Background:
Open arthrolysis is used for treating elbow stiffness in adults. This study evaluated the midterm outcomes after open arthrolysis in children and adolescents with posttraumatic elbow stiffness.
Methods:
Data of 31 children and adolescents with posttraumatic elbow stiffness following open arthrolysis with or without hinged external fixation from 2010 to 2014 were retrospectively analyzed. Their mean age was 15 (range: 6 to 19) years. At baseline and the follow-up (>4 y), we evaluated the outcomes (range of motion and Mayo Elbow Performance Index) and postoperative complications (pain, ulnar nerve symptoms, infections, and instability) and analyzed the association between outcomes and clinical variables.
Results:
The Mayo Elbow Performance Index improved from 67.9 (range: 35 to 95 points) to 93.7 points (range: 65 to 100 points; P<0.001). The elbow active flexion/extension arc increased significantly from 49 degrees (range: 0 to 120 degrees) to 108 degrees (range: 0 to 120 degrees; P<0.001), with a mean flexion of 123 degrees (range: 70 to 140 degrees; P<0.001) and mean extension of 15 degrees (range: 0 to 85 degrees; P<0.001) postoperatively. The increasing age at surgery was associated with improved elbow motions (P=0.004). Patients with increased preoperative serum alkaline phosphatase level demonstrated decreased arc of motion (P=0.015). Patients with extra-articular fractures had better outcomes than the other patients. At the final follow-up, 8 patients experienced recurrent contracture in the flexion arc with heterotopic ossification. Two patients had postoperative pain, 1 elbow instability, and 1 ulnar neuropathy.
Conclusions:
Most patients showed satisfactory functional outcomes after arthrolysis, indicating that open release with or without hinged external fixation is an effective and maintained technique for children and adolescents with posttraumatic elbow stiffness. The age at surgery, preoperative alkaline phosphatase level, and injury type should be considered to achieve good outcomes.
Level of Evidence:
Therapeutic level III.
Key Words: elbow ankylosis, posttraumatic, arthrolysis, children, adolescent, stiffness
Elbow stiffness commonly occurs after elbow trauma; it is defined as an elbow range of motion (ROM) of 30 to 130 degrees, which is adequate for performing most activities of daily living.1–3 There are different options in treating posttraumatic elbow stiffness, that is, mainly nonoperative and operative methods.4,5 In previous studies, open arthrolysis and hinged external fixation have been reported as an effective procedure for adult patients with elbow stiffness; similar good outcomes have also been reported in other studies.6–9 Meanwhile the application of hinged external fixator after ligament repair is necessary for unstable elbows to maintain elbow stability, resist shearing and varus-valgus force, recover the ligament, and to improve the efficacy of daily rehabilitation.10 However, the literature reporting posttraumatic stiffness in the elbows of pediatric and adolescent patients is limited and controversial.9,11,12 Stans et al11 found that the outcomes of open surgery for elbow stiffness in young patients were less favorable and less predictable than those in adult patients, whereas Ek et al13 demonstrated that the significant improvement in elbow motion was as good as that in adults. Although some factors had been found to affect the final outcomes of open release, such as type of injury, comatose condition, and radial head replacement, there have been contradicting findings on the age at surgery and the impact of serum alkaline phosphatase (AKP) levels in children and adolescents with posttraumatic elbow stiffness.6,12 Orzel and Rudd suggested that the serum AKP level was associated with heterotopic ossification (HO) while Citak and colleagues questioned the correlation.14,15 Moreover, to our knowledge, no related study has evaluated the midterm (≥4 y) outcomes after open arthrolysis in children and adolescents with elbow stiffness, considering that elbow injuries in children are relatively frequent, and the consequences greatly impact their quality of life. Herein, we evaluated the midterm outcomes after open arthrolysis in patients aged below 20 years with posttraumatic elbow stiffness and analyzed the prognostic factors influencing final clinical outcomes.
METHODS
After obtaining approval from our Institutional Review Board, we investigated 31 children and adolescents who underwent open arthrolysis combined with hinged external fixation for elbow contractures at our institution from January 2010 to December 2014. The inclusion criteria in this retrospective study were as follows: (1) age below 20 years, (2) unimproved posttraumatic elbow stiffness and arc of <100 degrees despite conservative treatment, and (3) follow-up duration of >4 years. Patients were excluded from the study if their elbow stiffness resulted from brain injuries, burns, and synovitis.
The demographic information of all patients is indicated in Table 1. The study group included 20 male patients and 11 female patients with a mean age of 15 (range: 6 to 19) years at the time of surgery; the mean age at the time of injury was 13 (range: 3 to 19) years. The mean interval from injury to surgery was 32.1 (range: 5 to 144) months. Three patients had a simple dislocation, and the 28 remaining patients included had a fracture of the radial head, proximal ulna, or distal humerus. Thirteen had an extra-articular fracture, and 11 had an intra-articular fracture. Four had a complex fracture dislocation.
TABLE 1.
Patient Demographics
| Age at surgery* (y) | 15 (6-19) |
| <10 | 7 |
| 10-14 | 13 |
| 15-19 | 11 |
| Etiology (number of patients) | |
| Dislocation | 3 |
| Extra-articular fracture | 13 |
| Intra-articular fracture | 11 |
| Complex fracture dislocation | 4 |
| Age at injury* (y) | 12.6 (3-19) |
| Interval from injury to surgery* (mo) | 32.1 (5-144) |
| Duration of immobilization* (wk) | 5.29 (0-19) |
| Earlier surgery | 27 (87.1%) |
| Preoperative AKP level* (/Ul) | 139.58 (42-287) |
| Follow-up duration* (y) | 5.3 (3-19) |
Mean values, with ranges in parentheses.
AKP indicates alkaline phosphatase.
All patients had HO on preoperative radiographs and they were managed surgically by the senior author, assisted by 2 experienced surgeons; they were followed up for at least 4 years (mean: 5.3 y; range: 3 to 19 y) by doctors in the group. At the follow-up, all of them were interviewed separately regarding elbow pain, ulnar nerve symptoms, infection, instability, any disabilities in daily life and sports and the range of elbow movement, which was recorded with a goniometer consistently. Plain radiographs were obtained, and the Mayo Elbow Performance Index (MEPI)16 was determined in all patients.
We also reviewed patient charts for assessing the age at injury and surgery, duration of the symptoms and immobilization after injury, type of fracture, initial treatment, AKP level before surgery, postoperative data, complications, and ROM.
Surgical Technique
The surgical techniques had been described in previous studies.17,18 All patients underwent surgery under general anesthesia, as well as brachial plexus block. We selected the surgical approach based on the previous incision, as well as pathology location. A combined medial and lateral approach was usually adopted. If patients had a previous posterior incision, we would prefer the posterior approach with the same procedures after soft tissue flap elevation. In the medial approach, the ulnar nerve was completely released and protected. The posterior and transverse bundles of the medial collateral ligament were detached to perform posterior arthrolysis, whereas the triceps muscle was split and released. The elbow joint was opened; posterior capsule, removed; olecranon fossa, debrided; and HO, resected subsequently.
For the anterior release, we used the lateral column approach. In patients with complex contractures and long-duration symptoms, the radial nerve was also released and protected throughout the surgery. After splitting the brachioradialis and extensor carpi, the hyperplastic capsule, scar tissue, and HO were excised. The deformed coronal fossa was trimmed. We also released the annular ligament and humeroradial joint when there was forearm rotation limitation.
While satisfactory ROM and rotation were achieved under minimal force, satisfactory release was also achieved; thereafter, a hinged external fixator (Orthofix, Lewisville, TX) was used for those unstable elbow joints. The axis of the fixator was determined using a 2.0-mm K-wire, positioned on the central capitellum. The extremities of the fixator were then fixed with 2 nails on the humerus and the radius. The injured medial and lateral collateral ligaments and muscles were reconstructed, with or without a suture anchor (Twinfix; Smith & Nephew, Andover, MA). Adequate tension was ensured throughout the elbow from extension to flexion. The ulnar nerve was transposed subcutaneously. Sufficient irrigation and meticulous hemostasis in the wound were achieved. The incision was then closed layer by layer with drains placed.
Postoperative Management
All patients engaged in active and passive motion exercises on the first postoperative day, with a duration of 30 minutes and frequency of 3 times per day. The protocol gradually increased to 1 hour per session on the following week. All patients were urged to achieve the operational arc of motion in every exercise, while extreme passive motion in extension or flexion was forbidden on the first week. The patients followed the rehabilitation schedule for at least 3 months postoperatively. We removed the hinged external fixator when the patients visited the outpatient clinic at ∼6 weeks postoperatively. Meanwhile, the patients were prescribed celecoxib (100 mg) twice a day for 6 weeks to prevent HO.19
Statistical Analysis
We included all independent variables in the statistical analysis, coding as measurement or categorical variables. After the normality test, measurement data were analyzed using the independent samples t test or nonparametric test. Categorical variables were compared using the nonparametric test and χ2 test. The Spearman rank correlation coefficient and the Pearson correlation were used to assess whether the continuous variables were significantly correlated with improvement in the arc of motion. Analysis of variance and the Kruskal-Wallis test were used to assess the relationship between the type of injury and improvement in the ROM. The statistical significance level was set at a P-value of 0.05 (SPSS, version 19; IBM, Armonk, NY).
RESULTS
Mobility
The mean duration of follow-up was 68 (range: 45 to 99) months. At the final follow-up, the elbow active flexion/extension (F/E) arc increased significantly from 49 degrees (range: 0 to 120 degrees) to 108 degrees (range: 0 to 120 degrees; P<0.001), with a mean flexion of 123 degrees (range: 70 to 140 degrees; P<0.001) and mean extension of 15 degrees (range: 0 to 85 degrees; P<0.001) postoperatively. And there was 1 patient who had a range of 0 to 140 degrees of flexion/extension arc, though the arc was 55 to 75 degrees before the operation. The pronation/supination arc for rotation increased from 129 to 151 degrees (P=0.05). The mean pronation increased from 57 degrees (range: -45 to 90 degrees) preoperatively to 70 degrees (range: 0 90 degrees; P<0.001) postoperatively, while the mean supination increased from 73 degrees (range: 0 to 90 degrees) to 80 degrees (range: 10 to 90 degrees; P<0.001). Two patients maintained the same F/E arc (0 to 120 degrees; 30 to 90 degrees) and had an increased P/S arc (10 degrees; 20 degrees), while 1 patient developed a worse motion arc of 10 degrees (Table 2).
TABLE 2.
Improvement in the Range of Motion
| Range of Motion (deg.) | Preoperative | Postoperative | P |
|---|---|---|---|
| Flexion* | 91.9 (30-135) | 123 (70-140) | <0.001 |
| Extension* | 42.6 (0-90) | 15 (0-85) | <0.001 |
| F/E arc | 49 | 108 | <0.001 |
| Pronation* | 57 (-45 to 90) | 70 (0-90) | <0.001 |
| Supination* | 73 (0-90) | 80 (0-90) | <0.001 |
| P/S arc | 129 | 151 | 0.05 |
Mean values, with ranges in parentheses.
F/E indicates flexion/extension; P/S, pronation/supination.
Functional Elbow Scores
The average MEPI at the final follow-up was 93.7 points (range: 65 to 100 points; P<0.001), while the preoperative MEPI was 67.9 (range: 35 to 95 points). Twenty-three patients had excellent outcomes (MEPI between 90 and 100 points); 5, good (MEPI between 75 and 89 points); and 3, fair (MEPI between 60 and 74 points); no patient had poor outcomes (MEPI < 60 points).8 At the follow-up, the patients with an F/E arc of >100 degrees (n=23) had an MEPI of 98.5 (SD: 4.38) points, whereas those with an F/E arc of <100 degrees (n=8) had an MEPI of 80.0 points (SD: 12.25 points; P<0.012). Eighty-seven percent of the patients were satisfied with their outcomes, and 32% would like to undergo the surgery again for a better motion arc as normal (Table 3).
TABLE 3.
Improvement in MEPI
| Characteristics | MEPI | P |
|---|---|---|
| Preoperative* | 67.9 (35-95) | <0.001 |
| Postoperative* | 93.7 (65-100) | |
| F/E arc of ≥100 (deg.) (n=23) | 98.5 (SD, 4.38) | <0.012 |
| F/E arc of <100 (deg.) (n=8) | 80.0 (SD, 12.25) |
Mean values, with ranges in parentheses.
F/E indicates flexion/extension; MEPI, Mayo Elbow Performance Index.
Independent Factors With Improvements in the Arc
At the final follow-up, the mean improvement in the arc of motion was 59.0 degrees (SD: 6.98 degrees). Significant relationships were evaluated between several factors and the improvement in the elbow motion. The increase in the age at surgery was associated with improved postoperative elbow motions. The mean preoperative serum AKP level was 139.58 (range: 42 to 287)/UL, and the increased AKP level resulted in a decreased arc of motion (Table 4). The type of injury was also associated with an improved arc; patients with extra-articular fractures who had a mean improvement were more likely to have a significant improvement in the arc of motion than those with intra-articular fractures (83.31±24.57 vs. 45.45±43.90 degrees, P=0.012) or complex fracture dislocation (83.31±24.57 vs. 36.25±22.87 degrees, P=0.023). The mean improvement in patients with dislocation was 33.33 degrees (SD: 41.63 degrees), which was less than the arc of the extra-articular fracture group (P=0.031); no difference was found in relation to the other groups (P>0.05) (Table 5).
TABLE 4.
Factors Affecting Improvement in the Arc
| Variable | P |
|---|---|
| Age at surgery | 0.004 |
| Serum alkaline phosphatase level | 0.015 |
| Type of injury | 0.019 |
TABLE 5.
Comparison of the Improvement in the Arc of Motion According to the Type of Injury
| Characteristics | ROM (deg.) | P |
|---|---|---|
| Extra-articular fracture | 83.31±24.57 | |
| Intra-articular fracture | 45.45±43.90 | 0.012* |
| Complex fracture dislocation | 36.25±22.87 | 0.023* |
| Dislocation | 33.33±41.63 | 0.031*, >0.05† |
Compared with extra-articular fracture.
†Compared with intra-articular fracture and complex fracture dislocation.
ROM indicates the range of motion.
In addition, there were no significant difference between the improved arc of motion with injury age, duration of symptoms, immobilization after injury, and initial treatment.
Complications
The total complication rate was 12.9%: 1 case of ulnar neuropathy with HO and elbow ankylosis, 2 cases of postoperative pain, and 1 case of elbow instability. These complications did not have a great impact on daily living and work, and the patients accepted their situation. Eight patients (25.8%) developed recurrent contracture with an ROM of <100 degrees at the final follow-up with recurrent HO after surgery on radiographs. There were no postoperative infections nor other complications. Three patients were also advised to undergo resurgery after the age of 20 years.
DISCUSSION
The elbow of young children occasionally will develop contractures when posttraumatic elbow conditions respond to inadequate treatment.20 A decreased ROM in the elbow has significantly interfered with qualities of daily living in children and adolescents.9,12 Several studies have investigated the management of adult posttraumatic elbow contractures, with satisfactory outcomes of open elbow release.1,6
However, the instructive literature on pediatric and adolescent elbow stiffness is insufficient, with varying outcomes.9,11–13,21–23 Recently, some studies have specifically reported equivocal outcomes of open surgical release in children and adolescents with stiff elbows. Stans et al11 studied 37 patients and showed an average improvement in the arc of motion of 28 degrees, with 2 patients losing motion and 1 patient developing total ankylosis. However, the outcomes were more favorable in three other studies, with a mean increase of ∼54 degrees in the F/E arc.11,22,23 Further, Ek et al13 followed up their patients for >5 years and reported the same improvement of 54 degrees. This finding was consistent with the outcomes of the latest literature. Piper et al9 studied 26 young patients and reported a similar increase of 49 degrees. Though the difference in pathologic condition and surgical solution makes the improvement different, here we used different approaches as a whole adapting to pathologic conditions and study the relationship between surgical methods and improvement according to the postoperative baseline in treating the stiff elbow. Our study is one of the longest follow-up studies to evaluate the outcomes of posttraumatic elbow stiffness and demonstrated that open release of elbow contractures in children and adolescents younger than 20 years yields a significant and maintained increase in elbow ROM and MEPI, with a mean increase of 59 degrees in the F/E arc. Moreover, we found that 54.8% of the patients obtained a functional F/E arc of motion (30 to 130 degrees), with a mean elbow arc of 131 degrees. In addition, 67.7% of the patients gained a 10 degrees-extended arc of motion (40 to 120 degrees), with a mean arc of 128 degrees.
In contrast, the outcomes of younger patients were not as successful as the outcomes of adult patients, who underwent surgery conducted by the same surgeons using the same protocol in previous studies.4,10,17,19 Whether there was anything different between children and adults remained unclear. Stans et al11 demonstrated that the improvement in the arc of motion decreased when the patients had an intra-articular fracture or a complex fracture dislocation; however, a contrasting finding was reported by Ek et al13 In this study, we found that the patients who had an extra-articular fracture tended to have better outcomes, but not those whose contracture had been caused by a simple dislocation. These analyses were limited to the fact that only 3 patients had a dislocation, and 2 of them had a preoperative F/E arc of >100 degrees; this indicates that the severity of elbow injuries needs further research.
We found that the age at surgery was positively associated with the improvement in the arc. Conversely, a previous study found no significant effect of the age at the time of surgery.12 Young patients who had an older age at surgery tend to have better improvements in the arc of motion. This is expected because of its consistency with our clinical experience, and patients with an older age are better suited for rehabilitation. Moreover, this result may explain the better postoperative outcomes in adults than in children. This may also represent the association between age and patient compliance, which is helpful in restoration and recovery.
The serum AKP level has been used to predict and identify the formation of HO, which mostly determines the outcomes of open arthrolysis for elbow stiffness.6,14 Orzel and Rudd14 suggested that the serum AKP level can be used for early diagnosis of heterotopic bone formation. In contrast, Citak et al15 questioned the benefits of the AKP level as a screening parameter in predicting HO. Despite the controversy, we found that the patients who had a higher preoperative AKP level tended to have a worse arc improvement. Zierk et al24 reported that the AKP activity in children would change with sex-specific and age-specific dynamics owing to extensive growth and puberty. With the increase in the age at surgery and the decrease in the preoperative AKP level, the patients appeared to have an improvement in the arc as good as that in adults (Fig. 1).
FIGURE 1.
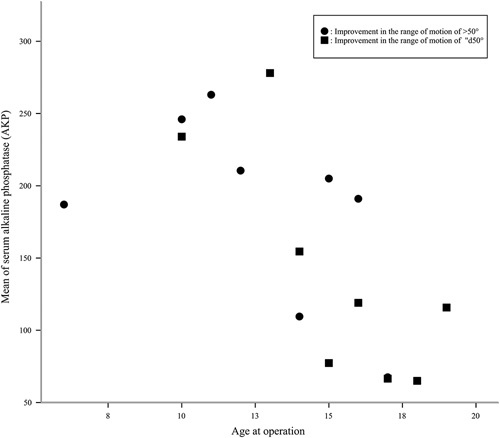
Scatterplot showing the relationship of the improvement in the range of motion at the final follow-up with the mean preoperative alkaline phosphatase level and age at surgery. With the increase in the age at surgery and the decrease in the preoperative alkaline phosphatase level, the proportion of the improvement in the range of motion (>50 degrees) increased.
There were 3 patients who had the same or worse F/E arc at the final follow-up. We found that they had poor compliance to the postoperative rehabilitation program, which could explain the unsatisfactory outcome and the bad condition of HO.
The present study has several limitations. First, we did not analyze the HO condition, which may provide information on the association of the age at surgery, AKP level, and ROM. Second, and most notably, our sample size is too small to control the heterogeneity of the pathology. Considering the importance of postoperative rehabilitation, we believe that the compliance in rehabilitation program should be given more attention. Furthermore, there should be an exploration on the necessity and validity of hinged external fixation in pediatric patients.
CONCLUSIONS
Despite such limitations, our data suggest that if open arthrolysis with or without hinged external fixation for the treatment of a posttraumatic elbow contracture is performed before the patient is aged 20 years, good midterm clinical outcomes may be expected. As expected, the functional scores improved with increased ROM, and the elbow ROM was ameliorated through open contracture release. However, open elbow arthrolysis should be further studied on a larger scale to analyze independent factors and determine the criterion for considering this procedure among young populations.
Footnotes
J.-H.R., H.-M.C., Z.-Y.S., S.C.: these authors contributed equally to this work.
This study was approved by the Ethics Committee of Shanghai Sixth People’s Hospital East Campus (No. 2016014).
This work was supported by the National Natural Science Foundation of China under Grant no. 81830076 and 81672146. The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Contributor Information
Ji-hao Ruan, Email: jihaoruan@gmail.com.
Hao-min Cui, Email: 790937981@qq.com.
Zi-yang Sun, Email: max_920@163.com.
Shuai Chen, Email: 812561965@qq.com.
Wei Wang, Email: 15800792527@163.com.
Cun-yi Fan, Email: cyfan@sjtu.edu.cn.
REFERENCES
- 1.Morrey BF. Post-traumatic contracture of the elbow. Operative treatment, including distraction arthroplasty. J Bone Joint Surg Am. 1990;72:601–618. [PubMed] [Google Scholar]
- 2.Morrey BF, Askew LJ, Chao EY. A biomechanical study of normal functional elbow motion. J Bone Joint Surg Am. 1981;63:872–877. [PubMed] [Google Scholar]
- 3.Onay T, Gümüştaş SA, Baykan SE, et al. Mid-term and long-term functional and radiographic results of 13 surgically treated adolescent capitellum fractures. J Pediatr Orthop. 2018;38:e424–e428. [DOI] [PubMed] [Google Scholar]
- 4.Sun C, Zhou X, Yao C, et al. The timing of open surgical release of post-traumatic elbow stiffness: a systematic review. Medicine. 2017;96:e9121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang W, Zhan YL, Yu SY, et al. Open arthrolysis with pie-crusting release of the triceps tendon for treating post-traumatic contracture of the elbow. J Shoulder Elbow Surg. 2016;25:816–822. [DOI] [PubMed] [Google Scholar]
- 6.Chen S, Liu J, Cai J, et al. Results and outcome predictors after open release of complete ankylosis of the elbow caused by heterotopic ossification. Int Orthop. 2017;41:1627–1632. [DOI] [PubMed] [Google Scholar]
- 7.Edwards SG, Rhodes DA, Jordan TW, et al. The olecranon osteotomy-facilitated elbow release (OFER). J Bone Joint Surg Am. 2017;99:1859–1865. [DOI] [PubMed] [Google Scholar]
- 8.Ouyang Y, Wang Y, Li F, et al. Open release and a hinged external fixator for the treatment of elbow stiffness in young patients. Orthopedics. 2012;35:e1365–e1370. [DOI] [PubMed] [Google Scholar]
- 9.Piper SL, Lattanza LL, Shen TS, et al. Open surgical release of posttraumatic elbow contracture in children and adolescents. J Pediatr Orthop. 2017;39:241–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhou Y, Cai JY, Chen S, et al. Application of distal radius-positioned hinged external fixator in complete open release for severe elbow stiffness. J Shoulder Elbow Surg. 2017;26:e44–e51. [DOI] [PubMed] [Google Scholar]
- 11.Stans AA, Maritz NG, O’Driscoll SW, et al. Operative treatment of elbow contracture in patients twenty-one years of age or younger. J Bone Joint Surg Am. 2002;84-A:382–387. [DOI] [PubMed] [Google Scholar]
- 12.Bae DS, Waters PM. Surgical treatment of posttraumatic elbow contracture in adolescents. J Pediatr Orthop. 2001;21:580–584. [PubMed] [Google Scholar]
- 13.Ek E, Paul S, Hotchkiss R. Outcomes after operative treatment of elbow contractures in the pediatric and adolescent population. J Shoulder Elbow Surg. 2016;25:2066–2070. [DOI] [PubMed] [Google Scholar]
- 14.Orzel J, Rudd T. Heterotopic bone formation: clinical, laboratory, and imaging correlation. J Nucl Med. 1985;26:125–132. [PubMed] [Google Scholar]
- 15.Citak M, Grasmücke D, Suero E, et al. The roles of serum alkaline and bone alkaline phosphatase levels in predicting heterotopic ossification following spinal cord injury. Spinal Cord. 2016;54:368–370. [DOI] [PubMed] [Google Scholar]
- 16.Cusick M, Bonnaig N, Azar F, et al. Accuracy and reliability of the Mayo Elbow Performance Score. J Hand Surg Am. 2014;39:1146–1150. [DOI] [PubMed] [Google Scholar]
- 17.Liu S, Fan CY, Ruan HJ, et al. Combination of arthrolysis by lateral and medial approaches and hinged external fixation in the treatment of stiff elbow. J Trauma Acute Care Surg. 2011;70:373–376. [DOI] [PubMed] [Google Scholar]
- 18.Ruan HJ, Liu S, Fan CY, et al. Open arthrolysis and hinged external fixation for posttraumatic ankylosed elbows. Arch Orthop Trauma Surg. 2013;133:179–185. [DOI] [PubMed] [Google Scholar]
- 19.Sun YB, Cai JY, Li F, et al. The efficacy of celecoxib in preventing heterotopic ossification recurrence after open arthrolysis for post-traumatic elbow stiffness in adults. J Shoulder Elbow Surg. 2015;24:1735–1740. [DOI] [PubMed] [Google Scholar]
- 20.Papandrea R, Waters P. Posttraumatic reconstruction of the elbow in the pediatric patient. Clin Orthop Relat Res. 2000;370:115–126. [DOI] [PubMed] [Google Scholar]
- 21.Mih AD, Wolf FG. Surgical release of elbow-capsular contracture in pediatric patients. J Pediatr Orthop. 1994;14:458–461. [DOI] [PubMed] [Google Scholar]
- 22.Andelman S, Walsh A, Sochol K, et al. Arthroscopic elbow contracture release in the pediatric patient. J Pediatr Orthop. 2018;38:e507–e513. [DOI] [PubMed] [Google Scholar]
- 23.Darlis NA, Kaufmann RW, Sotereanos DG. Open surgical treatment of post-traumatic elbow contractures in adolescent patients. J Shoulder Elbow Surg. 2006;15:709–715. [DOI] [PubMed] [Google Scholar]
- 24.Zierk J, Arzideh F, Haeckel R, et al. Pediatric reference intervals for alkaline phosphatase. Clin Chem Lab Med. 2017;55:102–110. [DOI] [PubMed] [Google Scholar]


