Abstract
Objective
Delayed presentation of complex acetabular fractures isn’t uncommon. Surgical treatment of such fractures demand special consideration with respect to surgical approach, reduction techniques, fixation and avoidance of complications. This paper intends to review the literature with regard to the suggested treatment modalities and the reported outcome in late presentations and conclude any recommendations appropriate to the practice in current times.
Background
Displaced fractures of acetabulum, when remained untreated for more than three weeks, pose significant challenge to fracture reduction due to rapid callus formation. In 1976, Letournel described the “Extended Ilio-Femoral Approach”(EIFA) to provide adequate exposure for effective reduction of such fractures. It offered greater exposure of both anterior and posterior columns through a single window, which allowed more precise and controlled reduction of the complex fractures under vision. But despite early enthusiasm in its practice, there has been a steep decline in its application due to reported higher risk of complications. Despite the challenges, the accuracy of fracture reduction in complex acetabular fractures with late presentation was found to be superior in EIFA than the reduction that were achieved by other approaches. Hence a debate to find out the utility of this approach for late reconstruction of complex acetabular fractures (in the face of reported risks of complications) is worthwhile especially in younger patients, who are not suitable candidates for an acute hip replacement surgery and who need their native hip to function well at least for a few years, for their professional and personal high demand activities in their active youthful period.
Methods
The articles for review were retrived using Google Scholar for data retrieval as Pubmed didn’t yield any meaningful results due to paucity of publication in this subject. There were only very few papers in the English literature since 1979, which focused on this condition and were considered for this review. We have included our experience on using EIFA in late presentations of complex acetabular fractures spanning from 1999 to 2019, an experience over two decades to this report.
Results
It was observed that despite delayed presentation, good articular reduction was possible by using EIFA even in complex acetabular fractures. Ultimate functional outcomes were directly related to the accuracy of fracture reduction thus achieved. The risk of heterotrophic ossification in EIFA, though emphasized as significant in the published literature, was found to be least of a problem in our experience.
Discussion
Surgical fixation in delayed cases of complex acetabular fractures was found to be challenging. The choice of surgical approach was found to have a great bearing on the accuracy of fracture reduction and long term functional outcome. In complex acetabular fractures, despite delay in presentation, precise reduction of such fractures was found to be possible when operated using EIFA. CONCLUSION: It was concluded that Every effort must be made to reconstruct the displaced fractures of acetabulum, even in the complex types,despite when they present late, provided the fracture fits into the selection criteria described by Letournel and operated using EIFA. This is very much appropriate to younger patients, who are not great candidate for total hip replacement surgery.
Keywords: Acetabulum fracture, Late presentation or delayed presentation, Internal fixation, Extended ilio-femoral approach, Outcome
1. Introduction
Operative reduction and internal fixation of displaced acetabular fractures received wider acceptance in the later part of the twentieth century, a huge contribution from the original work of Judet and Letournel. The results of such surgery, if performed with high precision, can be rewarding. The goal of treatment of displaced acetabular fractures was defined as absolute anatomical reduction, which is no different from such fractures presenting acutely. It is well known that accuracy of fracture reduction correlates directly with functional outcome.1
The time interval from the injury to surgery influences the quality of reduction. Earlier intervention improves the probability of achieving anatomic reduction. Optimal timing for open reduction and internal fixation (ORIF) is 2–3 days after injury when initial bleeding from intra-pelvic vessels subsides.2
When the ORIF is delayed beyond 3 weeks, the fracture reduction becomes increasingly difficult and outcome tends to be less favorable. Such fractures presenting later than 3 weeks were described as “Delayed or Late Presentations”3 by Letournel in 1979.
It is interesting to note that nothing much has been published on surgical fixation of lately presenting complex acetabular fractures and extended ilio-femoral approach ever since Emile Letournel published his work in 1979. Hence due to paucity of data, this paper is presented in a narrative form rather than in classical way with headings such as “introduction, methods, results, discussion and conclusion” for better understanding of readers. It includes many descriptions and illustrations from our personal experience in late presentations of complex acetabular fractures, which were operated using extended ilio-femoral approach since 1999. Further, the term “complex” used here denotes to mostly the “associated types” of acetabular fractures as classified by “Judet and Letournel” except the combination of posterior wall and posterior column fracture and the anterior column and posterior hemi-transverse types, which are operated using Kocher-Langenbeck or/and Ilio-inguinal approach. Additionally it includes the lately presenting transverse fractures, especially the trans-tectal types as these fractures require nothing less than an absolute anatomical articular reduction and when delayed, it becomes too difficult to reduce it anatomically without extensile exposures. Hence this trans-tectal transverse fracture types are included amongst the complex fractures described in here.
2. Reason for delay
Displaced acetabular fractures are high energy injuries, often seen in poly-trauma patients. Other serious injuries in such patients including injuries to the head, chest, spine, abdomen, and pelvis or limb fractures with open wounds may be present. The treatment of any associated life threatening injuries or open wounds takes priority over definitive acetabular fracture surgery, which can delay surgical fixation of acetabular fractures. Medical optimization of the multiply injured patient can sometimes take longer than expected due to the physiological response to associated multi organ injury, delaying ORIF of acetabular fractures. At times, delayed referrals from peripheral hospitals can impart significant delays.
3. Indication for ORIF in late presentations: Fig. 1
Fig. 1.
A: Displaced ABC Fracture remains "Reduced in Traction"B: It gets displaced proximally and remains unstable when the traction is taken off,(even after being in traction for six weeks) indicating failure to unite and unstable architecture of this fracture, an indication for ORIF as per Letournel’s criterion., C: 45 days old displaced Trans-tectal TV-fracture, The head is not damaged despite a small Hill-Sach like lesion. It is Not a contraindication to ORIF .
-
•
Displaced acetabular fractures with an incongruent hip
-
•
Unstable articular architecture not suitable for non-operative management.
-
•
Unreduced hip dislocation in displaced acetabular fractures
Letournel3 described some criteria to be verified prior to ORIF in late presentation. These are:
-
•
Femoral head must be normal both in density and outline (minor damage may not be contraindication)
-
•
Hip should be free from arthritis
-
•
AP & Judet Views must show different fractured portions of articular surface of acetabulum clearly and it should be possible to recognise primary fracture lines through articular surface.
4. Choice of approach in late presentation
It is reported that functional outcome after ORIF of acetabular fractures is directly related to the accuracy of reduction,4, 5, 6, 7, 8, 9 which indirectly depends on the selection of the correct surgical approach, based on the fracture pattern.10 While selection of approach is clear for most elementary fractures in Letournel’s classification, the decision for complex, associated patterns is a matter of surgeon’s choice, based on his experience and training.11
Delay in presentation makes ORIF of acetabular fracture profoundly difficult, especially in patients with complex fracture patterns. In acute acetabular fractures, the fracture reduction is facilitated by mobility between the fractured fragments. However, in late surgery, such mobility between the fractured fragments is lost due to the ongoing mal-union. Any attempt at fracture reduction demands prior removal of fracture callous and release of any contracted soft tissue, to allow movement between the fracture fragments, which is essential for reduction. In complex acetabular fractures, a single non-extensile approach such as Ilio-inguinal, Anterior Intra-Pelvic or Kocher- Langenbeck alone, may not provide adequate exposure necessary for complete debridement, soft tissue release and release of contracted soft tissues before fracture reduction is attempted. In these cases, a combination of the non-extensile approaches or an extensile approach remains the surgical approach of choice.
There have been several accounts of the use of extensile exposures in the treatment of these injuries.12, 13, 14 As a single exposure, the extended ilio femoral approach (EIFA) allows simultaneous exposure to the entire posterior column and the anterior column up to the ilio-pectineal eminence. It is versatile and permits the required exposure for complete debridement of all the fracture planes, offering the opportunity for direct reduction of fractures under vision. Thus EIFA allows a very high chance of anatomical reduction even in complex fractures despite the challenges of delayed presentation. When required, it even allows intra-articular verification of reduction through capsulotomy especially when an absolute anatomical reduction (which is at times termed as "chondrocytes to chondrocytes reduction") is only acceptable, such as in the case of a high trans-tectal transverse fracture . The intra-articular reduction under vision can be extremely useful to confirm the accuracy in reduction of the articular segments (Fig. 2). The main indications for the extended iliofemoral approach include fractures involving both columns with extension into the sacroiliac joint for which the other approaches will not provide adequate exposure, and old or malunited fractures.11
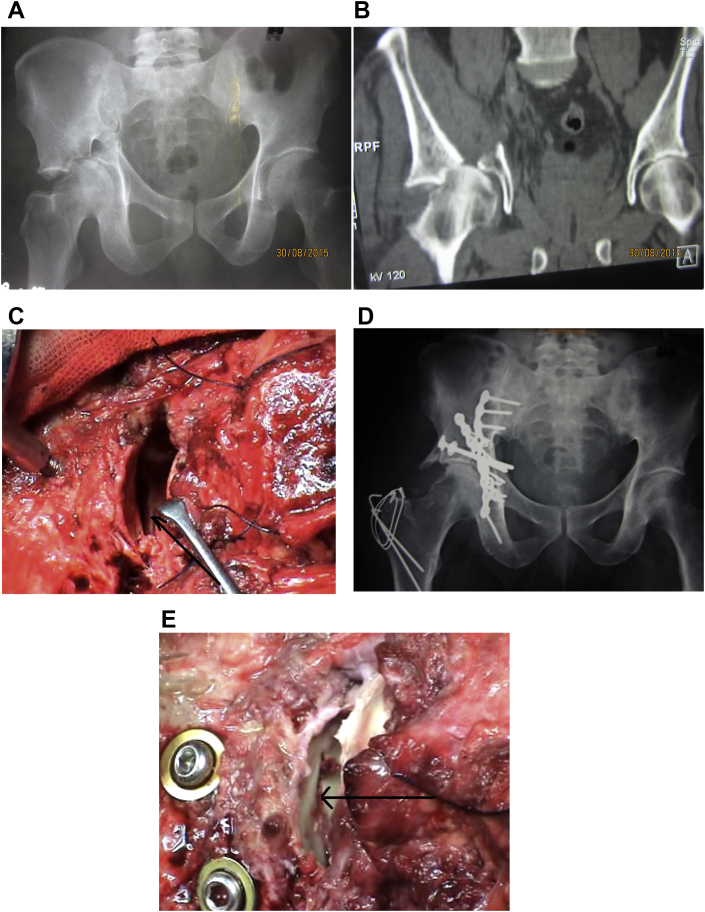
Fig. 2.
A: X ray pictures of a 47 days old displaced trans-tectal transverse fracture of acetabulum with Central dislocation of head of femur. B: Coronal CT shows Hill-Sach like lesion in the head of femur with some damage to the weight bearing part of the head. C: “Capsulotomy” as the “final part of the EIF approach” (and only possible in this approach): allowing intra articular exposure of reduction, so essential in assisting controlled anatomical reduction, especially in this trans-tectal transverse types of fractures. D: 9 years follow up x ray shows Matta's radiological scoring as “good” with minimal sclerosis in the hip:(the hip has been saved from replacement). E: Post internal fixation (intra-op picture) reduction verification through arthrotomy; the arrow head shows the accuracy of acetabular reduction.
However, due to the unfamiliarity of the surgeon with EIFA and sometimes for the fear of the so called higher reported rate of complications with EIFA, there is a trend towards avoiding this approach and resorting to alternative approaches. When operating through dual approaches, there is an awkwardness of turning the patient back and forth between supine and lateral positions throughout the surgery to work through anterior and posterior windows. This can be cumbersome, especially when one is operating on a complex type of acetabular fracture which is already delayed. Despite operating through two exposures, the reduction still remains indirect and intra-articular verification of reduction is not possible (unless a safe surgical hip dislocation is added as well) leaving some scope for ultimate mal-reduction. In an earlier study by Letournel,3 the mainstay for surgically operated delayed fractures was either K-L or EIFA.15 In our experience, EIFA offers unmatched exposure for debridement and more precise reduction of complex associate fractures, when they present late.
5. Effect of delay on Fracture Reduction
Acutely presenting associated fractures are generally reduced indirectly through Ilio-Inguinal or Kocher- Langenbeck approaches. Indirect reduction strategies depends on mobility between fracture fragments. With delay, the fracture starts to heal and organized hematoma and callus interfere with fracture mobility.16 Decreased mobility makes anatomic reduction difficult, often resulting in imperfect reductions. Standard techniques of indirect reduction are less effective in these situations. Strategies to deal with decreased fracture mobility involve complete mobilisation of all fracture fragments, use of more direct fracture reduction techniques16 and more powerful reduction instruments. However, this often requires multiple or extensile exposures with their associated morbidity.16 Delay in flxation may be detrimental to viability of the femoral head in cases of persistent subluxation. There is an increased incidence of chondrolysis and AVN with delayed reconstruction (Figure-3).6
Fig. 3.
A: 28 days old Transtectal-TV fracture with posterior dislocation operated through EIFA B: Chondrolysis evident at 1 year post-op.
6. Tips and tricks in Finer reduction techniques in late presentation
6.1. Fine tuning reduction
A)“Interference method”: A combi-locking plate (LCP), pre-contoured to the anatomical shape of the involved area is anchored to one side of the fracture by a locking bolt. A cortical screw (3.5 mm) is fixed at a distance of about a centi-meter from the other end of the plate in the opposite fracture fragment. Using a bone spreader, the fracture ends can be distracted, by applying force between the plate end and the screw head in a “push-pull” technique. Once the desired reduction is achieved, while the reduction is maintained by the bone spreader, definitive fixation is carried out by fixing screws and locking bolts in the plate, starting at the end that is in contact with the bone spreader. In complex fractures with multiple sites of mal-union, multiple such constructs are used at all the sites where there is over ridding, and finer reductions are required. Using large tools and applying direct force to reduce such fractures can lead to further fragmentations without helping effective reduction, because such over-riding fracture fragments are already weak due to osteopenia from neo-vascularisation and disuse and they fail to withstand the massive force applied by larger reduction tools used to facilitate finer reductions. The technique of fine reduction with a pre-contoured plate does effective finer reduction of fractures while avoiding further fragmentation of the already weakened fractured segments in late presentations. Because it keeps the fractured ends buttressed and supported all the time while reducing the fracture in distraction mode.
B)“Distraction Reduction By Over-Contoured Plate and Bolts”: In this technique, an over-contoured combi-locking plate is first fixed toeither side of the fracture plane to be reduced. It is aligned perpendicular to the fracture plane and anchored anchored to bones with locking bolts , which are locked to the plate holes on the far ends of the plate. It provides a strong “plate-bone coupling” to tolerate the distraction force during reduction even in the steoporotic bones. Then by bringing the over contoured part of the plate towards the bone surface, the plate ends tend to move away from each other causing elongation of the plate and thus push the over ridding fracture ends apart helping fracture reduction by distraction force. This gradual straightening of the over-contoured plate is performed by applying screws through the convex part of the plate and tightening the screws in sequence, which brings the over bent plate towards the bone surface. Such controlled distraction across the fracture site is done till the fracture is reducedcompletely. Once the reduction is verified to be accurate, the remaining holes are filled in with locking bolts. (Figure-4). This is again a delicate way of achieving finer reductions in weaker osteopenic bones.
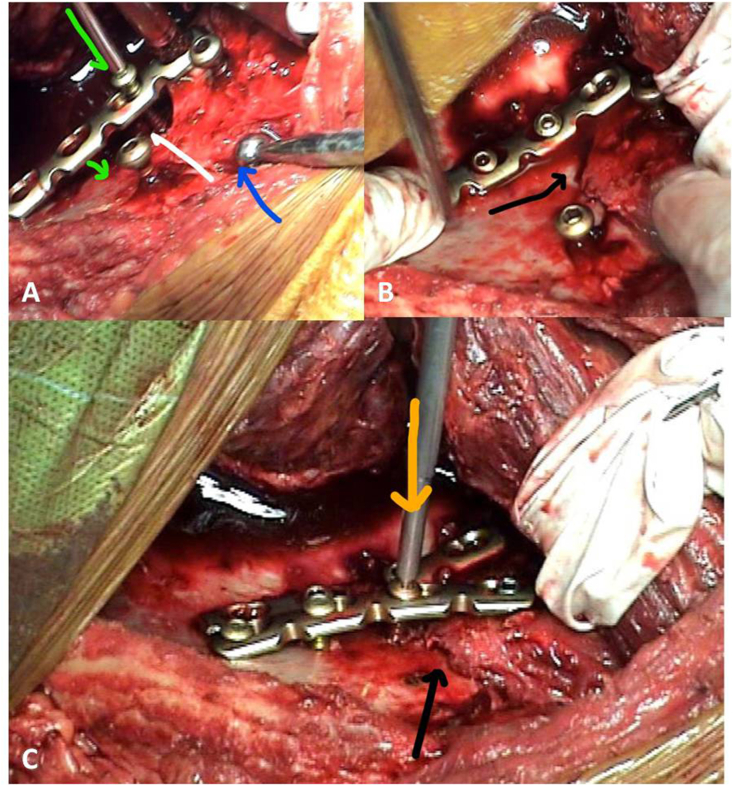
Fig. 4.
A: The two screws on either side of the fracture are evidence for failure of the attempted reduction by application of bone spreader. The technique of Reduction of Periarticular Step off by "Locking Plate Interference technique" is demonstrated-The over contoured plate is being brought on to the bone surface by gradual tightening of the cortical screw in picture-Fracture is over-riding B: Apex Of Fracture reduced by gradual tightening of screw C: Another Plate used in same manner anteriorly.
6.2. Tackling hip congruity in difficult mal-unions(Reversal of sequence of reduction)
These high energy complex fractures often produce smaller comminuted fragments between the major fracture fragments in the innominate bone, more in the periphery towards the iliac wing. These smaller fragments need to be anatomically reduced along with the major fracture fragments from periphery to centre in sequence without any mal-reduction to create an anatomically reduced acetabulum with a congruous hip joint. In early healing phase, these smaller fragments get engulfed by the formation of the exuberant callous and the surgeon removes them inadvertently along with the callous during debridement. While attempting anatomical reductions of the major fragments after such debridement and starting at the periphery in the iliac wing, the space which was earlier occupied by these smaller fragments (which are already excised along with the callous), gets obliterated, resulting in peripheral mal-reduction (but it appears as if there is an anatomical reduction in the periphery). It results in gapping between the fragments at the fracture line in the other end of these fragments, which is the acetabulum. Centrally the acetabulum gets wider and results in mal-reduction and incongruity of the hip. It needs to be checked during surgery. If it is seen intra-operatively during fluoro screening with c-arm, it requires immediate revision. If fixation is already performed in this mal-reduced position, then the entire fixation needs to be removed. Further, using the head of the femur as a template, the immediate peri-articular fragments are repositioned around the femoral head in most appropriate orientation creating anatomical articular reduction and congruous hip, this results in creation of voids between the major fragments peripherally (which was occupied by the comminuted fragments earlier), while the acetabulum is anatomically reduced in the centre. In this situation, conventional principle of reduction from periphery to centre is reversed. Accurate peri-articular approximation of fragments is performed first by direct reduction keeping the congruity of hip as the reference for such reduction. Any mal-reduction in the periphery is ignored (due to the gaps already explained) and the peripheral fixation is performed. This is done with complete disregard to status of peripheral reduction (Figure-5) (Video-2, Video-3) These complex manoeuvres are easier to perform through EIFA. In 1979 Prof. Letournel already explained that attempt is made to restore anatomy of both the ilium and the acetabulum, but in case total repair is impossible, priority is given to acetabulum.3
Fig. 5.
A: 23 Days old ABC fracture B: Saw-bones demonstrating small comminuted fragments, which are inadvertently removed during debridement C: Intra-articular malreduction due to apparent peripheral anatomical reduction ignoring the space occupied by the loss of smaller bony fragments, which were removed with callous during debridement D: Keeping hip congruous created gaps in the innominate bone peripherally in the iliac wing before fixation started E: Fixation done with congruous hip, no regards for attempting anatomical reduction on peripheral iliac wing F: c arm picture of revision fixation showing Congruous Hip with gaps in iliac wing G: Post Op X-ray H: 7 Years follow-up X-Ray showing Congruous Hip with Gap In Ilium at periphery.
Supplementary video related to this article can be found at https://doi.org/10.1016/j.jcot.2020.10.038
The following is the supplementary data related to this article:
Video 1.
Video 2: Functioal-Outcome of figure-5 pt.
Video 3Functioal-Outcome of figure-5 pt.
6.3. Effect of delay on radiological & functional outcome
Johnson et al.17 described the rate of anatomical reduction of only 52% in fractures which were operated on more than 21 days from injury compared with rate of reduction in fractures operated within 3 weeks at 71%.4 Mears et al.1 reported that patients with delay of more than 11 days had a significantly lower rate of anatomical reduction. It has been reported that odds of obtaining anatomical reduction and excellent/good functional outcome reduce significantly as time to surgery increases.16 Willet et al. reported that anatomical reduction was no longer possible after day 14 for elemental and after day six for associated fractures. Excellent/good functional outcome was most likely in those patients operated within 15 days for elementary and 10 days for associated fractures.18 The chance of achieving anatomical reduction and excellent/good functional outcome reduces significantly for both elementary and associated fractures as time to surgery increases. Delays in ORIF have more effect on outcome for associated fracture sub-group.18
In one of the earliest reports published on reconstruction in late presentations3, Prof. Letournel stated that surgical treatment of acetabular fractures, later than third week after accident, is difficult because new bone formation is rapid here. It is nevertheless possible. He further stated that “complete reconstruction of hip has been successfully achieved from one to twenty-seven months after accident and has given us very good clinical and radiological results in more than 50% of cases. Total joint replacement if necessary, is then much simpler after acetabular reconstruction”. Though these reports vary in their assessment of critical time limit for achieving anatomical reduction and excellent to good functional outcome, they all agree to the very fact that with delay, chances of achieving anatomic reduction and excellent functional outcome is reduced.
In 2015, a Chinese study showed that ORIF for fresh acetabular fractures might yield a better prognosis; however, for delayed acetabular fractures, clinical outcomes are also predictable when sophisticated surgical techniques are employed.15 From our experience, we are convinced that with the use of EIFA and modern reduction tools, the quality of reduction and hence functional outcome can be significantly improved in late presentations.
Factors determining the outcome of ORIF in late presentation:
-
A)Not controlled by the surgeon:
-
i.Age: Higher age group have poorer outcome.
-
ii.Complex fracture types have more adverse outcome.
-
iii.Associated other skeletal or visceral injuries. could affect outcome adversely
-
iv.Direction of dislocation: Posterior or anterior dislocation have better outcome than central dislocation.
-
v.Presence of dome comminution: difficult to reconstruct and can lead to early arthritis.
-
vi.Impacted articular fragments: Unless these are dis-impacted and aligned well, lead to traumatic arthritis.
-
vii.Osteoporosis: poor outcome
-
viii.Femoral head Injury: if in upper quadrant, can lead to rapid traumatic arthritis.
-
ix.Prior treatment: Any neglected dislocation and previous attempts of ORIF will increase risk of AVN and infection.19
-
i.
-
B)Factors Controlled by the surgeon:
-
i.Reduction: imperfect reduction leads to early arthritis, should be avoided.
-
ii.Peri-operative complications must be avoided or managed effectively by taking extra precautions.
-
iii.Poor case selection: Cases should be strictly assessed for risk and benefits for ORIF in late presentation. Criteria described by Letournel must be followed. These patients are likely candidates for future THR and hence, if one doesn’t fit well into the criteria, then primary THR or other salvage procedures might be considered instead of ORIF. Patients who are not well optimised could end up with complications.
-
i.
7. Complications
-
1
Mal-reduction: With delay, there is a drop in the rate of anatomical or good reduction. With delay, osteopenia occurs from lack of loading or disuse and from hyper-vascularity due to neo-vascularisation, giving poor purchase to fixation. It could result in secondary loss of fixation and mal-union. Locking implants are more effective in preventing loss of reduction. When there is any concern about the stability achieved during surgery, post-operative traction and delayed mobilisation may be advised for a period to prevent this complication. Any gap at the articular area adds to instability and in such a situation, post op traction and delayed mobilisation needs to be advised.
-
2
Heterotrophic Ossification (HO): It is considered to be clinically significant when it results in loss of 20% or more of hip movements.4,20 It is said that HO is commonly seen after dissection of abductor muscle mass from external ilium and it was seen to be clinically insignificant.21 Letournel recommended his protocol combining indomethacin and single-dose radiation as described by Moed and Letournel.22 Letournel observed that ORIF for acetabular fracture performed through EIFA 3 weeks after injury had much lower incidence of HO than those cases operated through same approach within 3 weeks of injury. We have observed that surgical exposure with EIFA when extended both distally and proximally adequately, it reduces the tension and pressure exerted by bone levers while retracting thick muscular posterior flap and hence the muscle damage from pressure under levers is significantly reduced. Further, intermittent release of pressure under levers during these long procedures also prevent such damage to muscles flap. It could reduce the chances of developing HO. Intermittent wound irrigation with hydrogen peroxide and normal saline removes debris and bone debris created during surgery. Additionally, keeping tissues hydrated by intermittent irrigation also prevent tissue damage significantly. We believe that by avoiding damage to the muscle with careful retraction and application of larger incision along with periodic irrigation to protect the muscle from drying up has helped us reduce the incidence of HO in cases operated by us. Also, the irrigation helped remove any bone or soft tissue debris, which could be a nidus for HO in the future,
We routinely use Indomethacin 75 mg in 3 divided doses daily for 12–16 weeks or a single 700 CGY dose of radiation to pelvis post-operatively. We have never used both in combination. Our first preference is Indomethacin, however if patients have any intolerance to this drug, we switch over to radiation. Though it is recommended to initiate Indomethacin on day one following surgery, most of our patients start anytime after day 5. Indomethacin is known to cause severe gastritis and in our opinion starting this therapy before the patient is taking oral diet is considered risky.
-
3
AVN and Chondrolysis: If the hip remains dislocated, the head of femur can suffer from AVN or chondrolysis. Every attempt should be made to reduce dislocations as early as possible and to maintain reduction.
-
4
Sciatic nerve palsy: Keeping the hip extended and knee flexed during EIFA keeps the sciatic nerve relaxed and protects from traction injury.
-
5
Infection: Patient optimization, surgical asepsis, intra-operative discipline, adequate wound care and appropriate antibiotic coverage can effectively prevent infection. However, these patients may have already undergone surgery for other injuries and their nutrition can be poor due to prolonged convalescence. Optimizing nutrition and physiology of these patients is paramount before subjecting them to any further major surgical insult like this major procedure.
-
6
Superior Gluteal Vessel and Nerve (SGVN) injury: It may occur in trans-tectal transverse, T shape & associated both column fractures. In these cases, the posterior column fracture is in proximity to where SGVN exits from pelvis. One should understand the anatomy of SGVN and be extra careful to prevent such injury by being cautious and meticulous in dissection and debridement in the greater sciatic notch area.
-
7
Secondary loss of reduction: This can be due to instability from gaps due to loss of bone from debridement especially in the articular zone, softened bones giving poor purchase to fixation and persistent deforming forces exerted by contracted soft tissues despite adequate release in delayed ORIF. The use of locking implants and (when in doubt), applying post-operative skeletal pin traction for 6–10 weeks can protect fractures and prevent redisplacement.
-
8
Deep vein thrombosis and Pulmonary embolism (DVT and PE): Patients with acetabulum and pelvis injuries are at a high risk for venous thrombo-embolism (VTE). Patients should be assessed, screened and managed with adequate prophylaxis or treatment depending on the case. We routinely use LMWH both pre and post operatively. We have used inferior vena cava filters in some extreme cases with very high risk of embolism. Upon discharge, majority of our patients receive low dose aspirin. In our series of 69 surgically treated fractures presenting late, we have not had any fatalities as a result of VTE.
8. Conclusion
Complex acetabular fractures tend to unite fast with rapid callous formation. When delayed beyond three weeks in surgical fixation, a reasonable fracture reduction becomes hard to achieve. However, despite rapid mal-union from delay, when a reasonable reduction is achieved through surgery, the long term functional outcome remains satisfactory. Hence, the goal of treatment of displaced acetabular fractures, especially in younger population, should be anatomical reconstruction despite the difficulties in reducing such mal-uniting fractures, because such patients are not appropriate for total hip replacement surgery.
The use of EIFA gives the best opportunity for most precise reduction of fractures in lately presenting complex acetabular fractures. Though EIFA has been discredited in the literature for some undesirable complications including development of heterotrophic ossification (HO), in our experience, the incidence of HO has been seen to be insignificant, the reasons for which need to be investigated further. The other complications associated with EIFA also needs further evaluation through more studies as there are publications failing to confirm such adverse effects.
Hence, despite the complexity of the acetabular fracture and the delay, if the case selection is executed according to the criteria described by Letournel, reconstruction through EIFA may be attempted by an experienced team in every young patient, who is far away from desrving a total hip replacement surgery due to his age and expected demand on the hip.
Funding
No funding or grants were received or will be received from any commercial party relating to the subject of this article.
Declaration of competing interest
On behalf of all authors, the corresponding author states that there is no conflict of interest to disclose.
Acknowledgements
We acknowledge the data contributed in the form of all the figures in this article by the erswhile West End Hospital at Cuttack,India, which was owned by the corresponding author.1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21
Abbreviations
- ORIF
Open Reduction Internal Fixation
- AIP
Anterior Intrapelvic Approach
- EIFA
Extended Ilio-femoral Approach
- HO
Heterotopic Ossification
- SGVN
Superior Gluteal Vessel and Nerve
- ABC
Associated Both Column Fracture
- AVN
Avascular Necrosis
- TV
Transverse Fracture
- VTE
Venous Thromboembolism
- LMWH
Low molecular weight heparin
References
- 1.Mears D.C., Velyvis J.H., Chang C.P. Displaced acetabular fractures managed operatively: indicators of outcome. Clin Orthop. 2003;407:173–186. doi: 10.1097/00003086-200302000-00026. [DOI] [PubMed] [Google Scholar]
- 2.Dailey S., Phillips C., Radley J., Archdeacon M. Achieving anatomic acetabular fracture reduction—when is the best time to operate? J Orthop Trauma. 2016;30(8):426–431. doi: 10.1097/BOT.0000000000000576. [DOI] [PubMed] [Google Scholar]
- 3.Letournel E. Surgical repair of acetabular fractures more than three weeks after injury, apart from total hip replacement. Int Orthop. 1979;2(4):305–313. [Google Scholar]
- 4.Matta J.M. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg [Am] 1996;78-A:1632–1645. [PubMed] [Google Scholar]
- 5.Mayo K.A. Open reduction and internal fixation of fractures of the acetabulum: results in 163 fractures. Clin Orthop. 1994;305:31–37. [PubMed] [Google Scholar]
- 6.Letournel E., Judet R. second ed. Springer Verlag; Berlin: 1993. Fractures of the Acetabulum; pp. 29–62. [Google Scholar]
- 7.Moed B., Yu P.H., Gruson K.I. Functional outcomes of acetabular fractures. J Bone Joint Surg [Am] 2003;85-A:1879–1883. doi: 10.2106/00004623-200310000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Giannoudis P.V., Grotz M.R.W., Papakostidis C., Dinopoulos H. Operative treatment of displaced fractures of the acetabulum: a meta-analysis. J Bone Joint Surg [Br] 2005;87-B:2–9. [PubMed] [Google Scholar]
- 9.Borelli J., Goldfarb C., Ricci W., Wagner J.M., Engsberg J.R. Functional outcome after isolated acetabular fractures. J Orthop Trauma. 2002;16:73–81. doi: 10.1097/00005131-200202000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Matta J.M. Operative indications and choice of surgical approach for fractures of the acetabulum. Tech Orthop. 1986;1:13–22. [Google Scholar]
- 11.Griffin D., Beaulé P., Matta J. Safety and efficacy of the extended iliofemoral approach in the treatment of complex fractures of the acetabulum. J. Bone Joint Surg. Br. 2005;87:1391–1396. doi: 10.1302/0301-620X.87B10.16538. [DOI] [PubMed] [Google Scholar]
- 12.Reinert C.M., Bosse M.J., Polka A. A modified extensile exposure for the treatment of complex or malunited acetabular fractures. J Bone Joint Surg [Am] 1988;70-A:329–337. [PubMed] [Google Scholar]
- 13.Alonso J.E., Davila R., Bradley E. Extended iliofemoral versus triradiate approaches in management of associated acetabular fractures. Clin Orthop. 1994;305:81–87. [PubMed] [Google Scholar]
- 14.Stockle U., Hoffmann R., Sudkamp N.P., Reindle R., Haas N.P. Treatment of complex acetabular fractures through a modified extended iliofemoral approach. J Orthop Trauma. 2002;16:220–230. doi: 10.1097/00005131-200204000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Gao Y., Zhou Z., Tang M. Late surgery for acetabular fractures in a Chinese level I trauma centre: surgical experience and outcomes. Int Orthop. 2015;39(9):1865–1871. doi: 10.1007/s00264-015-2932-2. [DOI] [PubMed] [Google Scholar]
- 16.Jenkinson R. Clinical Gate; 2015. Acetabular Fractures: Does Delay to Surgery Infl Uence Outcome?https://clinicalgate.com/acetabular-fractures-does-delay-to-surgery-influence-outcome/ [Internet] Available from: [Google Scholar]
- 17.Johnson E.E., Matta J.M., Mast J.W., Letournel E. Delayed reconstruction of acetabular fractures 21 to 120 days following injury. Clin Orthop. 1994;305:20–30. [PubMed] [Google Scholar]
- 18.Madhu R. Outcome of surgery for reconstruction of fractures of the acetabulum. J Bone Joint Surg [Br] 2006;88-B.9:1197–1203. doi: 10.1302/0301-620X.88B9.17588. [DOI] [PubMed] [Google Scholar]
- 19.Laud N.S. Acetabular fractures: late presentation. Indian J Orthop. 2002;36:31–32. [Google Scholar]
- 20.Matta J.M., Siebenrock K.A. Does indomethacin reduce heterotopic bone formation after operations for acetabular fractures? J Bone Joint Surg [Br] 1997;79-B:959–963. doi: 10.1302/0301-620x.79b6.6889. [DOI] [PubMed] [Google Scholar]
- 21.Alonso J.E., Davila R., Bradley E. Extended iliofemoral versus triradiate approaches in management of associated acetabular fractures. Clin Orthop. 1994;305:81–87. [PubMed] [Google Scholar]
- 22.Moed B., Letournel E. Low dose irradiation with indomethacin for the prevention of heterotopic ossification. J Bone Joint Surg [Br] 1994;76-B:895–900. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video 1.
Video 2: Functioal-Outcome of figure-5 pt.
Video 3Functioal-Outcome of figure-5 pt.