Abstract
Background/Aim: Isolated fractures of the lesser trochanter (LT) of adults are rare and most of them are pathologic fractures due to an underlying malignancy. The aim of our study was to provide comprehensive information on the epidemiology, etiology, diagnostic approach, and treatment algorithm of adult LT fractures. Patients and Methods: We present the cases of six patients who were treated for isolated LT fractures between November 2010 and May 2019. A literature review was performed to identify adult LT fracture cases in previous studies. Results: In two patients, the LT fracture was the first manifestation of the underlying tumors. Through a literature review, we identified 32 adults with isolated LT fractures. Among these, 27 were pathologic fractures. In 11 pathologic fractures, LT avulsion was the first manifestation of malignancy. Conclusion: Metastasis and the first manifestation of an underlying malignancy should be suspected in adult patients with isolated LT fracture. A stepwise approach can prevent misdiagnosis and offer rational treatment modality.
Keywords: Fracture, neoplasm metastasis, pathologic fracture
Isolated fracture of the lesser trochanter (LT) is rare (1), and has been known to have bimodal age-distribution (2,3). The bimodality of the age-incidence has been ascribed to the subgroups with different etiologies. Avulsion fractures of the lesser trochanter occur in adolescents prior to the fusion of the apophysis due to sudden forceful contraction of iliopsoas muscle during vigorous movements such as jumping or sprinting (4).
At the age of 18, the LT apophysis is fused. After this age, most avulsions of the lesser trochanter are pathological fractures due to malignant lesions, and occur without overt trauma (5-10). Sometimes, LT avulsion is the presenting symptom before the diagnosis of underlying tumor. For accurate diagnosis and appropriate treatment of this pathologic fracture in adults, thorough understanding of this injury is essential.
Patients with malignancy are treated with surgery, chemotherapy or irradiation depending on the pathologic nature and the stage of underlying tumor. The surgical treatment includes extensive resection of tumor with reconstruction using tumor prosthesis and prophylactic intramedullary nailing (2,3,11).
Although, cases of isolated LT fracture have been reported in the literature, there has been no study, which comprehensively elaborates on the patient demographics, diagnostic approach and treatment guidelines.
Therefore, the purposes of our study were 1) to present six isolated avulsion fractures of the lesser trochanter, 2) to characterize the fracture through systematic review of previous studies and our cases and 3) to establish a systematic algorithm for the diagnosis and treatment of isolated avulsion of the lesser trochanter in adult patients.
Patients and Methods
From November 2010 to May 2019 seven patients were diagnosed with isolated avulsion fracture of the LT at the author’s hospital. A 15-year old male who sustained traumatic LT avulsion during playing soccer was excluded from the study. The remaining six patients, who had pathological LT avulsion, were included.
We reviewed medical records of these six patients in terms of age, gender, mechanism of injury, clinical manifestation, degree of displacement, underlying malignancy, and treatment of LT fracture. The local recurrence, stem loosening, wear and osteolysis were evaluated on serial x-rays.
This study was approved by our institutional review board, and informed consent was waived (IRB No. B-1910/568-119).
Literature search for LT fractures in adult patients. A literature search was performed using the MEDLINE through PubMed, EMBASE, the Cochrane Library, and Scopus databases, as recommended by PRISMA guidelines. Two of the authors independently conducted the search process in November 2019. The search was performed using the following key terms in the title and abstract: (“avulsion fracture”[Title/Abstract] OR “avulsion”[Title/Abstract]) OR “traction”[Title/Abstract]) AND “lesser trochanter”[Title/Abstract]) or (“avulsion fracture”[Title/Abstract] OR “avulsion”[Title/Abstract]) OR “traction”[Title/Abstract]) AND “trochanter minor”[Title/Abstract]).
There were no restrictions to the language and the date of publication. Inclusion criteria were case report/series on isolated LT avulsion fracture in adult. Duplications, animal studies, reviews, textbooks, instructional course lectures and studies not including contents of isolated LT fracture or enrolling only childhood/adolescent LT fractures were excluded. Studies without available abstracts or full texts were also excluded. The two reviewers independently reviewed the titles and abstracts from the search results. Subsequently, full-texts were reviewed to determine whether to be included in the study. Through manual search, additional papers concerning LT avulsion fracture of adults were included to the study.
The following information was collected from the included articles: age, gender, pathologic fracture or non-pathologic fracture, primary tumor or metastasis, primary focus in case of metastasis, whether the patient was previously diagnosed with malignancy or the disease first manifested as a pathologic fracture.
Results
Case presentation. All six patients were male and their mean age at the time of LT fracture diagnosis was 63 years (range=56-79 years) (Table I).
Table I. Characteristics of six patients with isolated fracture of the lesser trochanter.
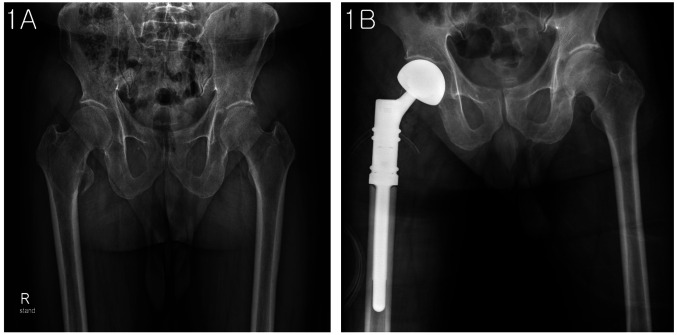
All six patients presented to hospital with groin pain and antalgic gait. Radiographs of the both hips revealed avulsion fractures of the LT (Figure 1A). The mean displacement of lesser trochanter fragment was 1.2 cm (range=0.5-2.2 cm).
Figure 1. A 68-year old man had a right hip pain without trauma. (A) Anterior-posterior radiograph of the hip showed right isolated lesser trochanter avulsion fracture. (B) He was treated with use of The MUTARS (Modular Universal Tumor and Revision System, Implantcast, Buxtehude, Germany).
In five patients, the fracture developed without definite trauma, while the other patient sustained a fall.
Magnetic resonance imaging (MRI) was performed in all six patients. The MRI scan showed metastatic or primary intramedullary lesions with avulsion fracture at the lesser trochanteric area (Figure 2A and B).
Figure 2. A 56-year old man had pain in the right hip without trauma. (A) T2 weighted coronal and (B) T2 transverse MRI showed right isolated lesser trochanter avulsion fracture and enhanced surrounding soft tissue.
Four patients had a history of internal organ malignancy; follicular thyroid cancer, renal cell carcinoma, prostate cancer and osteosarcoma. In the remaining two patients, the LT fracture was the first manifestation of underlying tumors; hepatocellular carcinoma and renal cell carcinoma, which were revealed on further diagnostic work-up including CT-guided core needle biopsy prior to definitive treatment in order to confirm the diagnosis.
Five patients were operated with wide resection and reconstruction of the proximal femur; Four patients were treated with the use of The MUTARS (Modular Universal Tumor and Revision System, Implantcast, Buxtehude, Germany) (Figure 1B), and one patient with bipolar hemiarthroplasty.
The patient with metastatic lesion from renal cell carcinoma underwent preoperative trans-arterial embolization (TAE) with the use of micro-coils to reduce blood loss during the operation. In the four patients treated with wide excision and skeletal reconstruction with MUTARS, the histological diagnosis of excised mass at LT was proven to be metastasis from primary underlying malignancies.
The remaining one patient was diagnosed with prostate cancer with multiple metastases, and was treated with radiation therapy.
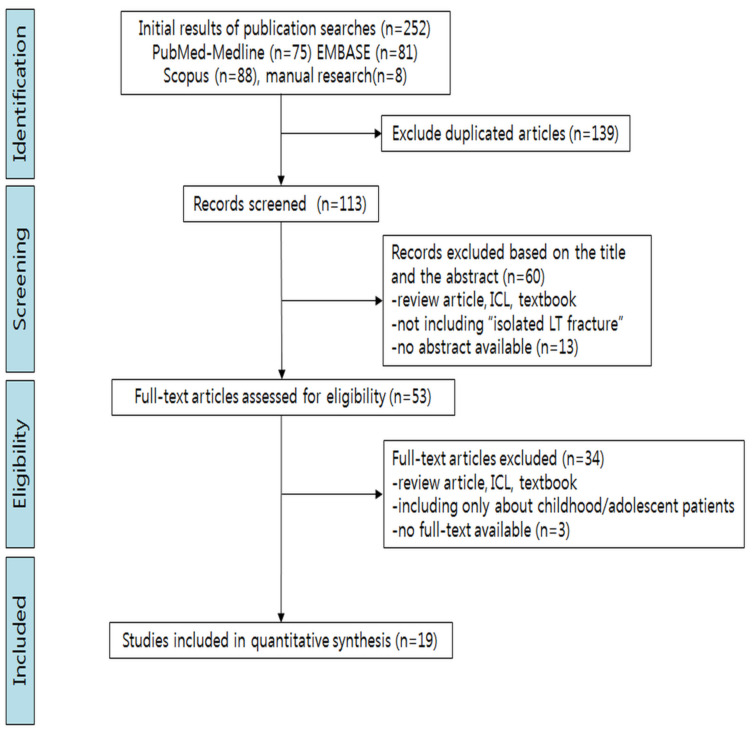
Case search in the literature. A total of 244 articles were retrieved from the search; 75 from MEDLINE via PubMed, 81 from EMBASE and 88 from Scopus database. Among them, 139 duplicates were excluded. The remaining 113 articles were screened based on the title and abstract, and 60 articles that did not include LT fractures were excluded. Review articles, instructional course lectures, textbooks were also excluded. The remaining 53 articles underwent full-text review. Review articles which did not include their own patient case, articles including only childhood/adolescent LT fracture, and articles without available full text were excluded.
By the full-text review, 34 articles were excluded and the remaining 19 articles including 32 isolated LT fractures were selected as the subjects of this review (Figure 3) (Table II).
Figure 3. Preferred Reporting Items for Systematic review and Meta-analysis flow diagram details the process of relevant study selection.
Table II. Summary of studies of isolated fracture of the lesser trochanter in adults.
*Primary pathologic; **Fracture as first manifestation of malignancy; NA: Not applicable; M: male; F: female
In the included studies, 17 patients were males and 13 patients were females except 2 patients whose sex and age were not specified. The average age of patients was 58.3 years (range=19-90 years). Among the 32 isolated LT fractures, 5 (15.6%) were non-pathologic fractures due to trauma, another 5 (15.6%) were pathologic fractures of primary malignancies, and the remaining 22 (68.8%) were pathologic fractures of metastatic lesions. Five primary malignancies at the LT consisted of two chondrosarcomas, one plasmacytoma, one Ewing’s sarcoma and one osteosarcoma. Among the 22 metastatic patients, the site of primary malignancy was breast in five, lung in four, thyroid in two, and prostate in two. Other primary malignancies included renal cell carcinoma, colon cancer, nasopharyngeal cancer, bronchogenic carcinoma, synovial cell sarcoma of popliteal fossa, non-Hodgkin lymphoma, pancreas cancer, hepatocarcinoma and adenocarcinoma of unknown origin.
In 11 patients with pathologic fractures, the LT avulsion was the first manifestation of the malignancies.
For 4 out of 5 patients with traumatic LT fractures, conservative treatment with nonweight bearing was initially performed (1,12,13). Three patients failed in conservative therapy and were eventually treated with open reduction and internal fixation (12). The other patient was treated with prophylactic internal fixation at the first place (12).
For 27 patients with pathologic LT fractures, initial treatment strategies were as follows; conservative treatment in 8 patients (9,14-18), prophylactic fixation in 8 patients (2,5,9,14,19-21) tumor prosthesis in 3 patients (3,5), and allograft-prosthesis composite in one patient (5). Among 8 patients who underwent conservative therapy, 3 patients were subsequently treated with open reduction and internal fixation (14). Treatment modality in 7 patients from 4 studies was not described (7,10,22,23).
Discussion
Of the 38 isolated LT fractures - 32 from the literature and 6 from our own cases - 33 (86.8%) were pathologic fractures. Among the 33 pathologic fractures, six (18.2%) were fractures due to primary malignancies at the LT and 27 (81.8%) were metastatic fractures.
The mechanism of LT fracture is mostly an avulsion injury by psoas tendon with or without the presence of underlying pathology around this area. In adults with LT fracture, pathologic fracture should be considered especially when there is no or low energy trauma prior to the fracture.
Several authors have reported that isolated LT fracture might be the first presentation of undiagnosed malignancies (14,15). In 13 patients (34.2%, 13/38), 11 patients from the literature and two from present study, the LT fracture was the first manifestation of malignancies. In these patients, the underlying primary malignancy should be identified for planning further treatment.
Even though metastases are the most probable diagnoses in adults aged over 40 years with a solitary LT fracture - especially without a history of cancer - biopsy should be considered in order to confirm the diagnosis. The criteria of biopsy in our institute includes 1) a solitary bone lesion of a patient with a history of cancer, that may change the treatment plan according to the diagnosis; 2) a solitary bone lesion of a patient without any history of cancer with features of malignancies; 3) multiple bone lesions of unknown primary site.
The guidelines of the National Comprehensive Cancer Network recommended that biopsy should be postponed until the completeness of thorough medical history taking, systemic review, physical examination, radiologic evaluation and laboratory test because of the following reasons (24): 1) the tumor may be a sarcoma; thus, a staging workup could prevent an inappropriately placed biopsy site or needle trajectory; 2) there may be a site that is easier to perform biopsy; 3) preoperative embolization may be needed to prevent bleeding; 4) a biopsy can be avoided if the diagnosis can be made on the basis of the laboratory analysis, such as with myeloma; 5) a working diagnosis or preoperative suspicion of a primary bone sarcoma on the basis of imaging studies can help the surgical pathologist to make an accurate diagnosis; 6) complete imaging combined with histopathologic analysis may make it more likely for the pathologist to accurately identify the source.
Moreover, poorly planned and impetuously performed biopsy in a patient with a primary bone sarcoma may have a negative impact on functional and oncological outcomes. Nevertheless, biopsy is necessary to make the diagnosis and treatment plan. A common mistake is to proceed with skeletal stabilization with an intramedullary nail for the primary bone cancer under the suspicion of metastasis for a destructive bone lesion (25). Some primary malignant bone tumors including chondrosarcoma, undifferentiated pleomorphic sarcoma of the bone and even osteosarcoma can develop in this age group.
Enhancement MRI and image-guided biopsy are mandatory to reveal the nature of LT fracture. Technetium-99m scintigraphy or positron emission tomography (PET) is necessary to detect other metastases (3,5,10,14).
When metastasis is suspected and an underlying primary malignancy is not evident, further laboratory examinations including various tumor markers are essential to rule out malignancies and to investigate their origin. In male patients, AFP (alpha-fetoprotein), PIVKA-II (protein induced by vitamin K absence or antagonist-II), CA19-9 (carbohydrate antigen 19-9), CEA (carcinoembryonic antigen), thyroglobulin, IL-2 (interleukin-2) and PSA (prostate-specific antigen) are necessary, while CA15-3 (carbohydrate antigen 15-3), CA 125 (carbohydrate antigen 125) are necessary in female patients (Table III) (26,27).
Table III. Tumor markers for screening for malignancy.
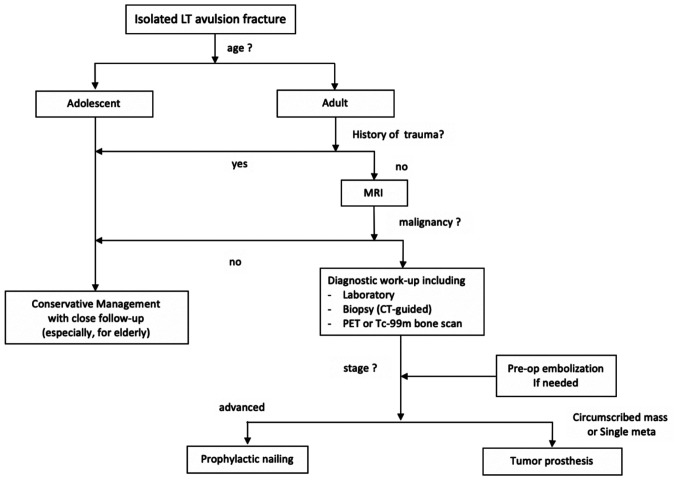
After the LT lesion is confirmed to be a primary malignancy or a metastasis, the extent and stage of the tumor should be evaluated. For the primary malignancy of the region, en bloc resection of the entire proximal femur is recommended in order to obtain local tumor control, and adjuvant chemotherapy is also considered according to the primary tumor type. As the weight bearing axis passes through the medial portion of the proximal femur, LT avulsion caused by the metastatic tumor is a sign of impending fracture in the femur proper. Classically, for LT avulsion with advanced disease, palliative treatment with prophylactic intra-medullary nailing of the proximal femur is recommended (11,28). However, there is a concern of mechanical/local failure especially in this anatomical site. Moreover, with the recent advancement of chemotherapy/targeted agents, the survival of patients with metastatic bone disease has been improved. The treatment strategy for these patients should be based on life expectancy. Therefore, a durable skeletal reconstruction is needed to avoid complicating future management in selected cases. In the literature, wide excision with prosthetic replacement of the proximal femur has been suggested in a single primary or single metastatic lesion (3,14). In our institute, proximal femur resection and endoprosthetic reconstruction is preferred for a primary bone malignancy or isolated bone metastasis after comprehensive discussion with medical oncologists when the life expectancy is expected to be longer than one year (Figure 4).
Figure 4. Treatment algorithm for isolated LT avulsion fracture.
Excision of metastatic lesion is associated with considerable bleeding, when the lesion is hypervascular (29,30). In this situation, preoperative trans-arterial embolization (TAE) is indicated to minimize blood loss (29,30). Hypervascular tumors that could benefit from TAE include giant cell tumor, aneurysmal bone cyst, sarcoma, osteoblastoma, arteriovenous malformation, and metastases of renal cell carcinoma or thyroid carcinoma (Table IV) (31,32).
Table IV. Malignancies where embolization might be helpful.
Conclusion
In summary, underlying malignancy should be suspected in adult patients with isolated LT fracture. For accurate diagnosis and appropriate treatment, thorough understanding of this injury is essential. A stepwise approach can reduce the possibility of misdiagnosis and offer a logical and rational treatment modality option.
Conflicts of Interest
This study was supported by a grant from the Seoul National University Bundang Hospital Research Fund, Seongnam, Korea (No.02-2012-015)
Authors’ Contributions
Hwan Seong Cho and Young-Kyun Lee contributed equally this study, so should be considered as co-first authors; Hwan Seong Cho: Writing – original draft, methodology; Young-Kyun Lee: Writing – original draft, formal analysis; Byung-Ho Yoon: Data curation, literature search; Jung-Wee Park: Writing-review & editing, visualization; Yong-Chan Ha: Conceptualization, project administration; Kyung-Hoi Koo: Writing – review & editing, supervision).
Acknowledgements
This study was supported by a grant from the Seoul National University Bundang Hospital Research Fund, Seongnam, Republic of Korea (No.02-2012-015).
References
- 1.Singh P, Kumar A, Shekhawat V, Singh P. Nonpathological lesser trochanter fracture in adult: Case report and brief review of literature. J Clin Diagn Res. 2015;9(11):RD04–RD05. doi: 10.7860/JCDR/2015/15760.6834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kumar P, Agarwal S, Rajnish RK, Kumar V, Jindal K. Isolated spontaneous atraumatic avulsion of lesser trochanter of femur-a pathognomonic sign of malignancy in adults? A case report and review of literature. J Orthop Case Rep. 2017;7(6):16–19. doi: 10.13107/jocr.2250-0685.930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rouvillain JL, Jawahdou R, Labrada Blanco O, Benchikh-El-Fegoun A, Enkaoua E, Uzel M. Isolated lesser trochanter fracture in adults: An early indicator of tumor infiltration. Orthop Traumatol Surg Res. 2011;97(2):217–220. doi: 10.1016/j.otsr.2010.11.005. [DOI] [PubMed] [Google Scholar]
- 4.Homma Y, Baba T, Ishii S, Matsumoto M, Kaneko K. Avulsion fracture of the lesser trochanter in a skeletally immature freestyle footballer. J Pediatr Orthop B. 2015;24(4):304–307. doi: 10.1097/BPB.0000000000000154. [DOI] [PubMed] [Google Scholar]
- 5.Afra R, Boardman DL, Kabo JM, Eckardt JJ. Avulsion fracture of the lesser trochanter as a result of a primary malignant tumor of bone. A report of four cases. J Bone Joint Surg - Series A. 1999;81(9):1299–1304. doi: 10.2106/00004623-199909000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Dimon JH. 3rd Isolated fractures of the lesser trochanter of the femur. Clin Orthop Relat Res. 1972;82:144–148. [PubMed] [Google Scholar]
- 7.Edmonds LD, Ly JQ, Carter MC, Lusk JD. Quiz case. Nontraumatic avulsion of the lesser trochanter secondary to metastatic adenocarcinoma of the colon. Eur J Radiol. 2003;47(1):57–59. doi: 10.1016/s0720-048x(03)00040-8. [DOI] [PubMed] [Google Scholar]
- 8.James SL, Davies AM. Atraumatic avulsion of the lesser trochanter as an indicator of tumour infiltration. Eur Radiol. 2006;16(2):512–514. doi: 10.1007/s00330-005-2675-3. [DOI] [PubMed] [Google Scholar]
- 9.Khoury JG, Brandser EA, Found Jr EM, Buckwalter JA. Non-traumatic lesser trochanter avulsion: A report of three cases. Iowa Orthop J. 1998;18:150–154. [PMC free article] [PubMed] [Google Scholar]
- 10.Phillips CD, Pope TL Jr., Jones JE, Keats TE, MacMillan RH 3rd. Nontraumatic avulsion of the lesser trochanter: A pathognomonic sign of metastatic disease. Skeletal Radiol. 1988;17(2):106–110. doi: 10.1007/BF00365136. [DOI] [PubMed] [Google Scholar]
- 11.Mirels H. Metastatic disease in long bones. A proposed scoring system for diagnosing impending pathologic fractures. Clin Orthop Relat Res. 1989;249:256–264. [PubMed] [Google Scholar]
- 12.Bonshahi AY, Knowles D, Hodgson SP. Isolated lesser trochanter fractures in elderly–a case for prophylactic dhs fixation. A case series. Injury. 2004;35(2):196–198. doi: 10.1016/s0020-1383(03)00213-4. [DOI] [PubMed] [Google Scholar]
- 13.Uzun E, Çirakli A, Günay AE, Mutlu M. Trochanter minor avulsion fracture in an old patient: Greater care in the diagnosis of hip pain in the elderly. Akademik Acil Tip Olgu Sunumlari Dergisi. 2016;7(4):77–79. doi: 10.5152/jemcr.2016.1527. [DOI] [Google Scholar]
- 14.Bertin KC, Horstman J, Coleman SS. Isolated fracture of the lesser trochanter in adults: An initial manifestation of metastatic malignant disease. J Bone Joint Surg Am. 1984;66(5):770–773. [PubMed] [Google Scholar]
- 15.Herren C, Weber CD, Pishnamaz M, Dienstknecht T, Kobbe P, Hildebrand F, Pape HC. Fracture of the lesser trochanter as a sign of undiagnosed tumor disease in adults. Eur J Med Res. 2015;20(1):72. doi: 10.1186/s40001-015-0167-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Phan TQ, Vu TT. Isolated fracture of the lesser trochanteran indicator of malignancy at proximal femoral head: A case report. Orthop Reum. 2018;10 doi: 10.19080/OROAJ.2018.10.555784. [DOI] [Google Scholar]
- 17.Reategui-Villegas D, Carrasco PC, Dijeres AZ, Betancourt JB. Isolated fracture of the lesser trochanter as a first manifestation of metastatic lung carcinoma. J Med Cases. 2013;4(4):259–261. doi: 10.4021/jmc1077w. [DOI] [Google Scholar]
- 18.Ruffing T, Suda AJ, Ruckauer T, Muhm M. Isolated fracture of the lesser trochanter-what age-related differences are important. Unfallchirurg. 2019;122(5):411–414. doi: 10.1007/s00113-018-0594-4. [DOI] [PubMed] [Google Scholar]
- 19.Abid H, El Idrissi M, Shimi M, El Ibrahimi A, El Mrini A. Isolated from the lesser trochanter fracture in adults, and if it was a metastasis: Report of a case and review of the literature. Pan Afr Med J. 2013;16:97. doi: 10.11604/pamj.2013.16.97.2983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fox TP, Lakkol S, Oliver G. Lesser trochanter fracture: The presenting feature of a more sinister pathology. BMJ Case Rep. 2014;2014:bcr2013202590. doi: 10.1136/bcr-2013-202590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Uddin F, Tayara B, Al-Khateeb H. Stage iv primary bronchogenic carcinoma presenting as a lesser trochanteric avulsion fracture. Current Orthopaedic Practice. 2016;27(3):336–338. doi: 10.1097/BCO.0000000000000364. [DOI] [Google Scholar]
- 22.Kho JS, Howlett DC. Hip pain in a middle aged woman. BMJ. 2016;355:i6129. doi: 10.1136/bmj.i6129. [DOI] [PubMed] [Google Scholar]
- 23.Peh WC, Muttarak M. Clinics in diagnostic imaging (82). Lesser trochanter metastasis. Singapore Med J. 2003;44(2):101–105. [PubMed] [Google Scholar]
- 24.Biermann JS, Adkins DR, Agulnik M, Benjamin RS, Brigman B, Butrynski JE, Cheong D, Chow W, Curry WT, Frassica DA, Frassica FJ, Hande KR, Hornicek FJ, Jones RL, Mayerson J, McGarry SV, McGrath B, Morris CD, O’Donnell RJ, Randall RL, Santana VM, Satcher RL, Siegel HJ, von Mehren M, Bergman MA, Sundar H, National Comprehensive Cancer Network Bone cancer. J Natl Compr Canc Netw. 2013;11(6):688–723. doi: 10.6004/jnccn.2013.0088. [DOI] [PubMed] [Google Scholar]
- 25.Potter BK, Chow VE, Adams SC, Letson GD, Temple HT. Endoprosthetic proximal femur replacement: Metastatic versus primary tumors. Surg Oncol. 2009;18(4):343–349. doi: 10.1016/j.suronc.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 26.Bochtler T, Loffler H, Kramer A. Diagnosis and management of metastatic neoplasms with unknown primary. Semin Diagn Pathol. 2018;35(3):199–206. doi: 10.1053/j.semdp.2017.11.013. [DOI] [PubMed] [Google Scholar]
- 27.Takagi T, Katagiri H, Kim Y, Suehara Y, Kubota D, Akaike K, Ishii M, Mukaihara K, Okubo T, Murata H, Takahashi M, Kaneko K, Saito T. Skeletal metastasis of unknown primary origin at the initial visit: A retrospective analysis of 286 cases. PLoS One. 2015;10(6):e0129428. doi: 10.1371/journal.pone.0129428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Haentjens P, Casteleyn PP, Opdecam P. Evaluation of impending fractures and indications for prophylactic fixation of metastases in long bones. Review of the literature. Acta Orthop Belg. 1993;59(Suppl 1):6–11. [PubMed] [Google Scholar]
- 29.Pazionis TJ, Papanastassiou ID, Maybody M, Healey JH. Embolization of hypervascular bone metastases reduces intraoperative blood loss: A case-control study. Clin Orthop Relat Res. 2014;472(10):3179–3187. doi: 10.1007/s11999-014-3734-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Son HY, An SY, Kim EY, Ahn SB, Lee BC. Selective embolization for hypervascular metastasis from differentiated thyroid cancer: A case series. J Med Case Rep. 2014;8:405. doi: 10.1186/1752-1947-8-405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Barton PP, Waneck RE, Karnel FJ, Ritschl P, Kramer J, Lechner GL. Embolization of bone metastases. J Vasc Interv Radiol. 1996;7(1):81–88. doi: 10.1016/s1051-0443(96)70738-8. [DOI] [PubMed] [Google Scholar]
- 32.Lau V, Sun M, Chu F. Embolisation of hypervascular bone tumours: A pictorial essay with literature review. J Med Imaging Radiat Oncol. 2013;57(2):191–197. doi: 10.1111/j.1754-9485.2012.02444.x. [DOI] [PubMed] [Google Scholar]