Abstract
In March 2020, the World Health Organization (WHO) issued a set of public guidelines for Coronavirus Disease 2019 (COVID-19) prevention measures that highlighted handwashing, physical distancing, and household cleaning. These health behaviors are severely compromised in parts of the world that lack secure water supplies, particularly in low- and middle-income countries (LMICs). We used empirical data gathered in 2017–2018 from 8,297 households in 29 sites across 23 LMICs to address the potential implications of water insecurity for COVID-19 prevention and response. These data demonstrate how household water insecurity presents many pathways for limiting personal and environmental hygiene, impeding physical distancing and exacerbating existing social and health vulnerabilities that can lead to more severe COVID-19 outcomes. In the four weeks prior to survey implementation, 45.9% of households in our sample either were unable to wash their hands or reported borrowing water from others, which may undermine hygiene and physical distancing. Further, 70.9% of households experienced one or more water-related problems that potentially undermine COVID-19 control strategies or disease treatment, including insufficient water for bathing, laundering, or taking medication; drinking unsafe water; going to sleep thirsty; or having little-to-no drinking water. These findings help identify where water provision is most relevant to managing COVID-19 spread and outcomes.
Keywords: COVID-19, SARS-CoV-2, Water insecurity, WASH, Global health
1. Introduction
The global response to COVID-19 has emphasised basic infection control strategies, such as self-quarantine, handwashing and physical distancing, to “flatten the epidemiological curve” in many contexts (WHO, 2020). Globally, over four billion people experience water scarcity at least one month per year (Mekonnen and Hoekstra, 2016), a reality that may make it difficult to enact COVID-19 control measures with far-reaching consequences across continents (Staddon et al., 2020; Stoler et al., 2020). Water insecurity (and more broadly, inadequate water, sanitation, and hygiene [WASH]) already contributes to the global disease burden (Prüss-Ustün et al., 2019), and has stood out as a potentially significant multiplier of COVID-19 risk, compounding the paucity of other healthcare resources—especially test kits, personal protective equipment, oxygen and ventilators—that has plagued many nations (Hopman et al., 2020). Identifying the likely location of relevant water insecurity hot spots and clarifying the pathways by which water insecurity adds to the burdens of COVID-19 are potentially vital to ongoing prevention and treatment, especially in low- and middle-income countries (LMICs).
Persistent household water insecurity is defined as the inability to ‘access and benefit from affordable, adequate, reliable and safe water’ (Jepson et al., 2017). The links between water insecurity and COVID-19 are only beginning to emerge. One early study from Indonesia noted a positive association between household water reuse and COVID-19 transmission (Sihaloho et al., 2020). It also remains unclear whether urban slums, which tend to house many of the most vulnerable, are being sufficiently targeted by national COVID-19 testing and tracing programs (Mollah and Islam, 2020; Monteiro de Oliveira et al., 2020). Overcrowding and lack of basic services in urban slums are believed to contribute to the pandemic in some regions, such as in Latin America (Burki, 2020), while other regions thought to be particularly vulnerable, such as sub-Saharan Africa (Ekumah et al., 2020), have responded well (Makoni, 2020). For example, many African nations have avoided catastrophic COVID-19 outcomes through advance planning and public adherence to preventive measures, and because of younger population structure (Makoni, 2020). But, evolving SARS-CoV-2 variants and recurring waves of infections in late-2020 clarified that many pandemic recovery timelines would be extended.
The World Health Organization's guidance for COVID-19 prevention includes: (1) frequent handwashing; (2) physical distancing; (3) avoiding touching one's face; (4) practicing respiratory hygiene; (5) seeking medical care for cough, fever, and difficulty breathing; and (6) following advice from one's healthcare provider (WHO, 2020). In addition, the United States Centers for Disease Control and Prevention (CDC) also recommends regularly cleaning and disinfecting household surfaces (CDC, 2020). Water is thus critical for stemming the spread of COVID-19 in health facilities and households (USAID Water Leadership Council, 2020).
Many organizations have noted the inherent conflicts between these guidelines and the realities of widespread water insecurity around the world. Among many other examples, WaterAid, one of the largest non-governmental implementers of WASH solutions for the poor and marginalized, has had to change how they work in the midst of this pandemic with increasing focus on water insecurity as a key element of their response (Casey, 2020).
Household-level COVID-19 control strategies are complicated by many factors beyond limits to handwashing and cleaning (Stoler et al., 2020). Physical distancing is less feasible when it impedes access to water, as has been noted with shared sanitation facilities (Caruso and Freeman, 2020). Over a billion people collect water from sources outside of their home (WHO/UNICEF, 2017), which often requires traveling significant distances and queuing for long periods in close proximity with others. Households also frequently cope by sharing water, an underappreciated global phenomenon (Wutich et al., 2018) that typically involves shared physical spaces or physical contact with water containers. Households may also increase water storage to avoid fetching, but improperly stored water increases vulnerability to viral and bacterial illnesses. Informal water vendors who are not officially deemed essential services may cease operation out of fear of illness, resulting in significant supply disruptions to informal water markets. The management of these water-related tradeoffs and disruptions—on top of fears about COVID-19—will likely increase stress, anxiety, and interpersonal violence. All of these factors are exacerbated by the realities of resource-poor settlements that are home to close to one billion people (Corburn et al., 2020).
Our analysis highlights the challenges that many living with household water insecurity may experience in following international COVID-19 control guidelines, many of which hamper their ability to protect themselves, their households, and their communities. Our global data set also allows us to speak with more precision about the magnitude of some of these effects. We use empirical data collected in 2017–2018 from 8,297 households in 29 sites across 23 LMICs to demonstrate how household-level water insecurity not only severely limits handwashing, cleaning, and disinfection of household surfaces, but also greatly complicates physical distancing. We also illustrate how conforming to current COVID-19 control measures may, in some scenarios, lead to cascading health risks beyond COVID-19, including how water insecurity intersects with other resource constraints such as food and sanitation insecurity. Finally, we explore other contextual vulnerabilities that, more broadly, may hinder compliance with WHO guidance, and conclude with considerations for COVID-19 control in resource-limited settings.
2. Material and methods
2.1. Study data
Data were drawn from the Household Water Insecurity Experiences (HWISE) study, which primarily aimed to develop and validate a cross-culturally equivalent household water insecurity scale (S. L. Young et al., 2019b; 2019a). Cross-sectional survey data were collected between 2017 and 2018 from samples of 101–574 households in each of 29 sites across 23 countries (Fig. 1 ). Sites were selected to maximize heterogeneity by climatic region, predominant water infrastructure, and types of water problems. In most sites, households were selected using simple random sampling, with the exceptions of purposive sampling used in Singida, Tanzania; Kampala, Uganda; and Upolu, Samoa; and parallel assignment in Pune, India. Adults were considered eligible respondents if they “were knowledgeable about their household's water situation” (S. L. Young et al., 2019b). These survey data provided a more detailed view of household water insecurity than other common household surveys such as Demographic and Health Surveys or Multiple Indicator Cluster Surveys.
Fig. 1.
The 29 HWISE study sites showing the percent of households in each site that experienced one or more water problems in the prior four weeks that potentially undermine COVID-19 control strategies or disease treatment.
Enumerators used paper and tablet-based surveys to collect data on sociodemographics and experiences with water availability, accessibility, reliability, and use, which are core components of household water insecurity (Jepson et al., 2017). The survey items elicited the frequency of 34 household experiences related to water in the four weeks prior to survey implementation, and responses were categorized as follows: never (0 times), rarely (1–2 times), sometimes (3–10 times), often (11–20 times), or always (more than 20 times). This paper presents data from the 34-question survey module to highlight pathways through which different dimensions of water insecurity complicate COVID-19 prevention and control. Data collection occurred in two waves between 2017 and 2018. The total sample size available for this analysis was 8,297 households across 29 sites.
All participants provided verbal or written informed consent in the respective local language. Study activities were reviewed and approved by all relevant ethical review boards (S. L. Young et al., 2019b).
2.2. Statistical analysis
We assessed the frequency of affirmation for each survey item related to handwashing, ability to enact physical distancing, and cleaning and disinfecting household surfaces to demonstrate heterogeneity across sites. We used a descriptive, rather than inferential, approach due to the current lack of reliable COVID-19 prevention or case data in the HWISE study sites that would otherwise help us extrapolate risk to other areas. Our objective was to present the breadth of water insecurity experiences that have implications for COVID-19 prevention and control.
In our analysis of socioeconomic status, we categorized HWISE study participants' responses to the MacArthur Scale of Subjective Social Status, a self-reported measure of one's perceived social standing in the community (Adler et al., 2007), into high, medium, and low tertiles, and examined their relationship with select water insecurity items using chi-square tests and two-sample tests of proportions. All analyses were conducted using Stata 14.0 (StataCorp, College Station, TX, USA).
3. Results
Frequency statistics for responses to individual water insecurity items among the 8,297 study households are presented in Fig. 2, Fig. 3, Fig. 4, Fig. 5, Fig. 6, Fig. 7, Fig. 8 . We report these results in sub-groups as they pertain to hygiene, physical distancing, and additional contextual vulnerabilities. Overall, 45.9% of households reported being unable to wash their hands or reported borrowing water in the four weeks prior to completing the survey, which confounds compliance with WHO's first two guidelines for COVID-19 control (frequent handwashing and physical distancing). We also considered households' ability to engage in a broader range of water-related activities that may serve as proximal and distal determinants to COVID-19 outcomes: drinking unsafe water, going to sleep thirsty, having no water or less water for drinking, and lacking water to take medications, bathe, launder clothes, or prepare foods, in addition to handwashing or borrowing water. We found that 70.9% of households experienced at least one of these water-related problems that can undermine COVID-19 control strategies or intensify disease progression.
Fig. 2.
Distribution by study site of percent of households that experienced interruptions to hygiene behavior in the prior four weeks due to problems with water (with percent across all sites in bold).
Fig. 3.
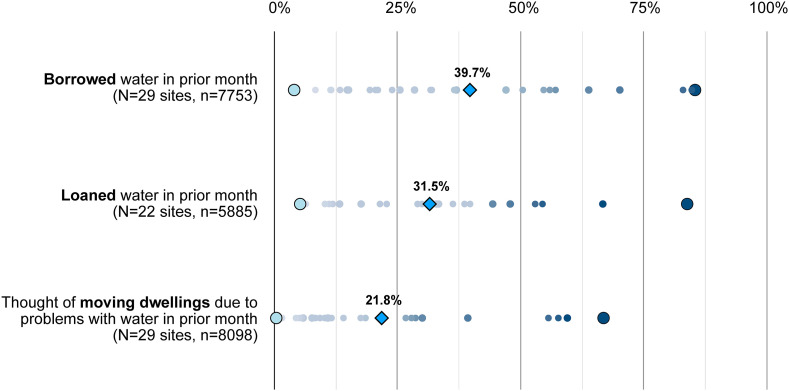
Distribution by study site of percent of households that borrowed or loaned water in the prior four weeks, as well as those who considered moving due to problems with water (with percent across all sites in bold).
Fig. 4.
Distribution by study site of round trip time to primary water source and trips made to water source per week (with percent across all sites in bold).
Fig. 5.
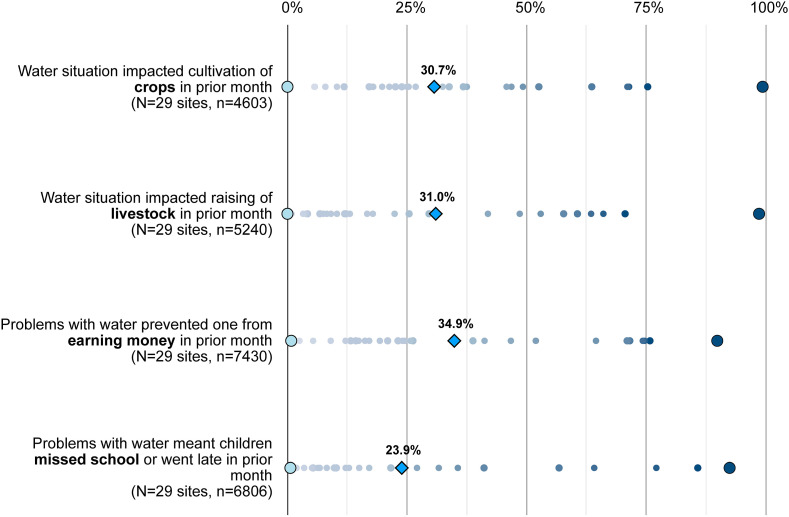
Distribution by study site of percent of households that experienced livelihood or educational opportunity costs in the prior four weeks due to problems with water (with percent across all sites in bold).
Fig. 6.
Percent of households across all study sites that worried about problems with water or experienced interruptions to hygiene in the prior four weeks by tertile of perceived socioeconomic status relative to others in their community.
Fig. 7.
Distribution by study site of percent of households that experienced water problems in the prior four weeks that could undermine physical or nutritional health (with percent across all sites in bold).
Fig. 8.
Distribution by study site of percent of households that experienced perceived stress or interpersonal conflict in the prior four weeks due to problems with water (with percent across all sites in bold).
3.1. Hygiene
3.1.1. Handwashing and bathing
Frequent handwashing with soap and water is critical for reducing the spread of communicable diseases, including COVID-19. Soap destroys the lipid bilayer that envelopes SARS-CoV-2 and water washes away the exposed, inactivated virus (Staddon et al., 2020). Yet nearly one in four households (23.0%) in our study reported that they were “unable to wash their hands in the prior four weeks after dirty activities” (e.g., defecating, changing diapers) due to problems with water (Fig. 2). Of households with children, 23.6% reported being unable to wash their young children's hands and faces because of problems with water. Over a third (33.7%) of households reported being unable to wash their bodies, varying widely from 4.1% of sampled households in Honda, Colombia, to 94.8% of households in Punjab, Pakistan.
Sometimes washing was limited or impossible because water was not available in sufficient quantities. For example, when water was limited due to shutoffs, some households reported that they prioritized water for drinking and cooking over hygiene. Other households reported that there was water available, but that the quality was too low for handwashing or bathing. Although water does not need to meet drinking-water standards for hygienic purposes (WHO/UNICEF, 2020a), handwashing with severely contaminated water can be unacceptable, irritate the skin and create open sores, or expose individuals to a variety of water-washed diseases (Bartram and Hunter, 2015).
The frequency with which households are unable to wash hands due to problems with water is likely to increase during the pandemic. As hand hygiene messaging spreads, individuals may wish to increase handwashing but may be unable to do so due to competing water demands. For instance, water may become more difficult to access because of physical distancing recommendations or the need to divert greater quantities of water to other household tasks that have increased in frequency due to sheltering in place, such as cooking, cleaning, or caring for the ill. Women and girls typically experience water inadequacy even more acutely (Maxfield, 2020). This can be due to unequal access within households, or specific needs related to menstrual or sexual hygiene. While there is currently no evidence that COVID-19 affects the menstrual cycle or can be spread by blood or semen, the concomitant stress and anxiety are nonetheless important to consider (UNICEF, 2020).
3.1.2. Household cleaning and disinfection
SARS-CoV-2, the virus that causes COVID-19, can travel in droplets and land on common household surfaces, where the virus can remain viable for hours to days, depending on the surface material (e.g., the virus survives longer on plastic and wood compared to copper surfaces) (van Doremalen et al., 2020). Regular disinfection of household surfaces is therefore recommended to reduce the risk of transmission (CDC, 2020). Best practices include laundering soft, porous surfaces (e.g., clothing) with hot water and non-porous surfaces (e.g., tables) with soap and water or bleach diluted with water. These preventative practices are difficult or impossible when a household experiences water problems.
Across all sites, 45.9% of households were unable to wash clothes due to problems with water in the prior four weeks (Fig. 2). Further, 59.1% of households worried that they would not have enough water for all of their needs and 27.9% reported they had no useable water, including for chores such as cleaning surfaces. As the price and availability of water fluctuates throughout the pandemic, households may reduce water-intensive chores and reserve limited water for higher priority activities, such as direct consumption. Indeed, in a previous study in western Kenya, respondents prioritized water for drinking, taking medications, and cooking over other activities such as washing clothes (Collins et al., 2019). The 2018 drought in Cape Town, South Africa, also showed how households can severely reduce water use during an emergency—change that was largely driven by policy discourse, social norms, and perceived threats to one's lifestyle (Booysen et al., 2019; Enqvist and Ziervogel, 2019).
3.2. Physical distancing
3.2.1. Water sharing
If people cannot readily access community water supplies when physical distancing, water sharing between neighboring households might increase as a coping strategy (Wutich et al., 2018); this common adaptation has been observed in many LMICs (Rosinger et al., 2020). Increased sharing potentially brings people into greater direct physical contact with each other. It can also bring people into greater contact with shared objects like water jugs that may then increase transmission risks of infectious disease (Stoler et al., 2019).
Frequency of borrowing water in the prior month ranged between 4.0 and 85.4% of households across all 29 sites, and lending ranged from 5.2 to 83.8% across the 22 sites with lending data (Fig. 3). Of the 3,078 households that borrowed water, 54.2% also reported loaning water. Of the households that loaned water, 66.9% also reported borrowing during the prior four weeks. Taken together, this suggests substantial transactional movement of water (and the containers used to haul it) both in and out of households.
The types of water containers used and the method of exchange may be important risk factors of COVID-19 transmission, given that SARS-CoV-2 survival varies across surfaces. While the HWISE study did not collect data on the types of water containers used during water exchanges, plastic jerrycans are a common water storage container in many water-insecure communities. Jerrycans may pass from one person's hands to another during the filling process, thus increasing transmission risk as the virus can survive on plastic for up to 72 h (van Doremalen et al., 2020). Both individuals involved in the water exchange should ideally wash their hands prior to exchanging water, and the surface of the container should be sanitized afterward. This assumes adequate water for handwashing (see Section 3.1.1), although households often participate in water sharing specifically because of a lack of access to water—including for handwashing.
3.2.2. Water fetching
Water fetching often involves long queues at water kiosks and borehole pumps (Geere and Cortobius, 2017). Spending extended time in close proximity with others is inconsistent with physical distancing guidelines. In the HWISE sample, we obtained data on the frequency of trips to collect water per day. We also collected data on the amount of time spent obtaining water per day (which includes queue time). We found that 18.5% of households had a roundtrip water collection time equal to or over 1 h (Fig. 4). Also, 9.9% of households made more than 21 trips to their water source each week and 23.4% reported spending at least 7 h/week fetching water. It is also well documented that there are frequently gender differences with respect to water fetching (Geere and Cortobius, 2017), potentially leading to differential disease exposure.
When households are unable to fetch water, or if fetching presents too large of an opportunity cost in terms of time spent, individuals may be forced to resort to higher-priced or lower-quality water from tankers, carts, and other forms of water vending, or use nearby surface water (Smiley and Stoler, 2020). For lower-income households, higher water costs may present tradeoffs for other household priorities, particularly health care for ill family members or COVID-19 preventive gear such as masks, gloves, disinfectant, soap, detergent and hand sanitizer.
Physical distancing guidelines would also seemingly discourage water fetching in groups, which eliminates a way of maintaining social capital and an important safety buffer for women and children, who frequently suffer harassment, assault, and accidents while fetching water (Collins et al., 2019; Venkataramanan et al., 2020). This reality can shape water-related decision making and cause women to take risks, such as using alternative inferior water sources or navigating physically dangerous terrain to obtain water elsewhere (Smiley and Stoler, 2020).
3.2.3. Mobility
Because human mobility facilitated rapid transmission of COVID-19 from the start of the outbreak (Kraemer et al., 2020), many nations and municipalities have enforced self-quarantine in order to reduce spread and flatten the epidemiological curve. Some lockdowns have been vigorously enforced by police and even military forces (Human Rights Watch, 2020). In many regions, lockdown restrictions have had the unintended consequence of triggering mobility, as many struggled to return home in the absence of work opportunities and public transport.
The HWISE study asked how frequently households had considered moving their dwelling due to their water situation in the prior four weeks. We found that for most sites, at least some households had considered moving in the past four weeks, with an average of 21.8% across all sites (Fig. 3). In San Borja, Bolivia, 66.8% of households considered moving due to problems with water.
When water insecurity drives relocation, the introduction of COVID-19 into new locations is possible. Further, households often seek out more desirable water sources that can be chained to their commute and may therefore increase the risk of transmission to new neighborhoods if this source is outside their daily activity space (Smiley and Stoler, 2020). Such dynamics may be further complicated if these destinations are ill-equipped to support new arrivals safely. Common forms of circular migration, such as commuting or agricultural migrant labor travel patterns, also present opportunities to spread COVID-19 to origin communities. If movement induced by water insecurity is migratory and COVID-19 is introduced, there is even greater potential for hostility in host destinations.
3.3. Contextual vulnerabilities
Many underlying biocultural and socio-economic vulnerabilities render water-insecure households even more susceptible to COVID-19 infection and at higher risk of severe disease. Context matters and can magnify vulnerabilities in communities with high population density and poverty, particularly places where self-isolation is impractical, such as informal settlements (Corburn et al., 2020) and refugee camps (Raju and Ayeb-Karlsson, 2020). For instance, in Beirut, Lebanon, we found that households inside urban refugee camps had higher water insecurity scores than nearby households outside the camps (mean ± sd, 10.2 ± 6.9 vs. 5.5 ± 6.5, P < 0.0001).
Water insecurity is shaped by water systems and the use and availability of different water sources. Water insecurity also intersects with livelihoods, socioeconomic status, and gender, as well as the sociomedical realities of food insecurity, thirst and dehydration, and mental health. We summarize the effects of each of these contextual factors in turn.
3.3.1. Water systems
The HWISE study evaluated the myriad configurations of how households collect, convey, and access water for domestic needs. We used these data to examine the variation in primary drinking water sources—one of the key metrics of the WHO Joint Monitoring Programme for Water Supply, Sanitation, and Hygiene—and assess how piped, collected, or delivered water may contribute to COVID-19 vulnerability.
Almost a quarter of surveyed households (24.3%) accessed water through a community water system (e.g., on-premises piped water). While the HWISE study did not collect data on shared connections across or among homesteads, overall these households are expected to face fewer risks of COVID-19 exposure unless they are selling water to others. Other important primary drinking water sources included dug wells (protected or unprotected) and boreholes, used by 17.9% of households. Only 1.8% of households engaged in rainwater collection as a primary drinking water source, though many sites were interviewed in the dry season. Taken together, these water sources—community water systems, wells, and rainwater collection, used by 44% of households—provide mechanisms of obtaining needed water for basic needs and hygiene that are generally compatible with physical distancing. Although community water systems depend on a labor force that may or may not be able to maintain systems during the height of quarantine, public systems and their workforce are still generally supported in ways that limit water service intermittency.
On the other hand, over half of our study households accessed water in ways that potentially place people at an increased risk of COVID-19 transmission. Water provisioning is a profoundly social activity that requires considerable physical labor and social relations to fetch or collect water (Geere and Cortobius, 2017). Water fetching, as noted earlier, frequently involves queuing in close proximity and spending significant time waiting for one's turn or for water to be available. In the HWISE study, 27.4% of households reported that their primary drinking water source was a spring (3.5%), surface water (6.6%), or public standpipe (17.4%). COVID-19 exposure may occur while collecting or fetching water at any one of these sources through person-to-person contact. At springs or surface water sources, increased risk may result from proximity to others when there are limited safe fetching locations. At public standpipes, increased risk may occur with contact of common water points that are not disinfected.
The HWISE study also reported that almost 11% of surveyed households depended on drinking water delivery services. Over 7% of households reported that their primary drinking water source was delivered by tanker truck, and another 3.9% received water from a small-scale vendor. Similarly, over 15% of households depended on bottled or sachet water. Although not all modes of water delivery necessarily come directly to households, nearly all involve person-to-person conveyance and payments. Water delivery services have varying practices of contact with water containers that do not guarantee disinfection. During a public health emergency, dependence on informal water vendors carries additional risk of service disruption, as the informal workforce may cease operations in the name of physical distancing or due to other pandemic-driven government mandates.
3.3.2. Livelihoods
Livelihood impacts can be divided into two basic categories: non-monetary and monetary (Scoones, 2009). Non-monetary impacts involve aspects of the domestic economy that are not directly part of the cash economy, such as household tasks linked to the social reproduction of labour including child-rearing, domestic maintenance, and subsistence food production. Monetary economic impacts are those that are directly linked to the earning or spending of cash income, such as day labouring, trading or commodity agriculture. In practice, households are likely to be involved in a complex range of monetary and non-monetary economic activities, all of which could be impacted by the COVID-19 pandemic. We first present data about non-monetary livelihood impacts before turning to impacts on cash dimensions of livelihood strategies.
The HWISE study revealed that, prior to COVID-19, a significant number of households borrowed (39.7%) and loaned (31.5%) water as part of their regular livelihoods (Fig. 3). The variability in these indicators across sites was high, with respondents in sites like Arua, Uganda, suggesting that they almost never borrow/loan water, while those in other sites such as Cartagena, Colombia, very frequently do. Depending on specific lockdown policies, such non-monetised exchanges of water could be significantly affected. In Uganda, for example, the military was used to police the nationwide lockdown, and research partners reported feeling like “prisoners” in their homes, often unable to go out even to secure basic necessities (Human Rights Watch, 2020).
More indirect consequences could ensue if any of the borrowed/loaned water is used for other sorts of productive activities, such as crop or livestock raising. In the HWISE study, 30.7% and 31.0% of households reported a lack of sufficient water for raising crops or livestock, respectively (Fig. 5). Moreover, 34.9% of respondents reported that problems with water prevented them from earning money, and 23.9% reported that water problems prevented children from attending school. It is plausible that suppression of the loaning/borrowing of water between vulnerable households could have damaging effects on income-generating activities (Wutich et al., 2018).
With respect to the monetary economy, there was considerable variability among the 29 sites; in Kisumu, Kenya, 74.7% of households experienced water problems that impacted their ability to earn money whereas only 0.8% of households in Ceará, Brazil, reported this. Many who reported significant impact were day laborers, and the escalation of water-related obstacles to income generation may produce catastrophic effects on households' ability to earn needed cash. As we have seen in Peru, India, and elsewhere, lockdown policies triggered an exodus of poorer people from the cities, presumably since returning to home towns and villages offered more immediate access to non-commodity subsistence production (Staddon et al., 2020). Even in smaller towns, as earning potential decreased, households decamped to even smaller villages and rural areas in order to be closer to their agricultural fields (World Bank, 2020). The sudden severe curtailment of informal markets has disproportionately hindered poorer households’ ability to satisfy even basic needs.
Across all sites, there was evidence that these impacts are experienced differently across socio-demographic groups. For example, in southwestern Uganda, minority Batwa communities reported more restrictive lockdown policing than in majority Bufimbira communities (Staddon et al., 2020). Indeed, as with many communicable disease outbreaks, socioeconomic status (SES) and gender disparities have considerable implications for COVID-19 risk and outcomes.
3.3.3. Socioeconomic status
The uneven distribution of resources, power, and voice by historical and current social and economic systems affects household water security (Jepson et al., 2017). The U.S. burden of COVID-19 has disproportionately fallen upon those of lower SES and communities of colour, intersecting with existing structural vulnerabilities, health comorbidities, and differential capacities for everyday mitigation efforts (Dorn et al., 2020) that has led to utility shutoffs and evictions (Meehan et al., 2020). These patterns are likely to be further magnified in LMICs (Hopman et al., 2020). We analysed the relationship between household SES tertile (i.e., relative low = 1, medium = 2, and high = 3) and the affirmation of several water insecurity experiences related to interruptions in household hygiene: (1) being worried that there would not be enough water for their needs, (2) unable to wash clothes, (3) unable to bathe due to water-related problems, (4) unable to wash their hands, and (5) unable to wash their children's hands. A higher percentage of low- and medium-SES households affirmed these water insecurity experiences than high-SES households (Fig. 6).
First, SES tertile was negatively associated with whether a household affirmed being worried that there would not be sufficient water for their needs (χ2: 93.20, P < 0.01). Using a two-sample test of proportions (adjusted for multiple comparisons), we found that 54.2% of high-SES households affirmed water worry, a lower percentage than low-SES (64.5%; P < 0.01) and middle-SES (65.6%; P < 0.01) households.
Second, SES tertile was negatively associated with whether a household affirmed the inability to wash clothes (χ2: 72.48, P < 0.01) and bathe (χ2: 90.69, P < 0.01) in the prior four weeks. High-SES households reported being unable to wash their clothes (40.5%) and body (28.4%), at lower frequencies than low-SES (51.2% and 40.5%; both P < 0.01) and medium-SES (50.1% and 36.8%; both P < 0.01) households.
Third, SES tertile was negatively associated with whether a household affirmed the inability to wash their hands (χ2: 39.90, P < 0.01) and wash the hands of their children (χ2: 56.14, P < 0.01). High-SES households affirmed being unable to wash their hands (19.7%) and children's hands (19.8%) at lower frequencies than low-SES (26.8% and 28.9%; both P < 0.01) and medium-SES (24.6% and 25.4%; both P < 0.01) households.
Overall, a higher percentage of medium- and low-SES households affirmed water insecurity experiences compared with high-SES households, but the overall percentages across tertiles were high, ranging from approximately 20-66%. This underscores the need for efforts at all scales to improve household water security across multiple dimensions of human well-being, particularly minimizing risks associated with COVID-19 transmission, morbidity, and mortality. Such efforts will require improved water service provision as well as efforts to reduce potential socioeconomic barriers to sufficient water access through government subsidies or other policies.
The HWISE study also recorded the sex of the household head, and we found that female-headed low-SES households most commonly affirmed water insecurity experiences related to aspects where higher quantities of water are required, such as not being able to bathe (43.3%) or wash their clothes (53.6%) in the prior four weeks. COVID-19 clearly presents specific risks for women, including challenges for menstrual hygiene (UNICEF, 2020), and serious economic impacts given potential for lower earnings and savings, higher exposure to COVID-19 through occupational work (women comprise 70% of the global healthcare workforce), additional unpaid work such as caring for sick children or elders, and gender-based violence resulting from policy measures designed to reduce the transmission of COVID-19 (United Nations, 2020).
3.3.4. Food insecurity
Household food insecurity often co-occurs with water insecurity. In the HWISE study, the overall correlation between food and water insecurity scores was 0.37 (P < 0.001), with correlations among study sites ranging from −0.02 to 0.74. Brewis et al. (2020) also tested multiple sub-dimensions of water insecurity (need, quality, water worry) using the same HWISE dataset, and found all to be associated with greater household food insecurity. In site-specific regressions, greater water need was positively associated with food insecurity for 24 of 27 sites. The only exceptions were Acatenango, Guatemala (the site with the smallest sample), Punjab, Pakistan (the most water-insecure site), and Pune, India (the most water-secure and also one of the most food-secure sites) (Brewis et al., 2020).
Theoretically, there is reason to expect that water insecurity is a driver of food insecurity rather than the other way around, particularly because water is needed to grow crops, feed livestock, and prepare and cook adequate safe foods but not the converse (Brewis et al., 2020; Wutich and Brewis, 2014). For example, water is needed to irrigate household gardens and maintain animals, prepare food safely, and many of the most readily available cereals, tubers, and grains (e.g., rice, cassava) specifically require treatment with water to make them digestible and safe. Note that many sites reported high levels of “having to change foods being prepared” (Fig. 7) and “water situation impacted livestock” and “water situation impacted crops” (Fig. 5).
The observation of a strong and consistent association between food and water insecurity across many of the global sites, with water insecurity as a potential driver, has implications for COVID-19 in several dimensions based on elevation of risk of food insecurity. There are many mechanisms by which household food insecurity might potentially impact COVID-19 risk to individuals, households, and communities, and we would then expect water insecurity to elevate these. First, it is well-established that acute and chronic undernutrition creates additional risks for infection (Calder and Jackson, 2000). Undernutrition undermines barrier function, allowing easier entry of infectious agents, and it also weakens immune function, making it harder to recover from infections. Also, water security appears to be important for mothers' capacity and decisions about how they (breast)feed their children (Collins et al., 2019; Schuster et al., 2020), an additional way in which water may be hypothesized to affect children's immune function. Third, under low-resource conditions, money, assets, or social capital deployed to deal with water (or food) insecurities can undermine household budgets or other means to cope with health challenges, including healthcare and other spending relevant to the prevention and treatment of infectious disease (Brewis et al., 2020).
3.3.5. Thirst and dehydration
One of the most common recommendations that patients with respiratory infections receive from doctors, is to “drink plenty of fluids” (Guppy et al., 2004). This recommendation is given to reduce risk of dehydration through insensible water loss and account for potential lower water intake, as well as reduce mucus thickness (Guppy et al., 2004). Poor water accessibility and reliability may make it difficult to meet this recommendation. Lacking access to water while in a mildly dehydrated condition increases anxiety and can change decision-making practices (H. A. Young et al., 2019), which may increase transmission risk of COVID-19.
Across all HWISE study sites, 17.6% of households reported going to sleep thirsty at least once in the last four weeks. At every site, some households reported water problems so severe that they reported at least one night of going to sleep thirsty, ranging from 0.4% in Ceara, Brazil, to 67.9% in Kahemba, DRC (Fig. 7). In addition, 27.9% of all households had no useable or drinking water at least once in the prior month; 40.5% drank water that looked, tasted, or smelled bad; and 40.8% drank water thought to be unsafe. We would not expect any of these experiences to be associated with optimum hydration.
Our results indicate that a large proportion of households would not be able to meet the treatment recommendation of “drink plenty of fluids” if they were to contract COVID-19. While dehydration was not explicitly measured in the HWISE study, from a physiological perspective, thirst can be indicative of dehydration (Weinberg et al., 1995). It is likely that some proportion of the individuals in these households are also dehydrated, which can negatively affect cognitive performance and lead to confusion, particularly among older adults, as well as lead to higher risk of kidney stones (Popkin et al., 2010; Weinberg et al., 1995). Therefore, prevention and at-home treatment of COVID-19 may be more challenging under these conditions.
3.3.6. Mental health
Water insecurity is strongly linked to mental ill-health. Early exploratory research found high rates of worry, anger, shame, and conflict among people experiencing water insecurity (Sultana, 2011; Wutich and Ragsdale, 2008). Recent research finds that water insecurity is associated with symptoms of anxiety and depression (Mushavi et al., 2020). Seven key mechanisms appear to produce water-related mental ill-health: (1) worry about illness and health problems, (2) conflict in households and communities, (3) status loss or social failure, (4) loss of connection to meaningful places, (5) reduced autonomy or opportunities, (6) poverty, deprivation and uncertainty, and (7) unjust or unfair treatment (Wutich et al., 2020). It is likely that COVID-19 will intensify most, if not all, of these pathways. We highlight three likely dynamics: worry about illness and health problems, conflict in households and communities, and status loss or social failure.
Water insecurity puts people at higher risk of contracting COVID-19, and thus is distressing. Past research shows that people feel significant worry over the risks of drinking contaminated water, the physical risks of water fetching, and thirst and hunger borne of water insecurity (Wutich et al., 2020). Our data indicate that 59.1% of households reported that at least one member experienced worry that they would not have enough water in the last four weeks (Fig. 8). This is likely to intensify as people worry about contracting COVID-19 at water-fetching points, contamination of stored water, and the necessity of drinking less-safe water if cash becomes short and water-points become inaccessible.
Water insecurity precipitates significant conflicts both within households and across communities. Within households, conflicts tend to center on financial worries and water shortages, with women often bearing the brunt of blame and experiencing higher risk of intimate partner violence (Choudhary et al., 2020). Within communities, water insecurity produces conflict as people argue over access to water sources (Sultana, 2011). In the HWISE study, 28.0% of households reported intra-household difficulties over water, and 21.5% reported extra-household difficulties over water (Fig. 8). As the stakes of water insecurity increase during a COVID-19 outbreak, we would predict such conflict would also increase—for example, if people are unable to meet physical distancing expectations while queuing for water.
Water insecurity can create status loss, especially for households that are impoverished, unable to maintain hygiene norms, or are perceived as too dependent on others (Wutich and Brewis, 2014). This can be particularly true for households that lean more heavily on water sharing arrangements when water becomes scarce (Wutich et al., 2018). Shame and anger are common emotional responses to the threat of status loss (Sznycer et al., 2016). In our sample, 47.0% of households reported anger/upset and 34.4% reported shame over water (Fig. 8). As communities experience economic and social disruptions related to COVID-19, people will likely find it increasingly difficult to conform to social norms and expectations (such as hygiene norms) and may experience anger and shame over status loss as a result.
3.3.7. Household sanitation
Inadequate sanitation and water insecurity are mutually reinforcing, as the inability to effectively separate human waste more readily introduces pathogens into the domestic environment. Recent evidence indicates gut involvement of SARS-CoV-2, with prolonged viral shedding found in both symptomatic and non-symptomatic patients (Wu et al., 2020). Although the HWISE study did not ask about water use for sanitation, the gut involvement of SARS-CoV-2 poses several implications for WASH-insecure households.
Gastrointestinal symptoms require increased attention to fecal management when sick individuals increase use of bathrooms, latrines, or chamber pots. Evidence is also emerging for fecal-oral transmission of the virus (Yeo et al., 2020), with implications for WASH-insecure areas. Even if fecal-oral transmission proves uncommon, sanitation security nonetheless is critical. Shared sanitation facilities, such as latrines, are often small enclosed spaces that experience high usage and thus present additional COVID-19 transmission risk (Caruso and Freeman, 2020). We may see increases in droplet and fomite transmission of COVID-19 if facilities are inadequately cleaned. Effective management of diarrhea requires sufficient quantities of safe water for cleaning as well as for hydration, hand hygiene, and caregiving.
Second, inadequate sanitation is a key driver of environmentally mediated transmission of enteric infections. As COVID-19 spreads to countries with high burdens of enteric infections, enteric infections may emerge as important comorbidities that shape epidemic trajectories given the noted effects of infection with SARS-CoV-2 in the gastrointestinal tract.
4. Conclusion
Water is a critical component of human well-being and development (Jepson et al., 2017), and household water insecurity presents an array of complications for COVID-19 prevention and control. Although the pandemic is exacerbating socio-medical inequalities in high-income nations (Dorn et al., 2020), water insecurity is experienced everywhere, and its effects are especially salient in LMICs. Our analysis of empirical data from 8,297 households across 29 LMIC sites illustrate how the WHO guidelines for COVID-19 control are difficult to meet given the everyday realities faced by billions of people. For example, 71% of households had recently experienced a water-related problem that has the potential to undermine COVID-19 control strategies or intensify disease progression, and 46% faced specific challenges with handwashing and physical distancing, both core elements of WHO's guidelines for COVID-19 prevention and control. In light of new, more infectious strains of COVID-19 like B.1.1.7 (Galloway et al., 2021), prevention strategies such as masking and physical distancing are even more important given initial delays to vaccine deployment. Although our study sample is not representative of all LMICs or communities in the countries sampled, the water problems documented here clearly exemplify the range of substantial issues endured by water-insecure households across diverse rural and urban contexts. While water issues alone cannot forecast COVID-19 intensity, these data suggest some practical means to identify where particular and layered risk for COVID-19 are located within LMICs: those communities with particularly high levels of water insecurity.
Our analysis has limitations. The data do not include information beyond households, and non-household water sources could be an important and effective means for households to obtain water. Nearly two billion people depend on healthcare facilities without basic water services, which increases COVID-19 risks for patients and health care workers (WHO/UNICEF, 2020b). Additionally, over 30% of schools globally lack access to an onsite water point and 36% have no hygiene facilities. These institutions are more likely to be found in communities with poor household water security, multiplying the risks to people living there, especially during the pandemic.
This pandemic necessitated legislation of economic stimulus and relief packages in high- and middle-income nations. Although the cost of achieving Sustainable Development Goal (SDG) 6 would require a significant increase over our current global investment, the cost of achieving universal basic WASH services has been estimated at US$28.4 billion per year from 2015 to 2030 (i.e., US$426 billion, non-discounted), or 0.10% of global GDP (Hutton and Varughese, 2016). In March and April 2020 alone, the United States committed US$3 trillion in a series of four economic relief packages, and the European Union committed €540 billion, with significant additional relief legislation pending on both continents. Other countries have followed suit, such as Japan's US$992 billion stimulus package, China's US$500 billion fiscal stimulus, and India's US$260 billion COVID-19 relief package. Compared to what the world will ultimately end up spending on emergency economic measures, the cost of universal basic WASH looks like a bargain, something we have known for years (Hutton et al., 2007). We emphasize that while these issues are most acute in situations such as the current pandemic, basic WASH services have implications for many other key considerations ranging from mitigating the global burden of disease to improving education outcomes and improving gender equity. WASH service coverage has long been a pressing global concern; COVID-19 has made its importance more visible and urgent.
In the short term, the COVID-19 crisis should trigger increased investments and attention to WASH issues by LMICs and the development community as seen after the 2014-16 Ebola outbreak in West Africa (Cooper, 2020a). Eleven African nations announced different forms of free water for the urban poor and other groups, for example paying users bills in some areas in Ghana (Amankwaa and Ampratwum, 2020; Smiley et al., 2020), providing water for vulnerable communities and informal settlements in Kenya, and the World Bank supporting 20 new water points for poor communities in Democratic Republic of the Congo supplied by utility-owned water tankers (Cooper, 2020b). Government stimulus programs may also need to directly address public-private partnerships (PPP) that have historically played a crucial role in WASH service provision. These partnerships may have the physical and social infrastructure to immediately improve water access for many vulnerable communities. But the pandemic has created financial stress for PPPs across industries globally and threatens widespread project failure from logistical disruption and new budget constraints, including the loss of revenue from regional lockdowns (Baxter and Casady, 2020; Casady and Baxter, 2020). PPP engagement requires caution, as goals and accountability are not always well-aligned between partners, and profit imperatives can clash with equity and other priorities.
As policymakers and program implementers scale-up the immediate distribution of emergency WASH supplies, we encourage deeper consideration of how these activities can be transitioned into targeted, sustainable, long-term WASH investments. High-resolution geospatial mapping of water and sanitation access, like those produced by the Local Burden of Disease WaSH Collaborators in 2020, can provide sub-national guidance on priority regions (Deshpande et al., 2020). Although solutions should be tailored to local needs and constraints, it is clear that most communities will benefit from improvements in both water infrastructure and water governance, and also the way water managers distribute water and remain responsive to the needs of diverse users. Ultimately, such strategies have the potential to greatly improve the overall health of communities and increase their resilience to future shocks, including another pandemic. Housing and utility policies may help deter COVID-19 transmission as well: in the US and Iran, moratoria on eviction and electricity and water shutoffs have helped contain disease spread, although the economic impacts on landlords and utilities remain unclear (Jowers et al., 2020; Seddighi et al., 2020).
Strengthening household water security is critical for preventing and mitigating the effects of future pandemics in underserved communities around the world (Cooper, 2020b). The world was already off track to achieve SDG 6 before the COVID-19 pandemic, and innovations in water economics, engineering, and management will be critical to accelerate the pace of progress (Sadoff et al., 2020). In the meantime, adequate and affordable WASH services can mitigate the potentially compounding effects of COVID-19 and future pandemics with the traditional burdens of water insecurity, especially in the most historically marginalized households and communities.
HWISE RCN Co-Authors
Ellis Adams, University of Notre Dame, South Bend, IN, USA. Farooq Ahmed, Quaid-e-Azam University, Islamabad, Pakistan. Mallika Alexander, Johns Hopkins University-Byramjee Jeejeebhoy Medical College Clinical Trials Unit, Pune, India. Gershim Asiki, African Population and Health Research Center, Nairobi, Kenya. Mobolanle Balogun, College of Medicine of the University of Lagos, Lagos, Nigeria. Michael J. Boivin, Michigan State University, East Lansing, MI, USA. Genny Carrillo, Texas A&M University, College Station, TX, USA. Kelly Chapman, University of Florida, Gainesville, FL, USA. Stroma Cole, University of Westminster, London, UK. Shalean M. Collins, Tulane University School of Public Health and Tropical Medicine, New Orleans, LA, USA. Hassan Eini-Zinab, Shahid Beheshti University of Medical Sciences, Tehran, Iran. Jorge Escobar-Vargas, Pontificia Universidad Javeriana, Bogotá, Colombia. Hala Ghattas, American University of Beirut, Beirut, Lebanon. Monet Ghorbani, Arizona State University, Tempe, AZ, USA. Ashley Hagaman, Yale University, New Haven, CT, USA. Nicola Hawley, Yale University, New Haven, CT, USA. Zeina Jamaluddine, American University of Beirut, Beirut, Lebanon. Divya Krishnakumar, Anode Governance Lab, Bengaluru, India. Kenneth Maes, Oregon State University, Corvallis, OR, USA. Jyoti Mathad, Weill Cornell Medicine, New York, NY, USA. Jonathan Maupin, Arizona State University, Tempe, AZ, USA. Patrick Mbullo Owuor, Northwestern University, Evanston, IL, USA. Hugo Melgar-Quiñonez, McGill University, Ste-Anne-de-Bellevue, Quebec, Canada. Milton Marin Morales, Universidad Autónoma del Beni José Ballivián, Trinidad, Bolivia. Javier Moran, Autonomous University of Coahuila, Coahuila, Mexico. Nasrin Omidvar, Shahid Beheshti University of Medical Sciences, Tehran, Iran. Sabrina Rasheed, International Centre for Diarrhoeal Disease Research Bangladesh, Dhaka, Bangladesh. Luisa Samayoa-Figueroa, McGill University, Ste-Anne-de-Bellevue, Quebec, Canada. Ernesto C. Sánchez-Rodriguez, Hospital Agustin O’Horan, Mérida, Yucatan, Mexico. Marianne V. Santoso, Northwestern University, Evanston, IL, USA. Roseanne C. Schuster, Arizona State University, Tempe, AZ, USA. Mahdieh Sheikhi, Shahid Beheshti University of Medical Sciences, Tehran, Iran. Sonali Srivastava, Anode Governance Lab, Bengaluru, India. Andrea Sullivan, University of Miami, Coral Gables, FL, USA. Yihenew Tesfaye, Oregon State University, Corvallis, OR, USA. Nathaly Triviño, Pontificia Universidad Javeriana, Bogotá, Colombia. Alex Trowell, University of Amsterdam, Amsterdam, The Netherlands. Desire Tshala-Katumbay, Oregon Health & Science University, Portland, OR, USA. Raymond Tutu, Delaware State University, Dover, DE, USA.
Credit author statement
Justin Stoler: Conceptualization, Funding Acquisition, Investigation, Project Administration, Resources, Writing - Original Draft, Writing - Review & Editing Joshua D. Miller: Conceptualization, Formal Analysis, Investigation, Project Administration, Resources, Visualization, Writing - Original Draft, Writing - Review & Editing Alexandra Brewis: Conceptualization, Funding Acquisition, Investigation, Resources, Writing - Original Draft, Writing - Review & Editing Matthew C. Freeman: Funding Acquisition, Investigation, Resources, Writing - Original Draft, Writing - Review & Editing Leila Harris: Conceptualization, Writing - Original Draft, Writing - Review & Editing Wendy E. Jepson: Conceptualization, Funding Acquisition, Investigation, Resources, Writing - Original Draft, Writing - Review & Editing Amber L. Pearson: Conceptualization, Funding Acquisition, Investigation, Resources, Writing - Original Draft, Writing - Review & Editing Asher Y. Rosinger: Conceptualization, Funding Acquisition, Investigation, Resources, Writing - Original Draft, Writing - Review & Editing Sameer H. Shah: Writing - Original Draft, Writing - Review & Editing Chad Staddon: Conceptualization, Funding Acquisition, Investigation, Resources, Writing - Original Draft, Writing - Review & Editing Cassandra Workman: Funding Acquisition, Investigation, Resources, Writing - Original Draft, Writing - Review & Editing Amber Wutich: Conceptualization, Funding Acquisition, Investigation, Resources, Writing - Original Draft, Writing - Review & Editing Sera L. Young: Conceptualization, Funding Acquisition, Investigation, Resources, Writing - Original Draft, Writing - Review & Editing HWISE RCN: Funding Acquisition, Investigation, Resources.
Declaration of competing interest
This research does not contain any conflict of interests.
Acknowledgments
The authors acknowledge the support of the Household Water Insecurity Experiences Research Coordination Network (HWISE RCN) funded by National Science Foundation grant number BCS-1759972. The HWISE study was funded with the Competitive Research Grants to Develop Innovative Methods and Metrics for Agriculture and Nutrition Actions (IMMANA). IMMANA is funded with UK Aid from the UK government. This project was also supported by the Buffett Institute for Global Studies and the Center for Water Research at Northwestern University; Arizona State University’s Center for Global Health at the School of Human Evolution and Social Change and Decision Center for a Desert City (National Science Foundation SES-1462086); the Office of the Vice Provost for Research of the University of Miami; and the National Institutes of Health grant NIEHS/FIC R01ES019841 for the Kahemba Study, DRC. SLY was supported by the National Institutes of Health (NIMH R21 MH108444; NIMH K01 MH098902). WEJ was supported by the National Science Foundation (BCS-1560962) and the Texas A&M University-CONACYT Research Collaborative Grant. CS was supported by the Lloyd’s Register Foundation. Funders of the study had no role in study design, data collection, data analysis, data interpretation or writing of the report. Authors had full access to all study data and had final responsibility for the decision to submit for publication.
Contributor Information
Household Water Insecurity Experiences Research Coordination Network (HWISE RCN):
Ellis Adams, Farooq Ahmed, Mallika Alexander, Gershim Asiki, Mobolanle Balogun, Michael J. Boivin, Genny Carrillo, Kelly Chapman, Stroma Cole, Shalean M. Collins, Hassan Eini-Zinab, Jorge Escobar-Vargas, Hala Ghattas, Monet Ghorbani, Ashley Hagaman, Nicola Hawley, Zeina Jamaluddine, Divya Krishnakumar, Kenneth Maes, Jyoti Mathad, Jonathan Maupin, Patrick Mbullo Owuor, Hugo Melgar-Quiñonez, Milton Marin Morales, Javier Moran, Nasrin Omidvar, Sabrina Rasheed, Luisa Samayoa-Figueroa, Ernesto C. Sánchez-Rodriguez, Marianne V. Santoso, Roseanne C. Schuster, Mahdieh Sheikhi, Sonali Srivastava, Andrea Sullivan, Yihenew Tesfaye, Nathaly Triviño, Alex Trowell, Desire Tshala-Katumbay, and Raymond Tutu
References
- Adler N., Stewart J., Psychosocial Working Group The MacArthur scale of subjective social status. 2007. https://macses.ucsf.edu/research/psychosocial/subjective.php Available at:
- Amankwaa G., Ampratwum E.F. COVID-19 ‘free water’ initiatives in the Global South: what does the Ghanaian case mean for equitable and sustainable water services? Water Int. 2020;45:722–729. doi: 10.1080/02508060.2020.1845076. [DOI] [Google Scholar]
- Bartram J., Hunter P. In: Routledge Handbook of Water and Health. Bartram J., Baum R., Coclanis P.A., Gute D.M., Kay D., McFadyen S., Pond K., Robertson W., Rouse M.J., editors. Routledge; London, UK: 2015. Bradley Classification of disease transmission routes for water-related hazards; pp. 38–55. [Google Scholar]
- Baxter D., Casady C.B. A coronavirus (COVID-19) triage framework for (sub) national public–private partnership (PPP) programs. Sustainability. 2020;12:5253. doi: 10.3390/su12135253. [DOI] [Google Scholar]
- Booysen M.J., Visser M., Burger R. Temporal case study of household behavioural response to Cape Town's “Day Zero” using smart meter data. Water Res. 2019;149:414–420. doi: 10.1016/j.watres.2018.11.035. [DOI] [PubMed] [Google Scholar]
- Brewis A., Workman C., Wutich A., Jepson W., Young S., the HWISE RCN Household water insecurity is strongly associated with food insecurity: evidence from 27 sites in low- and middle-income countries. Am. J. Hum. Biol. 2020;32 doi: 10.1002/ajhb.23309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burki T. COVID-19 in Latin America. Lancet Infect. Dis. 2020;20:547–548. doi: 10.1016/S1473-3099(20)30303-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calder P.C., Jackson A.A. Undernutrition, infection and immune function. Nutr. Res. Rev. 2000;13:3–29. doi: 10.1079/095442200108728981. [DOI] [PubMed] [Google Scholar]
- Caruso B.A., Freeman M.C. Shared sanitation and the spread of COVID-19: risks and next steps. The Lancet Planetary Health. 2020;4:e173. doi: 10.1016/S2542-5196(20)30086-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casady C.B., Baxter D. Pandemics, public-private partnerships (PPPs), and force majeure | COVID-19 expectations and implications. Construct. Manag. Econ. 2020;38:1077–1085. doi: 10.1080/01446193.2020.1817516. [DOI] [Google Scholar]
- Casey V. WaterAid; London, UK: 2020. Four Things that Help Water Services to Combat the COVID-19 Pandemic. [Google Scholar]
- CDC . 2020. Cleaning and Disinfection for Households: Interim Recommendations for U.S. Households with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19)https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cleaning-disinfection.html [WWW Document]. URL. [Google Scholar]
- Choudhary N., Brewis A., Wutich A., Bhushan Udas P. Sub-optimal household water access is associated with greater risk of intimate partner violence against women: evidence from Nepal. J. Water Health. 2020:579–594. doi: 10.2166/wh.2020.024. [DOI] [PubMed] [Google Scholar]
- Collins S.M., Mbullo Owuor P., Miller J.D., Boateng G.O., Wekesa P., Onono M., Young S.L. “I know how stressful it is to lack water!” Exploring the lived experiences of household water insecurity among pregnant and postpartum women in western Kenya. Glob. Publ. Health. 2019;14:649–662. doi: 10.1080/17441692.2018.1521861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper R. Institute of Development Studies; Brighton, UK: 2020. Water Security beyond COVID-19 (No. K4D Helpdesk Report 803) [Google Scholar]
- Cooper R. Institute of Development Studies; Brighton, UK: 2020. Water for the Urban Poor and COVID-19 (No. K4D Helpdesk Report 826) [Google Scholar]
- Corburn J., Vlahov D., Mberu B., Riley L., Caiaffa W.T., Rashid S.F., Ko A., Patel S., Jukur S., Martínez-Herrera E., Jayasinghe S., Agarwal S., Nguendo-Yongsi B., Weru J., Ouma S., Edmundo K., Oni T., Ayad H. Slum health: arresting COVID-19 and improving well-being in urban informal settlements. J. Urban Health. 2020;97:348–357. doi: 10.1007/s11524-020-00438-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deshpande A., Miller-Petrie M.K., Lindstedt P.A., Baumann M.M., Johnson K.B., Blacker B.F., Abbastabar H., Abd-Allah F., Abdelalim A., Abdollahpour I., Abegaz K.H., Abejie A.N., Abreu L.G., Abrigo M.R.M., Abualhasan A., Accrombessi M.M.K., Adamu A.A., Adebayo O.M., Adedeji I.A., Adedoyin R.A., Adekanmbi V., Adetokunboh O.O., Adhikari T.B., Afarideh M., Agudelo-Botero M., Ahmadi M., Ahmadi K., Ahmed M.B., Ahmed A.E., Akalu T.Y., Akanda A.S., Alahdab F., Al-Aly Z., Alam S., Alam N., Alamene G.M., Alanzi T.M., Albright J., Albujeer A., Alcalde-Rabanal J.E., Alebel A., Alemu Z.A., Ali M., Alijanzadeh M., Alipour V., Aljunid S.M., Almasi A., Almasi-Hashiani A., Al-Mekhlafi H.M., Altirkawi K.A., Alvis-Guzman N., Alvis-Zakzuk N.J., Amini S., Amit A.M.L., Amul G.G.H., Andrei C.L., Anjomshoa M., Ansariadi A., Antonio C.A.T., Antony B., Antriyandarti E., Arabloo J., Aref H.M.A., Aremu O., Armoon B., Arora A., Aryal K.K., Arzani A., Asadi-Aliabadi M., Asmelash D., Atalay H.T., Athari S.M., Athari S.S., Atre S.R., Ausloos M., Awasthi S., Awoke N., Ayala Quintanilla B.P., Ayano G., Ayanore M.A., Aynalem Y.A., Azari S., Azman A.S., Babaee E., Badawi A., Bagherzadeh M., Bakkannavar S.M., Balakrishnan S., Banach M., Banoub J.A.M., Barac A., Barboza M.A., Bärnighausen T.W., Basu S., Bay V.D., Bayati M., Bedi N., Beheshti M., Behzadifar Meysam, Behzadifar Masoud, Bejarano Ramirez D.F., Bell M.L., Bennett D.A., Benzian H., Berbada D.A., Bernstein R.S., Bhat A.G., Bhattacharyya K., Bhaumik S., Bhutta Z.A., Bijani A., Bikbov B., Bin Sayeed M.S., Biswas R.K., Bohlouli S., Boufous S., Brady O.J., Briko A.N., Briko N.I., Britton G.B., Brown A., Burugina Nagaraja S., Butt Z.A., Cámera L.A., Campos-Nonato I.R., Campuzano Rincon J.C., Cano J., Car J., Cárdenas R., Carvalho F., Castañeda-Orjuela C.A., Castro F., Cerin E., Chalise B., Chattu V.K., Chin K.L., Christopher D.J., Chu D.-T., Cormier N.M., Costa V.M., Cromwell E.A., Dadi A.F.F., Dahiru T., Dahlawi S.M.A., Dandona R., Dandona L., Dang A.K., Daoud F., Darwesh A.M., Darwish A.H., Daryani A., Das J.K., Das Gupta R., Dash A.P., Dávila-Cervantes C.A., Davis Weaver N., De la Hoz F.P., De Neve J.-W., Demissie D.B., Demoz G.T., Denova-Gutiérrez E., Deribe K., Desalew A., Dharmaratne S.D., Dhillon P., Dhimal M., Dhungana G.P., Diaz D., Dipeolu I.O., Do H.T., Dolecek C., Doyle K.E., Dubljanin E., Duraes A.R., Edinur H.A., Effiong A., Eftekhari A., El Nahas N., El Sayed Zaki M., El Tantawi M., Elhabashy H.R., El-Jaafary S.I., El-Khatib Z., Elkout H., Elsharkawy A., Enany S., Endalew D.A., Eshrati B., Eskandarieh S., Etemadi A., Ezekannagha O., Faraon E.J.A., Fareed M., Faro A., Farzadfar F., Fasil A.F., Fazlzadeh M., Feigin V.L., Fekadu W., Fentahun N., Fereshtehnejad S.-M., Fernandes E., Filip I., Fischer F., Flohr C., Foigt N.A., Folayan M.O., Foroutan M., Franklin R.C., Frostad J.J., Fukumoto T., Gad M.M., Garcia G.M., Gatotoh A.M., Gayesa R.T., Gebremedhin K.B., Geramo Y.C.D., Gesesew H.A., Gezae K.E., Ghashghaee A., Ghazi Sherbaf F., Gill T.K., Gill P.S., Ginindza T.G., Girmay A., Gizaw Z., Goodridge A., Gopalani S.V., Goulart B.N.G., Goulart A.C., Grada A., Green M.S., Gubari M.I.M., Gugnani H.C., Guido D., Guimarães R.A., Guo Y., Gupta Rajeev, Gupta Rahul, Ha G.H., Haagsma J.A., Hafezi-Nejad N., Haile D.H., Haile M.T., Hall B.J., Hamidi S., Handiso D.W., Haririan H., Hariyani N., Hasaballah A.I., Hasan M.M., Hasanzadeh A., Hassen H.Y., Hayelom D.H., Hegazy M.I., Heibati B., Heidari B., Hendrie D., Henok A., Herteliu C., Heydarpour F., Hidru H.D. de, Hird T.R., Hoang C.L., Hollerich G.I., Hoogar P., Hossain N., Hosseinzadeh M., Househ M., Hu G., Humayun A., Hussain S.A., Hussen M.A.A., Ibitoye S.E., Ilesanmi O.S., Ilic M.D., Imani-Nasab M.H., Iqbal U., Irvani S.S.N., Islam S.M.S., Ivers R.Q., Iwu C.J., Jahanmehr N., Jakovljevic M., Jalali A., Jayatilleke A.U., Jenabi E., Jha R.P., Jha V., Ji J.S., Jonas J.B., Jozwiak J.J., Kabir A., Kabir Z., Kanchan T., Karch A., Karki S., Kasaeian A., Kasahun G.G., Kasaye H.K., Kassa G.G., Kassa G.M., Kayode G.A., Kebede M.M., Keiyoro P.N., Ketema D.B., Khader Y.S., Khafaie M.A., Khalid N., Khalilov R., Khan E.A., Khan J., Khan M.N., Khatab K., Khater M.M., Khater A.M., Khayamzadeh M., Khazaei M., Khosravi M.H., Khubchandani J., Kiadaliri A., Kim Y.J., Kimokoti R.W., Kisa S., Kisa A., Kochhar S., Kolola T., Komaki H., Kosen S., Koul P.A., Koyanagi A., Krishan K., Kuate Defo B., Kugbey N., Kumar P., Kumar G.A., Kumar M., Kusuma D., La Vecchia C., Lacey B., Lal A., Lal D.K., Lam H., Lami F.H., Lansingh V.C., Lasrado S., Lebedev G., Lee P.H., LeGrand K.E., Leili M., Lenjebo T.L., Leshargie C.T., Levine A.J., Lewycka S., Li S., Linn S., Liu S., Lopez J.C.F., Lopukhov P.D., Magdy Abd El Razek M., Mahadeshwara Prasad D.R., Mahasha P.W., Mahotra N.B., Majeed A., Malekzadeh R., Malta D.C., Mamun A.A., Manafi N., Mansournia M.A., Mapoma C.C., Martinez G., Martini S., Martins-Melo F.R., Mathur M.R., Mayala B.K., Mazidi M., McAlinden C., Meharie B.G., Mehndiratta M.M., Mehrabi Nasab E., Mehta K.M., Mekonnen T., Mekonnen T.C., Meles G.G., Meles H.G., Memiah P.T.N., Memish Z.A., Mendoza W., Menezes R.G., Mereta S.T., Meretoja T.J., Mestrovic T., Metekiya W.M., Metekiya W.M., Miazgowski B., Miller T.R., Mini G.K., Mirrakhimov E.M., Moazen B., Mohajer B., Mohammad Y., Mohammad D.K., Mohammad Gholi Mezerji N., Mohammadibakhsh R., Mohammed S., Mohammed J.A., Mohammed H., Mohebi F., Mokdad A.H., Moodley Y., Moradi M., Moradi G., Moradi-Joo M., Moraga P., Morales L., Mosapour A., Mosser J.F., Mouodi S., Mousavi S.M., Mozaffor M., Munro S.B., Muriithi M.K., Murray C.J.L., Musa K.I., Mustafa G., Muthupandian S., Naderi M., Nagarajan A.J., Naghavi M., Naik G., Nangia V., Nascimento B.R., Nazari J., Ndwandwe D.E., Negoi I., Netsere H.B., Ngunjiri J.W., Nguyen C.T., Nguyen H.L.T., Nguyen Q.P., Nigatu S.G., Ningrum D.N.A., Nnaji C.A., Nojomi M., Norheim O.F., Noubiap J.J., Oancea B., Ogbo F.A., Oh I.-H., Olagunju A.T., Olusanya J.O., Olusanya B.O., Onwujekwe O.E., Ortega-Altamirano D.V., Osarenotor O., Osei F.B., Owolabi M.O., Pa M., Padubidri J.R., Pakhale S., Pana A., Park E.-K., Patel S.K., Pathak A., Patle A., Paulos K., Pepito V.C.F., Perico N., Pervaiz A., Pescarini J.M., Pesudovs K., Pham H.Q., Pigott D.M., Pilgrim T., Pirsaheb M., Poljak M., Pollock I., Postma M.J., Pourmalek F., Pourshams A., Prada S.I., Preotescu L., Quintana H., Rabiee N., Rabiee M., Radfar A., Rafiei A., Rahim F., Rahimi S., Rahimi-Movaghar V., Rahman M.A., Rahman M.H.U., Rajati F., Ranabhat C.L., Rao P.C., Rasella D., Rath G.K., Rawaf S., Rawal L., Rawasia W.F., Remuzzi G., Renjith V., Renzaho A.M.N., Resnikoff S., Riahi S.M., Ribeiro A.I., Rickard J., Roever L., Ronfani L., Rubagotti E., Rubino S., Saad A.M., Sabour S., Sadeghi E., Saeedi Moghaddam S., Safari Y., Sagar R., Sahraian M.A., Sajadi S.M., Salahshoor M.R., Salam N., Saleem A., Salem H., Salem M.R., Salimi Y., Salimzadeh H., Samy A.M., Sanabria J., Santos I.S., Santric-Milicevic M.M., Sao Jose B.P., Saraswathy S.Y.I., Sarrafzadegan N., Sartorius B., Sathian B., Sathish T., Satpathy M., Sawhney M., Sayyah M., Sbarra A.N., Schaeffer L.E., Schwebel D.C., Senbeta A.M., Senthilkumaran S., Sepanlou S.G., Serván-Mori E., Shafieesabet A., Shaheen A.A., Shahid I., Shaikh M.A., Shalash A.S., Shams-Beyranvand M., Shamsi M., Shamsizadeh M., Shannawaz M., Sharafi K., Sharma R., Sheikh A., Shetty B.S.K., Shiferaw W.S., Shigematsu M., Shin J.I., Shiri R., Shirkoohi R., Shivakumar K.M., Si S., Siabani S., Siddiqi T.J., Silva D.A.S., Singh V., Singh N.P., Singh B.B.S., Singh J.A., Singh A., Sinha D.N., Sisay M.M., Skiadaresi E., Smith D.L., Soares Filho A.M., Sobhiyeh M.R., Sokhan A., Soriano J.B., Sorrie M.B., Soyiri I.N., Spurlock E.E., Sreeramareddy C.T., Sudaryanto A., Sufiyan M.B., Suleria H.A.R., Sykes B.L., Tabarés-Seisdedos R., Tabuchi T., Tadesse D.B., Tarigan I.U., Taye B., Tefera Y.M., Tehrani-Banihashemi A., Tekelemedhin S.W., Tekle M.G., Temsah M.-H., Tesfay B.E., Tesfay F.H., Tessema Z.T., Thankappan K.R., ThekkePurakkal A.S., Thomas N., Thompson R.L., Thomson A.J., Topor-Madry R., Tovani-Palone M.R., Traini E., Tran B.X., Tran K.B., Ullah I., Unnikrishnan B., Usman M.S., Uthman O.A., Uzochukwu B.S.C., Valdez P.R., Varughese S., Veisani Y., Violante F.S., Vollmer S., W/hawariat F.G., Waheed Y., Wallin M.T., Wang Y.-P., Wang Y., Wangdi K., Weiss D.J., Weldesamuel G.T., Werkneh A.A., Westerman R., Wiangkham T., Wiens K.E., Wijeratne T., Wiysonge C.S., Wolde H.F., Wondafrash D.Z., Wonde T.E., Worku G.T., Yadollahpour A., Yahyazadeh Jabbari S.H., Yamada T., Yaseri M., Yatsuya H., Yeshaneh A., Yilma M.T., Yip P., Yisma E., Yonemoto N., Younis M.Z., Yousof H.-A.S.A., Yu C., Yusefzadeh H., Zadey S., Zahirian Moghadam T., Zaidi Z., Zaman S.B., Zamani M., Zandian H., Zar H.J., Zerfu T.A., Zhang Y., Ziapour A., Zodpey S., Zuniga Y.M.H., Hay S.I., Reiner R.C. Mapping geographical inequalities in access to drinking water and sanitation facilities in low-income and middle-income countries, 2000–17. Lancet Glob. Health. 2020;8:e1162–e1185. doi: 10.1016/S2214-109X(20)30278-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorn A. van, Cooney R.E., Sabin M.L. COVID-19 exacerbating inequalities in the US. Lancet. 2020;395:1243–1244. doi: 10.1016/S0140-6736(20)30893-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekumah B., Armah F.A., Yawson D.O., Quansah R., Nyieku F.E., Owusu S.A., Odoi J.O., Afitiri A.-R. Disparate on-site access to water, sanitation, and food storage heighten the risk of COVID-19 spread in Sub-Saharan Africa. Environ. Res. 2020;189:109936. doi: 10.1016/j.envres.2020.109936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enqvist J.P., Ziervogel G. Water governance and justice in Cape Town: an overview. WIREs Water. 2019;6:e1354. doi: 10.1002/wat2.1354. [DOI] [Google Scholar]
- Galloway S.E., Prabasaj P., MacCannell D.R., Johansson M.A., Brooks J.T., MacNeil A., Slayton R.B., Tong S., Silk B.J., Armstrong G.L., Biggerstaff M., Dugan V.G. Emergence of SARS-CoV-2 B.1.1.7 lineage — United States, december 29, 2020–january 12, 2021. MMWR Morb. Mortal. Wkly. Rep. 2021;70 doi: 10.15585/mmwr.mm7003e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geere J.-A., Cortobius M. Who carries the weight of water? Fetching water in rural and urban areas and the implications for water security. Water Altern. (WaA) 2017;10:513–540. [Google Scholar]
- Guppy M.P.B., Mickan S.M., Mar C.B.D. “Drink plenty of fluids”: a systematic review of evidence for this recommendation in acute respiratory infections. BMJ. 2004;328:499–500. doi: 10.1136/bmj.38028.627593.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopman J., Allegranzi B., Mehtar S. Managing COVID-19 in low- and middle-income countries. J. Am. Med. Assoc. 2020;323:1549–1550. doi: 10.1001/jama.2020.4169. [DOI] [PubMed] [Google Scholar]
- Human Rights Watch . 2020. Uganda: Respect Rights in COVID-19 Response. [Google Scholar]
- Hutton G., Haller L., Bartram J. Global cost-benefit analysis of water supply and sanitation interventions. J. Water Health. 2007;5:481–502. doi: 10.2166/wh.2007.009. [DOI] [PubMed] [Google Scholar]
- Hutton G., Varughese M. World Bank Group; Washington, DC: 2016. The Costs of Meeting the 2030 Sustainable Development Goal Targets on Drinking Water, Sanitation, and Hygiene. [Google Scholar]
- Jepson W.E., Wutich A., Colllins S.M., Boateng G.O., Young S.L. Progress in household water insecurity metrics: a cross-disciplinary approach. WIREs Water. 2017;4:e1214. doi: 10.1002/wat2.1214. [DOI] [Google Scholar]
- Jowers K., Timmins C., Bhavsar N. Nicholas Institute for Environmental Policy Solutions; 2020. Policy in the Pandemic: Housing Security Policies Reduce U.S. COVID-19 Infection Rates. [Google Scholar]
- Kraemer M.U.G., Yang C.-H., Gutierrez B., Wu C.-H., Klein B., Pigott D.M., du Plessis L., Faria N.R., Li R., Hanage W.P., Brownstein J.S., Layan M., Vespignani A., Tian H., Dye C., Pybus O.G., Scarpino S.V. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science. 2020;368:493–497. doi: 10.1126/science.abb4218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makoni M. COVID-19 in Africa: half a year later. Lancet Infect. Dis. 2020;20:1127. doi: 10.1016/S1473-3099(20)30708-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxfield A. Testing the theoretical similarities between food and water insecurity: buffering hypothesis and effects on mental wellbeing. Soc. Sci. Med. 2020;244:112412. doi: 10.1016/j.socscimed.2019.112412. [DOI] [PubMed] [Google Scholar]
- Meehan K., Jepson W., Harris L.M., Wutich A., Beresford M., Fencl A., London J., Pierce G., Radonic L., Wells C., Wilson N.J., Adams E.A., Arsenault R., Brewis A., Harrington V., Lambrinidou Y., McGregor D., Patrick R., Pauli B., Pearson A.L., Shah S., Splichalova D., Workman C., Young S. Exposing the myths of household water insecurity in the global north: a critical review. WIREs Water. 2020;7:e1486. doi: 10.1002/wat2.1486. [DOI] [Google Scholar]
- Mekonnen M.M., Hoekstra A.Y. Four billion people facing severe water scarcity. Sci. Adv. 2016;2 doi: 10.1126/sciadv.1500323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mollah S., Islam Z. Dhaka Slums: where Covid is curiously quiet. The Daily Star. 2020 [Google Scholar]
- Monteiro de Oliveira M., Fuller T.L., Brasil P., Gabaglia C.R., Nielsen-Saines K. Controlling the COVID-19 pandemic in Brazil: a challenge of continental proportions. Nat. Med. 2020;26:1505–1506. doi: 10.1038/s41591-020-1071-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mushavi R.C., Burns B.F.O., Kakuhikire B., Owembabazi M., Vořechovská D., McDonough A.Q., Cooper-Vince C.E., Baguma C., Rasmussen J.D., Bangsberg D.R., Tsai A.C. “When you have no water, it means you have no peace”: a mixed-methods, whole-population study of water insecurity and depression in rural Uganda. Soc. Sci. Med. 2020;245:112561. doi: 10.1016/j.socscimed.2019.112561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popkin B.M., D'Anci K.E., Rosenberg I.H. Water, hydration, and health. Nutr. Rev. 2010;68:439–458. doi: 10.1111/j.1753-4887.2010.00304.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prüss-Ustün A., Wolf J., Bartram J., Clasen T., Cumming O., Freeman M.C., Gordon B., Hunter P.R., Medlicott K., Johnston R. Burden of disease from inadequate water, sanitation and hygiene for selected adverse health outcomes: an updated analysis with a focus on low- and middle-income countries. Int. J. Hyg Environ. Health. 2019;222 doi: 10.1016/j.ijheh.2019.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raju E., Ayeb-Karlsson S. COVID-19: how do you self-isolate in a refugee camp? Int. J. Publ. Health. 2020 doi: 10.1007/s00038-020-01381-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosinger A.Y., Brewis A., Wutich A., Jepson W., Staddon C., Stoler J., Young S.L. Water borrowing is consistently practiced globally and is associated with water-related system failures across diverse environments. Global Environ. Change. 2020;64:102148. doi: 10.1016/j.gloenvcha.2020.102148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadoff C.W., Borgomeo E., Uhlenbrook S. Rethinking water for SDG 6. Nat. Sustain. 2020;3:346–347. doi: 10.1038/s41893-020-0530-9. [DOI] [Google Scholar]
- Schuster R.C., Butler M.S., Wutich A., Miller J.D., Young S.L., Household Water Insecurity Experiences-Research Coordination Network “If there is no water, we cannot feed our children”: the far-reaching consequences of water insecurity on infant feeding practices and infant health across 16 low- and middle-income countries. Am. J. Hum. Biol. 2020;32 doi: 10.1002/ajhb.23357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scoones I. Livelihoods perspectives and rural development. J. Peasant Stud. 2009;36:171–196. doi: 10.1080/03066150902820503. [DOI] [Google Scholar]
- Seddighi H., Seddighi S., Salmani I., Sharifi Sedeh M. Public-private-people partnerships (4P) for improving the response to COVID-19 in Iran. Disaster Med. Public Health Prep. 2020:1–6. doi: 10.1017/dmp.2020.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sihaloho E.D., Wiksadana W., Siregar C.D.T. Impacts of regional economic factors on the transmission of coronavirus disease 2019 (COVID-19) in Indonesia. Ekonomis: J. Econ. Bus. 2020;4:397–403. doi: 10.33087/ekonomis.v4i2.180. [DOI] [Google Scholar]
- Smiley S.L., Agbemor B.D., Adams E.A., Tutu R. COVID-19 and water access in Sub-Saharan Africa: Ghana's free water directive may not benefit water insecure households. Afr. Geog. Rev. 2020;39:398–404. doi: 10.1080/19376812.2020.1810083. 0. [DOI] [Google Scholar]
- Smiley S.L., Stoler J. Socio-environmental confounders of safe water interventions. WIREs Water. 2020;7:e1438. doi: 10.1002/wat2.1438. [DOI] [Google Scholar]
- Staddon C., Everard M., Mytton J., Octavianti T., Powell W., Quinn N., Uddin S.M.N., Young S.L., Miller J.D., Budds J., Geere J.-A., Meehan K., Charles K., Stevenson E.G.J., Vonk J., Miziniak J. Water insecurity compounds the global coronavirus crisis. Water Int. 2020;45:416–422. doi: 10.1080/02508060.2020.1769345. [DOI] [Google Scholar]
- Stoler J., Brewis A., Harris L.M., Wutich A., Pearson A.L., Rosinger A.Y., Schuster R.C., Young S.L. Household water sharing: a missing link in international health. Int. Health. 2019;11:163–165. doi: 10.1093/inthealth/ihy094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoler J., Jepson W.E., Wutich A. Beyond handwashing: water insecurity undermines COVID-19 response in developing areas. J. Glob. Health. 2020;10 doi: 10.7189/jogh.10.010355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sultana F. Suffering for water, suffering from water: emotional geographies of resource access, control and conflict. Geoforum. 2011;42:163–172. doi: 10.1016/j.geoforum.2010.12.002. [DOI] [Google Scholar]
- Sznycer D., Tooby J., Cosmides L., Porat R., Shalvi S., Halperin E. Shame closely tracks the threat of devaluation by others, even across cultures. Proc. Natl. Acad. Sci. Unit. States Am. 2016;113:2625–2630. doi: 10.1073/pnas.1514699113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNICEF . 2020. Mitigating the Impacts of COVID-19 on Menstrual Health and Hygiene. [Google Scholar]
- United Nations . United Nations; 2020. Policy Brief: the Impact of COVID-19 on Women. [Google Scholar]
- USAID Water Leadership Council . 2020. USAID Water, Sanitation and Hygiene (WASH): Strategic Approach to COVID-19 Response 9. [Google Scholar]
- van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N., Tamin A., Harcourt J.L., Thornburg N.J., Gerber S.I., Lloyd-Smith J.O., de Wit E., Munster V.J. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venkataramanan V., Geere J.-A.L., Thomae B., Stoler J., Hunter P.R., Young S.L., and the HWISE RCN In pursuit of ‘safe’ water: the burden of personal injury from water fetching in 21 low-income and middle-income countries. BMJ Glob. Health. 2020;5 doi: 10.1136/bmjgh-2020-003328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberg A.D., Minaker K.L., Coble Y.D., Davis R.M., Head C.A., Howe J.P., Karlan M.S., Kennedy W.R., Numann P.J., Spillman M.A., Skelton W.D., Steinhilber R.M., Strong J.P., Wagner H.N., Allen J.R., Rinaldi R.C. Dehydration: evaluation and management in older adults. J. Am. Med. Assoc. 1995;274:1552–1556. doi: 10.1001/jama.1995.03530190066035. [DOI] [PubMed] [Google Scholar]
- WHO, Coronavirus disease (COVID-19) advice for the public 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public [WWW Document]. URL.
- WHO/UNICEF Water, sanitation, hygiene, and waste management for the COVID-19 virus: interim guidance. 2020. https://www.who.int/publications-detail/water-sanitation-hygiene-and-waste-management-for-the-covid-19-virus-interim-guidance [WWW Document]. URL.
- WHO/UNICEF . WHO, UNICEF; 2020. Almost 2 Billion People Depend on Health Care Facilities without Basic Water Services. [Google Scholar]
- WHO/UNICEF . World Health Organization; Geneva: 2017. Progress on Drinking Water, Sanitation and Hygiene: 2017 Update and SDG Baselines. [Google Scholar]
- World Bank . World Bank Group; Washington, DC: 2020. COVID-19 Crisis through a Migration Lens. [Google Scholar]
- Wu Y., Guo C., Tang L., Hong Z., Zhou J., Dong X., Yin H., Xiao Q., Tang Y., Qu X., Kuang L., Fang X., Mishra N., Lu J., Shan H., Jiang G., Huang X. Prolonged presence of SARS-CoV-2 viral RNA in faecal samples. Lancet Gastroenterol. Hepatol. 2020;5:434–435. doi: 10.1016/S2468-1253(20)30083-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wutich A., Brewis A. Food, water, and scarcity: toward a broader anthropology of resource insecurity. Curr. Anthropol. 2014;55:444–468. doi: 10.1086/677311. [DOI] [Google Scholar]
- Wutich A., Brewis A., Tsai A.C. Water and mental health. WIREs Water. 2020;7 doi: 10.1002/wat2.1461. [DOI] [Google Scholar]
- Wutich A., Budds J., Jepson W., Harris L.M., Adams E., Brewis A., Cronk L., DeMyers C., Maes K., Marley T., Miller J., Pearson A., Rosinger A.Y., Schuster R.C., Stoler J., Staddon C., Wiessner P., Workman C., Young S. Household water sharing: A review of water gifts, exchanges, and transfers across cultures. WIREs Water. 2018;5 doi: 10.1002/wat2.1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wutich A., Ragsdale K. Water insecurity and emotional distress: coping with supply, access, and seasonal variability of water in a Bolivian squatter settlement. Soc. Sci. Med. 2008;67:2116–2125. doi: 10.1016/j.socscimed.2008.09.042. [DOI] [PubMed] [Google Scholar]
- Yeo C., Kaushal S., Yeo D. Enteric involvement of coronaviruses: is faecal–oral transmission of SARS-CoV-2 possible? Lancet Gastroenterol. Hepatol. 2020;5:335–336. doi: 10.1016/S2468-1253(20)30048-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young H.A., Cousins A., Johnston S., Fletcher J.M., Benton D. Autonomic adaptations mediate the effect of hydration on brain functioning and mood: evidence from two randomized controlled trials. Sci. Rep. 2019;9:16412. doi: 10.1038/s41598-019-52775-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young S.L., Boateng G., Jamaluddine Z., Miller J., Frongillo E., Neilands T., Collins S., Wutich A., Jepson W., Stoler J., the HWISE RCN The Household Water InSecurity Experiences (HWISE) Scale: development and validation of a household water insecurity measure for low- and middle-income countries. BMJ Glob. Health. 2019;4 doi: 10.1136/bmjgh-2019-001750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young S.L., Collins S.M., Boateng G.O., Neilands T.B., Jamaluddine Z., Miller J.D., Brewis A.A., Frongillo E.A., Jepson W.E., Melgar-Quiñonez H., Schuster R.C., Stoler J.B., Wutich A., the HWISE RCN Development and validation protocol for an instrument to measure household water insecurity across cultures and ecologies: the Household Water InSecurity Experiences (HWISE) Scale. BMJ Open. 2019;9 doi: 10.1136/bmjopen-2018-023558. [DOI] [PMC free article] [PubMed] [Google Scholar]