | 72.20 ± 4.83 | 72.37 ± 4.74 | 72.53 ± 4.89 | 72.69 ± 5.01 | 72.86 ± 5.12 |
| Age, group, n (%) | |||||
| 65–74 years | 2067 (66.6) | 1922 (66.7) | 1769 (63.0) | 1800 (60.8) | 1832 (63.1) |
| 75+ years | 1035 (33.4) | 959 (33.3) | 1037 (37.0) | 1159 (39.2) | 1256 (36.9) |
| Incomea, n (%) | |||||
| Quartile 1 ($1801–) | 775 (25.0) | 675 (23.4) | 685 (24.4) | 731 (24.7) | 745 (24.3) |
| Quartile 2 ($1051–1800) | 683 (22.0) | 715 (24.8) | 705 (25.1) | 696 (23.5) | 757 (24.0) |
| Quartile 3 ($601–1050) | 721 (23.2) | 648 (22.5) | 621 (22.1) | 649 (21.9) | 686 (22.4) |
| Quartile 4 (–$600) | 650 (21.0) | 695 (24.1) | 631 (22.5) | 686 (23.2) | 699 (22.7) |
| Medicaid | 273 (8.8) | 148 (5.2) | 164 (5.9) | 197 (6.7) | 201 (6.6) |
n, unweighted number of cases in the sample.
SD, standard deviation.
Based on the Korean national household income quartile criteria. Korean won is converted to US dollar.
Table 1 shows the characteristics of the study population by time periods. The percentage of women was consistently higher than men. The mean age remained approximately 72 years old across the survey years. The proportion of the older-old group within the entire population fluctuated slightly without a clear direction of change and it ranged from 33 to 39%. The quartile income distribution of older adults also remained stable, and the proportion of Medicaid remained between 6 and 9% across the years.
3.2. Prevalence of high CVD risk for different income levels by different age and gender groups (Table 2)
Table 2.
Prevalence of high CVD for different income levels by different age and gender groups.
| 2008–2009 |
2010–2011 |
2012–2013 |
2014–2015 |
2016–2017 |
p-value for x2 trend |
||
|---|---|---|---|---|---|---|---|
| % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | linear | polynomial | |
| 65–74 years | |||||||
| Men | |||||||
| Quartile 1 | 11.1 | 9.0 | 10.5 | 5.9 | 5.1 | .015a | .553 |
| (6.5–15.6) | (3.3–14.8) | (4.8–16.3) | (2.4–9.4) | (2.1–8.1) | |||
| Quartile 2 | 7.3 | 12.1 | 10.0 | 6.6 | 9.4 | .913 | .687 |
| (3.2–11.5) | (6.7–17.5) | (5.6–14.4) | (2.9–10.2) | (4.5–14.3) | |||
| Quartile 3 | 12.0 | 12.4 | 15.5 | 8.8 | 9.1 | .214 | .332 |
| (7.4–16.6) | (7.5–17.3) | (9.0–22.0) | (4.8–12.8) | (4.3–13.8) | |||
| Quartile 4 | 9.2 | 10.4 | 11.3 | 10.0 | 10.6 | .781 | .762 |
| (4.7–13.6) | (5.5–15.3) | (5.7–16.9) | (4.0–15.9) | (5.0–16.2) | |||
| Medicaid | 9.8 | 8.6 | 6.8 | 13.6 | 18.6 | .325 | .441 |
| (3.1–16.6) | (6.3–11.0) | (0.0–16.6) | (4.2–23.0) | (0.0–40.1) | |||
| Total | 10.0 | 11.0 | 11.6 | 7.9 | 9.0 | .245 | .471 |
| (8.0–12.0) | (8.3–13.6) | (8.9–13.6) | (5.8–10.0) | (6.2–11.8) | |||
| Women | |||||||
| Quartile 1 | 6.4 | 11.4 | 10.3 | 6.3 | 4.3 | .088 | .031a |
| (3.2–9.6) | (6.3–16.5) | (5.2–15.3) | (3.2–9.4) | (1.3–7.4) | |||
| Quartile 2 | 12.3 | 12.2 | 9.4 | 6.7 | 7.3 | .029a | .970 |
| (7.4–17.2) | (7.4–16.9) | (4.9–14.0) | (3.1–10.3) | (3.9–10.6) | |||
| Quartile 3 | 13.3 | 13.9 | 8.7 | 6.0 | 11.4 | .259 | .129 |
| (8.3–18.3) | (8.6–19.2) | (4.7–12.7) | (2.6–12.7) | (6.9–16.0) | |||
| Quartile 4 | 11.3 | 11.2 | 9.1 | 10.4 | 8.5 | .369 | .910 |
| (6.7–15.8) | (6.3–16.1) | (4.8–13.4) | (6.0–14.9) | (4.1–12.8) | |||
| Medicaid | 16.0 | 15.2 | 23.8 | 10.8 | 19.8 | .729 | .937 |
| (8.3–23.7) | (4.0–26.4) | (8.8–38.8) | (2.1–19.4) | (7.7–31.8) | |||
| Total | 11.0 | 12.3 | 10.2 | 7.5 | 8.3 | .007b | .740 |
| (8.8–13.3) | (10.0–14.6) | (7.8–12.6) | (5.7–9.2) | (6.3–10.4) | |||
| 75 + years | |||||||
| Men | |||||||
| Quartile 1 | 6.4 | 6.3 | 9.1 | 6.8 | 1.2 | .032a | .039a |
| (1.0–11.8) | (0.5–12.1) | (2.7–15.4) | (1.5–12.1) | (0–3.4) | |||
| Quartile 2 | 11.7 | 7.6 | 9.1 | 8.9 | 11.4 | .808 | .394 |
| (3.7–19.6) | (1.2–14.0) | (2.1–16.1) | (3.2–14.7) | (5.8–17.1) | |||
| Quartile 3 | 19.1 | 12.7 | 4.7 | 8.0 | 5.9 | .011a | .313 |
| (8.1–30.0) | (5.0–20.3) | (0–10.8) | (1.8–14.2) | (1.9–9.8) | |||
| Quartile 4 | 11.5 | 11.7 | 8.2 | 14.4 | 18.1 | .160 | .282 |
| (3.0–19.9) | (5.4–18.0) | (3.3–13.0) | (6.8–22.0) | (9.4–26.7) | |||
| Medicaid | 16.9 | 0.4 | 3.4 | 3.8 | 17.7 | .709 | .030a |
| (0.0–34.1) | (0.3–6) | (0.0–10.2) | (0–11.5) | (5.0–30.4) | |||
| Total | 12.4 | 9.3 | 7.6 | 9.4 | 9.6 | .473 | .142 |
| (8.0–16.8) | (6.0–12.5) | (4.6–10.5) | (6.4–12.4) | (6.5–12.7) | |||
| Women | |||||||
| Quartile 1 | 8.2 | 15.4 | 7.5 | 8.9 | 9.1 | .735 | .750 |
| (3.5–12.9) | (6.7–24.0) | (3.0–12.1) | (4.2–13.5) | (4.2–14.2) | |||
| Quartile 2 | 17.6 | 13.7 | 4.8 | 10.3 | 5.7 | .005b | .400 |
| (10.4–24.7) | (6.3–21.0) | (1.6–8.0) | (3.5–17.2) | (2.0–9.3) | |||
| Quartile 3 | 11.2 | 11.1 | 10.3 | 5.9 | 9.3 | .448 | .687 |
| (5.0–17.4) | (4.8–17.3) | (5.2–15.4) | (0.7–11.1) | (4.1–14.5) | |||
| Quartile 4 | 10.9 | 10.5 | 8.4 | 7.1 | 7.1 | .206 | .861 |
| (4.8–17.0) | (3.7–17.2) | (3.5–13.2) | (3.0–11.1) | (3.2–11.1) | |||
| Medicaid | 17.6 | 19.4 | 14.7 | 11.0 | 17.8 | .614 | .397 |
| (9.5–25.8) | (7.9–30.5) | (8.0–21.5) | (4.7–17.3) | (9.5–26.1) | |||
| Total | 12.5 | 13.2 | 8.4 | 8.4 | 8.6 | .009b | .471 |
| (9.4–15.7) | (9.7–16.6) | (5.8–10.9) | (6.1–10.8) | (6.3–10.9) | |||
CI, confidence interval; CVD, cardiovascular disease.
p < .05.
p < .01.
For men aged 65–74 years, the proportion of the high CVD risk individuals decreased linearly among the quartile 1 group (p = .015), but remained unchanged for other quartile groups and this age group as a whole. Only the Medicaid group showed an increasing trend from 2012/2013, but the increase was not statistically significant. For women in the same age group, an inverse U-shaped polynomial trend (p = .031) was seen in the quartile 1 group and the highest proportion was found in 2010/2011. A significant decreasing linear trend was observed for the quartile 2 (p = .029) and for the entire group (p = .007).
For men aged 75 years and up, the risk trend for quartile 1 showed an inverse U-shaped pattern (p = .039); it spiked in 2012/2013, then sharply decreased in the following time periods. On the other hand, the Medicaid group showed a U-shaped pattern (p = .030), with the year 2010/2011 being the lowest. The quartile 3 showed a significant decreasing linear trend (p = .011). For women of this age groups, the proportion of the high CVD risk individuals showed a significant linear decreasing trend for the quartile 2 and for the entire group (p < .05).
The male group as a whole, the proportion of the high CVD adults among the Medicaid group were noticeably higher compared to other SEP groups in more recent years. In the female group as a whole, a strong socioeconomic gradient existed in each time period due to the fact that lower SEPs were associated with a higher proportion of the high CVD risk individuals, especially in the Medicaid groups.
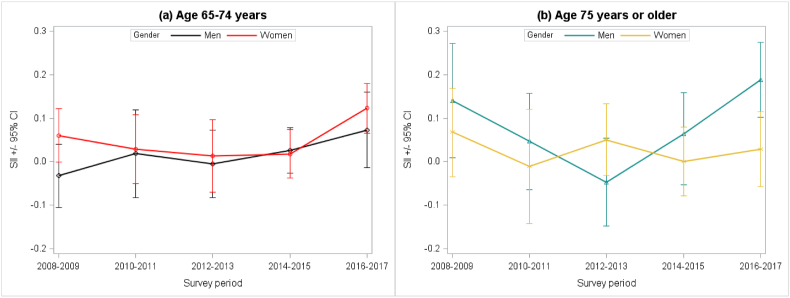
3.3. Trend in absolute disparities in high CVD risk among older adults from 2008 to 2017 (Table 3, Fig. 1)
Table 3.
Trend in absolute disparities in high CVD risk among older adults from 2008 to 2017.
| 2008–2009 |
2010–2011 |
2012–2013 |
2014–2015 |
2016–2017 |
p-trend |
||
|---|---|---|---|---|---|---|---|
| linear | polynomial | ||||||
| 65–74 years | |||||||
| Men | |||||||
| PD (95% CI) | |||||||
| Quartile1vs2 | −3.7 | 3.1 | −0.5 | 0.6 | 4.3 | .139 | .945 |
| (-9.9–2.5) | (-4.8 - 10.9) | (-7.7 – 6.7) | (-4.4 - 5.7) | (-1.2 - 9.8) | |||
| Quartile1vs3 | 0.9 | 3.4 | 5.0 | 2.9 | 4.0 | .625 | .652 |
| (-5.7 – 7.7) | (-4.2 - 10.9) | (-3.6 - 13.6) | (-2.6 - 8.3) | (-2.1 - 10.0) | |||
| Quartile1vs4 | −1.9 | 1.4 | 0.8 | 4.0 | 5.5 | .089 | .979 |
| (-8.3 - 4.5) | (-6.2 - 8.9) | (-7.3 – 8.8) | (-2.4 - 10.5) | (-0.8 - 11.8) | |||
| Quartile1vs Medicaid | −1.2 | −0.4 | −3.7 | 7.7 | 13.5 | .167 | .397 |
| (-10.4–7.9) | (-12.1–11.3) | (-15.0–7.6) | (-4.9 - 20.2) | (-8.3 - 35.3) | |||
| SIIa(95% CI) | -.032 | .019 | -.005 | .026 | .073 | .071 | .983 |
| (-.105–.040) | (-.082–.119) | (-.082–.072) | (-.026–.078) | (-.014–.160) | |||
| Women | |||||||
| PD (95% CI) | |||||||
| Quartile1vs2 | 5.9 | 0.8 | −0.8 | 0.4 | 2.9 | .695 | .096 |
| (0.3–11.5) | (-6.1 - 7.6) | (-7.8–6.1) | (-4.0 – 5.4) | (-1.7 - 7.6) | |||
| Quartile1vs3 | 6.9 | 2.5 | −1.6 | −0.3 | 7.1 | .739 | .007f |
| (1.1–12.8) | (-5.0 - 10.0) | (-8.0 - 4.9) | (-4.9–4.3) | (1.6–12.7) | |||
| Quartile1vs4 | 4.9 | −0.2 | −1.1 | 4.2 | 4.2 | .648 | .212 |
| (-1.4 – 11.3) | (-7.4 - 7.0) | (-7.8–5.5) | (-1.2 - 9.6) | (-1.2 – 9.5) | |||
| Quartile1vs Medicaid | 9.6 | 3.8 | 13.5 | 4.5 | 15.5 | .323 | .570 |
| (1.8–17.4) | (-8.2 - 15.8) | (-0.2 - 29.6) | (-4.5 – 13.5) | (3.0–27.9) | |||
| SIIb(95% CI) | .060 | .029 | .014 | .018 | .123 | .357 | .072 |
| (-.001–.122) | (-.050–.108) | (-.070–.097) | (-.038–.074) | (.066 - .180) | |||
| 75 + years | |||||||
| Men | |||||||
| PD (95% CI) | |||||||
| Quartile1vs2 | 5.3 | 1.3 | 0.3 | 2.2 | 10.2 | .085 | .072 |
| (-4.1 - 14.7) | (-0.7 - 9.8) | (-9.3 - 9.4) | (-5.4 – 9.7) | (4.2–16.2) | |||
| Quartile1vs3 | 12.7 | 6.3 | −4.3 | 1.2 | 4.7 | .624 | .032e |
| (0.5–24.8) | (-0.3 - 15.9) | (-12.9–4.2) | (-6.9 - 9.3) | (0.1–9.2) | |||
| Quartile1vs4 | 5.1 | 5.4 | −0.8 | 7.6 | 16.8 | .013e | .037e |
| (-0.5 - 14.8) | (-0.4 - 14.4) | (-8.8–7.1) | (-1.3 – 16.4) | (8.1–25.5) | |||
| Quartile1vs Medicaid | 10.5 | −5.9 | −5.6 | −3.0 | 16.5 | .327 | .008f |
| (-0.7 - 28.1) | (-12.0 to −0.1) | (-14.7–3.4) | (-11.9–5.9) | (1.7–31.3) | |||
| SIIc(95% CI) | .140 | .047 | -.047 | .064 | .188 | .078 | .001f |
| (.009 - .271) | (-.064–.157) | (-.148–.054) | (-.053–.159) | (.102 - .275) | |||
| Women | |||||||
| PD (95% CI) | |||||||
| Quartile1vs2 | 9.4 | −1.7 | −2.8 | 1.5 | −3.5 | .086 | .332 |
| (0.7–18.0) | (-13.1–9.8) | (-8.3 – 2.8) | (-6.7 - 9.6) | (-9.6–2.5) | |||
| Quartile1vs3 | 3.0 | −4.3 | 2.8 | −3.0 | 0.1 | .767 | .566 |
| (-5.3 – 11.2) | (-15.2–6.7) | (-3.5 - 9.0) | (-9.8–3.8) | (-7.1 - 7.3) | |||
| Quartile1vs4 | 2.7 | −4.9 | 0.8 | −1.9 | −0.2 | .548 | .660 |
| (-5.0 – 10.4) | (-15.9–6.1) | (-5.6 - 7.3) | (-8.1 - 4.4) | (-8.2 - 4.1) | |||
| Quartile1vs Medicaid | 9.4 | 4.1 | 7.2 | 2.2 | 8.6 | .861 | .444 |
| (-1.1 – 20.0) | (-11.9–20.0) | (-2.7 – 17.0) | (-6.2 - 10.5) | (-4.1 - 21.3) | |||
| SIId(95% CI) | .068 | -.010 | .050 | .001 | .029 | .843 | .643 |
| (-.034–.168) | (-.142–.120) | (-.032–.133) | (-.078–.080) | (-.057–.115) | |||
CI, confidence interval; CVD, cardiovascular disease; PD, prevalence difference; SII, slope index of inequality.
Adjusted for regular physical activity, weight control, and regular health check-up.
Adjusted for activity limitation, weight control, and regular health check-up.
Adjusted for activity limitation and geographical location.
Adjusted for regular physical activity, weight control, and geographical location.
p < .05.
p < .01.
Fig. 1.
Trends in slope index of inequality over time by age group and gender.
For men aged 65–74 years, no statistically significant trends were found for the PDs. However, although not statistically significant, the absolute magnitude of income disparities for high CVD risk measured by SII increased over time peaking in 2016/2017. For women of this age group, the PDs between quartiles 1 vs 2, quartiles 1 vs 3, quartiles 1 vs 4, and SII showed U-shaped trends; however, only the risk trend between quartiles 1 vs 3 was significant (p = .007).
For men aged 75 years and up, the PDs between quartiles 1 vs 3, quartiles 1 vs 4 and quartile 1 vs Medicaid followed significant U-shaped trends over time (p < .05). SII also showed a significant U-shaped trend (p = .001), peaking in 2016/2017. Notably, the SII value in the 2016/2017 period was significantly higher when compared to other years. For women in this age group, no specific trends were found for PDs or SII; however, results indicated a constant absolute health gap exists between individuals at the lowest and highest SEP ranks.
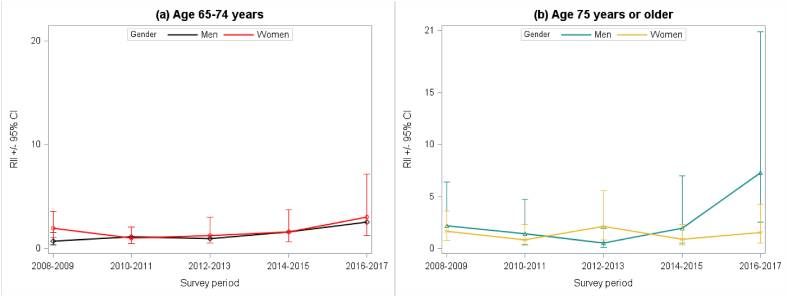
3.4. Trend in relative disparities in high CVD risk among older adults from 2009 to 2017 (Table 4, Fig. 2)
Table 4.
Trend in relative disparities in high CVD risk among older adults from 2008 to 2017.
| 2008–2009 |
2010–2011 |
2012–2013 |
2014–2015 |
2016–2017 |
p-trend |
||
|---|---|---|---|---|---|---|---|
| linear | polynomial | ||||||
| 65–74 years | |||||||
| Men | |||||||
| RR (95% CI) | |||||||
| Quartile1vs2 | 0.67 | 1.34 | 0.95 | 1.11 | 1.84 | .115 | .849 |
| (0.33–1.35) | (0.62–2.90) | (0.47–1.91) | (0.49–2.50) | (0.85–3.97) | |||
| Quartile1vs3 | 1.09 | 1.37 | 1.47 | 1.48 | 1.77 | .340 | .875 |
| (0.06–1.95) | (0.65–2.90) | (0.75–2.92) | (0.69–3.18) | (0.76–4.14) | |||
| Quartile1vs4 | 0.83 | 1.10 | 1.07 | 1.68 | 2.07 | .809 | .078 |
| (0.44–1.57) | (1.08–1.11) | (0.52–2.24) | (0.78–3.61) | (0.93–4.62) | |||
| Quartile1vs Medicaid | 0.89 | 0.96 | 0.65 | 2.29 | 3.62 | .075 | .372 |
| (0.36–2.21) | (0.25–3.64) | (0.14–2.95) | (0.79–6.62) | (0.97–13.57) | |||
| RIIa(95% CI) | 0.74 | 1.13 | 0.95 | 1.61 | 2.58 | .069 | .793 |
| (0.35–1.57) | (0.47–2.72) | (0.41–2.19) | (0.66–3.92) | (0.97–6.86) | |||
| Women | |||||||
| RR (95% CI) | |||||||
| Quartile1vs2 | 1.93 | 1.07 | 0.92 | 1.07 | 1.68 | .767 | .091 |
| (1.04–3.60) | (0.59–1.91) | (0.46–1.86) | (0.50–2.28) | (0.71–3.96) | |||
| Quartile1vs3 | 2.09 | 1.22 | 0.85 | 0.95 | 2.69 | .666 | .009f |
| (1.12–3.90) | (0.67–2.21) | (0.43–1.67) | (0.45–2.02) | (1.17–6.00) | |||
| Quartile1vs4 | 1.78 | 0.98 | 0.89 | 1.68 | 1.96 | .575 | .111 |
| (0.89–3.54) | (0.52–1.85) | (0.45–1.76) | (0.78–3.61) | (0.81–4.71) | |||
| Quartile1vs Medicaid | 2.51 | 1.33 | 2.32 | 1.71 | 4.58 | .180 | .183 |
| (1.29–4.88) | (0.57–3.09) | (1.03–5.23) | (0.68–4.34) | (1.78–11.76) | |||
| RIIb(95% CI) | 1.95 | 1.03 | 1.25 | 1.60 | 3.03 | .284 | .008f |
| (1.07–3.57) | (0.50–2.11) | (0.52–3.01) | (0.69–3.74) | (1.28–7.16) | |||
| 75 + years | |||||||
| Men | |||||||
| RR (95% CI) | |||||||
| Quartile1vs2 | 1.82 | 1.20 | 1.00 | 1.32 | 9.28 | .084 | .028e |
| (0.64–5.24) | (0.36–4.08) | (0.36–2.82) | (0.50–3.49) | (1.51–57.00) | |||
| Quartile1vs3 | 2.98 | 2.11 | 0.52 | 1.18 | 4.77 | .731 | .025e |
| (1.08–8.26) | (2.04–2.17) | (0.12–2.21) | (0.39–3.50) | (0.75–30.24) | |||
| Quartile1vs4 | 1.79 | 2.00 | 0.90 | 2.11 | 14.65 | .011e | .019e |
| (0.60–5.34) | (0.68–5.91) | (0.36–2.26) | (0.85–5.19) | (2.47–86.74) | |||
| Quartile1vs Medicaid | 2.65 | 0.07 | 0.38 | 0.55 | 14.36 | .230 | .003f |
| (0.71–9.94) | (0.01–0.69) | (0.05–2.99) | (0.07–4.42) | (2.13–96.77) | |||
| RIIc(95% CI) | 2.21 | 1.44 | 0.54 | 1.95 | 7.32 | .046e | .009f |
| (0.77–6.39) | (0.43–4.77) | (0.15–1.95) | (0.54–7.03) | (2.57–20.9) | |||
| Women | |||||||
| RR (95% CI) | |||||||
| Quartile1vs2 | 2.14 | 0.89 | 0.64 | 1.17 | 0.62 | .062 | .431 |
| (1.06–4.31) | (0.41–1.95) | (0.26–1.55) | (0.51–2.68) | (0.27–1.40) | |||
| Quartile1vs3 | 1.36 | 0.72 | 1.37 | 0.66 | 1.01 | .742 | .613 |
| (0.59–3.13) | (0.32–1.63) | (0.68–2.74) | (0.24–1.80) | (0.46–2.20) | |||
| Quartile1vs4 | 1.33 | 0.68 | 1.11 | 0.80 | 0.78 | .478 | .734 |
| (0.60–2.94) | (0.29–1.60) | (0.49–2.50) | (0.36–1.75) | (0.37–1.64) | |||
| Quartile1vs Medicaid | 2.15 | 1.27 | 1.95 | 1.24 | 1.93 | .928 | .479 |
| (0.98–4.7) | (0.5–3.11) | (0.84–4.51) | (0.55–2.8) | (0.83–4.53) | |||
| RIId(95% CI) | 1.67 | 0.83 | 2.15 | 0.91 | 1.56 | .972 | .667 |
| (0.77–3.65) | (0.29–2.34) | (0.83–5.59) | (0.36–2.31) | (0.57–4.30) | |||
CI, confidence interval; CVD, cardiovascular disease; RR, risk ratio; RII, relative index of inequality.
Adjusted for regular physical activity, weight control, and regular health check-up.
Adjusted for activity limitation, weight control, and regular health check-up.
Adjusted for activity limitation and geographical location.
Adjusted for regular physical activity, weight control, and geographical location.
p < .05.
p < .01.
Fig. 2.
Trends in relative index of inequality over time by age group and gender.
A similar pattern was observed based on both the absolute and the relative measures for men aged 65–74 years; no specific trend was observed within the RRs for high CVD risk among different SEP groups. In addition, the relative magnitude of disparities measured by RII tend to increase over time, although this was not significant according to the trend analysis. For women aged 65–74 years, the RRs for the quartiles 1 vs 3 and RII revealed strong U-shaped trends (p < .05). The highest RII was observed in 2016/2017 for both genders.
For men aged 75 years and up, the RRs showed a significant U-shaped trend in all between-group comparisons (p < .05), all peaking in 2016/2017. The RII also showed a significant U-shaped trend (p = .009) with the value increasing significantly in recent years. On the other hand, the women of this age group showed no statistically significant trend. However, it is noteworthy that the highest RRs were reported between the quartile 1 and Medicaid groups over the analysis time periods.
4. Discussion
4.1. The failure to achieve an equitable reduction in high CVD risk
This study described the 10-year trends of income disparities in CVD risk among older Koreans. In general, the proportion of the older adults with a high-CVD risk followed a declining trend over time across all age and gender groups. The large decline of high CVD risk individuals in more affluent individuals seem to contribute significantly to this trend. Indeed, the proportion of the high CVD risk adults increased in the lower-income groups such as Quartile 4 and Medicaid. These results are consistent with the findings of recent trend studies in the US (Beckman et al., 2017; Odutayo et al., 2017; Valero-Elizondo et al., 2018); they commonly reported that the percentage of adults with high CVD risk declined in the high-income stratum but remained unchanged for the lower income groups despite the overall improvements in controlling CVD risk factors.
National CVD management programs and advances in cardiovascular care may have contributed to the overall decrease of the high CVD risk population seen in the analysis. However, our findings indicate that such efforts may have not equally benefited older adults of all socioeconomic statuses. In fact, a prior study reported that many lower-income Koreans of older age have been excluded from national health plans due to limited access to public resources and insufficient information (Cho & Chu, 2016). Although national programs such as the Korean National Cardio-Cerebrovascular Disease Plan (“KCDC,” n.d.) has worked to provide accessible health care for older adults, additional progress is needed.
In addition, our findings on inequitable distribution in CVD risk may help evaluate the Korean healthcare system, which has been structured in a way that substantially positions older impoverished adults at a disadvantage. The objective of the Korean government has been to provide universal coverage at a low cost by excluding certain diseases and diagnostic procedures and minimizing select benefits (Yoon, 2013). As such, KNHI offers relatively broad but shallow protection for illnesses. This restricts access for those needing treatment for chronic diseases and those unable to afford out-of-pocket costs (Lee & Shaw., 2014). The system also poses an additional barrier for the poor since copayments do not depend on income (Yoon, 2013), resulting an unequal economic health burden among older adults, as can be observed in our analysis.
Several political efforts have attempted to ensure equal provision of cardiovascular care. For example, CVD cost-sharing policies have been altered twice within the past 15 years. In September 2005 (Policy 1), the individual share of costs for CVD prevention were reduced from 20% to 10%, and January 2010 (Policy 2) they were further reduced from 10% → 5%. However, according to Jang (2018), these efforts produced little change in most income quintiles, except for a significant CVD mortality risk reduction only in the 1st income quintile during Policy 2. Separate from health insurance, the government also introduced a new social insurance scheme for long-term care in 2008 aimed at easing burdens on the aging population. However, this initiative yielded minimal improvements in healthcare access for poorer groups primarily due to low initiative in local governments to ensure provision of long-term care and lack of care staff and facilities in disadvantaged areas (Chon, 2012; Kwon, 2008).
4.2. The high burden of CVD risk for the medicaid group
Although the trends vary by age and gender, a clear socioeconomic gradient in CVD risk was discernible for every survey period, with an exceptionally high burden for the Medicaid group. Unlike the situation in the United States, Medicaid in Korea should provide the same service as KNHI at minimal cost because the two are officially in the same healthcare benefit bracket. However, chronic underfunding and delayed payments to healthcare providers have led to discrimination against Medicaid patients (Jang et al., 2015). As such, patients covered by Medicaid suffer from poorer healthcare than those covered by KNHI, and to this end, previous reports also revealed that Medicaid patients have lower appointment rates, fewer medical services available, and longer wait times for medical care (Bae et al., 2016; Jang et al., 2015). Although our results do not establish a causal relationship between such circumstances and the widening national disparity in cardiovascular health, they do indicate that more institutional support is needed to improve the cardiovascular health of Medicaid recipients.
4.3. An increasing absolute and relative disparities in high CVD risk
Both the absolute and relative disparities among younger-old men showed an increasing linear trend over time although not it was not statistically significant. This result is partially in agreement with the study of Yang et al. (2015), which reported that both types of disparities in predicted 10-year CVD risk persisted from 2009 when examined using similar methods. Previous studies have reported that income disparities for major CVD risk factors were either decreased (Shin & Kang, 2018) or remained stable (Kim et al., 2017) among Korean men aged 25–64 years. These contrasting observations prompt the need to carefully examine the health policies to identify factors that may have led to the health disparities in older adults.
The overall rates of high CVD risk have declined in younger-old women. However, their relative disparity decreased in 2008–2011 and then has increased from 2012. Although further investigation is needed to explain this polynomial trend, it should be noted that the relative health gap between higher-income groups and the Medicaid group was still evident even in 2008–2011 where RII showed a decreasing trend (RII > 1; 2008–2017). Indeed, Moon et al. (2019) found CVD risk in female Medicaid recipients aged over 60 years was consistently higher during 2008–2012 when compared to health insurance subscribers of those with the same demographics (Moon et al., 2019).
Among older-old men, both the absolute and relative income disparities in CVD risk have drastically increased in recent years (2016/2017: SII > 0.18, RII > 7), more so than for any of the other groups. The increasing income inequality among older adults has recently been a great concern in Korea. Despite the government efforts to reduce poverty in older populations (e.g., the Basic Pension Scheme [2014]; Yoon, 2013), economic equity has not been achieved; according to Statistics Korea (2017), the income quintile share ratio and disposable income Gini coefficient, which had begun to decrease in early 2012, dramatically increased from 2015 among those aged over 66. Although the temporal relationships between income inequality and disparities in cardiovascular health are complex, these sobering statistics warn that health policies should treat unequal income distribution seriously to improve cardiovascular health among the low-income, older-old male group. This is of particular importance in Asian countries, where rapid aging accompanies a significant rise in income inequality due to the high elderly poverty rate (Kang & Rudolf, 2016; Shirahase, 2015).
On the other hand, no specific disparity trend was found among older-old women. These results may be due to differences in healthcare utilization between men and women in Korea. Although oldest-old women with less severe conditions use more medical resources than men with the same conditions, they tend to use intensive services less (Noh et al., 2017). In rural areas, oldest-old women have higher untreated rates for acute diseases, fewer hospital treatments, and shorter hospital stays (Shin et al., 2009). Accordingly, while they are already in the weakest position in healthcare utilization, insurance status as a KNHI versus Medicaid beneficiary or income bracket may have less of an impact on the health of the oldest-old women. However, the hypothesis of gender-associated discrepancies should be validated with further research.
4.4. Methodological aspects of the study
For younger-old women, although both types of disparity notably exhibited a similar trend, the change in the absolute disparity was not significant. Changes in population-level and social inequalities related to the associated health risks can manifest differently depending on the analysis methods – i.e., whether the absolute or relative terms are considered (Houweling et al., 2007). Previous research has shown that absolute inequalities decrease more substantially than relative inequalities under a wider range of conditions (Mackenbach et al., 2015); in the case of declining overall rates, relative inequalities can increase while absolute inequalities do not. This explains the results of this study where the change in RII was significant while both RII and SII showed a similar increasing trend and the overall rates of high CVD risk declined. Accordingly, it is important to consider both the absolute and relative terms when examining the trends in inequality over time.
4.5. Limitations and strengths
This study has several limitations. First, the datasets analyzed in this study are derived from periodic cross-sectional surveys. Therefore, it was not feasible to analyze the trajectory of high CVD risk, which would require longitudinal follow-up data. Second, the intervals between surveys were not annually based, which may have potentially biased the results for time trends. Third, the monthly income variable used in this study may not accurately reflect the true economic status of the sample, as it was taken as an estimated average for the given year. Lastly, the single imputation used in this study may reduce data variability, resulting in the underestimation of variances and standard errors.
Despite these concerns, one of this study's strengths was its use of population-based data, which reduces the likelihood of selection bias. Moreover, this study considered both absolute and relative disparities, which show a more complete picture of the disparity trends. This study also addressed disparities in CVD risk through the cardiovascular risk model, which is widely accepted as a primary preventive tool for CVD. The findings of this study will provide crucial insights into designing early interventions that effectively address socioeconomic disparities in cardiovascular health.
Interpretation of the main findings of this study needs caution. Few participants were covered by Medicaid (upward 5% of the Korean population), which hinders the statistical power of some analyses. For instance, small sample data (e.g., only 87 participants in the Medicaid group among younger-old men sampled between the years 2012 and 2013) led to a wide confidence interval. As of yet, the number of participants with a high CVD risk in these groups was not insignificant, and subgroup analysis produced consistent results, which prompted the belief that these findings are relatively reliable.
5. Conclusion
This study investigated time trends of income disparities in CVD risk among Korean older adults from 2008 to 2017. While results showed that the proportion of high CVD risk individuals generally declined over time, this can be attributed to the large decrease in more affluent groups. We also found overall strong evidence of persisting and increasing absolute and relative disparities in high CVD risk across groups, with a worsening trend for Medicaid recipients, especially in older-old men.
Our results have global implications, especially for countries with increasing income inequality, including Korea. First, the failure to achieve an equitable reduction in high CVD risk highlights the need to improve CVD risk management services offered to the economically disadvantaged. Second, it is important to improve overall accessibility to social and healthcare resources for older adults on Medicaid to address their CVD burden. Lastly, social policies need to pay more attention to alleviating poverty in older adults especially among the older-old men to reduce income-related health disparities.
Ethical considerations
Korean National Health and Nutrition Examination Survey is a free public data which do not include personal information. However, this study received the institutional review board approval from the institution where the corresponding author was affiliated (protocol number: Pro00103112).
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
We declare no conflicts of interest.
Acknowledgements
none.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2020.100682.
Contributor Information
Chiyoung Lee, Email: clee33@uw.edu.
Qing Yang, Email: qing.yang@duke.edu.
Eun-Ok Im, Email: eun.ok.im@emory.edu.
Eleanor Schildwachter McConnell, Email: eleanor.mcconnell@duke.edu.
Sin-Ho Jung, Email: sinho.jung@duke.edu.
Hyeoneui Kim, Email: hyeoneui.kim@duke.edu.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- KCDC (n.d.). Program for prevention and management for a cardio-cerebrovascular disease. http://www.cdc.go.kr/contents.es?mid=a30335000000 (Accessed May 7, 2020).
- Anderson K.M., Odell P.M., Wilson P.W., Kannel W.B. Cardiovascular disease risk profiles. American Heart Journal. 1991;121(1):293–298. doi: 10.1016/0002-8703(91)90861-B. [DOI] [PubMed] [Google Scholar]
- Backholer K., Peters S.A., Bots S.H., Peeters A., Huxley R.R., Woodward M. Sex differences in the relationship between socioeconomic status and cardiovascular disease: A systematic review and meta-analysis. Journal of Epidemiology & Community Health. 2017;71(6):550–557. doi: 10.1136/jech-2016-207890. [DOI] [PubMed] [Google Scholar]
- Bae S.H., Choi E.O., Lee I.Y. Health status and health service utilization: Barriers and facilitators for Korea Medicaid beneficiaries. Journal of Korean Biological Nursing Science. 2016;18(3):144–152. doi: 10.7586/jkbns.2016.18.3.144. [DOI] [Google Scholar]
- Beckman A.L., Herrin J., Nasir K., Desai N.R., Spatz E.S. Trends in cardiovascular health of US adults by income, 2005-2014. JAMA Cardiology. 2017;2(7):814–816. doi: 10.1001/jamacardio.2017.1654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho H.W., Chu C. Evaluation of self-assessment in cardiovascular diseases among Korean older population. Osong Public Health and Research Perspectives. 2016;7(2):75–76. doi: 10.1016/j.phrp.2016.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi J.W., Choi J.W., Kim J.H., Yoo K.B., Park E.C. Association between chronic disease and catastrophic health expenditure in Korea. BMC Health Services Research. 2015;15(1):26. doi: 10.1186/s12913-014-0675-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chon Y. Long-term care reform in Korea: Lessons from the introduction of asia's second long-term care insurance system. Asia Pacific Journal of Social Work and Development. 2012;22(4):219–227. doi: 10.1080/02185385.2012.726422. [DOI] [Google Scholar]
- Coke L.A. Eliminating cardiovascular health disparities: There has been progress, but there is more to do! Journal of Cardiovascular Nursing. 2018;33(6):506–508. doi: 10.1097/JCN.0000000000000529. [DOI] [PubMed] [Google Scholar]
- Donaldson G.W. Ridit scores for analysis and interpretation of ordinal pain data. European Journal of Pain. 1998;2(3):221–227. doi: 10.1016/s1090-3801(98)90018-0. [DOI] [PubMed] [Google Scholar]
- Ernstsen L., Strand B.H., Nilsen S.M., Espnes G.A., Krokstad S. Trends in absolute and relative educational inequalities in four modifiable ischaemic heart disease risk factors: Repeated cross-sectional surveys from the nord-trøndelag health study (HUNT) 1984–2008. BMC Public Health. 2012;12(1):266. doi: 10.1186/1471-2458-12-266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houweling T.A., Kunst A.E., Huisman M., Mackenbach J.P. Using relative and absolute measures for monitoring health inequalities: Experiences from cross-national analyses on maternal and child health. International Journal for Equity in Health. 2007;6(1):15. doi: 10.1186/1475-9276-6-15. doi: 10.1186/1475-9276-6-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang S.H. Dissertation, Seoul National University Graduate School; 2018. The effect of cost sharing on healthcare utilization and health: A focus on cardiovascular disease. [Google Scholar]
- Jang S.I., Yi S.W., Sull J.W., Park E.C., Kim J.H., Ohrr H. Association between all-cause mortality and insurance status transition among the elderly population in a rural area in Korea: Kangwha Cohort Study. Health Policy. 2015;119(5):680–687. doi: 10.1016/j.healthpol.2014.10.012. [DOI] [PubMed] [Google Scholar]
- Jee S.H., Batty G.D., Jang Y., Oh D.J., Oh B.H., Lee S.H., Mok Y. The Korean heart study: Rationale, objectives, protocol, and preliminary results for a new prospective cohort study of 430,920 men and women. European Journal of Preventive Cardiology. 2014;21(12):1484–1492. doi: 10.1177/2047487313497602. [DOI] [PubMed] [Google Scholar]
- Jee S.H., Jang Y., Oh D.J., Oh B.H., Lee S.H., Park S.W., Yun Y.D. A coronary heart disease prediction model: The Korean heart study. BMJ Open. 2014;4(5) doi: 10.1136/bmjopen-2014-005025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeon B., Kwon S. Health and long-term care systems for older people in the Republic of Korea: Policy challenges and lessons. Health Systems & Reform. 2017;3(3):214–223. doi: 10.1080/23288604.2017.1345052. [DOI] [PubMed] [Google Scholar]
- Kang M.Y., Hong Y.C. Crossover effect of spouse weekly working hours on estimated 10-years risk of cardiovascular disease. PloS One. 2017;12(8) doi: 10.1371/journal.pone.0182010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang S.J., Rudolf R. Rising or falling inequality in Korea? Population aging and generational trends. Singapore Economic Review. 2016;61(5):1550089. doi: 10.1142/S0217590815500897. [DOI] [Google Scholar]
- Khang Y.H., Lee S.I. Health inequalities policy in Korea: Current status and future challenges. Journal of Korean Medical Science. 2012;27(Suppl):S33–S40. doi: 10.3346/jkms.2012.27.S.S33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khang Y.H., Lynch J.W., Kaplan G.A. Health inequalities in Korea: Age-and sex-specific educational differences in the 10 leading causes of death. International Journal of Epidemiology. 2004;33(2):299–308. doi: 10.1093/ije/dyg244. [DOI] [PubMed] [Google Scholar]
- Kim Y.J., Lee J.S., Park J., Choi D.S., Kim D.M., Lee K.H., Lee J. Trends in socioeconomic inequalities in five major risk factors for cardiovascular disease in the Korean population: A cross-sectional study using data from the Korea national health and nutrition examination survey, 2001–2014. BMJ Open. 2017;7(5) doi: 10.1136/bmjopen-2016-014070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Y., Oh J., Jha A. Contribution of hospital mortality variations to socioeconomic disparities in in-hospital mortality. BMJ Quality and Safety. 2014;23(9):741–748. doi: 10.1136/bmjqs2013-002744. [DOI] [PubMed] [Google Scholar]
- Kweon S., Kim Y., Jang M.J., Kim Y., Kim K., Choi S., Oh K. Data resource profile: The Korea national health and nutrition examination survey (KNHANES) International Journal of Epidemiology. 2014;43(1):69–77. doi: 10.1093/ije/dyt228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwon S. Future of long-term care financing for the elderly in Korea. Journal of Aging & Social Policy. 2008;20(1):119–136. doi: 10.1300/J031v20n01_07. [DOI] [PubMed] [Google Scholar]
- Kwon S. Thirty years of national health insurance in South Korea: Lessons for achieving universal health care coverage. Health Policy and Planning. 2009;24(1):63–71. doi: 10.1093/heapol/czn037. [DOI] [PubMed] [Google Scholar]
- Lee J., Cho S.I., Chun H., Jung-Choi K., Kang M., Jang S.N. Life course indices for social determinants of self-rated health trajectory in Korean elderly. Archives of Gerontology and Geriatrics. 2017;70:186–194. doi: 10.1016/j.archger.2017.02.003. [DOI] [PubMed] [Google Scholar]
- Lee H., Cho J., Shin D.W., Lee S.P., Hwang S.S., Oh J., Cho B. Association of cardiovascular health screening with mortality, clinical outcomes, and health care cost: A nationwide cohort study. Preventive Medicine. 2015;70:19–25. doi: 10.1016/j.ypmed.2014.11.007. [DOI] [PubMed] [Google Scholar]
- Lee D.W., Hong Y.C., Min K.B., Kim T.S., Kim M.S., Kang M.Y. The effect of long working hours on 10-year risk of coronary heart disease and stroke in the Korean population: The Korea national health and nutrition examination survey (KNHANES), 2007 to 2013. Annals of Occupational and Environmental Medicine. 2016;28(1):64. doi: 10.1186/s40557-016-0149-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee C.Y., Im E.O. Socioeconomic disparities in cardiovascular health in South Korea: A systematic review. Journal of Cardiovascular Nursing. 2019 doi: 10.1097/JCN.0000000000000624. [DOI] [PubMed] [Google Scholar]
- Lee W.Y., Shaw I. The impact of out-of-pocket payments on health care inequity: The case of national health insurance in South Korea. International Journal of Environmental Research and Public Health. 2014;11(7):7304–7318. doi: 10.3390/ijerph110707304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackenbach J.P., Kulhánová I., Menvielle G., Bopp M., Borrell C., Costa G., Leinsalu M. Trends in inequalities in premature mortality: A study of 3.2 million deaths in 13 European countries. Journal of Epidemiology & Community Health. 2015;69(3):207–217. doi: 10.1136/jech-2014-204319. [DOI] [PubMed] [Google Scholar]
- Martinson M.L., Teitler J.O., Plaza R., Reichman N.E. Income disparities in cardiovascular health across the lifespan. SSM-population health. 2016;2:904–913. doi: 10.1016/j.ssmph.2016.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills K.T., Bundy J.D., Kelly T.N., Reed J.E., Kearney P.M., Reynolds K., He J. Global disparities of hypertension prevalence and control: A systematic analysis of population-based studies from 90 countries. Circulation. 2016;134(6):441–450. doi: 10.1161/CIRCULATIONAHA.115.018912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moon S.H., Seo H.J., Lee D.Y., Kim S.M., Park J.M. Associations among health insurance type, cardiovascular risk factors, and the risk of dementia: A prospective cohort study in Korea. International Journal of Environmental Research and Public Health. 2019;16(14):2616. doi: 10.3390/ijerph16142616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreno-Betancur M., Latouche A., Menvielle G., Kunst A.E., Rey G. Relative index of inequality and slope index of inequality: A structured regression framework for estimation. Epidemiology. 2015;26(4):518–527. doi: 10.1097/EDE.0000000000000311. [DOI] [PubMed] [Google Scholar]
- Noh J.W., Kim K.B., Park H., Kwon Y.D. Gender differences in outpatient utilization: A pooled analysis of data from the Korea health panel. Journal of Women's Health. 2017;26(2):178–185. doi: 10.1089/jwh.2016.5771. [DOI] [PubMed] [Google Scholar]
- Odutayo A., Gill P., Shepherd S., Akingbade A., Hopewell S., Tennankore K., Emdin C.A. Income disparities in absolute cardiovascular risk and cardiovascular risk factors in the United States, 1999-2014. JAMA Cardiology. 2017;2(7):782–790. doi: 10.1001/jamacardio.2017.1658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oh J.Y., Yang Y.J., Kim B.S., Kang J.H. Validity and reliability of Korean version of international physical activity Questionnaire (IPAQ) short form. Journal of the Korean Academy of Family Medicine. 2007;28(7):532–541. [Google Scholar]
- Pahigiannis K., Thompson-Paul A.M., Barfield W., Ochiai E., Loustalot F., Shero S., Hong Y. Progress toward improved cardiovascular health in the United States: Healthy People 2020 heart disease and stroke objectives. Circulation. 2019;139(16):1957–1973. doi: 10.1161/CIRCULATIONAHA.118.035408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park E.J., Cho S.I., Jang S.N. Poor health in the Korean older population: Age effect or adverse socioeconomic position. Archives of Gerontology and Geriatrics. 2012;55(3):599–604. doi: 10.1016/j.archger.2012.06.001. [DOI] [PubMed] [Google Scholar]
- Shin H.Y., Kang H.T. Recent trends in blood pressure according to economic status: Korean national health and nutrition examination survey from 2005 to 2015. Asia-Pacific Journal of Public Health. 2018;30(3):266–275. doi: 10.1177/1010539518761482. [DOI] [PubMed] [Google Scholar]
- Shin H.C., Kang J.Y., Park W.S., Kim S.A. Health status and medical utilization of women in rural area. Journal of Agricultural Medicine and Community Health. 2009;34(1):67–75. doi: 10.5393/JAMCH.2009.34.1.067. [DOI] [Google Scholar]
- Shirahase S. Income inequality among older people in rapidly aging Japan. Research in Social Stratification and Mobility. 2015;41:1–10. doi: 10.1016/j.rssm.2015.03.001. [DOI] [Google Scholar]
- Statistics Korea . 2017. Income index.http://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1L6E003&vw_cd=MT_OTITLE&list_id=G_A3&scrId=&seqNo=&lang_mode=ko&obj_var_id=&itm_id=&conn_path=E1 [Google Scholar]
- OECD (n.d.). Adjusting household incomes: equivalence scales. Retrieved from http://www.oecd.org/els/soc/OECD-Note-EquivalenceScales.pdf (Accessed May 27, 2020).
- Office of Disease Prevention and Health Promotion . 2020. Healthy People 2020 heart disease and stroke topic area. Healthy People 2020. U.S. Department of Health and Human Services.https://www.healthypeople.gov/2020/topics-objectives/topic/heart-disease-and-stroke [Google Scholar]
- Valero-Elizondo J., Hong J.C., Spatz E.S., Salami J.A., Desai N.R., Rana J.S., Nasir K. Persistent socioeconomic disparities in cardiovascular risk factors and health in the United States: Medical Expenditure Panel Survey 2002–2013. Atherosclerosis. 2018;269:301–305. doi: 10.1016/j.atherosclerosis.2017.12.014. [DOI] [PubMed] [Google Scholar]
- Yang Q., Zhong Y., Ritchey M., Loustalot F., Hong Y., Merritt R., Bowman B.A. Predicted 10-year risk of developing cardiovascular disease at the state level in the US. American Journal of Preventive Medicine. 2015;48(1):58–69. doi: 10.1016/j.amepre.2014.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon H.S. Korea: Balancing economic growth and social protection for older adults. The Gerontologist. 2013;53(3):361–368. doi: 10.1093/geront/gnt018. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.