Abstract
Although the linkage between traumatic life events and psychotic-like experiences (PLEs) is well established, the knowledge of potential mechanisms of this relationship is scarce. The aim of the present study was to better understand the structure of connections between traumatic life events and PLEs by considering at the same time the role of cognitive biases and depressive symptoms in the population of young adults (18–35 years of age, M = 26.52, SD = 4.74, n = 6772). Our study was conducted within a framework of network analysis. PLEs were measured with the Prodromal Questionnaire (PQ-16), cognitive biases were measured with nine items from the Davos Assessment of Cognitive Biases Scale-18 (DACOBS-18), depressive symptoms were assessed with the Center for Epidemiologic Studies–Depression Scale (CESD-R) and exposure to traumatic life events was measured with a combination of Childhood Experience of Care and Abuse Questionnaire (CECA.Q) and Traumatic Experience Checklist (TEC). The results present a network of all nodes being interconnected within and between domains, with no isolated factors. Exposures to sexual trauma were the most central node in the network. Pathways were identified from trauma to PLEs via cognitive biases and depressive symptoms. However, the shortest pathway between the most central traumatic life event and PLEs was through other traumatic life events, without cognitive biases or depressive symptoms along the way. Our findings suggest the importance of environmental adversities as well as dysfunctional information processing and depression in the network of psychosis risks.
Keywords: psychosis, early trauma, cognitive biases, network analysis, risk of psychosis
Introduction
Accumulating empirical evidence supports the notion that psychopathology constitutes a dynamic, complex, and multifactorial system.1–3 In addition, boundaries between different psychiatric disorders, as well as boundaries between mental health and illness, have been found to be rather fluid, suggesting psychopathology should best be approached as a dimensional entity.4 In parallel, over the last decade, there were exceptional advances in dynamic system theories and network statistics,5–7 in which psychopathology is viewed as a dimensional and multifactorial construct consisted of different interconnected elements (eg, symptoms, cognition, and emotional regulation). An assumption of the network approach is that different symptoms within the network are causally coupled (ie, one symptom may activate another). These developments have led to a growing interest in the empirical applicability of network theories to the field of psychopathology8–10 and, more recently, to psychosis in particular.11,12
Although there is an increasing number of promising network studies investigating the psychopathology of psychosis or its risk states as a network of different interconnected symptoms,13–19 our understanding of interrelations between various processes involved in psychosis risk (eg, cognitive biases and exposure to traumatic life events) associated with psychotic symptoms or psychotic-like experiences (PLEs) in the network is scarce. To date, only a few studies considered factors beyond psychopathological symptoms in the network of psychosis.20,21 Recently, Isvoranu and colleagues20 have found that all measured types of childhood trauma are related to psychotic symptoms via general psychopathology symptoms dimension (anxiety exclusively), which was interpreted as in accordance with an affective pathway from trauma to psychosis risk. Similarly, there is only a limited number of studies on schizotypal traits14,15 and PLEs in the general population.22 In a recent general population study,22 it was shown that paranoia-like ideations were the most central in the PLEs network. These studies investigated the interconnectedness of different PLEs or schizotypal traits in large samples focusing mainly on the network structure of different symptoms.14,15 Hence, the extended network structure that goes beyond PLEs or schizotypal traits, as well as potential mechanisms of the information spread within the network, remains unknown.
Furthermore, the interconnectedness between environmental risk (eg, exposure to traumatic life events), cognitive biases and depression, that have been consistently linked to the risk for psychosis and psychotic-like experiences,23–26 have not been well incorporated into the network approach. Howes and Murray in their model27 suggested that dysfunctional cognitive biases may moderate or mediate the relationship between exposure to traumatic life events and psychosis. In line with these predictions, recent studies have found that different dysfunctional cognitive biases are significant mediators in the relationship between exposures to traumatic life events and the risk for psychosis in clinical28 and nonclinical populations.29–32 These findings are in accordance with a general cognitive model suggesting that exposure to traumatic events change cognitive architecture and lead to a dysfunctional response to environmental circumstances. At the same time, it has also been found that exposure to traumatic life events may lead to the risk states of psychosis via increased stress-sensitivity.33 According to cognitive models of psychosis34,35 and empirical studies,36–38 these two perspectives, cognitive and emotional, are no alternatives, but rather should be considered jointly.
In the present study, we aimed to extend prior investigations of the unifactorial symptom network structure to a multifactorial network structure of psychosis risks. In particular, we were interested in the potential cognitive and emotional pathways linking exposure to childhood traumatic life events, cognitive biases, and depression, that have been consistently reported in the literature as risk factors for psychosis, to PLEs. For that purpose, we measured exposure to different types of traumatic life events, cognitive biases, depressive symptoms, and PLEs in a large nonclinical sample. Moreover, we aimed to identify the most central traumatic life event and PLEs in the network as well as to find the shortest pathways between them.
Methods
Participants
A total sample of 6772 young adults, aged 18–35 years, were recruited from the general population to participate in an online survey. The computer-assisted web interview (CAWI) method was used. Completing the online survey took about 30 min. Participants were enrolled from three large Polish cities: Warsaw (1 700 000 inhabitants), Krakow (770 000 inhabitants), and Wroclaw (640 000 inhabitants). A history of any psychiatric diagnosis was screened with a self-report questionnaire (“Have you ever been diagnosed with the psychiatric disorder? If so, specify the disorder”). Demographic information (age, gender, education, and professional situation) was also obtained. The study was approved by the Ethics Committee of the Medical University of Warsaw, Poland.
Measures
Psychotic-like Experiences (PLEs)
To assess PLEs, we used the Prodromal Questionnaire (PQ-16)39—a 16-item self-report scale to screen for psychosis risk operationalized as the presence of PLEs. The original PQ-16 includes two scales: present vs non-present (true vs false) and distress associated with the experience (four-point Likert scale). In the current study, we focused only on the first scale (presence vs absence), which we modified to better capture the frequency of PLEs. Specifically, we used a four-point scale: “never,” “sometimes,” “often,” and “almost always.” We excluded two items regarding anxiety and depression symptoms as we concentrated only on the attenuated positive symptoms.
Cognitive Biases
For the measurement of cognitive biases, we used a short 18-item version of the Davos Assessment of Cognitive Biases Scale (DACOBS).40 We focused on two subscales of the DACOBS-18 that have been proven to be the best predictors of psychosis risk.41 These two subscales included in the study consist of nine items that assess Safety Behaviors and Attentional Biases.
Exposure to Childhood Trauma
To evaluate an early exposure to traumatic life events, we focused on emotional, peer-on-peer, and sexual abuse that took place during childhood. To assess emotional neglect and abuse, we used two items from the Traumatic Experience Checklist (TEC).42 Sexual trauma was measured with three items that we took from the Childhood Experience of Care and Abuse Questionnaire (CECA.Q).43 In addition, we included one item to assess bullying and/or physical abuse from peers.
Depressive Symptoms
The Center for Epidemiologic Studies–Depression Scale (CESD-R)44 was used to measure current depressive symptomatology according to DSM-IV-R. In our study, we used a short version of the scale that consists of five items with the highest correlations with the total score.
A detailed description of all measures can be found in Supplementary Material.
Statistical Analyses
First, we estimated the network where each node (depicted as a circle) represents single items from the scales: PQ-16, DACOBS, CES-D, and CT (childhood trauma). Nodes are connected by edges (depicted as lines), which represent the relationship between two variables, after controlling for all other variables in the network. Thus, if two nodes are unconnected, they are conditionally independent. Wider and more saturated edges represent stronger relations. As our data consisted of both ordinal and binary data, we estimated the network with the use of Mixed Graphical Models that are designed for mixed data.45 Following recent work by Fried et al,46 we treated variables on a four-point scale (PQ-16 and CES-D), along with variables on a seven-point scale (DACOBS), as continuous. Items representing exposure to childhood trauma (CT) were coded as binary variables. In our model, all relationships represent pairwise interactions. In order to limit the number of estimated parameters and avoid estimating spurious relations among variables, we used an L1-penalized regression (LASSO).47 This shrinks all edge weights, setting the smallest exactly to zero, which results in a more parsimonious and interpretable network. We selected the penalty parameter using the Extended Bayesian Information Criterion (EBIC).48 The EBIC itself utilizes a tuning hyperparameter γ, which we set to 0.5, as suggested in the literature.47,48 The network layout was based on the Fruchterman–Reingold algorithm, which places highly connected nodes towards the center and weakly associated closer to the periphery.
Second, we analyzed the resulting network by estimating node strength and node predictability. Node strength is a centrality indicator that captures the importance of each node in the network. More precisely, it is a measure of the sum of the absolute edge weights connected to the node. This measure is considered to be the most important centrality estimate in psychopathology research as the activation of a symptom represented by a node of the highest strength will presumably be followed by the activation of other symptoms.49 Node predictability is a measure that calculates how much of a node’s variance can be explained by nodes directly connected to it in the network. For continuous variables, predictability is equal to the proportion of variance that is explained by neighboring nodes. For binary variables, predictability provides a normalized accuracy measure, which shows how well a node was determined by connecting nodes in the network beyond the intercept model.50
Next, the robustness of the obtained network was investigated by testing the accuracy of edge weights and the stability of strength centrality.7 We used a nonparametric bootstrapping (n = 1000) to construct 95% bootstrapped confidence intervals (CIs) for all edge weights and to calculate the edge weights difference test that estimates if edge weights differ from each other significantly. Further, we estimated the stability of the strength centrality coefficient with the use of subsetting bootstrap. This procedure results in a centrality-stability coefficient (CS-coefficient) that should be above 0.5. We also performed the strength centrality difference test that calculates which centrality estimates differ from each other significantly.7
The final step was the estimation of the network that illustrates the shortest pathways between the most central item of CT and the items of PQ-16. This type of network highlights the possible pathways of influence and mediating items between exposure to trauma and PLEs.20 The shortest path between any two nodes reflects the minimum number of steps needed to go from one node to the other (eg, from childhood trauma to PLEs), which is calculated using Dijkstra’s algorithm.51
Descriptive analyses were performed using the Statistical Package for Social Sciences (SPSS), version 25.0. Network analyses were conducted with R software (version 3.6.3). Specifically, we used the following packages: mgm52 (version 1.2–10) for network estimation and node predictability, qgraph45 (version 1.6.5) for network visualization, and bootnet7 (version 1.4.3) for stability analysis.
Results
Sample Characteristics
There was no missing data in our sample, therefore all of 6772 participants were included in the analyses. In our sample, 4383 (64.7%) participants obtained the Ising’s cutoff score of 6 or more symptoms in the PQ-16.1 Ising et al39 found in their study that this cutoff identifies “caseness” of UHR/psychosis best with a sensitivity of 87%. The characteristics of the sample are presented in table 1.
Table 1.
Sample Characteristics
| N (%) | |
|---|---|
| Gender | |
| Male | 2488 (36.7%) |
| Female | 4284 (63.3%) |
| Professional situation | |
| Study | 2365 (34.9%) |
| Work | 4951 (73.1%) |
| Unemployed | 414 (6.1%) |
| Rent | 43 (0.6%) |
| Education | |
| Primary | 180 (2.7%) |
| Secondary | 227 (3.4%) |
| Vocational | 2234 (33.0%) |
| Incomplete higher | 1094 (16.2%) |
| Higher | 3037 (44.8%) |
| Psychiatric Diagnosis | 1154 (17.0%) |
| Anxiety disorder | 564 (8.3%) |
| Depression | 809 (11.9%) |
| Bipolar disorder | 71 (1.0%) |
| Psychotic disorder | 33 (0.5%) |
| Obsessive-compulsive disorder | 104 (1.5%) |
| SPA dependence | 82 (1.2%) |
| Eating disorder | 167 (2.5%) |
| Personality disorder | 184 (2.7%) |
| Other disorder | 127 (1.9%) |
| Mean (SD) | |
| Age | 26.52 (4.74) |
| PQ-16 (total score) | 9.27 (6.41) |
| DACOBS-9 (total score) | 26.89 (8.88) |
| CES-D (total score) | 9.14 (3.70) |
| Childhood Trauma (CT, total score) | 1.74 (1.49) |
| N (%) | |
| Participants without any exposition to trauma | 1795 (26.5%) |
| Participants exposed to 1 trauma event | 1502 (22.2%) |
| Participants exposed to 2 trauma events | 1297 (19.2%) |
| Participants exposed to 3 trauma events | 1514 (22.4%) |
| Participants exposed to >3 trauma events | 664 (9.7%) |
Note: PQ-16, Prodromal Questionnaire; DACOBS-9, Davos Assessment of the Cognitive Biases Scale; CES-D, The Center for Epidemiologic Studies-Depression Scale.
Network Structure
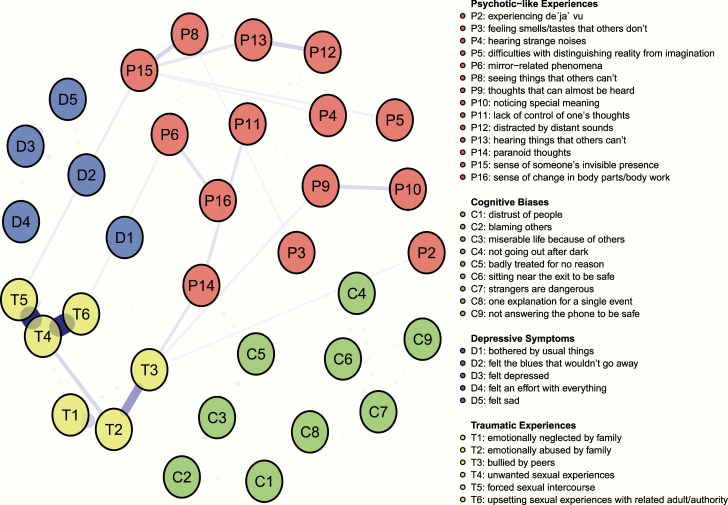
The resulting network of 34 items representing exposure to trauma, PLEs, cognitive biases, and depressive symptoms is depicted in figure 1.2 The network was well connected and had no isolated nodes. Nodes within each of the four domains were more closely related to each other than with nodes of other domains. The strongest connections across domains emerged between psychosis items P14 (paranoid thoughts) and cognitive bias item C5 (badly treated for no reason); P14 and trauma item T3 (bullied by peers); trauma item T6 (upsetting sexual experiences with related adult/authority) and cognitive bias item C4 (not going out after dark). All edges were positive.
Fig. 1.
The network.
Strength Centrality
The strength centrality measure is illustrated in figure 2. Items representing exposure to trauma, especially item T4 (unwanted sexual experiences), had the highest standardized strength, suggesting that these may be influential nodes within this network. Nodes that showed the highest strength in other domains were: node P14 (paranoid thoughts) for PLEs; node D3 for depressive symptoms (felt depressed); and node C3 for cognitive biases (miserable life because of others).
Fig. 2.
The strength centrality estimates for each node in the network. Note: Presented strength centrality indices are standardized (ie, z-scores).
Node Predictability
Node predictability ranges from 0.04 in node T6 (upsetting sexual experiences with related adult/authority) to 0.67 in node D3 (felt depressed), with an average of 0.35. This means that, on average, 35% of the variance of each node in the network can be explained by its neighbors. The average predictability of each domain was: 0.51 for depressive symptoms, 0.34 for cognitive biases, 0.32 for PLEs, and 0.29 for exposure to trauma. The lowest average predictability for trauma indicates that the variance in these nodes is not well explained by other nodes included in the network. Node predictability values for each item are presented in Supplementary table S1).
Shortest Pathways
The shortest paths between node T4 (unwanted sexual experiences), which is the most central node within the trauma domain, and all individual nodes from the PLEs domain are presented in figure 3. Node T4 has no direct connection with any of PLEs items and to reach them, it needs to run via at least one other trauma item. Such shortest pathways with only one item mediating go from T4 via T5 (forced sexual intercourse) to P8 (seeing things that others cannot) and P15 (sense of someone’s invisible presence), and via T6 (upsetting sexual experiences with related adult/authority) to P6 (mirror-related phenomena). All other shortest paths involve various combinations of two or three trauma and PLEs items. Most of these pathways run through items T5 and P15 or T2 (emotionally abused by family) and T3 (bullied by peers). None of the shortest paths goes via nodes representing cognitive biases or depressive symptoms. The shortest pathways from the remaining five items representing trauma to PLEs are presented in Supplementary figures S5–S9).
Fig. 3.
The shortest path between node T4 and all items of PQ-16.
Network Accuracy and Stability
Results of stability and accuracy analyses are presented in Supplementary Materials. The edge weight bootstrap reported bootstrapped confidence intervals of an acceptable width suggesting estimation of sufficient precision. The edge weight and centrality difference tests revealed that stronger edges in the network were significantly stronger than the other edges as well as strength estimates in nodes with high strength centrality were statistically different from strength estimates in nodes with low strength centrality. The subset bootstrap showed high stability of strength centrality measure with CS value of 0.75.
Discussion
For the very first time, in the present study, we provided the network structure of the relationship between exposure to traumatic life events, cognitive biases, depressive symptoms, and PLEs in a large sample of young adults at their highest peak for the risk for psychosis in terms of age (ie, 18–35 years old) recruited from the general population. Hence, we were able to extend prior studies on the structure of PLEs and of the mechanisms of the relationship between trauma and psychosis53,54 by considering cognitive biases and depressive symptoms, that is, two risk factors for psychosis. The network derived from the study has satisfactory stability. In general, our findings depicted the network with well-connected nodes within and between different domains. In line with prior theoretical accounts27 and empirical studies,29,31,32,55,56 our findings thus suggest the importance of the interplay between different risk factors in predicting PLEs in the nonclinical population. Interestingly, in accordance with studies showing an important impact of life-adversities on the risk for psychosis,53,57 the network structure suggests that the most central nodes are related to exposure to traumatic life events. In line with a recent study on the network structure of PLEs conducted in the US general population,22 the most central node for the PLEs domain was related to paranoia-like ideations. Importantly, the node (a single item) related to sexual abuse had a higher strength centrality indicator showing that this type of life-adversity has the strongest relationships with other nodes in the network, particularly to the remaining trauma nodes. Strong connectivity between sexual trauma and different types of childhood traumatic life events may partially explain the centrality of unwanted sexual experiences in the network. At the same time, persecutory-like ideations, a feeling of being depressed and external attributions also have strong connections to the rest of the network’s nodes. The analyses of the shortest pathways between traumatic life events and PLEs revealed only direct connections, no bridging role of cognitive biases and depressive symptoms has been observed.
In accordance with theoretical accounts suggesting the importance of environmental factors in the development of the risk for psychosis,27 our findings suggest the strongest input to the network from nodes denoting exposures to traumatic life events. Although our study’s design was cross-sectional and thus did not allow for causal inferences, this finding fits well with Borsboom’s10 suggestion that important changes in the environment (ie, external field) may activate information spread in the network leading to the development of symptoms. It should be noted that although many relationships between nodes risk factors and symptoms may be bi-directional, we considered the relationship between early life adversity and the risk of psychosis as unidirectional. However, further developments in psychiatric symptoms and associated risk factors may increase the likelihood of exposures to life-adversities in the future (eg, increase the risk of violent victimization).58,59 Growing evidence from clinical and nonclinical populations suggests that exposures to trauma have an impact on the risk for psychosis.53,60,61 Some studies have also linked specific types of traumatic life events with specific PLEs,57,62 but others have not confirmed the specificity in the relationships.63 According to a recent meta-analysis, trauma is predominantly related to hallucinations and delusions,64 and some studies suggested a specific role of sexual trauma in predicting transition to psychosis among those at high clinical risk for psychosis.65 We found a strong connection between sexual abuse and paranoia-related ideations (P14). However, our analyses suggested that the shortest pathway between the most central node of traumatic experiences (ie, sexual abuse) leads to the most central PLEs (ie, persecutory-like ideations) via other traumatic experiences. Additional analyses suggested that most of the nodes of traumatic experiences (eg, emotional neglect and abuse) also lead to PLEs via other childhood life adversities. It implies that nodes within the childhood trauma domain are highly interconnected and information from any specific node in this domain is spread out to the PLEs domain via other traumatic experiences. Similar results have been obtained recently by Isvoranu et al20 in a network study conducted among patients diagnosed with psychotic disorders in which sexual trauma was related to psychotic symptoms via other traumatic experiences. Importantly, prior studies have reported a dose–response between exposures to traumatic life events and psychotic symptoms,66 which may be in accordance with the finding that different types of traumatic life events are strongly connected in the network.
Furthermore, in the previous study,20 the authors found that anxiety was the main link in the relationship between trauma and positive psychotic symptoms. Depression and emotional tension also played the role but to a smaller extent. Our study did not consider anxiety, with only different kinds of depressive symptoms included. However, none of the depressive symptoms bridged the shortest pathway between traumatic life events and PLEs. Similarly, our results suggest also that there are no shortest cognitive pathways between traumatic life events and PLEs. Our findings may seem contrary to a line of recent studies showing a mediating role of the cognitive biases in the relationship between exposures to traumatic life experiences and PLEs,29,31,32 or subclinical psychotic symptoms in a clinical sample.28 However, given the fact that the network analysis does not allow for testing mediation, one should not interpret our results as a lack of mediation. Prior studies31,32 tested mediation used regression of structural equation modeling approach on accumulating number of traumatic life events, cognitive biases, and PLEs. In the present study, in line with previous network studies, we analyzed single items as representing nodes in the network. Please note that when we conducted a supplementary analysis (see Supplementary table S2) of mediation according to some prior studies,28,29 we were able to confirm that both depressive symptoms and cognitive biases partially mediated the relationship between exposures to traumatic life experiences and PLEs.
Although the shortest pathways analysis between nodes of traumatic life events and PLEs did not suggest a pathway through depressive symptoms or cognitive biases, we found that the strongest connection in the network was between paranoia-related ideations (P14) and external attributions. This finding is in line with well-established knowledge of the linkage between paranoia and other psychotic symptoms with externalization as assessed with different measures.67,68 Subsequently, we also observed strong connections between sexual abuse (T6) and safety behaviors, which suggest, unsurprisingly, that exposures to severe adverse life events change cognitive, as well as the behavioral repertoire of response to environmental requirements following exposures to severe and, most notably, interpersonal trauma. It should be noted, that according to a recent study40 that used the same measure of cognitive biases as in our study, both attribution biases and safety behaviors had the highest discriminative power for clinical psychosis, suggesting that these domains may be important risk factors for psychosis.
Some limitations of our study should be discussed. First, our results are derived from an online survey conducted on a large nonclinical sample. Hence, we were unable to investigate extensively clinical characteristics of our participants with structured clinical interviews. However, it was shown that PLEs might be reliably assessed with self-report measures.69 It should also be noted that although there is a potential to generalize our results—within an extended psychosis phenotype hypothesis70—to clinical samples, this should be approached cautiously (eg, relatively low intensity of psychotic experiences). It is likely that exposure to trauma may differently impact cognition in a clinical and nonclinical sample, for example,71 and thus, differences in the network between different groups may appear. However, it seems that the general link between trauma and PLEs may be observed among both clinical and nonclinical contexts.72 Second, as stated above in the discussion, our study is cross-sectional, allowing no causal inferences. Longitudinal network studies are infeasible for time-invariant factors (eg, childhood trauma, genetics).21 Hence, at this stage, we are able to investigate the spatial architecture of the network (ie, connections within the network). However, future studies may investigate group differences (eg, traumatized vs untraumatized participants) on temporal characteristics of the network consists of time-variant factors (eg, cognition, symptoms, and emotional dysregulation). This will move from static to more dynamic models as suggested recently by some authors.73 It should also be noted that the results of node strength may be biased as variables belonging to the same domains (especially the biggest ones) may have stronger connections among themselves than with other nodes in the network, thus could rank higher on the centrality measure.74 Although the trauma domain, along with the depression domain, was the smallest one in our network, its variables had the strongest connections within. This could partially explain its high strength indices. Finally, future studies may explore other risk factors that we did not consider in the network (eg, genetics, aberrant salience, and emotional dysregulation).
To conclude, our study described a well-connected network of relationships between exposures to traumatic life experiences, depressive symptoms, cognitive biases, and PLEs in a large sample of young adults. Exposure to sexual abuse and its connections to other traumatic life events (ie, cumulative impact—traumatic events often co-occur75,76) seem to have, along with paranoia-related ideations, the strongest impact in the network. These findings suggest the importance of severe childhood adversities in the psychopathology of psychosis risks. Depressive symptoms and cognitive biases are both connected to PLEs and exposures to traumatic life events. However, these emotional and cognitive pathways are not a part of the shortest pathways between the most central, as well as other traumatic life events and PLEs.
Supplementary Material
Footnotes
In order to calculate the cutoff score we dichotomized the 4-point frequency scale to reflect the original scale used in Ising’s study (answers: “sometimes,” “often,” “almost always” were recoded as the presence of the experience).
The network is presented with cut value = 0.
Funding
This study was supported by the OPUS grant from the National Science Center, Poland (Ł.G., 2016/21/B/HS6/03210). B.N. was supported by an NHMRC Senior Research Fellowship (1137687). J.H. was supported by a McKenzie Fellowship.
Acknowledgment
The authors have declared that there are no conflicts of interest in relation to the subject of this study.
References
- 1. Wichers M, Wigman J, Myin-Germeys I. Micro-level affect dynamics in psychopathology viewed from complex dynamical system theory. J Index Metric. 2015;7(4):362–367. [Google Scholar]
- 2. Saxe GN, Statnikov A, Fenyo D, et al. A complex systems approach to causal discovery in psychiatry. PLoS One. 2016;11(3):e0151174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nelson B, McGorry PD, Wichers M, Wigman JTW, Hartmann JA. moving from static to dynamic models of the onset of mental disorder: a review. JAMA Psychiatry. 2017;74(5):528–534. [DOI] [PubMed] [Google Scholar]
- 4. Kotov R, Krueger RF, Watson D, et al. The Hierarchical Taxonomy of Psychopathology (HiTOP): a dimensional alternative to traditional nosologies. J Abnorm Psychol. 2017;126(4):454–477. [DOI] [PubMed] [Google Scholar]
- 5. Epskamp S, Cramer AOJ, Waldorp LJ, Schmittmann VD, Borsboom D. qgraph: network visualizations of relationships in psychometric data. J Stat Softw 2012;48(4):1–18. [Google Scholar]
- 6. Blanken TF, Van Der Zweerde T, Van Straten A, Van Someren EJW, Borsboom D, Lancee J. Introducing network intervention analysis to investigate sequential, symptom-specific treatment effects: a demonstration in co-occurring insomnia and depression. Psychother Psychosom. 2019;88(1):52–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: a tutorial paper. Behav Res Methods. 2018;50(1):195–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fried EI, van Borkulo CD, Cramer AO, Boschloo L, Schoevers RA, Borsboom D. Mental disorders as networks of problems: a review of recent insights. Soc Psychiatry Psychiatr Epidemiol. 2017;52(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Borsboom D, Cramer AO. Network analysis: an integrative approach to the structure of psychopathology. Annu Rev Clin Psychol. 2013;9:91–121. [DOI] [PubMed] [Google Scholar]
- 10. Borsboom DJWp. A network theory of mental disorders. World Psychiatry. 2017;16(1):5–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Galderisi S, Rucci P, Kirkpatrick B, et al. Interplay among psychopathologic variables, personal resources, context-related factors, and real-life functioning in individuals with schizophrenia: a network analysis. JAMA Psychiatry. 2018;75(4):396–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Strauss GP, Nuñez A, Ahmed AO, et al. The latent structure of negative symptoms in schizophrenia. JAMA Psychiatry. 2018;75(12):1271–1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dodell-Feder D, Saxena A, Rutter L, Germine L. The network structure of schizotypal personality traits in a population-based sample. Schizophr Res. 2019;208:258–267. [DOI] [PubMed] [Google Scholar]
- 14. Fonseca-Pedrero E, Ortuño J, Debbané M, et al. The network structure of schizotypal personality traits. Schizophr Bull. 2018;44(suppl_2):S468–S479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Polner B, Faiola E, Urquijo MF, et al. The network structure of schizotypy in the general population. Eur Arch Psychiatry Clin Neurosci. 2019:1–11. [DOI] [PMC free article] [PubMed]
- 16. Wigman JT, de Vos S, Wichers M, van Os J, Bartels-Velthuis AA. A transdiagnostic network approach to psychosis. Schizophr Bull. 2017;43(1):122–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bak M, Drukker M, Hasmi L, van Os JJPO. An n= 1 clinical network analysis of symptoms and treatment in psychosis. PLoS One 2016;11(9):e0162811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Klippel A, Viechtbauer W, Reininghaus U, et al. The cascade of stress: a network approach to explore differential dynamics in populations varying in risk for psychosis. Schizophr Bull. 2017;44(2):328–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. van Rooijen G, Isvoranu AM, Meijer CJ, et al. A symptom network structure of the psychosis spectrum. Schizophr Res. 2017;189:75–83. [DOI] [PubMed] [Google Scholar]
- 20. Isvoranu AM, van Borkulo CD, Boyette LL, et al. A network approach to psychosis: pathways between childhood trauma and psychotic symptoms. Schizophr Bull. 2017;43(1):187–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Isvoranu A-M, Guloksuz S, Epskamp S, van Os J, Borsboom D. Toward incorporating genetic risk scores into symptom networks of psychosis. Psychol Med. 2020;50(4):636–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Murphy J, McBride O, Fried E, Shevlin M. Distress, impairment and the extended psychosis phenotype: a network analysis of psychotic experiences in an US general population sample. Schizophr Bull. 2018;44(4):768–777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Fusar-Poli P, Nelson B, Valmaggia L, Yung AR, McGuire PK. Comorbid depressive and anxiety disorders in 509 individuals with an at-risk mental state: impact on psychopathology and transition to psychosis. Schizophr Bull. 2014;40(1):120–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Armando M, Nelson B, Yung AR, et al. Psychotic-like experiences and correlation with distress and depressive symptoms in a community sample of adolescents and young adults. Schizophr Res. 2010;119(1–3):258–265. [DOI] [PubMed] [Google Scholar]
- 25. Gawęda Ł, Li E, Lavoie S, Whitford TJ, Moritz S, Nelson B. Impaired action self-monitoring and cognitive confidence among ultra-high risk for psychosis and first-episode psychosis patients. Eur Psychiatry. 2018;47:67–75. [DOI] [PubMed] [Google Scholar]
- 26. Nelson B, Lavoie S, Gawęda Ł, et al. The neurophenomenology of early psychosis: an integrative empirical study. Conscious Cogn. 2020;77:102845. [DOI] [PubMed] [Google Scholar]
- 27. Howes OD, Murray RM. Schizophrenia: an integrated sociodevelopmental-cognitive model. Lancet. 2014;383(9929):1677–1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Appiah-Kusi E, Fisher HL, Petros N, et al. Do cognitive schema mediate the association between childhood trauma and being at ultra-high risk for psychosis? J Psychiatr Res. 2017;88:89–96. [DOI] [PubMed] [Google Scholar]
- 29. Gawęda Ł, Göritz AS, Moritz SJSr. Mediating role of aberrant salience and self-disturbances for the relationship between childhood trauma and psychotic-like experiences in the general population. Schizophr Res. 2019;206:149–156. [DOI] [PubMed] [Google Scholar]
- 30. Mętel D, Arciszewska A, Daren A, et al. Mediating role of cognitive biases, resilience and depressive symptoms in the relationship between childhood trauma and psychotic-like experiences in young adults. Early Interv Psychia. 2020;14(1):87–96. [DOI] [PubMed] [Google Scholar]
- 31. Gawęda Ł, Pionke R, Krężołek M, et al. Self-disturbances, cognitive biases and insecure attachment as mechanisms of the relationship between traumatic life events and psychotic-like experiences in non-clinical adults–a path analysis. Psychiatry Res. 2018;259:571–578. [DOI] [PubMed] [Google Scholar]
- 32. Gibson LE, Reeves LE, Cooper S, Olino TM, Ellman LM. Traumatic life event exposure and psychotic-like experiences: a multiple mediation model of cognitive-based mechanisms. Schizophr Res. 2019;205:15–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Rössler W, Ajdacic-Gross V, Rodgers S, Haker H, Müller M. Childhood trauma as a risk factor for the onset of subclinical psychotic experiences: exploring the mediating effect of stress sensitivity in a cross-sectional epidemiological community study. Schizophr Res. 2016;172(1–3):46–53. [DOI] [PubMed] [Google Scholar]
- 34. Garety PA, Kuipers E, Fowler D, Freeman D, Bebbington PE. A cognitive model of the positive symptoms of psychosis. Psychol Med. 2001;31(2):189–195. [DOI] [PubMed] [Google Scholar]
- 35. Freeman D, Garety PA. Connecting neurosis and psychosis: the direct influence of emotion on delusions and hallucinations. Behav Res Ther. 2003;41(8):923–947. [DOI] [PubMed] [Google Scholar]
- 36. Reininghaus U, Gayer-Anderson C, Valmaggia L, et al. Psychological processes underlying the association between childhood trauma and psychosis in daily life: an experience sampling study. Psychol Med. 2016;46(13):2799–2813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ered A, Gibson LE, Maxwell SD, Cooper S, Ellman LM. Coping as a mediator of stress and psychotic-like experiences. Eur Psychiatry. 2017;43:9–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Jaya ES, Ascone L, Lincoln TMJSb. Social adversity and psychosis: the mediating role of cognitive vulnerability. Schizophr Bull. 2016;43(3):557–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ising HK, Veling W, Loewy RL, et al. The validity of the 16-item version of the Prodromal Questionnaire (PQ-16) to screen for ultrahigh risk of developing psychosis in the general help-seeking population. Schizophr Bull. 2012;38(6):1288–1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Gawęda Ł, Prochwicz K, Krężołek M, Kłosowska J, Staszkiewicz M, Moritz S. Self-reported cognitive distortions in the psychosis continuum: a Polish 18-item version of the Davos Assessment of Cognitive Biases Scale (DACOBS-18). Schizophr Res. 2018;192:317–326. [DOI] [PubMed] [Google Scholar]
- 41. van der Gaag M, Schütz C, Ten Napel A, et al. Development of the Davos assessment of cognitive biases scale (DACOBS). Schizophr Res. 2013;144(1–3):63–71. [DOI] [PubMed] [Google Scholar]
- 42. Nijenhuis ERS, Van der Hart O, Kruger K. The psychometric characteristics of the Traumatic Experiences Checklist (TEC): first findings among psychiatric outpatients. Clin Psychol Psychother. 2002;9(3):200–210. [Google Scholar]
- 43. Smith N, Lam D, BifulcoA, Checkley S. Childhood experience of care and abuse questionnaire (CECA.Q). Soc Psychiatr Psychiatr Epidemiol. 2002;37(12):572–579. [DOI] [PubMed] [Google Scholar]
- 44. Eaton WW, Smith C, Ybarra M, Muntaner C, Tien A Center for Epidemiologic Studies Depression Scale: Review and Revision (CESD and CESD-R). In: Maruish ME, ed. The Use of Psychological Testing for Treatment Planning and Outcomes Assessment: Instruments for Adults. Lawrence Erlbaum Associates Publishers; 2004:363–377. [Google Scholar]
- 45. Haslbeck J, Waldorp LJ. mgm: Estimating time-varying mixed graphical models in high-dimensional data. arXiv preprint 2015;arXiv:151006871. [Google Scholar]
- 46. Fried EI, von Stockert S, Haslbeck JMB, Lamers F, Schoevers RA, Penninx BWJH. Using network analysis to examine links between individual depressive symptoms, inflammatory markers, and covariates. Psychological Medicine 2019:1–9. [DOI] [PubMed] [Google Scholar]
- 47. Epskamp S, Fried EI. A tutorial on regularized partial correlation networks. Psychol Methods. 2018;23(4):617–634. [DOI] [PubMed] [Google Scholar]
- 48. Foygel R, Drton M. Extended Bayesian information criteria for Gaussian graphical models. In Advances in Neural Information Processing Systems. 2010:604–612.
- 49. Murphy J, McBride O, Fried E, Shevlin MJSb. Distress, impairment and the extended psychosis phenotype: a network analysis of psychotic experiences in an US general population sample. Schizophr Bull. 2017;44(4):768–777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Haslbeck JMB, Fried EI. How predictable are symptoms in psychopathological networks? A reanalysis of 18 published datasets. Psychol Med. 2017;47(16):2767–2776. [DOI] [PubMed] [Google Scholar]
- 51. Dijkstra EW. A note on two problems in connexion with graphs. Numerische mathematik 1959;1(1):269–271. [Google Scholar]
- 52. Haslbeck JMB, Waldorp LJ. mgm: Structure estimation for time-varying mixed graphical models in high-dimensional data. arXiv preprint 2015;arXiv:151006871. [Google Scholar]
- 53. Stanton KJ, Denietolis B, Goodwin BJ, Dvir Y. Childhood trauma and psychosis: an updated review. Child Adolesc Psychiatr Clin N Am. 2020;29(1):115–129. [DOI] [PubMed] [Google Scholar]
- 54. Misiak B, Krefft M, Bielawski T, Moustafa AA, Sąsiadek MM, Frydecka D. Toward a unified theory of childhood trauma and psychosis: A comprehensive review of epidemiological, clinical, neuropsychological and biological findings. Neurosci Biobehav Rev. 2017;75:393–406. [DOI] [PubMed] [Google Scholar]
- 55. Padmanabhan JL, Shah JL, Tandon N, Keshavan MS. The “polyenviromic risk score”: aggregating environmental risk factors predicts conversion to psychosis in familial high-risk subjects. Schizophr Res. 2017;181:17–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Aas M, Etain B, Bellivier F, et al. Additive effects of childhood abuse and cannabis abuse on clinical expressions of bipolar disorders. Psychol Med. 2014;44(8):1653–1662. [DOI] [PubMed] [Google Scholar]
- 57. Bentall RP, Wickham S, Shevlin M, Varese FJSb. Do specific early-life adversities lead to specific symptoms of psychosis? A study from the 2007 the Adult Psychiatric Morbidity Survey. Schizophr Bull. 2012;38(4):734–740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Latalova K, Kamaradova D, Prasko J. Violent victimization of adult patients with severe mental illness: a systematic review. Neuropsychiatr Dis Treat. 2014;10:1925–1939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. de Vries B, van Busschbach JT, van der Stouwe ECD, et al. Prevalence rate and risk factors of victimization in adult patients with a psychotic disorder: a systematic review and meta-analysis. Schizophrenia Bulletin 2018;45(1):114–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Fisher HL, Schreier A, Zammit S, et al. Pathways between childhood victimization and psychosis-like symptoms in the ALSPAC birth cohort. Schizophr Bull. 2013;39(5):1045–1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Varese F, Smeets F, Drukker M, et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull. 2012;38(4):661–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Ered A, Ellman LM. Specificity of childhood trauma type and attenuated positive symptoms in a non-clinical sample. J Clin Med 2019;8(10):1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. van Nierop M, Lataster T, Smeets F, et al. Psychopathological mechanisms linking childhood traumatic experiences to risk of psychotic symptoms: analysis of a large, representative population-based sample. Schizophr Bull. 2014;40Suppl 2:S123–S130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Bailey T, Alvarez-Jimenez M, Garcia-Sanchez AM, Hulbert C, Barlow E, Bendall S. Childhood trauma is associated with severity of hallucinations and delusions in psychotic disorders: a systematic review and meta-analysis. Schizophr Bull. 2018;44(5):1111–1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Thompson AD, Nelson B, Yuen HP, et al. Sexual trauma increases the risk of developing psychosis in an ultra high-risk “prodromal” population. Schizophr Bull. 2014;40(3):697–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Trauelsen AM, Bendall S, Jansen JE, et al. Childhood adversity specificity and dose-response effect in non-affective first-episode psychosis. Schizophr Res. 2015;165(1):52–59. [DOI] [PubMed] [Google Scholar]
- 67. Thompson A, Papas A, Bartholomeusz C, Nelson B, Yung A. Externalized attributional bias in the ultra high risk (UHR) for psychosis population. Psychiatry Res. 2013;206(2–3):200–205. [DOI] [PubMed] [Google Scholar]
- 68. Brookwell ML, Bentall RP, Varese F. Externalizing biases and hallucinations in source-monitoring, self-monitoring and signal detection studies: a meta-analytic review. Psychol Med. 2013;43(12):2465–2475. [DOI] [PubMed] [Google Scholar]
- 69. van der Steen Y, Myin-Germeys I, van Nierop M, et al. ‘False-positive’ self-reported psychotic experiences in the general population: an investigation of outcome, predictive factors and clinical relevance. Epidemiol Psychiatr Sci. 2019;28(5):532–543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. van Os J, Reininghaus U. Psychosis as a transdiagnostic and extended phenotype in the general population. World Psychiatry. 2016;15(2):118–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Vargas T, Lam PH, Azis M, OsborneKJ, Lieberman A, Mittal VAJSb. Childhood trauma and neurocognition in adults with psychotic disorders: a systematic review and meta-analysis. Schizophr Bull. 2019;45(6):1195–1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. van Dam DS, van der Ven E, Velthorst E, Selten JP, Morgan C, de Haan L. Childhood bullying and the association with psychosis in non-clinical and clinical samples: a review and meta-analysis. Psychol Med. 2012;42(12):2463–2474. [DOI] [PubMed] [Google Scholar]
- 73. Nelson B, McGorry PD, Wichers M, Wigman JTW, Hartmann JA. Moving from static to dynamic models of the onset of mental disorder: a review. JAMA Psychiatry. 2017;74(5):528–534. [DOI] [PubMed] [Google Scholar]
- 74. Letina S, Blanken TF, Deserno MK, Borsboom D. Expanding network analysis tools in psychological networks: Minimal spanning trees, participation coefficients, and motif analysis applied to a network of 26 psychological attributes. Complexity 2019;2019:1–27. [Google Scholar]
- 75. Ackner S, Skeate A, Patterson P, Neal A. Emotional abuse and psychosis: a recent review of the literature. J Aggr Malt Trauma 2013;22(9):1032–1049. [Google Scholar]
- 76. Shevlin M, Houston JE, Dorahy MJ, Adamson G. Cumulative traumas and psychosis: an analysis of the national comorbidity survey and the British Psychiatric Morbidity Survey. Schizophr Bull. 2008;34(1):193–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.