Abstract
Background: Trocar-site hernias (TSHs) are an uncommon but potentially severe complication of robot-assisted urologic surgery, with an incidence of incarcerated hernias varying from 0.4% to 0.66%. Currently, there are no standardized guidelines on trocar site fascial closure. Although it is widely recommended to close the midline 12-mm port site, there is no agreement on the need for fascial closure of lateral port sites, especially if ≤12 mm.
Cases Presentation: We report three cases of incarcerated intestinal TSHs in the past 10 years in our institution. All were from lateral abdominal ports (two 12 and one 8 mm), after robot-assisted radical prostatectomy. Patients were Caucasian and from 60 to 71 years; symptoms varied widely from obstinate hiccups, abdominal distention with fever, to acute abdomen. In all cases reduction of the herniated loop from the outside, using a minilaparotomy over the port site, was safe and effective. However, in one case bowel resection for bowel ischemic necrosis was necessary. No specific clinical risk factors could be identified in our cases.
Conclusion: Incarcerated TSH after robotic urologic surgery may arise from any trocar site, regardless of size and location. This could be treated effectively with a minilaparotomy over the trocar site, to avoid more serious life-threatening consequences such as bowel necrosis and perforation. No risk factor seems to be predictive of TSHs.
Keywords: trocar-site hernia, robotic surgery, minimally invasive surgery, robotic complications
Introduction and Background
Trocar-site hernias (TSHs) are rare, but they can be a potential cause of major complications of laparoscopic and robotic procedures, causing possible severe postoperative morbidity. Herniation and strangulation of a bowel segment through a port site can occur during trocars removal or release of the pneumoperitoneum at the end of the operation, or during removal of surgical drains.
In robot-assisted urologic surgery, the incidence of incarcerated TSH varies from 0.4% to 0.66%, but the rate of asymptomatic radiographically demonstrated TSH is higher and it has been correlated to trocar size, being unusual in ports ≤10 mm (0%–0.09%), or to trocar location, with higher risk in midline/periumbilical ports.1–3 In our experience, 2138 robotic procedures were performed between January 2010 and January 2020, 1531 of which were robot-assisted radical prostatectomies (RARPs).
On these series, we are reporting three cases of incarcerated intestinal TSH (3 out of 2138 total robotic cases, 0.14%), all of which occurred after RARP (3/1531 RARPs, 0.19%) and all originating from the lateral abdominal ports (two 12 and one 8 mm).
Surgical technique
RARPs were performed with the 4-arm DaVinci Si or, in the past 2 years, Xi Surgical System (Intuitive Surgical, Inc., Sunnydale, CA). A transperitoneal approach was used in all cases. The patient is positioned supine on the operating table, with a 30° Trendelenburg position. Bladeless trocars have been used in all cases, and six ports: a 1.5 cm supraumbilical incision is performed on midline and a 12-mm trocar is placed for laparoscope (8 mm in case of Da Vinci Xi); then three 8-mm robotic ports and two 12-mm assistant ports are placed. At the end of the procedure, a tubular drainage is inserted through the left inferior lateral robotic trocar site. All trocars are then removed under vision. The specimen is removed through a 2 cm enlargement of the 12-mm periumbilical port, and the fascia is sutured only at this level.
Presentation of Cases
The first patient is a 70-year-old Caucasian man who underwent RARP in March 2014. His body mass index (BMI) was 25.7 and the Charlson comorbidity index (CCI) was 1. Two years before, he had undergone a right laparoscopic radical nephrectomy for renal cancer.
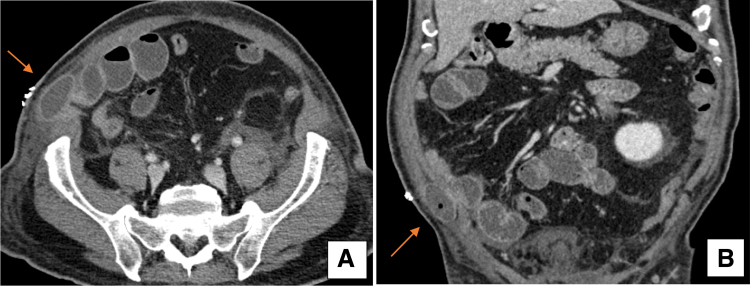
The surgical approach was completed with the 4-arm DaVinci Si Surgical System, without intraoperative issues. Four days after surgery, the patient developed abdominal distention, nausea, and fever. He had no flatus passage and no bowel sounds at abdominal auscultation, with a progressive raise of white blood cells up to 13 × 109/L. On physical examination, there was no palpable bulge or visible changes at the level of the trocar sites. A contrast-enhanced abdominopelvic CT was performed, which revealed a bowel obstruction secondary to an incarcerated ileal loop, herniated through a fascial defect at the level of the inferior right 12-mm trocar site (Fig. 1A, B). The patient underwent a 3-cm minilaparotomy, extending medially the right lateral trocar incision; the ileal loop, incarcerated in the fascial defect, was visible from the outside, and appeared vital, without signs of perforation. The loop was carefully reduced inside the peritoneal cavity and the fascial defect was repaired. The postoperative course was regular and the patient was discharged 4 days later.
FIG. 1.
Abdominal CT images of the first case, showing an incarcerated bowel loop at the level of the right lateral 12-mm trocar port site. The bowel loop is visible in the axial (A) and coronal (B) views, indicated by the arrows.
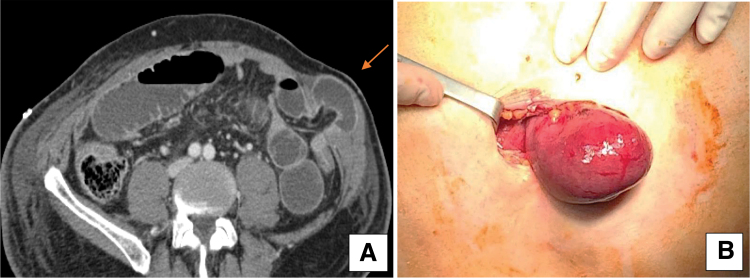
The second case occurred in September 2017. The patient was a 60-year-old Caucasian man who underwent RARP with the 4-arm DaVinci Si Surgical System, without intraoperative issues. His BMI was 20.1 and CCI was 1; he had no history of previous abdominal surgical procedures. On the fourth postoperative day, the patient presented severe asthenia, fever, abdominal pain, and bloating in the left quadrants. After a few hours he started vomiting. Laboratory studies revealed rise of white blood cells up to 18 × 109/L. On physical examination, there was a palpable, tender, and painful swelling on the site of the previous drainage at the level of the left lateral 8-mm inferior robotic port, with overlying skin erythema. Abdominal CT showed a herniated ileal loop through the fascia at the 8-mm robotic left inferior port site (Fig. 2A). We performed a 3-cm minilaparotomy over the port site, extending medially the previous trocar incision. On exploration, a 5-cm ileal loop appeared, herniated through the fascia: the loop was ischemic (Fig. 2B). The bowel was carefully pushed back into the abdomen. An additional midline subumbilical incision was added, the ischemic loop was identified and kept under a warm gauze for 5 minutes, without signs of returned blood flow; a 15-cm ileum resection was then necessary, followed by a manual anastomosis. The abdominal herniation site and the median incision were closed. The postoperative course was uneventful and the patient was discharged 4 days later.
FIG. 2.
The second case presented a left lateral inferior 8-mm port-site TSH, diagnosed with an abdominal CT scan (A): axial view, shown by the arrow. A minilaparotomy over the port site showed a herniated ischemic bowel loop (B). TSH, trocar-site hernia.
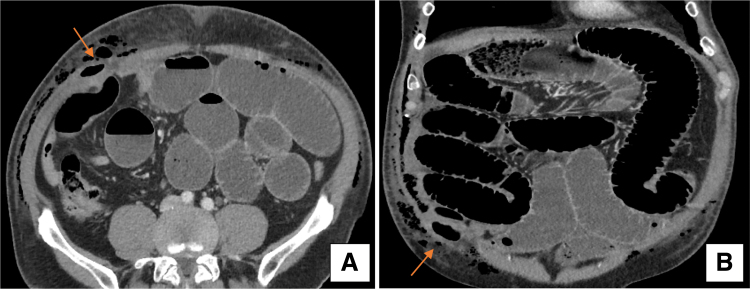
The last patient was a 71-year-old Caucasian man who underwent RARP on February 2019. His BMI was 24.5 and he had a CCI of 2. He had no history of previous abdominal surgery. The surgical procedure had been performed with the 4-arm DaVinci Xi Surgical System. On the first postoperative day, he started having continuous hiccups. Upon examination, the abdomen was tender without suspicious bulges and the patient had passed stools. He had no fever, a normal leukocyte count, normal lactic acid level (0.8 μmol/L), mild elevation of C-reactive protein to 50.7 mg/L, and elevated serum creatinine up to 152 μmol/L. A contrast-enhanced abdominal CT revealed mechanical ileus, with luminal distention at the right quadrants, where the bowel was trapped in a wall defect at the level of the inferior right 12-mm port site (Fig. 3A, B). A quick laparoscopic procedure was performed, which confirmed the herniated loop through a fascial defect at the pararectal right trocar site (the 12-mm port site used for the AirSeal® Dynamic Pressure System). The loop appeared viable. An attempt to reduce the herniated loop from the inside was unsuccessful. A 3-cm minilaparotomy over the right lateral incision was then performed, and the bowel was manually reduced in the abdomen. The fascial defect was closed and the patient was discharged 3 days later.
FIG. 3.
Abdominal CT images of the third case, showing an incarcerated bowel loop at the level of the right lateral 12-mm AirSeal® trocar-site. The bowel loop is incarcerated inside the abdominal wall (A, axial view; B, coronal view), as shown by the arrows.
Clinical features of the three cases are summarized in Table 1.
Table 1.
Clinical Data of Incarcerated Trocar-Site Hernias After Robot-Assisted Radical Prostatectomy: 10-Year Experience (3/1531 Cases, 0.19%)
| Case | Year | Age | BMI | CCI | DaVinci robot | OT (minute) | Port site | POD | Clinical presentation | Necrosis | WC | CRP (mg/L) | Lactic acid (μmol/L) | Treatment |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2014 | 70 | 25.7 | 1 | Si | 200 | 12-mm right inferior | 3 | Nausea, fever, abdominal distention | No | 13 × 109/L | 145 | 0.3 | Minilaparotomy + reduction of bowel loop + fascial closure |
| 2 | 2017 | 60 | 20.1 | 1 | Si | 180 | 8-mm left inferior | 4 | Severe asthenia, abdominal pain, vomit | Yes | 18 × 109/L | 180 | 2 | Minilaparotomy + reduction of bowel loop + intestinal resection (midline incision) |
| 3 | 2019 | 71 | 24.5 | 1 | Xi | 210 | 12-mm right inferior (AirSeal®) | 4 | Hiccups | No | 8 × 109/L | 51 | 0.8 | Minilaparotomy + reduction of bowel loop + fascial closure |
BMI, body mass index; CCI, Charlson comorbidity index; CRP, C-reactive protein; OT, operative time; POD, postoperative day; WC, white cell count.
Discussion
TSH is an uncommon but potentially severe complication of laparoscopic or robotic surgery, in case of incarcerated intestinal hernias. Available data show an incidence of 0.4%–0.9% after RARP2. The risk factors associated with TSH have not been clearly identified, and could be surgical factors, such as type of trocar (bladed or not), trocar size, port location, fascial closure, intraoperative manipulation and operative time, or patient-related factors, such as age, obesity, presence of wound infection, and nutritional status. A study has identified size (>12 mm), type of trocar and longer surgery as the main risk factors for TSH.3 These risk factors were not present in all our cases. As shown in Table 1, we could not identify any parameter linked to the incidence of TSH: age, BMI, CCI, operative time, trocar size and site, clinical signs. Moreover, one case presented severe hiccups, a symptom not reported so far in previous experiences.
The need for correct fascial closure at the trocar site level remains a controversial issue, especially regarding the lateral port sites: the multiple layers of musculature in the lateral abdominal quadrants should coapt after release of pneumoperitoneum and trocars removal.1 Therefore, there should be no need to close the fascia at the lateral ports level.2 Recently, however, a case of incarcerated TSH at the lateral port site after RARP has been reported.4 A number of laparoscopic studies recommend closure of all port sites ≥10 mm (at umbilical or off-midline site): Chiong et al. retrospectively reviewed 1055 laparoscopic urologic procedures, reporting seven TSHs, six of which were located at the 12-mm lateral port sites.2 Other studies, however, do not recommend fascial closure of nonmidline port sites ≤12 mm, particularly when created with bladeless splitting (rather than cutting) trocars.1
In our institution, 1531 RARPs were performed between 2010 and 2020, with three reported incarcerated TSHs (0.19%): two of these cases occurred at the inferior right lateral 12-mm port site; one at the inferior left lateral 8-mm site. All cases required immediate surgery, with bowel resection in one case (8-mm port site hernia). Therefore, in our experience, incarcerated TSH happened only through the lateral ports, <10 mm in one case. We could suggest some practical tips to prevent this complication: fascial closure of all port sites; removal of all ports under vision; do not remove the trocars before reducing the pneumoperitoneum; finally, pay attention during removal of the abdominal drain.
In all our cases, reduction of the herniated loop from the outside, using a minilaparotomy over the port site, was possible. This maneuver seems to be safe and effective, even in the third case, when laparoscopic reduction of the herniated loop from the inside was not possible.
Conclusions
Incarcerated TSHs after robotic urologic surgery are rare but should be considered as a differential diagnosis among patients with prominent abdominal complaints postoperatively.
A high index of suspicion is key to its timely diagnosis and treatment. Furthermore, meticulous fascial closure after the robotic surgery is essential to prevent this potential life-threatening complication.
Abbreviations Used
- BMI
body mass index
- CCI
Charlson comorbidity index
- CRP
C-reactive protein
- CT
computed tomography
- OT
operative time
- POD
postoperative day
- RARP
robot-assisted radical prostatectomy
- TSHs
trocar-site hernias
- WC
white cell count
Disclosure Statement
No competing financial interests exist.
Funding Information
No funding was received for this article.
Cite this article as: Mancini M, Righetto M, Dal Moro F, Zattoni F (2020) Incidence and treatment of incarcerated trocar-site hernias after robotic surgery: presentation of three cases, Journal of Endourology Case Reports 6:4, 271–274, DOI: 10.1089/cren.2020.0110.
References
- 1. Kang D, Woo SH, Lee DH, et al. Incidence of port-site hernias after robot-assisted radical prostatectomy with the fascial closure of only the midline 12-mm port site. J Endourol 2012;26:848–851 [DOI] [PubMed] [Google Scholar]
- 2. Chiong E, Hegarty PK, Davis JW, et al. Port-site hernias occurring after the use of bladeless radially expanding trocars. Urology 2010;75:574–580 [DOI] [PubMed] [Google Scholar]
- 3. Swank HA, Mulder M, La Chapelle CF, et al. Systematic review of trocar-site hernia. Br J Surg 2012;99:315–323 [DOI] [PubMed] [Google Scholar]
- 4. Kocher NJ, Ilinsky D, Raman JD. Incarcerated right lateral trocar-site hernia as a rare complication of robot-assisted laparoscopic prostatectomy. J Endourol 2017;3:155–157 [DOI] [PMC free article] [PubMed] [Google Scholar]