Abstract
Objective:
To perform a systematic review of the literature to identify the long-term effects of presurgical orthopedic (PSO) device use on patient outcomes.
Design:
A comprehensive literature review of Embase and Ovid databases was performed to identify all English-language publications related to unilateral cleft lip and palate, presurgical devices, and patient outcomes. Studies were excluded if they did not report patient outcomes beyond 2 years of age, did not describe the use of a PSO device, were case reports (n < 10), or were purely descriptive studies.
Main Outcome Measures:
Reported patient outcomes following the use of PSO devices.
Results:
Following a review of all articles by 2 independent reviews, 30 articles were selected for inclusion. Overall, there was no reported consensus as to the long-term effects of PSO devices. Furthermore, this study identified that only 10% of published research controlled for confounding factors that could influence the reported results. Confounding factors that were identified included different operating surgeon, different surgical protocols, and different rates of revision surgeries.
Conclusions:
Overall, this systematic review identified 2 important conclusions. Firstly, there is no consensus in the literature about the long-term effects of PSO devices on long-term patient outcomes. Secondly, research in this domain is limited by confounding factors that influence the applicability of the reported results.
Keywords: cleft palate, presurgical orthopedic devices, outcomes, growth, nasolabial aesthetics, occlusion
Introduction
Clinical use of active and passive presurgical orthopedic (PSO) devices for the management of patients with cleft lip and palate is controversial. It is widely accepted that these devices are useful for decreasing alveolar gap size prior to lip repair (Winters and Hurwitz, 1995; Grayson et al., 1999; Prahl et al., 2001; Isik Aslan et al., 2018), but their long-term effects on nasolabial aesthetics, dental occlusion, and facial growth are still debated (Larson et al., 1993; Henkel and Gundlach, 1997; Bajaj et al., 2011; Monasterio et al., 2013; Shetty et al., 2017; Hay et al., 2018; Kornbluth et al., 2018; Liang et al., 2018). Consequently, the use of these devices is dependent on surgeon experience and caregiver preference (Heliovaara et al., 2020).
To date, there is a large body of research examining the outcomes of patients treated with PSO devices, but there is no consensus on their effect on long-term patient outcomes (Uzel and Alparslan, 2011; Kornbluth et al., 2018). The lack of consensus on the use of these devices is likely in part due to limitations of the research itself. Research in cleft lip and palate is often biased by small sample sizes and variable management protocols. Frequently, patients from numerous sites and surgeons are included in a single study to try and increase the study cohort. Although advantageous for increasing the power of studies, grouping patients undergoing dissimilar management ultimately creates confounding factors within the studies (eg, surgeon experience, surgical procedure) (Hegde et al., 2015; Isik Aslan et al., 2018; Kornbluth et al., 2018). The variability that exists within and in between comparison groups creates bias and confusion when drawing conclusions from the research performed. In addition, there is also a paucity of research actually comparing the difference in outcomes between patients treated with different types of PSO devices (Kornbluth et al., 2018).
The primary purpose of this research was to complete a systematic review of the literature pertaining to the use of PSO devices in cleft lip/palate and their effect on long-term patient outcomes. Specifically, we sought to identify the type of PSO device being used, the surgical protocol including PSO device and timing of lip/palate repair, the patient outcomes being measured, and the overall conclusions drawn about the PSO device (ie, positive effect, negative effect, or no effect).
Methods
The systematic review was designed using the published preferred reporting items for systematic reviews and meta-analyses PRISMA guidelines (Moher et al., 2009). The search protocol was not registered prior to undertaking the systematic review. Systematic searches were conducted in Ovid MEDLINE and Embase electronic databases (from inception to November 2019) and were restricted to infants (younger than 1 year of age), and studies published in the English language. The search queries were developed using a combination of subject headings and free text words such as but not limited to cleft palate, cleft lip palate, cleft lip, cleft lip face palate, orthodontics, nasoalveolar molding (NAM), passive nasoalveolar molding (PNAM), presurgical infant orthopedic (PSIO), and preoperative period. Optimized methodological search “filters” and text words were used to focus search results on research from comparative studies to complement data from randomized controlled trials published on the topic. The search strategies were adapted for each database to include database-specific thesaurus terms and field names. To identify additional relevant studies that met our inclusion criteria we also examined bibliographies of the relevant retrieved articles. Conference publications presented at major national and international meetings were also reviewed for relevance. A detailed description of our search strategy can be found in Online Appendix 1.
After initial abstraction of all studies from both databases, all duplicate studies were eliminated. All titles were initially screened for inclusion, followed by abstract review. Finally, all remaining studies were screened via full text review for appropriateness for inclusion. Selection criteria for included studies were as follows:
Inclusion Criteria
Described the use of PSO device for management of unilateral cleft lip and palate.
Described patient outcomes beyond 2 years of age.
Included human subjects.
English-language articles.
Published at any date.
Any study design, including case series (>10 cases).
Studies were excluded if they did not describe the use of a PSO device for cleft management did not describe patient outcomes beyond 2 years of age, were case reports (<10 cases), or nonoriginal studies. In addition, studies that did not separate unilateral and bilateral cleft lip/palate patients were excluded, as these are 2 separate populations whose overall outcomes could vary greatly. Studies comparing patients with a cleft to those without a cleft were also excluded; growth, occlusion, and aesthetics in patients without cleft lip/palate are vastly different, and this was considered to be an inappropriate comparison when trying to evaluate the effects of PSO devices.
Review of abstracts and full texts was performed independently by 2 reviewers, and any disagreement about study inclusion was resolved by consensus with the help of senior authors. All study data were extracted in duplicate using a standardized form. The same 2 reviewers extracted study data including: (1) study title, (2) authors, (3) year of publication, (4) journal of publication, (5) type of publication, (6) number of patients included in study, (7) type of PSO device used, (8) patient management protocols within and between groups, (9) patient outcomes measured (eg, growth, nasolabial aesthetics, occlusion), (10) age of patients at analysis, and (11) conclusions drawn about the device being evaluated. Within the evaluation of patient management protocol, we also recorded number of surgeons and sites. The clinical outcomes measured were as follows: nasolabial aesthetics, facial growth, dental arch/occlusion outcomes, rates of revision surgeries, and change in airway anatomy. When abstracting data about the conclusions draw about the device, these conclusions were summarized as positive (ie, the device improved the measured outcomes), negative (ie, the device worsened the reported outcomes), or neutral (ie, the device made no difference on the reported outcomes).
Basic demographics were calculated, but meta-analysis was not performed due to the heterogeneity of the reported methods. A risk of bias assessment was performed using the checklist described by Downs and Black (1998). This checklist was modified to fit the included studies. This checklist is binary; a score of 1 is awarded to studies that include the specified element and 0 if the element is not included. Maximum score was 21. The checklist was reviewed independently by 2 reviewers, any disagreement about the awarded score was resolved by consensus.
Results
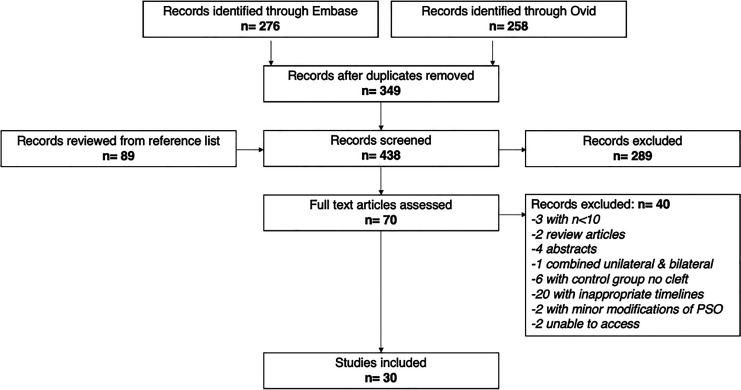
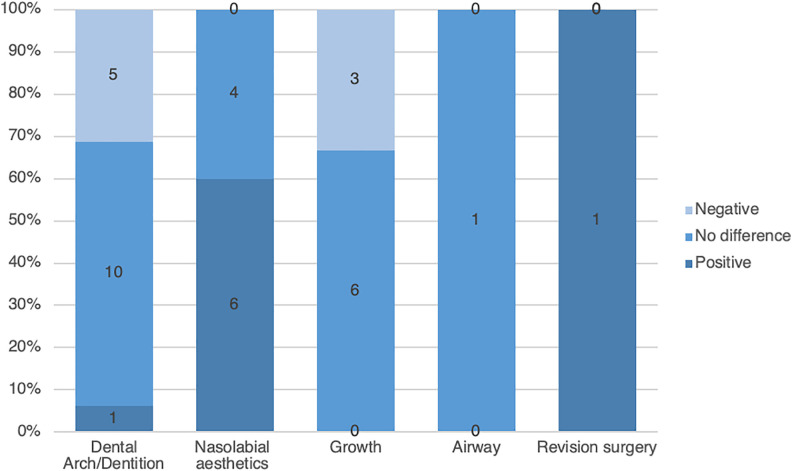
The literature search yielded a total of 438 studies to review, of which studies met criteria for inclusion in the systematic review (Table 1; Figure 1) (Asher-McDade et al., 1992; Brattstrom et al., 1992; Mars et al., 1992; Molsted et al., 1992; Larson et al., 1993; Joos, 1995; Henkel & Gundlach, 1997; Millard et al., 1999; Mishima et al., 2000; Chan et al., 2003; Bongaarts et al., 2004; Brattstrom et al., 2005; Molsted et al., 2005; Bongaarts et al., 2006; Bongaarts et al., 2008; Barillas et al., 2009; Bongaarts et al., 2009; Nakamura et al., 2009; Mishra et al., 2010; Clark et al., 2011; Daskalogiannakis et al., 2011; Hathaway et al., 2011; Patel et al., 2015; Lin et al., 2017; Shetty et al., 2017; Kornbluth et al., 2018; Liang et al., 2018; Massie et al., 2018; Peanchitlerkajorn et al., 2018; Singer et al., 2018; Rubin et al., 2019). The results of the bias assessment are included in Online Appendix 2. Of the 30 studies, 24 were retrospective studies and 6 were prospective studies. On average, the included studies had a total of 33.7 patients per intervention group and the majority focused on outcomes from 5 to 10 years of age (Table 1). Seven articles focused on nasoalveolar molding devices, 3 on the Latham device, 4 on a passive plate, 1 on a Hotz plate, 2 on a T-traction device, 1 on an unspecified active device, and 1 on an unspecified device. In addition, 11 articles compared several different devices. In total, 10 articles described nasolabial aesthetics, 9 described facial growth, 16 described dental arch/occlusion outcomes, 1 described rates of revision surgeries, and 1 described change in airway anatomy (Figure 2).
Table 1.
Study Characteristics.
| Paper | Authors | Year | Type of publication | Sites | Device | Age of measurements | Outcome | |
|---|---|---|---|---|---|---|---|---|
| 1 | Effect of presurgical nasoalveolar molding on nasal symmetry in unilateral complete cleft lip/palate patients after primary cheiloplasty without concomitant nasal cartilage dissection: early childhood evaluation. | Liang et al. | 2018 | Retrospective cohort | 1 surgeon | NAM | 4 years | Nasolabial aesthetics |
| 2 | Active presurgical infant orthopedics for unilateral cleft lip and palate: Intercenter outcome comparison of Latham, modified McNeil, and nasoalveolar molding. | Kornbluth et al. | 2018 | Retrospective cohort | 4 sites | (1) Latham (2) NAM (3) McNeil |
7-10 years | (1) Dental arch/occlusion (2) Facial growth (3) Nasolabial aesthetics |
| 3 | Midface growth in patients with unilateral cleft lip and palate treated with a nasoalveolar molding protocol. | Rubin et al. | 2019 | Retrospective cohort | 1 surgeon | NAM | 6-11 years | Facial growth |
| 4 | The effect of nasoalveolar molding on nasal airway anatomy: a 9-year follow-up of patients with unilateral cleft lip and palate. | Massie et al. | 2018 | Retrospective cohort | 1 site | NAM | 8-10 years | Airway measurements |
| 5 | Burden of care of various infant orthopedic protocols for improvement of nasolabial esthetics in patients with CUCLP. | Singer et al. | 2018 | Retrospective cohort | 3 sites | (1) NAM (2) McNeil |
5 years | Nasolabial aesthetics |
| 6 | Long-term effect of presurgical nasoalveolar molding on growth of maxillary arch in unilateral cleft lip and palate: randomized controlled trial. | Shetty et al. | 2017 | Prospective RCT | 1 surgeon | NAM | (1) Device insertion (2) Device stop (3) 6 years |
Dental arch/occlusion |
| 7 | A comparison of mixed dentition dental development in cleft patients treated with and without the latham-type appliance. | Lin et al. | 2017 | Retrospective cohort | 1 site | Latham | 7.5-9 years | Dental arch/occlusion |
| 8 | Skeletal growth after muscular reconstruction for cleft lip, alveolus, and palate | Joos | 1995 | Prospective RCT | 1 site | Unspecified | 6.5 years | (1) Dental arch/occlusion (2) Facial growth |
| 9 | Long-term treatment outcome of presurgical nasoalveolar molding in patients with unilateral cleft lip and palate. | Clark et al. | 2011 | Retrospective cohort | 1 surgeon | NAM | 5 years | (1) Dental arch/occlusion (2) Nasolabial aesthetics |
| 10 | Nasoalveolar molding improves long-term nasal symmetry in complete unilateral cleft lip-cleft palate patients. | Barillas et al. | 2009 | Retrospective cohort | 1 surgeon | NAM | 1 year | Nasolabial aesthetics |
| 11 | Infant orthopedics and facial growth in complete unilateral cleft lip and palate until six years of age (Dutchcleft). | Bongaarts et al. | 2009 | Prospective RCT | 3 sites | Passive plate | (1) 4 years (2) 6 years |
Facial growth |
| 12 | Effect of infant orthopedics on facial appearance of toddlers with complete unilateral cleft lip and palate (Dutchcleft). | Bongaarts et al. | 2008 | Prospective RCT | 3 sites | Passive plate | (1) 4 years (2) 6 years |
Nasolabial aesthetics |
| 13 | Infant orthopedics has no effect on maxillary arch dimensions in the deciduous dentition of children with complete unilateral cleft lip and palate (Dutchcleft). | Bongaarts et al. | 2006 | Prospective RCT | 3 sites | Passive plate | (1) 4 years (2) 6 years |
Dental arch/occlusion |
| 14 | The effect of infant orthopedics on the occlusion of the deciduous dentition in children with complete unilateral cleft lip and palate (Dutchcleft). | Bongaarts et al. | 2004 | Prospective RCT | 3 sites | Passive plate | (1) 4 years (2) 6 years |
Dental arch/occlusion |
| 15 | The effects of active infant orthopedics on occlusal relationships in unilateral complete cleft lip and palate. | Chan et al. | 2003 | Retrospective cohort | 1 surgeon | Latham | 5-10 years | Dental arch/occlusion |
| 16 | Comparison between palatal configurations in UCLP infants with and without a Hotz plate until four years of age. | Mishima et al. | 2000 | Retrospective cohort | 1 site | Hotz plate | (1) 0 months (2) 4 months (3) 6 months (4) 18 months (5) 4 years |
Dental arch/occlusion |
| 17 | Cleft lip and palate treated by presurgical orthopedics, gingivoperiosteoplasty, and lip adhesion (POPLA) compared with previous lip adhesion method: A preliminary study of serial dental casts. | Millard et al. | 1999 | Retrospective cohort | 1 site | Active device | (1) 3 years (2) 6 years (3) 9 years |
Dental arch/occlusion |
| 18 | Analysis of primary gingivoperiosteoplasty in alveolar cleft repair. Part I: Facial growth. | Henkel et al. | 1997 | Retrospective cohort | 1 surgeon | Latham | (1) 3 years (2) 7 years (3) 10 years (4) 16 years |
(1) Dental arch/occlusion (2) Facial growth |
| 19 | Craniofacial development in children with unilateral cleft of the lip, alveolus, and palate treated according to three different regimes. Assessment of nasolabial appearance. | Brattstrom et al. | 1992 | Retrospective cohort | 2 sites | T traction | 16 years | Nasolabial aesthetics |
| 20 | Early bone grafting in complete cleft lip and palate cases following maxillofacial orthopedics. III. A study of the dental occlusion. | Larson et al. | 1983 | Retrospective cohort | 1 site | T traction | 8-10 years | Dental arch/occlusion |
| 21 | An intercenter comparison of dental arch relationships and craniofacial form including a center using nasoalveolar molding. | Peanchitlertkajorn et al. | 2018 | Retrospective cohort | 5 sites | (1) Taping (2) NAM (3) McNeil (4) Passive plate |
8-10 years | (1) Dental arch/occlusion (2) Facial growth |
| 22 | A six-center international study of treatment outcome in patients with clefts of the lip and palate: part 4. assessment of nasolabial appearance | Asher-Mcdade et al. | 1992 | Retrospective cohort | 6 sites | (1) Hotz plate (2) None (3) None (4) Extra-oral strap (5) None (6) T-traction |
8-10 years | Nasolabial aesthetics |
| 23 | A six-center international study of treatment outcome in patients with clefts of the lip and palate: part 3. Dental arch relationships | Mars et al. | 1992 | Retrospective cohort | 6 sites | (1) Hotz plate (2) None(3) None (4) Extra-oral strap (5) None (6) T-traction |
8-10 years | Dental arch/occlusion |
| 24 | Comparative study of early secondary nasal revisions and costs in patients with clefts treated with and without nasoalveolar molding | Patel et al. | 2015 | Retrospective cohort | 1 surgeon | NAM | 5-14 years | Revision surgery |
| 25 | The Eurocleft study: intercenter study of treatment outcome in patients with complete cleft lip and palate. Part 2: Craniofacial form and nasolabial appearance | Brattstrom et al. | 2005 | Retrospective cohort | 5 sites | (1) Hotz plate (2) None (3) Extra-oral strap (4) None (5) T-traction |
(1) 9 years (2) 12 years (3) 17 years |
(1) Nasolabial aesthetics (2) Growth |
| 26 | Postoperative nasal forms after presurgical nasoalveolar molding followed by medial-upward advancement of nasolabial components with vestibular expansion for children with unilateral complete cleft lip and palate | Nakamura et al. | 2009 | Retrospective cohort | 1 surgeon | (1) NAM (2) Hotz plate |
1-5 years | Nasolabial aesthetics |
| 27 | The Americleft study: an inter-center study of treatment outcomes for patients with unilateral cleft lip and palate part 3. Analysis of craniofacial form | Daskaloginannakis et al. | 2011 | Retrospective cohort | 5 sites | (1) None (2) Passive plate (3) None (4) McNeil (5) McNeil |
6-12 years | Facial growth |
| 28 | The Americleft study: an inter-center study of treatment outcomes for patients with unilateral cleft lip and palate part 2. Dental arch relationships | Hathaway et al. | 2011 | Retrospective cohort | 5 sites | (1) None (2) Passive plate (3) None (4) McNeil (5) McNeil |
6-12 years | Dental arch/occlusion |
| 29 | A six-center international study of treatment outcome in patients with clefts of the lip and palate: part 2. craniofacial form and soft tissue profile | Molsted et al. | 1992 | Retrospective cohort | 6 sites | (1) Hotz plate (2) None (3) None (4) Extra-oral strap (5) None (6) T-traction |
8-10 years | Facial growth |
| 30 | The Eurocleft study: intercenter study of treatment outcome in patients with complete cleft lip and palate. Part 3: dental arch relationships | Molsted et al. | 2005 | Retrospective cohort | 5 sites | (1) Hotz plate (2) None (3) Extra-oral strap (4) None (5) T-traction |
(1) 9 years (2) 12 years (3) 17 years |
Dental arch/occlusion |
Figure 1.
Flowchart of study inclusion.
Figure 2.
Distribution of positive, negative, or inconclusive results in all articles.
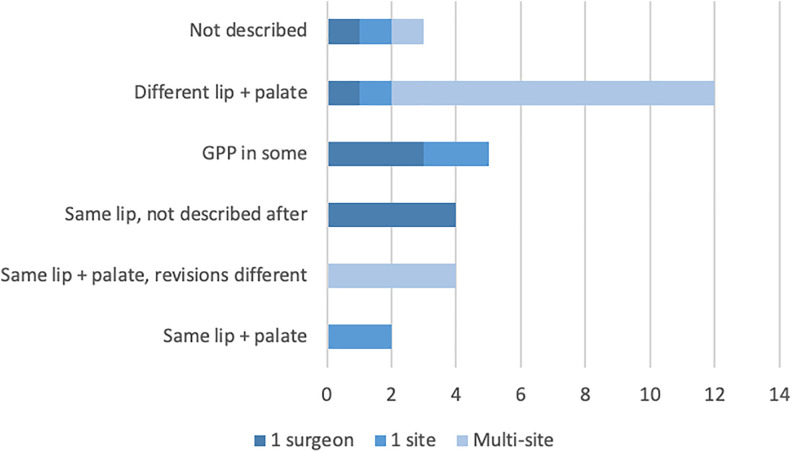
A total of 9 articles examined a patient cohort from a single surgeon’s practice, 15 used a cohort from multiple sites and/or surgeons, and 6 examined a cohort from one site with an unspecified number of surgeons involved in the care of the patients. Consistency in management protocols was quite variable between these 3 groups (Figure 3). Variability in the protocols included different operating surgeons (n = 21), different type and timing of lip and/or palate repair (n = 12), whether patients received gingivoperiosteoplasty (GPP) (n = 5), and whether patients received revision surgeries (n = 4). In total, 3 papers did not describe their management protocols and 4 described similar management for lip repair but did not describe management following lip repair. In total, 2 papers had a consistent management protocol within and between experimental groups, but even these 2 papers were not single-surgeon studies.
Figure 3.
Types of variability in the methodology of the reviewed studies.
With respect to the 9 articles that investigated a single surgeon’s practice, 7 articles examined the effects of a passive device and 2 examined the effects of an active device. Three articles reported on nasolabial aesthetics, 2 reported on dental arch/occlusion, 1 reported on facial growth, 1 reported on dental arch/occlusion and growth, 1 article reported on dental arch/occlusion and nasolabial aesthetics, and 1 article compared rates of revision surgeries. Five of the 9 single-surgeon articles had inconsistent management protocols for all of their patients or did not specify whether the management between the control and experimental groups was the same. In the 4 remaining articles, consistent management up to the time of lip repair was reported, but no study specified whether the treatment/control groups differed in their management following lip repair (eg, palate surgery, revision surgeries etc).
Discussion
Overall, this systematic review identified 30 studies examining the long-term effects of PSO device use. The primary objective of this systematic review was to describe the current literature on the long-term outcomes of patients treated with PSO devices. To this effect, the main clinical outcomes measured in these studies were nasolabial aesthetics, facial growth, and dental arch/occlusion. Overall, this systematic review identified studies that report positive, negative, or no effects of PSO devices on patient outcomes with no particular predominance. The discrepancy of findings between studies highlights the lack of consensus on the long-term effects of PSO device use in patients with cleft lip/palate.
A potential reason for the discrepancy found in this systematic review is the large variability in management of the patients in these studies. This variability in management within experimental groups creates many confounding factors that make it difficult to draw meaningful conclusions from the results. Variability in patient management has previously been identified as a weakness in cleft lip/palate literature but has never been quantified as was done in this review (Isik Aslan et al., 2018; Kornbluth et al., 2018). In total, this review identified no single-surgeon article that had a consistent management protocol between and within comparison groups.
Identified sources of variability in patient management included different operating surgeons, different timing/type of lip and/or palate repair, inconsistent use of GPP, and patients receiving different types of revision surgeries. These differences in management protocols are especially apparent in the Eurocleft studies, Americleft studies, and the Dutchcleft studies (Asher-McDade et al., 1992; Mars et al., 1992; Molsted et al., 1992; Prahl et al., 2001; Prahl et al., 2003; Bongaarts et al., 2004; Brattstrom et al., 2005; Molsted et al., 2005; Bongaarts et al., 2006; Prahl et al., 2006; Bongaarts et al., 2008; Bongaarts et al., 2009; Daskalogiannakis et al., 2011; Hathaway et al., 2011). These large cohort studies were some of the earliest studies describing nasolabial aesthetic, dental occlusion, and facial growth outcomes in patients with cleft palate that received PSO device treatment. Although they were essential to developing the cleft palate literature, each of these studies compared patients from 4 to 6 centers that all differed in the PSO device used (active vs passive), type/timing of lip and palate surgery, and the surgeon who operated on the patients. Differing times of lip and palate repair can reduce the applicability of the comparisons being drawn between the PSO groups as the age of the repair has been previously shown to affect growth (Mylin and Hagerty, 1983; Bardach et al., 1984; Friede and Enemark, 2001). Moreover, in all of these studies the comparison groups were each operated on by different surgeons. It cannot be excluded that the reported results may be a consequence of the operating surgeon and not the PSO device used (Adali et al., 2012). Despite being large trials, the variability in patient management makes it difficult to isolate and conclude how the PSO devices may have influenced patient outcomes.
In an effort to eliminate some potential bias, this review also focused on studies from a single surgeon’s practice; however, multiple confounding factors and methodology flaws were still identified. Our review identified a total of 9 single surgeon studies from which 6 studies still had inconsistent management protocols between groups. In total, 3 single-surgeon studies had consistent management protocols up to the time of lip repair (Barillas et al., 2009; Clark et al., 2011; Liang et al., 2018). By maintaining a consistent management protocol with a single surgeon, these studies eliminated many confounding variables but still had several weaknesses that decreased the validity of their results. Specifically, all 3 studies did not report on the number of patients requiring further surgeries following palate repair. This is an important distinction that must be made when evaluating patients long term as changes in clinical outcomes could be attributed to their revision surgeries instead of their initial management.
Previously, Uzel and Alparslan published a retrospective review which included only prospective studies examining the long-term effects of PSO devices; a total of 12 studies were identified in their review. Their review concluded that passive devices have no positive effect on motherhood satisfaction, feeding, speech, facial growth, dental arch, occlusion, and nasolabial aesthetics and active devices have no positive effects on feeding (Uzel and Alparslan, 2011). Overall, the earlier review was the first to summarize long-term patient outcomes from PSO device use but was limited by the exclusion of retrospective studies. Retrospective studies form a large proportion of cleft palate literature, our review suggests 73% of cleft palate literature is retrospective in nature. As such, excluding retrospective studies in this field significantly limits the strength of the review by limiting the number studies from which conclusions may be integrated. With our more recent review and inclusion of retrospective studies, this second review is a more inclusive and up-to-date systematic review than the original review done in 2011 (Uzel and Alparslan, 2011). Despite differences in the timeline and inclusion criteria of both systematic reviews, the overall results are similar; there is no definite conclusion on the long-term outcomes in patients who have received PSO treatment.
A limitation of this study is the search terms that were used. The search terms were selected to be broad in an attempt to include the maximum number of articles possible. Despite this, not all published articles may have been included using the search terms that were selected. For this reason, all of the reference lists were also included in an attempt to find any articles not included by the selected search terms.
Conclusion
According to the present literature, there still remains no consensus on the long-term effects of PSO devices. Research in the field of cleft lip and palate is greatly limited by small sample sizes and confounding factors such as multisurgeon cohorts with multiple different protocols for patient management. This systematic review has further highlighted the variability that exists in cleft palate literature. In addition, there are very few studies comparing different types of PSO devices and the studies that do exist are often limited by methodological flaws. Moving forward, further research comparing within the different types of active and passive PSO devices may provide additional insight. However, in such research confounding factors need to be eliminated from the comparison groups so that control and experimental groups are uniform in the way they are managed clinically. An additional confounding factor that may influence patient outcomes and that should be accounted for in future research is the experience and skill of the individual making and adjusting the PSO devices. Finally, these studies should match patients between treatment groups based on cleft severity. This would improve reliability of the research and may help resolve the differing conclusions as to how PSO devices affect long-term facial growth, dental arch development, and nasolabial aesthetics.
Supplemental Material
Supplemental Material, sj-pdf-1-cpc-10.1177_1055665621998176 for Systematic Review of the Long-Term Effects of Presurgical Orthopedic Devices on Patient Outcomes by Katie Garland, Brendan McNeely, Luc Dubois and Damir Matic in The Cleft Palate-Craniofacial Journal
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Katie Garland, MSc https://orcid.org/0000-0001-9069-5683
Brendan McNeely, BSc, MSc https://orcid.org/0000-0002-3862-4404
Supplemental Material: Supplemental material for this article is available online.
References
- Adali N, Mars M, Petrie A, Noar J, Sommerlad B. Presurgical orthopedics has no effect on archform in unilateral cleft lip and palate. Cleft Palate Craniofac J. 2012;49(1):5–13. doi:10.1597/11-030 [DOI] [PubMed] [Google Scholar]
- Asher-McDade C, Brattström V, Dahl E, McWilliam J, Mølsted K, Plint DA, Prahl-Andersen B, Semb G, Shaw WC, The RP. A six-center international study of treatment outcome in patients with clefts of the lip and palate: part 4. Assessment of nasolabial appearance. Cleft Palate Craniofac J. 1992;29(5):409–412. doi:10.1597/1545-1569_1992_029_0409_asciso_2.3.co_2 [DOI] [PubMed] [Google Scholar]
- Bajaj A, Rao KS, Sharma SM, Shetty V. Modified presurgical nasoalveolar molding in the infants with complete unilateral cleft lip and palate: a stepwise approach. J Maxillofac Oral Surg. 2011;10(3):275–280. doi:10.1007/s12663-011-0232-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bardach J, Morris HL, Olin WH. Late results of primary veloplasty: the Marburg Project. Plast Reconstr Surg. 1984;73(2):207–218. doi:10.1097/00006534-198402000-00007 [DOI] [PubMed] [Google Scholar]
- Barillas I, Dec W, Warren SM, Cutting CB, Grayson BH. Nasoalveolar molding improves long-term nasal symmetry in complete unilateral cleft lip-cleft palate patients. Plast Reconstr Surg. 2009;123(3):1002–1006. doi:10.1097/PRS.0b013e318199f46e [DOI] [PubMed] [Google Scholar]
- Bongaarts CAM, Kuijpers-Jagtman AM, van ‘t Hof MA, Prahl-Andersen B. The effect of infant orthopedics on the occlusion of the deciduous dentition in children with complete unilateral cleft lip and palate (Dutchcleft). Cleft Palate Craniofac J. 2004;41(6):633–641. doi:10.1597/03-051.1 [DOI] [PubMed] [Google Scholar]
- Bongaarts CAM, Prahl-Andersen B, Bronkhorst EM, Prahl C, Ongkosuwito EM, Borstlap WA, Kuijpers-Jagtman AM. Infant orthopedics and facial growth in complete unilateral cleft lip and palate until six years of age (Dutchcleft). Cleft Palate Craniofac J. 2009;46(6):654–663. doi:10.1597/08-034.1 [DOI] [PubMed] [Google Scholar]
- Bongaarts CAM, Prahl-Andersen B, Bronkhorst EM, Spauwen PH, Mulder JW, Vaandrager JM, Kuijpers-Jagtman AM. Effect of infant orthopedics on facial appearance of toddlers with complete unilateral cleft lip and palate (Dutchcleft). Cleft Palate Craniofac J. 2008;45(4):407–413. doi:10.1597/07-043.1 [DOI] [PubMed] [Google Scholar]
- Bongaarts CAM, van ‘t Hof MA, Prahl-Andersen B, Dirks IV, Kuijpers-Jagtman AM. Infant orthopedics has no effect on maxillary arch dimensions in the deciduous dentition of children with complete unilateral cleft lip and palate (Dutchcleft). Cleft Palate Craniofac J. 2006;43(6):665–672. doi:10.1597/05-129 [DOI] [PubMed] [Google Scholar]
- Brattstrom V, McWilliam J, Larson O, Semb G. Craniofacial development in children with unilateral clefts of the lip, alveolus, and palate treated according to three different regimes. Assessment of nasolabial appearance. Scand J Plast Reconstr Surg Hand Surg. 1992;26(3):313–319. doi:10.3109/02844319209015277 [DOI] [PubMed] [Google Scholar]
- Brattström V, Mølsted K, Prahl-Andersen B, Semb G, Shaw WC. The Eurocleft study: intercenter study of treatment outcome in patients with complete cleft lip and palate. Part 2: craniofacial form and nasolabial appearance. Cleft Palate Craniofac J. 2005;42(1):69–77. doi:10.1597/02-119.2.1 [DOI] [PubMed] [Google Scholar]
- Chan KT, Hayes C, Shusterman S, Mulliken JB, Will LA. The effects of active infant orthopedics on occlusal relationships in unilateral complete cleft lip and palate. Cleft Palate Craniofac J. 2003;40(5):511–517. doi:10.1597/1545-1569_2003_040_0511_teoaio_2.0.co_2 [DOI] [PubMed] [Google Scholar]
- Clark SL, Teichgraeber JF, Fleshman RG, Shaw JD, Chavarria C, Kau CH, Gateno J, Xia JJ. Long-term treatment outcome of presurgical nasoalveolar molding in patients with unilateral cleft lip and palate. J Craniofac Surg. 2011;22(1):333–336. doi:10.1097/SCS.0b013e318200d874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daskalogiannakis J, Mercado A, Russell K, Hathaway R, Dugas G, Long RE, Jr, Cohen M, Semb G, Shaw W. The Americleft study: an inter-center study of treatment outcomes for patients with unilateral cleft lip and palate part 3. Analysis of craniofacial form. Cleft Palate Craniofac J. 2011;48(3):252–258. doi:10.1597/09-185.1 [DOI] [PubMed] [Google Scholar]
- Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384. doi:10.1136/jech.52.6.377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friede H, Enemark H. Long-term evidence for favorable midfacial growth after delayed hard palate repair in UCLP patients. Cleft Palate Craniofac J. 2001;38(4):323–329. doi:10.1597/1545-1569_2001_038_0323_lteffm_2.0.co_2 [DOI] [PubMed] [Google Scholar]
- Grayson BH, Santiago PE, Brecht LE, Cutting CB. Presurgical nasoalveolar molding in infants with cleft lip and palate. Cleft Palate Craniofac J. 1999;36(6):486–498. doi:10.1597/1545-1569_1999_036_0486_pnmiiw_2.3.co_2 [DOI] [PubMed] [Google Scholar]
- Hathaway R, Daskalogiannakis J, Mercado A, Russell K, Long RE, Jr, Cohen M, Semb G, Shaw W. The Americleft study: an inter-center study of treatment outcomes for patients with unilateral cleft lip and palate part 2. Dental arch relationships. Cleft Palate Craniofac J. 2011;48(3):244–251. doi:10.1597/09-181.1 [DOI] [PubMed] [Google Scholar]
- Hay N, Patel B, Haria P, Sommerlad B. Maxillary growth in cleft lip and palate patients, with and without vomerine flap closure of the hard palate at the time of lip repair: a retrospective analysis of prospectively collected nonrandomized data, with 10-year cephalometric outcomes. Cleft Palate Craniofac J. 2018;55(9):1205–1210. doi:10.1177/1055665618764960 [DOI] [PubMed] [Google Scholar]
- Hegde RJ, Kharkar VR, Kamath S. Presurgical nasoalveolar molding in unilateral cleft lip and palate. Contemp Clin Dent. 2015;6(4):567–569. doi:10.4103/0976-237X.169865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heliovaara A, Skaare P, Kuseler A, Shaw W, Mølsted K, Karsten A, Marcusson A, Brinck E, Rizell S, Sæle P, et al. Scandcleft randomized trials of primary surgery for unilateral cleft lip and palate. Dental arch relationships in 8 year-olds. Eur J Orthod. 2020;42(1):1–7. doi:10.1093/ejo/cjz067 [DOI] [PubMed] [Google Scholar]
- Henkel KO, Gundlach KK. Analysis of primary gingivoperiosteoplasty in alveolar cleft repair. Part I: facial growth. J Craniomaxillofac Surg. 1997;25(5):266–269. [DOI] [PubMed] [Google Scholar]
- Isik Aslan B, Gulsen A, Findikcioglu K, Uzuner D, Ucuncu N. Effects of nasoalveolar molding therapy on alveolar and palatal cleft deformities in unilateral and bilateral cleft lip and palate. J Craniofac Surg. 2018;29(2):e179–e184. doi:10.1097/SCS.0000000000004243 [DOI] [PubMed] [Google Scholar]
- Joos U. Skeletal growth after muscular reconstruction for cleft lip, alveolus, and palate. Br J Oral Maxillofac Surg. 1995;33(3):139–144. doi:10.1016/0266-4356(95)90285-6 [DOI] [PubMed] [Google Scholar]
- Kornbluth M, Campbell RE, Daskalogiannakis J, Ross EJ, Glick PH, Russell KA, Doucet JC, Hathaway RR, Long RE, Jr, Sitzman TJ. Active presurgical infant orthopedics for unilateral cleft lip and palate: intercenter outcome comparison of Latham, modified McNeil, and nasoalveolar molding. Cleft Palate Craniofac J. 2018;55(5):639–648. doi:10.1177/1055665618757367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson M, Sallstrom KO, Larson O, McWilliam J, Ideberg M. Morphologic effect of preoperative maxillofacial orthopedics (T-traction) on the maxilla in unilateral cleft lip and palate patients. Cleft Palate Craniofac J. 1993;30(1):29–34. doi:10.1597/1545-1569_1993_030_0029_meopmo_2.3.co_2 [DOI] [PubMed] [Google Scholar]
- Liang Z, Yao J, Chen PKT, Zheng C, Yang J. Effect of presurgical nasoalveolar molding on nasal symmetry in unilateral complete cleft lip/palate patients after primary cheiloplasty without concomitant nasal cartilage dissection: early childhood evaluation. Cleft Palate Craniofac J. 2018;55(7):935–940. doi:10.1597/14-296 [DOI] [PubMed] [Google Scholar]
- Lin J, Allareddy V, Ross E, Shusterman S. A comparison of mixed dentition dental development in cleft patients treated with and without the Latham-type appliance. Pediatr Dent. 2017;39(1):53–58. [PubMed] [Google Scholar]
- Mars M, Asher-McDade C, Brattström V, Dahl E, McWilliam J, Mølsted K, Plint DA, Prahl-Andersen B, Semb G, Shaw WC, et al. A six-center international study of treatment outcome in patients with clefts of the lip and palate: part 3. Dental arch relationships. Cleft Palate Craniofac J. 1992;29(5):405–408. doi:10.1597/1545-1569_1992_029_0405_asciso_2.3.co_2 [DOI] [PubMed] [Google Scholar]
- Massie JP, Bruckman K, Rifkin WJ, Runyan CM, Shetye PR, Grayson B, Flores RL. The effect of nasoalveolar molding on nasal airway anatomy: a 9-year follow-up of patients with unilateral cleft lip and palate. Cleft Palate Craniofac J. 2018;55(4):596–601. doi:10.1177/1055665617744062 [DOI] [PubMed] [Google Scholar]
- Millard DR, Latham R, Huifen X, Spiro S, Morovic C. Cleft lip and palate treated by presurgical orthopedics, gingivoperiosteoplasty, and lip adhesion (POPLA) compared with previous lip adhesion method: a preliminary study of serial dental casts. Plast Reconstr Surg. 1999;103(6):1630–1644. doi:10.1097/00006534-199905060-00009 [DOI] [PubMed] [Google Scholar]
- Mishima K, Mori Y, Sugahara T, Minami K, Sakuda M. Comparison between palatal configurations in UCLP infants with and without a Hotz plate until four years of age. Cleft Palate Craniofac J. 2000;37(2):185–190. doi:10.1597/1545-1569_2000_037_0185_cbpciu_2.3.co_2 [DOI] [PubMed] [Google Scholar]
- Mishra B, Singh AK, Zaidi J, Singh GK, Agrawal R, Kumar V. Presurgical nasoalveolar molding for correction of cleft lip nasal deformity: experience from northern India. Eplasty. 2010;10:e55. [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi:10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mølsted K, Asher-McDade C, Brattström V, Dahl E, Mars M, McWilliam J, Plint DA, Prahl-Andersen B, Semb G, Shaw WC, et al. A six-center international study of treatment outcome in patients with clefts of the lip and palate: part 2. Craniofacial form and soft tissue profile. Cleft Palate Craniofac J. 1992;29(5):398–404. doi:10.1597/1545-1569_1992_029_0398_asciso_2.3.co_2 [DOI] [PubMed] [Google Scholar]
- Mølsted K, Brattström V, Prahl-Andersen B, Shaw WC, Semb G. The Eurocleft study: intercenter study of treatment outcome in patients with complete cleft lip and palate. Part 3: dental arch relationships. Cleft Palate Craniofac J. 2005;42(1):78–82. doi:10.1597/02-119.3.1 [DOI] [PubMed] [Google Scholar]
- Monasterio L, Ford A, Gutierrez C, Tastets ME, Garcia J. Comparative study of nasoalveolar molding methods: nasal elevator plus DynaCleft(R) versus NAM-Grayson in patients with complete unilateral cleft lip and palate. Cleft Palate Craniofac J. 2013;50(5):548–554. doi:10.1597/11-245 [DOI] [PubMed] [Google Scholar]
- Mylin WK, Hagerty RF. Midfacial skeletal profile in early and late closure of the hard palate. South Med J. 1983;76(5):610–612. doi:10.1097/00007611-198305000-00020 [DOI] [PubMed] [Google Scholar]
- Nakamura N, Sasaguri M, Nozoe E, Nishihara K, Hasegawa H, Nakamura S. Postoperative nasal forms after presurgical nasoalveolar molding followed by medial-upward advancement of nasolabial components with vestibular expansion for children with unilateral complete cleft lip and palate. J Oral Maxillofac Surg. 2009;67(10):2222–2231. doi:10.1016/j.joms.2009.04.098 [DOI] [PubMed] [Google Scholar]
- Patel PA, Rubin MS, Clouston S, Lalezaradeh F, Brecht LE, Cutting CB, Shetye PR, Warren SM, Grayson BH. Comparative study of early secondary nasal revisions and costs in patients with clefts treated with and without nasoalveolar molding. J Craniofac Surg. 2015;26(4):1229–1233. doi:10.1097/SCS.0000000000001729 [DOI] [PubMed] [Google Scholar]
- Peanchitlertkajorn S, Mercado A, Daskalogiannakis J, Hathaway R, Russell K, Semb G, Shaw W, Lamichane M, Fessler J, Long RE, Jr. An intercenter comparison of dental arch relationships and craniofacial form including a center using nasoalveolar molding. Cleft Palate Craniofac J. 2018;55(6):821–829. doi:10.1597/16-018 [DOI] [PubMed] [Google Scholar]
- Prahl C, Kuijpers-Jagtman AM, Van ‘t Hof MA, Prahl-Andersen B. A randomized prospective clinical trial of the effect of infant orthopedics in unilateral cleft lip and palate: prevention of collapse of the alveolar segments (Dutchcleft). Cleft Palate Craniofac J. 2003;40(4):337–342. doi:10.1597/1545-1569_2003_040_0337_arpcto_2.0.co_2 [DOI] [PubMed] [Google Scholar]
- Prahl C, Kuijpers-Jagtman AM, van’t Hof MA, Prahl-Andersen B. A randomised prospective clinical trial into the effect of infant orthopedics on maxillary arch dimensions in unilateral cleft lip and palate (Dutchcleft). Eur J Oral Sci. 2001;109(5):297–305. doi:10.1034/j.1600-0722.2001.00056.x [DOI] [PubMed] [Google Scholar]
- Prahl C, Prahl-Andersen B, van ‘t Hof MA, Kuijpers-Jagtman AM. Infant orthopedics and facial appearance: a randomized clinical trial (Dutchcleft). Cleft Palate Craniofac J. 2006;43(6):659–664. doi:10.1597/05-139 [DOI] [PubMed] [Google Scholar]
- Rubin MS, Clouston SAP, Esenlik E, Shetye PR, Flores RL, Grayson BH. Midface growth in patients with unilateral cleft lip and palate treated with a nasoalveolar molding protocol. J Craniofac Surg. 2019;30(6):1640–1643. doi:10.1097/SCS.0000000000005356 [DOI] [PubMed] [Google Scholar]
- Shetty V, Agrawal RK, Sailer HF. Long-term effect of presurgical nasoalveolar molding on growth of maxillary arch in unilateral cleft lip and palate: randomized controlled trial. Int J Oral Maxillofac Surg. 2017;46(8):977–987. doi:10.1016/j.ijom.2017.03.006 [DOI] [PubMed] [Google Scholar]
- Singer E, Daskalogiannakis J, Russell KA, Mercado AM, Hathaway RR, Stoutland A, Long RE, Jr, Fessler J, Semb G, Shaw WC. Burden of care of various infant orthopedic protocols for improvement of nasolabial esthetics in patients with CUCLP. Cleft Palate Craniofac J. 2018;55(9):1236–1243. doi:10.1177/1055665618766978 [DOI] [PubMed] [Google Scholar]
- Uzel A, Alparslan ZN. Long-term effects of presurgical infant orthopedics in patients with cleft lip and palate: a systematic review. Cleft Palate Craniofac J. 2011;48(5):587–595. doi:10.1597/10-008 [DOI] [PubMed] [Google Scholar]
- Winters JC, Hurwitz DJ. Presurgical orthopedics in the surgical management of unilateral cleft lip and palate. Plast Reconstr Surg. 1995;95(4):755–764. doi:10.1097/00006534-199504000-00024 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-pdf-1-cpc-10.1177_1055665621998176 for Systematic Review of the Long-Term Effects of Presurgical Orthopedic Devices on Patient Outcomes by Katie Garland, Brendan McNeely, Luc Dubois and Damir Matic in The Cleft Palate-Craniofacial Journal