Abstract
Introduction
Diffuse idiopathic skeletal hyperostosis (DISH), or Forestier disease, is a condition characterized by calcification and ossification of ligaments and enthuses (ligament and tendon insertion sites), which mainly affect the vertebral column. The clinical manifestation of DISH is variable. Some patients can be completely asymptomatic, whereas others can complain of painful stiffness, decreased range of movement, and myelopathy symptoms. OPLL usually produce myelopathy symptoms. Combined of OPLL and DISH are rare case.
Illustration
A 59 years old woman patient complained of neck and shoulder pain in the last 20 years ago, with decreased neck range of motion and dysphagia. There was no gross abnormality on patient's neck and back. Cervical x ray was showing a continuous ossification extending from the anterior surface of C2 to C7 in lateral radiograph. A similar ossification was also noticed on the posterior surface of the vertebral bodies from C2 to C6 abutting the spinal canal.
Discussion
Despite striking abnormal appearance of cervical DISH and OPLL seen on radiologic examinations, absence of myelopathy is an indication to non-operative treatment. Presence of dysphagia was not an indication of surgery in this patient, as dysphagia was not severe and myelopathy was absent. Patient was observed during her clinical course to document the progression of myelopathy. Prophylactic surgery was not indicated for this patient, and progression of myelopathy during observation is an indication for surgical intervention.
Conclusion
Diffuse and large abnormalities in cervical area with normal neurological function is not indication for surgery. Selective treatment based on individual case.
Keywords: DISH cervical, OPLL, Myelopathy, Observation, Case report
Highlights
-
•
Reporting a rare case combine of DISH Cervical and OPLL.
-
•
Controversy indication for surgery.
-
•
Dysphagia and correlation of diffuse ossification in cervical region.
1. Introduction
Diffuse idiopathic skeletal hyperostosis (DISH), or Forestier disease, is a condition characterized by calcification and ossification of ligaments and enthuses (ligament and tendon insertion sites), which mainly affect the vertebral column [1]. DISH occurs primarily in the elderly population and is often associated with osteoarthritis and ossification of the posterior longitudinal ligament (OPLL), with the prevalence of up to 50% [1]. Forestier's disease was first described by Jacques Forestier and his student Jaume Rotes-Querol in 1950 under the name of “senile ankylosing vertebral hyperostosis”. They perceived this disease as an ankylosing disease of the spine developing in old people, with a painless onset and clinical, pathological, and radiological features distinguishing it from ankylosing spondylitis. Some other literature in before that period, such as Leri (1904) and Marie and Astie (1897) gave the name for this condition as “heredo-traumatic kyphosis of Bechterew “. Meyer and Förster (1938), based on their observation, gave the name of “moniliform hyperostosis " for this condition. Oppenheimer (1942), based on his observation, noticed this condition is a type of ossification associated with ankylosing spondylitis. Lacapere (1949) in his study of osteophytosis of the spine in dried bones often mentions outgrowths which he calls " melorheostosis of the spine ". In 1976, Resnick and Niwayama gave the term “diffuse idiopathic skeletal hyperostosis” (DISH), which is currently widely accepted. This disease consists of a systemic noninflammatory disease characterized by ossification of the entheses – the bony attachment of tendons, ligaments, and joint capsules. This is a systemic condition and is often underdiagnosed [2]. There is a predisposing locus for OPLL on chromosome 6p, close to the HLA locus. There is genetic linkage and allelic association of the COL 11 A2 gene which would constitute an inherited predisposition for OPLL [3]. It has long been considered that OPLL is a disease of Asian origin, and more specifically of the Japanese population. The prevalence of OPLL in Japanese and East Asian countries has ranged from 1.9% to 4.3% [4]. The etiology of DISH is unknown, but it has a strong correlation with obesity and type 2 diabetes mellitus. Long standing metabolic abnormalities will increase the production of several growth factors including insulin-like growth factor 1, and inflammatory mediators IL-1 and IL-6. This chemical substances through the receptor activator of nuclear factor kappa-B ligand mechanism will cause proliferation of osteoblasts and ultimately bone deposition. Due to increased prevalence of obesity and type 2 diabetes mellitus, the prevalence of DISH also increases. The risk of developing DISH 80 years old men is 32.1%, whereas for 80 years old women is 16.9% [2].
The clinical manifestation of DISH is variable. Some patients can be completely asymptomatic, whereas others can complain of painful stiffness, decreased range of movement, and symptoms secondary to encroachment of the bony excrescences on neighbouring structures. Pharyngoesophageal and tracheal compression can cause dysphagia, dyspnea, and stridor [1]. Five percent of patients diagnosed with OPLL are asymptomatic, but varying degrees of neurologic symptoms can be present including both radiculopathy and myelopathy. Myelopathy is caused by a decrease in the space available for the spinal cord due to the OPLL. The severity of myelopathy symptoms may be exacerbated by coexisting congenital cervical stenosis. Patients with myelopathy often give a history of changes in balance and fine motor skills (worsening handwriting, difficulty buttoning buttons). As myelopathy progresses, difficulty in walking ensues. Findings in physical examination includes Rhomberg and tandem gait tests which identify the signs of gait or balance dysfunction, brisk reflex and clonus in upper and lower extremities, pathologic reflexes such as Hoffmann and inverted radial reflexes suggesting upper motor neuron, and hyperactive scapulohumeral reflex if the cord compression occurs above the C3 vertebrae [5]. Dysdiadochokinesia or difficulty with rapid supination and protonation of the hand can be found in myelopathy. In some cases of OPLL, the patient may complain of radicular symptoms and may demonstrate radicular signs such as a positive Spurling test [5]. The radiographic diagnostic criteria for DISH of the spine is based on Resnick et al. [6]. The criteria are the presence of osseous bridging along the anterolateral aspect of at least four vertebral bodies, relative sparing of the intervertebral disc height with minimal or absent disc degeneration, and absence of apophyseal joint ankylosis and sacroiliac sclerosis [6]. OPLL is readily demonstrated by lateral radiography. But because of the presence of overlying bony structures, CT is indicated for establishing the diagnosis. MRI can demonstrate a narrowing of the spinal cord even though the ossification itself is not clear [6,7].
Patients without myelopathy are likely to remain progression-free, and patients with myelopathy have a high rate of progression. Therefore, prophylactic surgery is not recommended for patients without myelopathy. Operative management of OPLL with cervical involvement is reserved for patients with progressive myelopathy and myeloradiculopathy that has not responded to nonoperative treatment [5]. We presented a case with a concurrence of DISH and OPLL of the cervical spine. This is a rare case in Indonesia region and south east asia region due the theory proposed predispotion of racial and gene factors. It is also unique case while despite of diffuse and large abnormalities in cervical area but still normal neurological function not indication into surgery, selective treatment based on individual case.
2. Case illustration
A 59 years old woman complained of neck and shoulder pain which is occasionally accompanied by vertigo in the last 20 years ago, and went to neurologist 17 years ago. The neurologist suggested patient to have neck radiography with the result of ossification of neck bones. MRI was performed and the findings were ossification of the cervical spine without nerve entrapement. The patient then given analgesic diclofenac sodium 25 mg twice a day and the symptoms reduced. Recently, patient complained of mild neck pain and difficulty in swallowing and dysphagia. The neck movement was also becoming more restricted. The activity of everyday life was normal, patient was not smoking and patient was able to perform her routine tasks as housewife.
Patient presented at hospital walking normally without aid. During examination, there was no gross abnormality on patient's neck and back. The range of motion of the neck was restricted. There were no tingling sensation and paresthesia on the limbs and radicular pain. Focused examination showed that Spurling sign was negative, Lhermitte sign was negative, Hoffmann-Tromner test was negative, and grab finger hand test was negative. (Fig. 1)
Fig. 1.
Clinical Manifestation. No sign of deformity.
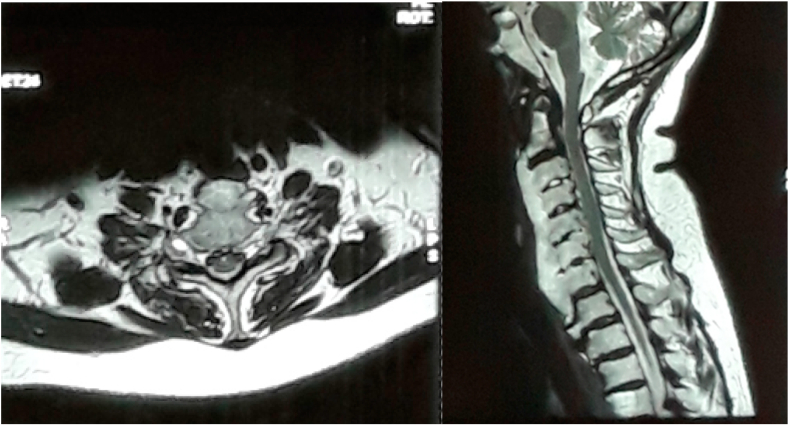
Cervical x ray was performed, showing a continuous ossification extending from the anterior surface of C2 to C7 in lateral radiograph (Fig. 2). CT Cervical perfomed showed apart from sign of Diffuse ossification we founda similar ossification was also noticed on the posterior surface of the vertebral bodies from C2 to C6 abutting the spinal canal or Ossification of posterior longitudinal ligament (Fig. 3). Intervertebral discs heights were normal. however from MRI examination no sign of compression spinal canal (Fig. 4).
Fig. 2.
Plain Cervical X ray. Lateral view radiograph shows 'flowing' anterior osteophytes and ossification of the posterior longitudinal ligament and calcification of the posterior longitudinal ligament.
Fig. 3.
CT Cervical. Axial and sagittal view showed diffuse ossification of the corpus of vertebra cervical 2 to 7 and anterior thickening of the OPLL.
Fig. 4.
MRI Cervical. The axial and sagittal MRI showed diffuse ossification of the corpus of vertebra cervical 2 to 7 and anterior thickening of the OPLL but there is no sign of protrusion, compression nor destruction of spinal canal.
We followed up this patient by phone due to patient unwillingly control to our hospital fear of pandemic, patient stated the complained of neck stiffness and dyshpagia still same but no further worsening nor neurological deterioration. This case report had been presented in accordance to SCARE guideline [8].
3. Discussion
Patient was treated non-operatively using pain medication, topical agents, NSAIDs, bed rest and assist devices. For the symptom of dysphagia, change of food habit and swallow training was advised. Patient was observed during her clinical course to document the progression of myelopathy. Patient was advised to visit doctor every 3 month or if the disease progress fast. Prophylactic surgery was not performed.
When DISH occurs in cervical spine, it can cause dysphagia, although it is rare. A study by Dutta et al. [10] showed that dysphagia is the most common symptom of DISH affecting the cervical spine. In cervical spine, DISH most commonly occurs in the lower vertebrae. Other symptoms are neck pain, reduced neck mobility, voice change, stridor or even aspiration related complications. Primary and definitive treatment for dysphagia due to cervical DISH is surgical removal of the osteophytes. If surgery is contraindicated, change of food habit and swallow training can be advised and can be of value in maintaining nutritional requirement.
In the early stage, most of OPLL patients do not have symptoms. However, complaints of mild pain, discomfort, or numbness in hands may occur. As OPLL grows, symptoms increase in severity due to compression of the spinal cord and nerve roots. The most common symptoms in the early stages of OPLL include dysesthesia and tingling sensation in hands, and clumsiness. With the progression of neurologic deficits, lower extremity symptoms such as gait disturbance may appear. OPLL patients show symptoms of myelopathy caused by spinal cord compression rather than radicular pain due to nerve roots compression [11].
The treatment of OPLL is symptomatic, such as pain medication, topical agents, anti-inflammatory drugs, antidepressants, anticonvulsants, non-steroidal anti-inflammatory drugs and opioid can be applied, and bed rest and assist devices, such as a brace, are recommended for local stabilization. The prevalence of cervical myelopathy in OPLL is related to the severity of spinal canal obliteration by the OPLL. When the myelopathy ensues causing gait disturbance and disorders of fine motor movement in the hand, appropriate recovery is not expected with conservative treatments, and therefore surgery is indicated [,[11], [12]].
In this Case report, patient came with chief complaint of dysphagia and neck discomfort without other neurological deficits. Physical examination showed no evidence of myelopathy and plain radiographs showed evidence of DISH with ‘flowing’ anterior osteophytes in the cervical spine. Careful inspection of lateral views of the cervical spine showed calcification of the posterior longitudinal ligament. The differential diagnosis is ankylosing spondylitis. CT and MRI examinations show no signs of spinal cord compression. Due to absence of myelopathy, patient was treated non-operatively and observation was performed to see the presence of progression [[5], [9]].
This case report showed that the probable risk factor for DISH and OPLL of this patient is the racial cause. DISH and OPLL was thought to be a disease of Asian population. This patient has a multi-racial descendant, and it probably accounted for the disease. Despite striking abnormal appearance of cervical DISH and OPLL seen on radiologic examinations, surprisingly this patient didn't have any sign of myelopathy and this is an indication to non-operative treatment. Presence of dysphagia is not an indication of surgery in this patient, as dysphagia is not severe and myelopathy is absence. Prophylactic surgery is not indicated for this patient, and progression of myelopathy during observation is an indication for surgical intervention.
A retrospective multicentre study from Japanese Organization of the Study for Ossification of Spinal Ligament reported prevalence of DISH in patients with cervical OPLL was 48.7%, with older age as significant correlating factor. Although there were various clinical and radiological feature of DISH cervical with OPLL, the pathogenesis is not fully understood [12]. Several studies reported cases without sign of neurological deficit or myelopathy were treated with conservative treatment and cases with sign of mild myelopathy and severe dysphagia are indication for surgery to prevent progression of disease. case report from Murayama et al. reporting a 70 years old man with severe dysphagia and mild myelopathy treated with anterior approach with corpectomy, discectomy and fusion with cage and posterior approach decompression and posterior stabilization lateral mass screw [13].
Strength of this study is patient first came to our institution with normal neurological status. From history taking, physical examination and imaging from x ray, CT and MR Cervical, we didn't find any sign of neurological destruction despite of large ossification and fusion in almost the entire cervical spine. Our limitation in this study, we followed up this patient by phone due to patient unwillingly control to our hospital fear of pandemic. After third time visited our polyclinic, we educate the patient to regularly report every 6 month or if they feel any sign of neurological disturbance. However, after several months patient never came back to our hospital since two years ago.
Declaration of competing interest
The authors declare that there is no conflict of interest regarding publication of this paper.
Acknowledgement
No conflict of interest regarding for the publication of this paper.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.amsu.2020.11.028.
Contributor Information
Fahmi Anshori, Email: fhmanshori@gmail.com.
Witantra Dhamar Hutami, Email: witantra.dhamar.h@gmail.com.
S.Dohar A.L. Tobing, Email: tobing.dohar@yahoo.com.
Ethical approval
This is a case report; therefore, it did not require ethical approval from ethics committee. However, we have got permission from the patient to publish his data.
Sources of funding
No sponsorship for this case report.
Author contribution
S Dohar AL Tobing contributes in the study concept or design, data collection, analysis and interpretation, oversight and leadership responsibility for the research activity planning and execution, including mentorship external to the core team
Witantra Dhamar Hutami contributes in the study concept or design, data collection, analysis and interpretation.
Fahmi Anshori contributes to the study concept or design, data collection and writing the paper.
Registration of Research Studies
This is a case report and not a first in man trial, thus registry is not needed.
Guarantor
S Dohar AL Tobing is the sole guarantor of this submitted article.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Baxi V., Gaiwal S. Diffuse idiopathic skeletal hyperostosis of cervical spine - an unusual cause of difficult flexible fiber optic intubation. Saudi J. Anaesth. 2010;66:379–384. doi: 10.1007/s12070-011-0334-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Verlaan J.J., Boswijk P.F.E., De Ru J.A., Dhert W.J.A., Oner F.C. Diffuse idiopathic skeletal hyperostosis of the cervical spine: an underestimated cause of dysphagia and airway obstruction. Spine J. 2011;11(11):1058–1067. doi: 10.1016/j.spinee.2011.09.014. [DOI] [PubMed] [Google Scholar]
- 3.Havelka S., Pavelkova A., Vesela M., Ruzickova S. Are DISH and OPLL genetically related. Ann. Rheum. Dis. 2001;60(9):902–903. [PMC free article] [PubMed] [Google Scholar]
- 4.Kalb S., Martirosyan N.L., Perez-Orribo L., Kalani M.Y.S., Theodore N. Analysis of demographics, risk factors, clinical presentation, and surgical treatment modalities for the ossified posterior longitudinal ligament. Neurosurg. Focus. 2011;30(3):1–9. doi: 10.3171/2010.12.FOCUS10265. [DOI] [PubMed] [Google Scholar]
- 5.Abiola R., Rubery P., Mesfin A. Ossification of the posterior longitudinal ligament: etiology, diagnosis, and outcomes of nonoperative and operative management. Global Spine J. 2015;6(2):195–204. doi: 10.1055/s-0035-1556580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Resnick D., Shaul S.R., Robins J.M. Diffuse Idiopathic Skeletal Hyperostosis (DISH): Forestier’s Disease with Extraspinal Manifestations. Radiology. 1975;115(3):513–524. doi: 10.1148/15.3.513. [DOI] [PubMed] [Google Scholar]
- 7.Sarzi-Puttini P., Atzeni F. New developments in our understanding of DISH (diffuse idiopathic skeletal hyperostosis) Curr. Opin. Rheumatol. 2004;16(3):287–292. doi: 10.1097/00002281-200405000-00021. [DOI] [PubMed] [Google Scholar]
- 8.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A.J., Orgill D.P. The SCARE 2018 statement: updating consensus Surgical case report (SCARE) guidelines. Int. J. Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 9.taljanovic M, Hunter Tim B, Wisneski Ronald J. Imaging characteristics of diffuse idiopathic skeletal hyperostosis with an emphasis on acute spinal fractures: Review. American Journal of Roentgenology. 2009;193(3 SUPPL):10–19. doi: 10.2214/AJR.07.7102. [DOI] [PubMed] [Google Scholar]
- 10.Dutta S, Biswas Das K, Mukherjee A. Dysphagia Due to Forestier Disease: Three Cases and Systematic Literature Review Sirshak. Indian Journal of Otolaryngology and Head and Neck Surgery. 2014;66(SUPPL.1):379–384. doi: 10.1007/s12070-011-0334-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Choi BW, Song KJ, Chang H. Ossification of the posterior longitudinal ligament: A review of literature. Asian Spine Journal. 2011;5(4):267–276. doi: 10.4184/asj.2011.5.4.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Murayama K, Inoe S, Tachibana T. Ossified posterior longitudinal ligament with massive ossification of the anterior longitudinal ligament causing dysphagia in a diffuse idiopathic skeletal hyperostosis patient. Medicine Clinical Case Report. 2015;94(32):1–6. doi: 10.1097/MD.0000000000001295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nishimura S, Nagoshi N, Iwanami A. Prevalence and Distribution of Diffuse Idiopathic Skeletal Hyperostosis on Whole-spine Computed Tomography in Patients with Cervical Ossification of the Posterior Longitudinal Ligament. Clinical Spine Surgery. 2018;31(9):E460–E465. doi: 10.1097/BSD.0000000000000701. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.