Abstract
Spontaneous pharyngeal haematoma is a rare but life-threatening cause of acute upper airway obstruction, and the clinical manifestation may mimic haemoptysis. A 65-year-old man presented to our emergency department with symptoms of sore throat and haemoptysis. He had no medical history. At arrival, O2 saturation was 95% on 5 L/min of oxygen with a mask. Results of a blood examination including a coagulation test were normal. Laryngoscopy showed enlargement of the left pharynx and a narrowed airway. Contrast-enhanced CT showed extravascular leakage of contrast medium inside the left pharyngeal haematoma. Fortunately, the haematoma did not lead to airway obstruction, and it decreased spontaneously. We finally diagnosed this case as spontaneous pharyngeal haematoma. When we examine a patient with a symptom of haemoptysis accompanied by sore throat, it is necessary to consider pharyngeal haematoma and to prepare emergency airway protection for acute upper airway obstruction.
Keywords: emergency medicine, ear, nose and throat/otolaryngology
Background
Acute haematomas of the neck and upper airway are usually caused by trauma, tumours1 or anticoagulants.2 Only a few cases of spontaneous haematomas of these sites have been reported.3 4 These conditions have the possibility of causing acute upper airway obstruction, and we should recognise them even if their frequency is low. Spontaneous pharyngeal haematoma is a rare but life-threatening condition that can cause acute upper airway obstruction. We present a case of spontaneous pharyngeal haematoma in a patient with a symptom of haemoptysis, which could have resulted in upper airway obstruction.
Case presentation
A 65-year-old man presented to our emergency department with symptoms of sudden sore throat and haemoptysis. He had no medical history and also had no history of trauma, foreign body ingestion or antithrombotic medication. On examination, blood pressure was 125/71 mm Hg, heart rate was 63 beats/min, respiratory rate was 16 breaths/min and O2 saturation was 95% on 5 L/min of oxygen with a mask. His left anterior neck was tender and there was fresh blood in his mouth with mild strider. A blood examination showed haemoglobin level of 125 g/L and platelet count of 191×109 /L with normal coagulation. Plain CT showed a mass lesion in the left pharynx with upper airway narrowing. He was transported to a tertiary medical hospital due to the possibility of airway obstruction.
Investigations
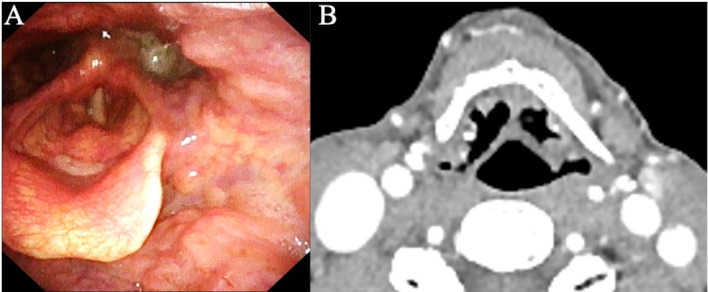
Laryngoscopy showed enlargement of the left pharynx, adhesion of blood and a narrowed airway (figure 1A). Contrast-enhanced CT showed extravascular leakage of contrast medium inside the left pharyngeal haematoma (figure 1B).
Figure 1.

Laryngoscopy showed enlargement of the left pharynx, adhesion of blood and a narrowed airway (A). Contrast-enhanced CT showed extravascular leakage of contrast medium (yellow arrow) inside the left pharyngeal haematoma (B). The yellow arrowhead indicates the superior thyroid artery.
Differential diagnosis
These findings suggest pharyngeal haematoma with active bleeding. The differential causes of bleeding may be hypopharyngeal cancer or ruptured aneurysm of external carotid artery branch. This patient had no history of spontaneous bleeding, and his blood examination was normal. Thus, the possibility of a disease with bleeding tendency is extremely low.
Treatment
He was admitted to the intensive care unit (ICU) due to the high risk of airway obstruction. He was fortunately discharged without endotracheal intubation 1 week later.
Outcome and follow-up
Laryngoscopy showed that the left pharyngeal haematoma had disappeared (figure 2A), and contrast-enhanced CT showed no mass lesion, aneurysm or vascular malformation in the left pharynx 4 weeks later (figure 2B). Therefore, we finally diagnosed this case as spontaneous pharyngeal haematoma.
Figure 2.
Laryngoscopy (A) and contrast-enhanced CT (B) showed that the left pharyngeal haematoma had disappeared.
Discussion
The course of the patient indicated two important clinical issues: (1) spontaneous pharyngeal haematoma is a rare but life-threatening cause of acute upper airway obstruction and (2) the clinical manifestation may mimic haemoptysis.
First, spontaneous pharyngeal haematoma is a rare but life-threatening cause of acute upper airway obstruction. Possible causes of acute airway obstruction include airway foreign bodies, anaphylaxis, infections such as acute epiglottitis, and posterior pharyngeal abscess, and angioedema. Acute haematomas of the upper airway including the pharynx are rare but life-threatening conditions that may rapidly cause acute airway obstruction. In fact, it has been reported that these conditions compromised the upper airway for a few minutes to several hours.3 4 Our patient was carefully observed in the ICU because he had strider and hypoxia, which indicated a high risk of upper airway obstruction. Fortunately, he was discharged without endotracheal intubation. However, we needed to prepare emergency airway equipment in case of upper airway compromise. In order to rescue upper airway compromise, we should recognise this life-threatening condition as soon as possible and protect the airway with an appropriate measure including emergency surgical airway.5
Second, acute haematomas of the upper airway including the pharynx may present expectoration of blood which mimics haemoptysis. The differential diagnosis of expectoration of blood is haemoptysis (ie, bleeding from the lower respiratory tract) or pseudohaemoptysis (ie, expectoration of blood other than haemoptysis). The most common causes of haemoptysis such as bronchiectasis, lung cancer, pulmonary tuberculosis and pulmonary mycosis are not life-threatening.6 7 Upper airway tract bleeding including epistasis and bleeding originating from the upper gastrointestinal tract are important to differentiate haemoptysis because they may mimic haemoptysis, and their management is greatly different from that of pseudohaemoptysis.8 Trauma, tumours, anticoagulants and rupture of an aneurysm are possible causes of acute haematomas of the upper airway and expectoration of blood. However, in our case, we could not identify these conditions even after examination by contrast-enhanced CT after the haematoma had disappeared. Thus, we finally diagnosed this case as spontaneous pharyngeal haematoma. In contrast, we could not identify the vessels causing bleeding. The pharynx is fed by vessels originating from the external carotid artery, and spontaneous rupture of vessels originating from the external carotid artery (eg, superior thyroid artery) has been reported.9 We assumed that this case may be related to these conditions.
In conclusion, spontaneous pharyngeal haematoma is a rare but life-threatening cause of acute upper airway obstruction, and the clinical manifestation may mimic haemoptysis. When we examine a patient with a symptom of haemoptysis accompanied by sore throat, it is necessary to consider pseudohaemoptysis due to pharyngeal haematoma and to prepare emergency airway protection for acute upper airway obstruction.
Learning points.
Spontaneous pharyngeal haematoma is a rare but life-threatening cause of acute upper airway obstruction.
Upper airway tract bleeding is important to differentiate haemoptysis because they may mimic haemoptysis, and their management is greatly different from that of pseudohaemoptysis.
When we examine a patient with a symptom of haemoptysis accompanied by sore throat, it is necessary to consider pseudohaemoptysis due to pharyngeal haematoma and to prepare emergency airway protection for acute upper airway obstruction.
Footnotes
Contributors: All authors contributed to the development of this manuscript. KO was responsible for literature search and writing of all manuscripts. YO, TI and YH were supervisors.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Hanashiro N, Yamashiro T, Iraha Y, et al. Non-Traumatic rupture of the superior thyroid artery with concomitant parathyroid adenoma and multinodular goiter. Acta Radiol Open 2017;6:205846011772281. 10.1177/2058460117722813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bloom DC, Haegen T, Keefe MA. Anticoagulation and spontaneous retropharyngeal hematoma. J Emerg Med 2003;24:389–94. 10.1016/S0736-4679(03)00035-0 [DOI] [PubMed] [Google Scholar]
- 3.Ditkofsky N, Hanna T. Spontaneous retropharyngeal hematoma. N Engl J Med Overseas Ed 2016;374:e3. 10.1056/NEJMicm1505596 [DOI] [PubMed] [Google Scholar]
- 4.Eidesheim M, Bouaziz H, François T, et al. Spontaneous laryngeal haematoma leading to airway obstruction after vaginal delivery. Int J Obstet Anesth 2018;36:137–8. 10.1016/j.ijoa.2018.05.003 [DOI] [PubMed] [Google Scholar]
- 5.Higgs A, McGrath BA, Goddard C, et al. Guidelines for the management of tracheal intubation in critically ill adults. Br J Anaesth 2018;120:323–52. 10.1016/j.bja.2017.10.021 [DOI] [PubMed] [Google Scholar]
- 6.Mondoni M, Carlucci P, Job S, et al. Observational, multicentre study on the epidemiology of haemoptysis. Eur Respir J 2018;51:1701813. 10.1183/13993003.01813-2017 [DOI] [PubMed] [Google Scholar]
- 7.Lee BR, Yu JY, Ban HJ, et al. Analysis of patients with hemoptysis in a tertiary referral hospital. Tuberc Respir Dis 2012;73:107–14. 10.4046/trd.2012.73.2.107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scott J, Thompson TD. Hemoptysis: evaluation and management. Am Fam Physician 2015;15:243–9. [PubMed] [Google Scholar]
- 9.Stenner M, Helmstaedter V, Spuentrup E, et al. Cervical hemorrhage due to spontaneous rupture of the superior thyroid artery: case report and review of the literature. Head Neck 2010;32:1277–81. 10.1002/hed.21213 [DOI] [PubMed] [Google Scholar]


