Abstract
Objective
This case report describes the effect of Cox flexion-distraction manipulation on a patient with a symptomatic L4-L5 extruded disc above an L5-S1 spondylolytic spondylolisthesis.
Clinical Features
A 40-year-old man presented to a chiropractor with complaints of acute low back pain and stiffness with pain and tingling radiating into the left leg and foot. Plain-film radiography revealed bilateral pars defects at L5, and magnetic resonance imaging revealed the L4-L5 disc extrusion.
Intervention and Outcome
Treatment consisted solely of Cox flexion-distraction for a total of 9 visits over a period of 4 weeks. The pain was assessed initially and at the end of care using a numeric scale of 0 to 10. At treatment conclusion, the original low back and radicular-type symptoms were no longer present, and the patient rated the pain as a 0 after an initial pain assessment of 9 on the 0-10 scale. After 10 years, a follow-up examination showed no orthopedic or neurologic deficits and no recurrence of the original symptoms.
Conclusion
This patient responded favorably to the chiropractic treatment provided. Cox flexion-distraction manipulation may be a viable nonsurgical treatment for similar symptomatic individuals with disc extrusions and concurrent spondylolytic spondylolisthesis.
Key Indexing Terms: Low Back Pain, Sciatica, Manipulation, Chiropractic, Spondylolisthesis
Introduction
Lumbar disc extrusions, a type of lumbar disc herniation (LDH), have often been considered a surgical condition by clinicians. Isthmic spondylolytic spondylolisthesis is the most common form of spondylolisthesis, caused by a defect in the pars interarticularis.1 Spondylolytic spondylolisthesis (SS) is a condition which may result in pain and disability for which surgical intervention, to fuse and stabilize the affected level, is a treatment option. Symptomatic individuals with both an LDH and concurrent SS may prove to be clinically challenging for many medical doctors and chiropractic physicians alike.
This case documents the improvement of a symptomatic 40-year-old man presenting with a noncontained extrusion-type LDH at L4-L5 immediately above an L5-S1 SS. Treatment consisted solely of Cox flexion-distraction manipulation a total of 9 times over a period of 1 month. A 10-year follow-up of the patient revealed no recurrences and normal orthopedic and neurologic status.
Case Report
History
A 40-year-old white man presented to a chiropractor certified in Cox flexion-distraction with complaints of severe, acute low back pain radiating into the left buttock and thigh with an ache in the calf and tingling in the toes. The man stated that the pain began 2 days prior when he bent forward while sitting in a chair, attempting to pick up a small item on the floor. The pain and associated stiffness immediately limited all lumbosacral ranges of motion and restricted activities of daily living.
The pain was initially rated a 9 on a numeric pain scale from 0 to 10, with 10 being the worst pain imaginable. The man's motion was significantly guarded, being limited by pain and lower back stiffness. He denied any loss of bowel or bladder control. No lower extremity weakness, foot drop, or abdominal complaints were noted. It should be noted that during the first 2 to 3 days after the injury, the man reported that he had taken over-the-counter NSAIDs (ibuprofen).
Examination
Physical examination showed a man 69 inches tall and weighing 175 pounds. No specific range of motion measurements were taken because of the pain, although attempted extension of the lumbosacral spine was noted as the most painful motion. All lumbosacral motions were reduced and guarded, and the man was in a slightly flexed, antalgic position. The Bechterew test (sitting straight leg rest) on the left produced an increase in low back pain, pain radiation into the left thigh, and increased tingling/numbness sensation on the dorsum of the left foot. The straight leg raise test at approximately 50° on the left caused increased low back and thigh pain and also numbness/tingling on the dorsal aspect of the left foot. Patellar and Achilles reflexes were equally responsive (2+) bilaterally. Sharp-dull testing produced an altered sensation (paresthesia) at the L5 dermatome on the left. Lower extremity muscle strength was strong (5 of 5) and equal bilaterally. The man was able to heel and toe walk, but heel walking on the left increased symptoms. Tenderness was noted at the L4-L5 and L5-S1 levels bilaterally. Hypertonicity was found in the lumbar paraspinal musculature and also in the gluteal muscles bilaterally. Lumbar spine plain-film radiographs were performed during the initial evaluation. The man decided on his own to have a lumbar spine magnetic resonance imaging (MRI), which was performed the following day.
Imaging
A 5-view plain-film x-ray series of the lumbar spine was obtained and demonstrated the following:
-
•
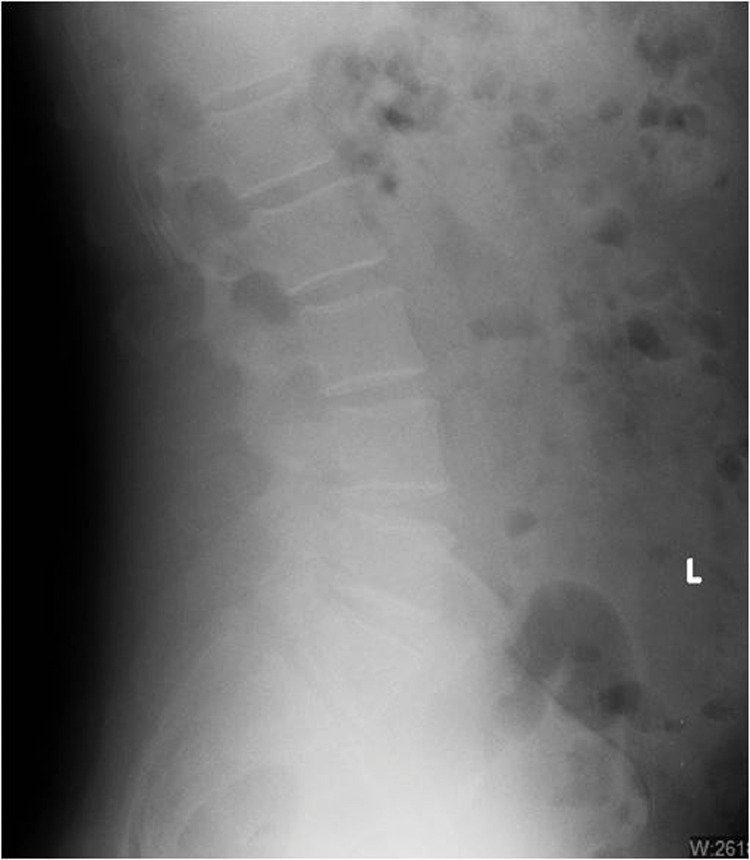
Mild degenerative disc disease at T11-T12, T12-L1, L4-L5, and L5-S1 (Fig 1)
-
•
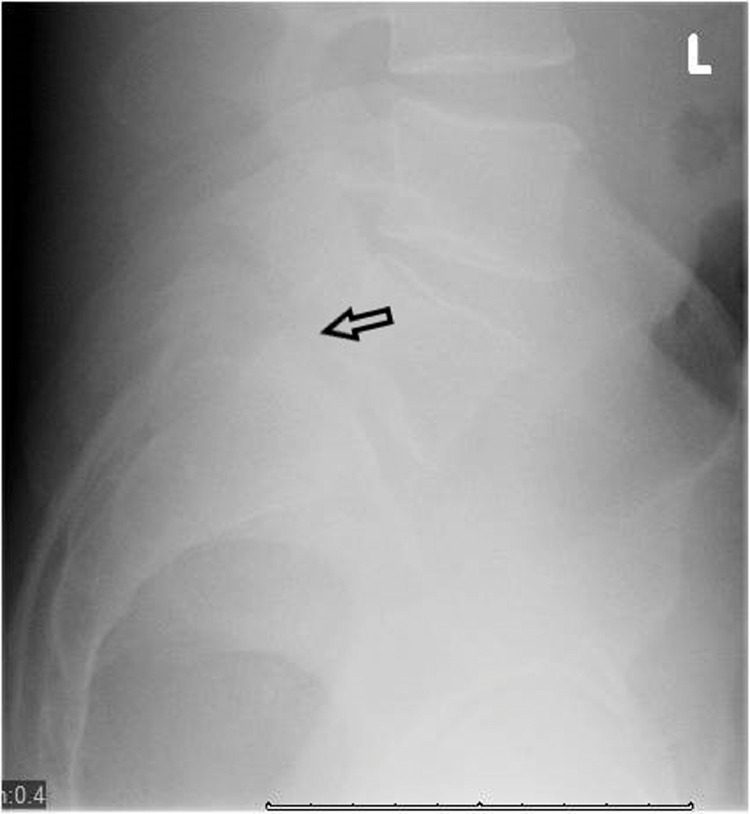
Bilateral L5 pars defects with grade 1 anterolisthesis of L5 on S1 (Fig 2)
-
•
Mild facet arthrosis at L5-S1
-
•
S1 spina bifida occulta
Fig 1.
Lateral lumbar x-ray shows mild multilevel degenerative disc disease.
Fig 2.
Lateral L5/S1 spot x-ray shows spondylolytic spondylolisthesis at L5-S1.
An MRI study consisting of T1-T2 sagittal and axial images of the lumbosacral spine showed the following:
-
•
A posterior disc prominence at L4-L5 measuring 4.0 mm in the anteroposterior dimension and 6.0 mm of inferior extension of the discal material through the annulus fibers that were not intact. (Fig 3, Fig 4)
-
•
Minor compression of the thecal sac with encroachment of the left L4-L5 intervertebral foramen (Fig 5)
-
•
Grade 1 spondylolytic spondylolisthesis at L5-S1 with bilateral intervertebral foramen stenosis and mild facet arthropathy (Fig. 3, 4, and 5)
Fig 3.
Sagittal MRI demonstrates L4-L5 disc extrusion.
Fig 4.
Sagittal MRI demonstrates L4-L5 herniated nucleus pulposus and L5-S1 anterolisthesis.
Fig 5.
Axial MRI demonstrates minor thecal sac compression and left intervertebral foramen stenosis at L4-L5.
Treatment
Treatment was initiated on the first visit and consisted of Cox flexion-distraction manipulation, which is a form of spinal decompression using hands-on manipulation. This technique uses a specialized adjusting table, where flexion and traction may be applied to a specific spinal level, for treatment of low back pain and radiculopathy. The treatment in this case, Cox protocol I, consisted of the doctor's hand contacting the spinous process of L4, above the affected disc, with the patient prone on the adjusting table.1 Three sets of 5 repetitions occurred of flexion of the caudal part of the table with a return to the treatment starting position. No other physical treatment modalities were used during the course of treatment. Treatment frequency was 3 times per week for 2 weeks, 2 visits during the third week, and 1 during the fourth week.1 The patient was informed that a referral for a surgical consultation would be made if progressive subjective and objective improvement was not achieved according to Cox Technic protocol.1
Outcome
During the course of treatment, the patient reported progressive relief of his pain and stiffness and improvement of the initially limited activities of daily living. On the ninth (final) visit, approximately 4 weeks after beginning treatment, he reported a pain level of 0 on the 0-to-10 pain scale. The final examination on the last visit revealed full and pain-free lumbar ranges of motion and no abnormalities with lumbar orthopedic or lower extremity neurologic testing.
On a follow-up visit 10 years after the conclusion of care, the man reported no recurrence of the low back or lower extremity symptoms previously related to his L4-L5 disc herniation. Orthopedic and neurologic testing on reexamination produced no abnormal findings or complaints. The patient in this study gave permission to have his personal health information published in this study.
Discussion
Lower back pain is a worldwide dilemma, with annual costs exceeding $100 billion in the United States alone. It is estimated that approximately 80% of individuals will suffer from lower back pain at least once in their lifetime, with the most common causes being degenerative disc disease and LDH.2 Deyo and Mirza write that in addition to LDH, disorders that must be included in the differential diagnosis of lower back pain with radiculopathy are spondylolisthesis, lumbar stenosis, spinal tumors, synovial cysts, vertebral fracture, and diabetic mononeuropathy.3
LDH can be classified as a bulging disc, a protrusion (contained herniation), an intervertebral endplate herniation (Schmorl node), or a noncontained disc (extrusion or sequestration).4 Spinal disc extrusions with sequestration, such as the noncontained LDH in this case, occur when the annular fibers no longer contain the nucleus pulposus, and the fragmented disc material is able to migrate. Although an extrusion or sequestration is usually indicative of greater insult to the disc compared with a contained disc, several studies have demonstrated that noncontained discs typically have superior outcomes in comparison to contained discs and are better managed with conservative treatment rather than surgical intervention.5,6 Daghighi et al found in a study of over 1000 patients with extruded discs that almost 75% of the cases involved a caudal migration of the fragment, and caudally migrated extrusions were more frequently associated with radiculopathy.7 The present case was representative of a caudally migrated disc extrusion with associated radicular symptoms.
Spondylolysis is a defect in the pars interarticularis on either 1 or both sides of a lumbar vertebra, with over 90% of these defects occurring at the L5 level.8 Liu et al report that lumbar SS most commonly occurs at only 1 spinal level and is typically associated with heavy labor, trauma, sports injuries, or Albers-Schönberg disease.9 Spondylolytic or true spondylolisthesis occurs when 1 vertebra slips forward on the segment below due to the pars interarticularis fracture. The primary concern with an SS is lumbar spine instability. Spondylolistheses can cause pain in the lower back and lower extremity, in addition to weakness and numbness in the lower extremity.10 Lumbosacral spondylolistheses have been found to have a negative impact on physical and mental health-related quality of life.11
Plain-film x-ray imaging that includes anteroposterior, lateral, and oblique views has proven to be useful in identifying pars defects. MRI is an effective imaging method to study degenerative disc disease and disc herniations. It is in fact considered the gold standard in evaluating disc pathology owing to the superior quality of soft-tissue visualization, the ability to view the structures in multiple planes, and the lack of radiation dosage to the patient.12 In this case, both plain-film radiographs and MRI were utilized to correlate with the clinical findings.
Different protocols have been used to treat LDH, ranging from noninvasive therapies to invasive surgical methods. Current literature favors nonsurgical management in most cases of LDH.2,5,6,13 Nonsurgical treatment regimens may include nonsteroidal anti-inflammatory drugs, epidural steroid injections, mesenchymal stem cell therapy, platelet-rich plasma injection, physical therapy, exercise, traction therapy, acupuncture, chiropractic spinal manipulation, and patient education.2,14 Lumbosacral manipulation and therapeutic exercise have been effective in treating LDH associated with low back pain and radicular symptoms.1 Flexion-distraction manipulation has been demonstrated to be a highly effective nonsurgical option for successful management of LDH.15,16 Gudavalli et al found that patients with lumbar radiculopathy had significantly greater improvement and reduction of pain compared with individuals who were conservatively treated with active trunk exercises alone.17
Dunn et al conclude that the in the absence of significant neurologic deficit, conservative care is the standard of care for spondylolysis with a grade 1 or 2 spondylolisthesis.18 SS in young adults and in athletes responds favorably to nonsurgical care, with a significant reduction in pain and good long-term outcomes in nearly 80% of cases.19 Longo et al report that most patients with spondylolistheses experience satisfactory results with nonsurgical care, and surgery should be considered only in patients with “high-grade slippage” (greater than 50%) with persistent neurologic symptoms or pain in the lower back or leg, those with persistent signs of neurogenic claudication, and those who have failed to improve with a minimum of 3 months of conservative, nonsurgical care.20 Successful conservative care options for the treatment of SS include modification of activities, therapeutic exercises, and traction, in addition to spinal manipulative therapy and flexion-distraction manipulation applied above and below the involved spinal level.18 Fedorchuk et al also describe conservative care for the treatment of SS as including patient education, active physical therapy, nonsteroidal anti-inflammatory drugs, soft-tissue methods, and homeopathic remedies, in addition to spinal mobilization and chiropractic care applied to specific regions of the spine.21
Common surgical procedures for LDH include microdiscectomy, open discectomy, decompression, intertransverse process fusion, segmental pedicle screw fixation, transforaminal lumbar interbody fusion, lumbar foraminoplasty, posterior lumbar interbody fusion, and anterior lumbar interbody fusion with or without PEEK cage and posterior pedicle screw fixation.2,22 Koenders et al report that lumbar spinal fusion, with or without decompression, did not render superior outcomes over nonsurgical treatments regarding pain, degenerative spondylosis, or cost-effectiveness.22 Additionally, lumbar surgical procedures are associated with several unacceptable complications such as infection, neurologic complications including dural tear and nerve root injury, and a surprising incidence of recidivism and subsequent revision surgery.22,23 Common surgical procedures for the stabilization of spondylolistheses include spinal arthrodesis and reduction in situ; however, both procedures have been associated with complications such as pseudoarthrosis, neurologic deficits, failure of instrumentation requiring revision surgery, deep wound infection, dural tear, urinary retention, thrombosis, pulmonary embolus, and increased regional back pain.20
It should be noted that in addition to conservative care and surgical intervention, LDHs have been known to spontaneously regress. The regression of the herniated nuclear material is thought to be due to the inflammatory infiltration, neovascularization, and granulation of the protruded discs and phagocytosis of the extruded or sequestered disc material.24 The inflammation associated with LDHs is a common causative factor regarding low back pain but is also thought to be the main factor responsible for the regression of the herniated nuclear material.5,6,13,24
The occurrence of LDH is often present in the population of individuals with sciatica or low back pain. Treatment for this condition includes both surgical and nonsurgical procedures. Current clinical reasoning dictates that all nonsurgical treatments for acute LDH should be exhausted before considering surgery owing to the efficacy of conservative treatments and the incidence of spontaneous LDH regression.5,13 Benson et al report that patients seeking a surgical consultation too early in the treatment of an acute LDH may result in unnecessary surgical procedures, and that patients who received conservative care for herniated discs had a 90% satisfaction rate upon 7-year follow-up, compared with a 50% satisfaction rate for operative patients.6 This report was meant to discuss the results of a single case of a symptomatic L4-L5 disc extrusion causing radicular symptoms above a concurrent L5-S1 SS. A surgical consultation was not recommended for this patient because of the progressive subjective and objective improvement throughout the course of care. Based on the encouraging results of this case study, including the long-term 10-year follow-up, management of similar cases using the Cox flexion-distraction method of chiropractic manipulation may be a viable treatment option. Further appropriate studies regarding this conservative, nonsurgical option need to be performed.
Limitations
This case study reports on the use of Cox flexion-distraction manipulation for treating a symptomatic L4-L5 disc extrusion above an L5-S1 spondylolytic spondylolisthesis. Because it reflects the outcome of only 1 case being treated by the Cox flexion-distraction method, it may be of limited value. Another possible reason for the positive outcome is that the symptoms were self-limiting. All authors are certified in Cox Technic, but there was no notable source of bias.
Conclusion
The patient in this case responded favorably to the chiropractic treatment provided. Cox flexion-distraction manipulation may be a viable nonsurgical treatment for similar symptomatic individuals with disc extrusions and concurrent spondylolytic spondylolisthesis.
Acknowledgments
Acknowledgments
Sharina Gudavalli was the treating physician of this patient and was previously involved in the writing of this case report before she passed away.
Funding Sources and Conflicts of Interest
No funding sources or conflicts of interest were reported for this study.
Contributorship Information
Concept development (provided idea for the research): R.A.K., S.G.
Design (planned the methods to generate the results): S.G.
Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): R.A.K., B.A.W.
Data collection/processing (responsible for experiments, patient management, organization, or reporting data): S.G.
Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results): R.A.K., B.A.W.
Literature search (performed the literature search): R.A.K., B.A.W.
Writing (responsible for writing a substantive part of the manuscript): R.A.K., B.A.W.
Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): BA.W.
Practical Applications.
-
•
This is a case of conservative chiropractic treatment of a patient with both a disc extrusion and spondylolytic spondylolisthesis. Results for similar cases have not been reported previously, and thus this case study adds to the literature on conservative management of such conditions. This knowledge has implications for the treatment of similar cases in private practice and possible larger research studies.
Alt-text: Unlabelled box
References
- 1.Cox JM. Spondylolisthesis. In: Cox JM, editor. Low Back Pain: Mechanism, Diagnosis, and Treatment. 7th ed. Lippincott Williams & Wilkins; Philadelphia, PA: 2011. pp. 533–577. [Google Scholar]
- 2.Amin RM, Andrade NS, Neuman BJ. Lumbar disc herniation. Curr Rev Musculoskelet Med. 2017;10(4):507–516. doi: 10.1007/s12178-017-9441-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Deyo RA, Mirza SK. Herniated lumbar intervertebral disk. N Engl J Med. 2016;374(18):1763–1772. doi: 10.1056/NEJMcp1512658. [DOI] [PubMed] [Google Scholar]
- 4.Ehrler M, Peterson C, Leemann S, Schmid C, Anklin B, Humphreys BK. Symptomatic, MRI confirmed, lumbar disc herniations: a comparison of outcomes depending on the type and anatomical axial location of the hernia in patients treated with high-velocity, low-amplitude spinal manipulation. J Manipulative Physiol Ther. 2016;39(3):192–199. doi: 10.1016/j.jmpt.2016.02.013. [DOI] [PubMed] [Google Scholar]
- 5.Cunha C, Silva AJ, Pereira P, Vaz R, Gonçalves RM, Barbosa MA. The inflammatory response in the regression of lumbar disc herniation. Arthritis Res Ther. 2018;20(1):251. doi: 10.1186/s13075-018-1743-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Benson RT, Tavares SP, Robertson SC, Sharp R, Marshall RW. Conservatively treated massive prolapsed discs: a 7-year follow-up. Ann R Coll Surg Engl. 2010;92(2):147–153. doi: 10.1308/003588410X12518836438840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Daghighi MH, Pouriesa M, Maleki M, Fouladi DF, Pezeshki MZ, Khameneh RM, Bazzazi AM. Migration patterns of herniated disc fragments: a study on 1,020 patients with extruded lumbar disc herniation. Spine J. 2014;14(9):1970–1977. doi: 10.1016/j.spinee.2013.11.056. [DOI] [PubMed] [Google Scholar]
- 8.Xing R, Dou Q, Li X. Posterior dynamic stabilization with direct pars repair via Wiltse approach for the treatment of lumbar spondylolysis: the application of a novel surgery. Spine (Phila Pa 1976) 2016;41(8):E494–E502. doi: 10.1097/BRS.0000000000001295. [DOI] [PubMed] [Google Scholar]
- 9.Liu X, Wang L, Yuan S, Tian Y, Zheng Y, Li J. Multiple-level lumbar spondylolysis and spondylolisthesis. J Neurosurg Spine. 2015;22(3):283–287. doi: 10.3171/2014.10.SPINE14415. [DOI] [PubMed] [Google Scholar]
- 10.Ahn K, Jhun H.-J. New physical examination tests for lumbar spondylolisthesis and instability: low midline sill sign and interspinous gap change during lumbar flexion-extension motion. BMC Musculoskelet Disord. 2015;16(1):97. doi: 10.1186/s12891-015-0551-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gussous Y, Theologis AA, Demb JB, Tangtiphaiboontana J, Berven S. Correlation between lumbopelvic and sagittal parameters and health-related quality of life in adults with lumbosacral spondylolisthesis. Global Spine J. 2018;8(1):17–24. doi: 10.1177/2192568217696692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Suthar P, Patel R, Mehta C, Patel N. MRI evaluation of lumbar disc degenerative disease. J Clin Diagn Res. 2015;9(4):TC04–TC09. doi: 10.7860/JCDR/2015/11927.5761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim SG, Yang JC, Kim TW, Park KH. Spontaneous regression of extruded lumbar disc herniation: three cases report. Korean J Spine. 2013;10(2):78–81. doi: 10.14245/kjs.2013.10.2.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thackeray A, Fritz JM, Lurie JD, Zhao W, Weinstein JN. Non-surgical treatment choices by individuals with lumbar intervertebral disc herniation in the United States: associations with long-term outcomes. Am J Phys Med Rehabil. 2017;96(8):557–564. doi: 10.1097/PHM.0000000000000685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oh H, Lee S, Lee K, Jeong M. The effects of flexion-distraction and drop techniques on disorders and Ferguson's angle in female patients with lumbar intervertebral disc herniation. J Phys Ther Sci. 2018;30(4):536–539. doi: 10.1589/jpts.30.536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Choi J, Hwangbo G, Park J, Lee S. The effects of manual therapy using joint mobilization and flexion-distraction techniques on chronic low back pain and disc heights. J Phys Ther Sci. 2014;26(8):1259–1262. doi: 10.1589/jpts.26.1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gudavalli MR, Cambron JA, McGregor M, Jedlicka J, Keenum M, Ghanayem AJ, Patwardhan AG. A randomized clinical trial and subgroup analysis to compare flexion-distraction with active exercise for chronic low back pain. Eur Spine J. 2006;15(7):1070–1082. doi: 10.1007/s00586-005-0021-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dunn AA, Baylis S, Ryan D. Chiropractic management of mechanical low back pain secondary to multiple-level lumbar spondylolysis with spondylolisthesis in a United States Marine Corps veteran: a case report. J Chiropr Med. 2009;8(3):125–130. doi: 10.1016/j.jcm.2009.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Madhavan K, Chieng LO, Hofstetter CP, Wang MY. Transforaminal endoscopic discectomy to relieve sciatica and delay fusion in a 31-year-old man with pars defects and low-grade spondylolisthesis. Neurosurg Focus. 2016;40(2):E4. doi: 10.3171/2015.11.FOCUS15512. [DOI] [PubMed] [Google Scholar]
- 20.Longo UG, Loppini M, Romeo G, Maffulli N, Denaro V. Evidence-based surgical management of spondylolisthesis: Reduction or arthrodesis in situ. J Bone Joint Surg. 2014;96(1):53–58. doi: 10.2106/JBJS.L.01012. [DOI] [PubMed] [Google Scholar]
- 21.Fedorchuk C, Lightstone DF, McRae C, Kaczor D. Correction of grade 2 spondylolisthesis following a non-surgical structural spinal rehabilitation protocol using lumbar traction: a case study and selective review of literature. J Radiol Case Rep. 2017;11(5):13–26. doi: 10.3941/jrcr.v11i5.2924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Koenders N, Rushton A, Verra ML, Willems PC, Hoogeboom TJ, Staal JB. Pain and disability after first-time spinal fusion for lumbar degenerative disorders: a systematic review and meta-analysis. Eur Spine J. 2019;28(4):696–709. doi: 10.1007/s00586-018-5680-3. [DOI] [PubMed] [Google Scholar]
- 23.Lurie JD, Tosteson TD, Tosteson A. Surgical versus non-operative treatment for lumbar disc herniation: eight-year results for the Spine Outcomes Research Trial (SPORT) Spine (Phila Pa 1976) 2014;39(1):3–16. doi: 10.1097/BRS.0000000000000088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ikeda T, Nakamura T, Kikuchi T, Umeda S, Senda H, Takagi K. Pathomechanism of spontaneous regression of the herniated lumbar disc: histologic and immunohistochemical study. J Spinal Disord. 1996;9(2):136–140. [PubMed] [Google Scholar]