Abstract
Objective:
To evaluate clinical utility and feasibility of universal somatization screening in the pediatric emergency department (ED) using a standardized approach of (1) identifying potential somatizing symptoms within the ED, (2) introducing these patients and their caregivers to the concept of the ‘mind-body connection’, (3) corroborating the likelihood of a somatization diagnosis via brief psychiatric assessment, and (4) inviting families to a psychoeducational follow-up session.
Methods:
We conducted a cross-sectional study to carry out this approach with families visiting a pediatric ED. Our primary outcome of screening utility was measured as the proportion of youth who screened positive for somatization by the ED clinician. Our secondary outcome of screening feasibility was measured as the proportion of patients with positives who (1) agreed to meet with the study psychiatrist, (2) consented to an ED psychiatric assessment, (3) were assessed by the study psychiatrist as likely experiencing somatization, and (4) were invited for follow-up and attended.
Results:
Of the 344 screened patients, 27 (7.8%) screened positive for somatization. Of these, 25 (92.6%) families verbally consented to meet the study psychiatrist to learn about the mind-body connection, and 21 (77.8%) consented to further psychiatric assessment. Upon assessment, the somatization likelihood was supported for all 21 youth. Twenty families were invited to follow-up and ultimately two (10%) attended.
Conclusions:
Somatization can be detected through ED-based universal screening. Few families attended psychoeducational follow-up. Further research is needed to determine appropriate ED-initiated pediatric somatization intervention.
Keywords: Somatization, screening, child and adolescent, emergency department
Introduction
Somatization represents the interaction of psychological and biological processes in producing unintentional physical symptoms that can occur either in the presence or absence of verifiable physical illness (Lipowski, 1988). Population-level studies have shown somatization to be common, estimating that up to 50% of the general pediatric population experience at least one somatic symptom at some point (Campo & Fritsch, 1994; Lieb et al., 2000). Somatization is a normal phenomenon, but sometimes has short-or long-term impacts on health and functioning, including developmental impairment, mental health disorders, reduced school attendance, and poor academic performance (Beck, 2008; Offord et al., 1987). Youth experiencing somatizing complaints incur high health care costs associated with more frequent health care utilization, including primary and acute care visits, inpatient admissions, and specialist consultations (Saunders et al., 2020).
The rising number of mental health-related visits across pediatric emergency departments (Canadian Institute for Health Information, 2015; Mapelli et al., 2015; Sills & Bland, 2002), coupled with evidence that physical complaints can also involve underlying mental health concerns, suggests that a number of ED visits may implicate some component of somatization (de Gusmão et al., 2014; Gelauff et al., 2014). Somatization is not routinely recognized in the ED, as prioritization of serious physical symptoms may overshadow identification of underlying psychological distress (Stephenson & Price, 2006). Early identification of somatization is important in order to avoid excessive medical workup and to help facilitate transition to appropriate mental health services (Barsky & Borus, 1999; Dworetzky et al., 2015; Furness et al., 2009; LaFrance & Benbadis, 2006; Mayou et al., 2000; Stephenson & Price, 2006; Stone et al., 2009). However, carrying out lengthy assessments may be impractical for emergency personnel, and doing so could disrupt patient flow and contribute to existing ED challenges such as overcrowding.
Brief clinical screening may be an effective alternative to lengthy assessments in rapidly identifying potential somatic presentations before the initiation of excessive diagnostic testing. To our knowledge, no screening tool has been specifically designed, modified, or validated for pediatric ED use. To address this need, we developed a standardized approach to identifying and managing somatization in pediatric acute care, drawing from best practices, and expertise in mental health care (Garralda & Rask, 2015; Ibeziako et al., 2019; Malas et al., 2017). The current study describes this approach and evaluates its utility and feasibility for universal screening and psychoeducational referral in a pediatric ED.
Materials and methods
Study design, setting, and population
Between June and September 2018, we conducted a cross-sectional study at a quaternary-referral ED where over 50,000 visits occur yearly. We included all patients aged 5 to 16 years. We excluded patients and families unable to communicate in English or identified as requiring critical care intervention upon arrival (e.g. ventilation/ airway/hemodynamic support). Participants were recruited over 18 randomly selected study shifts, stratified by day (e.g. weekdays/weekends) and time (e.g. 9 am–5 pm/3 pm–11 pm). This study was approved our institution’s behavioral research ethics board.
Objectives and outcome measures
The primary objective of the study was to estimate the clinical utility of universal screening for somatization in the pediatric ED. Utility was measured as the proportion of patients screening positive for somatization on a short, standardized ED clinician-completed questionnaire. Our secondary objective was to measure the feasibility of our approach to identify, introduce, and follow up with somatization in the pediatric ED. First, an ED clinician completed a brief somatization screening tool. The ED clinician then used a script to help introduce the mind-body connection to positively screened patients and their families and invited them to meet a study psychiatrist to learn more. Those that met the study psychiatrist were offered additional assessment, to further corroborate likelihood of somatization affecting the patient. These families were also invited to a psychoeducational follow-up session. We measured feasibility as (1) the proportion of positive screens who agreed to meet the study psychiatrist to learn about the mind-body connection, (2) the proportion who then consented to further psychiatric assessment, (3) among consenting positive screens, the proportion the psychiatrist supported as likely involving a somatization component (agreed with screening results), and invited to psychoeducational follow-up, and (4) the proportion who attended follow-up. We recorded age, gender, symptoms, triage acuity, and ED investigations and management plan of consented participants. The Research Electronic Data Capture (REDCap) platform was used to store study data.
Study procedures
Intervention approach
We developed a standardized approach to detect and introduce somatization in the ED, which presents somatization as a potential diagnosis, consistent with pediatric liaison psychiatry settings (Ibeziako et al., 2019). Components of this approach include:
Screening tool: A less than 1 minute, five-item, clinician-reported questionnaire to determine if the patient’s presentation may have a somatization component (see Supplemental Material 1). The tool consists of probing questions pertaining to factors associated with somatization. After completing these questions, the ED clinician is asked to use their clinical judgment in answering the following question: ‘Do you suspect that your patient’s presentation is linked to somatization?’. An answer of ‘yes’ or ‘maybe’ constitutes a positive screen.
ED clinician script: A 2-5-minute, guiding prompt for ED clinicians to introduce families to the ‘mind-body connection’ (Supplemental Material 2).
Support for positive somatization screen: A 15-minute assessment in the ED by a psychiatrist to determine the likelihood that somatization contributes to the patient’s presentation and to solicit their interest in attending a psychoeducational session. Psychiatric interviews consist of providing patients examples of the mind-body connection and exploring their symptoms (e.g. gauging impact on enjoyable activities/function, exacerbating/relieving factors, patient journey, and understanding potential etiologies).
Follow-up session: A 90-minute post-ED visit group psychoeducational session for parents to attend without their child, facilitated by psychiatrists and mental health colleagues to provide additional information about the mind-body connection and available mental health services.
Screening tool development
Our tool development process involved (1) extensive literature review and initial item generation, (2) clinical expert feedback, (3) patient feedback, consistent with the PROMIS® Instrument Development and Validation Scientific Standard.(PROMIS Cooperative Group, 2013) In stage one, the study team, composed of mental health and emergency medicine clinicians, collaboratively generated an initial set of items deemed crucial for ED-based pediatric somatization screening, based on clinical expertise, extant literature, and DSM-V criteria (de Gusmão et al., 2014; Ibeziako et al., 2019; Stone et al., 2009). In stage two, we shared our initial item set with the members of the Pediatric Consultation-Liaison Psychiatrists of Canada Group (PCLP) to gauge feedback on item clarity, relevance, and coverage of pediatric somatization. We collected free-form feedback and suggested revisions through multiple iterations of review. Expert review was virtual, remote, and collected over email. The study team reviewed and considered all comments. Expert feedback was sought until no novel content-related comments were made, that had not already been considered. Our team aimed to ensure that tool content was non-judgmental and presented somatization as a possibility rather than a firm diagnosis.
ED visit
During study shifts, screening tools were attached to eligible patients’ ED charts and completed by ED clinicians (pediatric or general emergency physicians). Assisted by a script, the ED clinician provided information about the mind-body connection to positive screen patients and their families and asked if they would agree to meet a study psychiatrist to learn more. If they agreed, families were then introduced to the psychiatrist, who was onsite the entire study shift. The psychiatrist informed the family of the current study and, if written informed consent was obtained, the psychiatrist proceeded with their assessment. If the psychiatrist agreed somatization was a likely contributor to the ED presentation, parents were invited to psychoeducational follow-up and were sent reminders (phone and email) 1 week prior to the scheduled session.
Analytic approach
We report descriptive statistics on study population characteristics and outcomes. Frequencies of categorical variables are reported as percentages with 95% confidence intervals, while continuous variables are reported as means with standard deviation. Based on an a priori sample size calculation, we estimated that 323 completed screens would allow us to detect a positive screen proportion of 30% (a mid-range figure based on reported prevalence of somatization among youth of 10%–50%),(Sergeant, 2019) with 95% confidence and ±5% precision.
Results
ED clinicians completed 344 screening forms, of which 27 (7.8%; 95% CI: 5.2%, 11.2%) screened positive. Among these, 9 (2.6%; 1.2%, 4.9%) were screened as ‘Yes’ and 18 (5.2%; 3.1%, 8.1%) as ‘Maybe’ to whether the ED clinician suspected somatization.
Among the 27 patients who screened positive, 25 (92.6%; 95% CI: 75.7%, 99.1%) verbally consented to meet the study psychiatrist to learn more about the mind-body connection. Eventually, 21 (77.8%; 57.7%, 91.4%) provided written consent to data collection (demographic and visit information) and further study participation including a psychiatry assessment in the ED. For all 21 patients, the psychiatrist corroborated the ED clinician’s decision-making about the likelihood of somatization contributing to the physical symptoms and were invited to a follow-up session. One family dropped out at this stage, the family and study psychiatrist discussed that further psychoeducation may not be beneficial as the somatizing complaint had minimal functional impact. Invited participants were, on average, 12 years old (SD: 2.0), 12 (60%) were female, and 17 (85%) experienced pain as their chief complaint; additional details are reported in Table 1. Only 2 of the 21 invited families (10%) attended follow-up, additional details are offered in Figure 1.
Table 1.
Characteristics of patients confirmed as experiencing a somatizing complaint.
| Patient characteristics | Total (n = 20) a N (%) |
|---|---|
| Age, average (SD) | 12.1 (2.4) |
| Sex, female | 12 (60) |
| Triaged acuity b | |
| Emergent | 2 (13.3) |
| Urgent | 7 (35.3) |
| Less urgent | 11 (48.0) |
| Non-urgent | − |
| Assessment time c | |
| Day shift | 8 (40.0) |
| Night shift | 12 (60.0) |
| Assessment day | |
| Weekday | 18 (90.0) |
| Weekend | 2 (10.0) |
| Chief complaint | |
| Pain | 17 (85.0) |
| Other | 3 (5.0) |
| Affected body system d | |
| Gastrointestinal | 11 (55.0) |
| Neurological | 4 (20.0) |
| Musculoskeletal | 4 (20.0) |
| Other e | 6 (30.0) |
| ED investigations f | |
| Review past investigations | 6 (30.0) |
| Order analgesia | 6 (30.0) |
| Order one new test | 7 (35.0) |
| Order two or more new tests | 3 (15.0) |
| ED discharge diagnosis g | |
| Gastrointestinal | 8 (40.0) |
| Musculoskeletal | 5 (25.0) |
| Not yet diagnosed | 7 (35.0) |
| ED discharge planning h | |
| Prescription of medication | 14 (70.0) |
| Physician follow-up | 12 (60.0) |
| Mental health support | 3 (15.0) |
Demographic could not be collected for one confirmed somatizing patient as they refused further study after the parent and study psychiatrist both agreed psychoeducation follow-up would not be helpful.
Based on the Canadian Triage Acuity Scale.
Day is defined as assessments taking place between 08:00 and 15:59 and night as those done between 16:00 and 23:59
Total section percentage exceeds 100% as youth could have had more than one affected system.
Integumentary system-related, patient presented for suture removal.
The total section percentage exceeds 100% as clinicians could have made multiple investigations per youth
Gastrointestinal diagnoses included abdominal pain and constipation, musculoskeletal diagnoses included sprains and musculoskeletal chest pains. Not yet diagnosed indicated early or inconclusive diagnostic formulation.
The total section percentage exceeds 100% as clinicians could have made multiple discharge instructions per youth. Mental health support included ED clinicians referencing the mind-body connection or suggesting psychiatric input.
Figure 1.
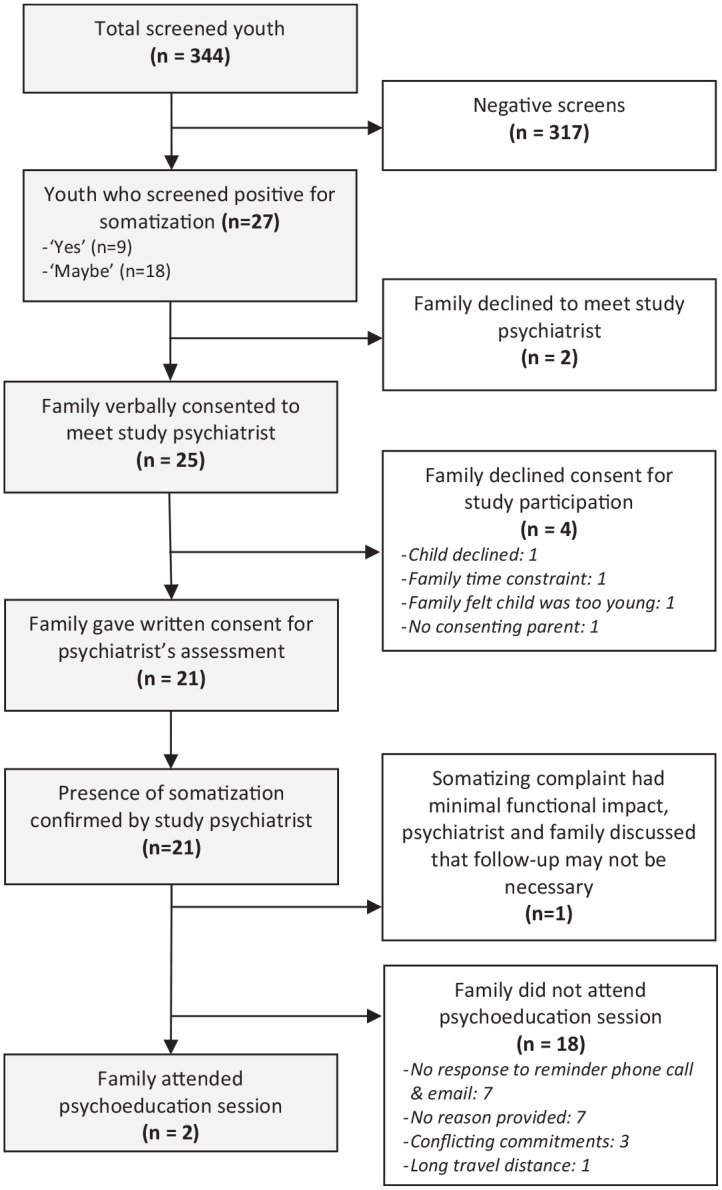
Participant flow from screening through to the psychoeducation follow-up session.
Discussion
Our study found that 7.8% of screened pediatric ED presentations likely involved a somatization component, a majority of whom (93%) agreed to further exploring the mind-body connection with a psychiatrist, with 78% consenting to full study participation. The psychiatrist corroborated the likelihood of somatization in 100% of cases willing to be assessed, producing no false positives. However, only two families attended the group follow-up session.
The prevalence of pediatric somatization in the ED has previously only been measured among youth with pain-related complaints. Cozzi et al reported 22% of the patients experienced non-organic, non-post-trauma-related pain (somatizing pain), of which 8.6% met strict somatic symptom disorder criteria and 13.4% were broadly classified with functional pain (Cozzi et al., 2017). These previous figures are higher than what we observe in the current study, but likely overestimate the ED’s somatization prevalence compared to the general ED-visiting pediatric population, as pain is the most commonly seen symptom of somatization (Dworkin, 1994; Tsai, 2010). Additionally, we observed non-pain-related somatizing complaints (see Table 1) that would have otherwise been missed, supporting that ED screening efforts would benefit from a universal approach (Hatcher & Arroll, 2008). Overall, we found ED-based universal screening may be useful in identifying a considerable proportion of visits with some degree of somatization. An estimated 1.9% to 5.0% of all Canadian pediatric ED visits are made for identified mental health concerns (Canadian Institute for Health Information, 2015; Mapelli et al., 2015). Comparably, close to 8% of our study population screened positive and 6% were corroborated by the psychiatrist as likely having a component of somatization to their ED presentation. Indeed, these figures suggest a substantial proportion of potentially hidden mental health-related concerns in the ED, that without timely screening may go unidentified or misattributed, putting patients at risk for iatrogenic harm from unnecessary testing procedures (Hatcher & Arroll, 2008).
Somatizing patients, compared to those with non-somatizing complaints, are more likely to seek emotional support from their health provider and often offer clinicians cues for greater explanation of their symptoms (Ring et al., 2005; Salmon et al., 2005). In line with the literature, when ED clinician used a non-dualistic script to introduce the mind-body connection, most families (93%) agreed to meet an onsite psychiatrist during their ED visit, and most were willing to be more closely assessed by a psychiatrist (78%). The immediate nature of the ED clinician’s invitation may explain the high follow-through we observed. Consistent with our findings, a direct and seamless approach to somatization intervention is supported by existing clinical recommendation and work done in primary care settings (Abbass, 2005; Abbass et al., 2009; Cozzi et al., 2021). Our findings support the potential for cross-disciplinary collaboration between emergency and consultation psychiatry teams, in somatization identification and psychoeducation. Simultaneous involvement of both teams may help avoid unnecessary testing seen with outdated exclusionary approaches to diagnosing somatization. Ongoing communication across specialities also helps dismantle illusions of a mind-body duality, which may prevent delayed clinical intervention and facilitate the comprehensive and integrative management indicated for somatizing patients (Ibeziako et al., 2019; Jenkins & Smart, 2020). Indeed, our own intervention approach and study procedures benefited greatly from informal feedback received from ED clinicians through ongoing engagement (e.g. conversations, shadowing, somatization teaching sessions).
The initiation of ED-based intervention following screening has shown success, with care models like SBIRT for substance use disorders demonstrating treatment uptake during the ED visit, and reduced consumption and substance-related injury at follow-up (Agerwala & McCance-Katz, 2012; Bernstein & D’Onofrio, 2017; Woolard et al., 2011). However, post-ED visit resource engagement for ED identified mental health concerns is typically low (Dobscha et al., 1999; Grupp-Phelan et al., 2007; Solomon & Gordon, 1988). Grupp-Phelan et al. saw low family follow through with treatment, even after controlling for known service barriers such as care of provisions (appointments were made for patients) and finances (payment was not required) (Grupp-Phelan et al., 2007). The authors speculated that having a seasoned mental health provider (compared to a research assistant) introduce and advise families on follow-up treatment may increase accessing of treatment. However, we report similarly low engagement, despite having a study psychiatrist, suggesting that families may indeed experience scheduling or transportation-related challenges (Owens et al., 2002), in attending onsite psychoeducation. Somatic symptoms can also spontaneously resolve (Hurwitz, 2004), which could also explain our low follow-up rate, as patients could potentially no longer have been impacted by somatization after their ED visit.
Compared to the ED-based intervention components, which were individualized and occurred in a somewhat personalized clinical setting, psychoeducational follow-up was group-based. Families may have perceived the session would be more generic and would not specifically target their personal concerns. In mental health settings, a significant amount of rapport building, and assessment is often required to bridge somatizing patients to appropriate care (Newlove et al., 2016). The first line of care is seldom group-based, as families may be sensitive to stigma and social judgment, particularly in the early stages of their clinical journey, which may explain our low follow-up engagement (Looper & Kirmayer, 2004). Further studies would benefit from qualitative methodologies. Working with somatizing youth and families who have already navigated care systems, may support the development of more patient-centered (e.g. accessible, trauma-informed) strategies to carrying out post-ED psychoeducation.
Limitations of the current study include our lack of ED visit data on negative screens; therefore, we cannot assess for any systematic differences between youth with or without suspected somatization. Our 7.8% positive screen rate may be a conservative estimate, as we excluded non-English speakers and low English language proficiency is a significant risk factor for somatization across immigrant communities (Lanzara et al., 2019). It was not feasible for our study psychiatrist to assess all negative cases; therefore, we do not have information on false negatives. Without the study psychiatrist’s input on negative screens, we cannot comment on sensitivity/specificity and the tool’s negative predictive value. However, we did note a high predictive value (no false positives), this is particularly notable given the relatively low prevalence of somatization-related complaints reported in pediatric acute care, compared to other health settings (Cozzi et al., 2017; Virk et al., 2020). Indeed, further evaluation of tool predictive performance is necessary to better understand its usefulness in clinical practice.
While our tool development procedures were limited to establishing face and content validity among health providers, further research is necessary to quantitatively evaluate the screening tool’s psychometric properties, to ensure accurate and reliable clinical application. We recognize that while the current study focuses on specific components of clinical utility and feasibility, these are indeed broad, multifaceted constructs involving psychometric properties, screening impact on clinical outcomes, cost-effectiveness, and acceptability among patients and clinicians (Smart, 2006). A comprehensive evaluation of ED-based somatization screening interventions across these dimensions will allow us to better gauge intervention viability and implementation potential.
Universal screening by ED clinician identified a considerable proportion of varied presentations with a somatization component. However, introduction of a downstream psychoeducation intervention in the ED had poor uptake. Efforts to implement somatization screening will require further consideration and evaluation of interventions that can enable patient engagement with treatment and ensure somatic symptoms are addressed.
Supplemental Material
Supplemental material, sj-pdf-1-ccp-10.1177_13591045211017619 for The utility of universal screening for somatization in a pediatric emergency department: A prospective evaluation by Punit Virk, Jacob Ellis, Amrit Dhariwal, Andrea Chapman and Quynh Doan in Clinical Child Psychology and Psychiatry
Acknowledgments
The study co-authors would like to gratefully acknowledge the contributions of Dr. Elizabeth Stanford, Dr. Katelynn Boerner, Dr. Theresa Newlove and the Pediatric Consultation-Liaison Psychiatrists of Canada Group (PCLP) to the development of the study components and design. We would also like to thank Mr. Andy Liu, Mr. Bohan Hans Yang, Ms. Heather Burt, and Dr. David Chapman for their thoughtful and constructive feedback on this manuscript.
Author biographies
Punit Virk, MSc, is doctoral candidate at the School of Population and Public Health at the University of British Columbia. His research focuses on preventative and population-level approaches to improving the mental health and well-being of youth and young adults in clinical and community-based settings.
Jacob Ellis, MBBS MRCPsych, is a Consultant Child and Adolescent Liaison Psychiatrist at University College London Hospitals Foundation Trust. He completed a one year clinical and research fellowship in Paediatric Liaison Psychiatry with a focus on somatization at British Columbia Children’s Hospital during the authorship of this article. His clinical and research interests include the assessment and management of somatic disorders and PTSD.
Amrit Dhariwal, PhD RPsych, is a clinical researcher and practicing psychologist. By relying on patient narratives and longitudinal outcome trajectories, she is interested in learning how to optimize family-based treatments in the care of children affected by somatic symptoms.
Andrea Chapman, MD FRCPC, is a Clinical Professor in Psychiatry at University of British Columbia. She is the director of the consultation-liaison service at BC Children’s Hospital. Dr. Chapman’s clinical and research interests focus on pediatric somatization.
Quynh Doan, MDCM MHSc PhD FRCPC, is an Associate Professor in the Department of Pediatrics at the University of British Columbia and is the Director of Clinical Research at the BC Children’s Hospital Research Institute. She is a clinician scientist in health services research with a program of research focusing on patterns of healthcare use, health services access, and high value care delivery.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Study operations were supported through funding from the Children’s Hospital Emergency Physician Associates
ORCID iD: Punit Virk  https://orcid.org/0000-0003-4589-1911
https://orcid.org/0000-0003-4589-1911
Supplemental material: Supplemental material for this article is available online.
References
- Abbass A. (2005). Somatization: Diagnosing it sooner through emotion-focused interviewing. The Journal of Family Practice, 54(3), 231–239, 243. [PubMed] [Google Scholar]
- Abbass A., Campbell S., Magee K., Tarzwell R. (2009). Intensive short-term dynamic psychotherapy to reduce rates of emergency department return visits for patients with medically unexplained symptoms: Preliminary evidence from a pre–post intervention study. CJEM, 11(6), 529–534. 10.1017/S1481803500011799 [DOI] [PubMed] [Google Scholar]
- Agerwala S. M., McCance-Katz E. F. (2012). Integrating Screening, Brief Intervention, and Referral to Treatment (SBIRT) into clinical practice settings: A brief review. Journal of Psychoactive Drugs, 44(4), 307–317. 10.1001/archinternmed.2012.950.Large-Scale [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barsky A. J., Borus J. F. (1999). Functional somatic syndromes. Annals Of Internal Medicine, 130(11), 910–921. https://doi.org/26/0003-4819-130-11-199906010-00016 [DOI] [PubMed] [Google Scholar]
- Beck J. E. (2008). A developmental perspective on functional somatic symptoms. Journal of Pediatric Psychology, 33(5), 547–562. 10.1093/jpepsy/jsm113 [DOI] [PubMed] [Google Scholar]
- Bernstein S. L., D’Onofrio G. (2017). Screening, treatment initiation, and referral for substance use disorders. Addiction Science and Clinical Practice, 12(1), 10–13. 10.1186/s13722-017-0083-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campo J. V., Fritsch S. L. (1994). Somatization in children and adolescents. Journal of the American Academy of Child & Adolescent Psychiatry, 33(9), 1223–1235. 10.1097/00004583-199411000-00003 [DOI] [PubMed] [Google Scholar]
- Canadian Institute for Health Information. (2015). Care for Children and Youth With Mental Disorders (Issue May). https://secure.cihi.ca/free_products/CIHI CYMH Final for pubs_EN_web.pdf
- Cozzi G., Lucarelli A., Borrometi F., Corsini I., Passone E., Pusceddu S., Morabito G., Barbi E., Benini F. (2021). How to recognize and manage psychosomatic pain in the pediatric emergency department. Italian Journal of Pediatrics, 47(1), 74. 10.1186/s13052-021-01029-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cozzi G., Minute M., Skabar A., Pirrone A., Jaber M., Neri E., Montico M., Ventura A., Barbi E. (2017). Somatic symptom disorder was common in children and adolescents attending an emergency department complaining of pain. Acta Paediatrica, International Journal of Paediatrics, 106(4), 586–593. 10.1111/apa.13741 [DOI] [PubMed] [Google Scholar]
- de Gusmão C. M., Guerriero R. M., Bernson-Leung M. E., Pier D., Ibeziako P. I., Bujoreanu S., Maski K. P., Urion D. K., Waugh J. L. (2014). Functional neurological symptom disorders in a pediatric emergency room: Diagnostic accuracy, features, and outcome. Pediatric Neurology, 51(2), 233–238. 10.1016/j.pediatrneurol.2014.04.009 [DOI] [PubMed] [Google Scholar]
- Dobscha S. K., Delucchi K., Young M. L. (1999). Adherence with referrals for outpatient follow-up from a VA psychiatric emergency room. Community Mental Health Journal, 35(5), 451–458. 10.1023/A:1018786512676 [DOI] [PubMed] [Google Scholar]
- Dworetzky B. A., Weisholtz D. S., Perez D. L., Baslet G. (2015). A clinically oriented perspective on psychogenic nonepileptic seizure-related emergencies. Clinical EEG and Neuroscience, 46, 26–33. 10.1177/1550059414566880 [DOI] [PubMed] [Google Scholar]
- Dworkin S. F. (1994). Somatization, distress and chronic pain. Quality of Life Research : An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 3(1), 77–83. 10.1007/bf00433380 [DOI] [PubMed] [Google Scholar]
- Furness P., Glazebrook C., Tay J., Abbas K., Slaveska-Hollis K. (2009). Medically unexplained physical symptoms in children: Exploring hospital staff perceptions. Clinical Child Psychology and Psychiatry, 14(4), 575–587. 10.1177/1359104509338437 [DOI] [PubMed] [Google Scholar]
- Garralda M. E., Rask C. U. (2015). CHAPTER 72 Somatoform and related disorders (pp. 1035–1054). [Google Scholar]
- Gelauff J., Stone J., Edwards M., Carson A. (2014). The prognosis of functional (psychogenic) motor symptoms: A systematic review. Journal of Neurology, Neurosurgery & Psychiatry, 85(2), 220–226. 10.1136/jnnp-2013-305321 [DOI] [PubMed] [Google Scholar]
- Grupp-Phelan J., Delgado S. V., Kelleher K. J. (2007). Failure of psychiatric referrals from the pediatric emergency department. BMC Emergency Medicine, 7(1), 12. 10.1186/1471-227X-7-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatcher S., Arroll B. (2008). Assessment and management of medically unexplained symptoms. BMJ (Clinical Research Ed.), 336(7653), 1124–1128. 10.1136/bmj.39554.592014.BE [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurwitz T. A. (2004). Somatization and conversion disorder. Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie, 49(3), 172–178. 10.1177/070674370404900304 [DOI] [PubMed] [Google Scholar]
- Ibeziako P., Brahmbhatt K., Chapman A., De Souza C., Giles L., Gooden S., Latif F., Malas N., Namerow L., Russell R., Steinbuchel P., Pao M., Plioplys S. (2019). Developing a clinical pathway for somatic symptom and related disorders in pediatric hospital settings. Hospital Pediatrics, 9(3), 147–155. 10.1542/hpeds.2018-0205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkins W., Smart K. (2020). Somatization in acute care pediatrics: Respecting the mind–body connection. Clinical Child Psychology and Psychiatry, 25(3), 604–609. 10.1177/1359104520905065 [DOI] [PubMed] [Google Scholar]
- LaFrance W. C., Benbadis S. R. (2006). Avoiding the costs of unrecognized psychological nonepileptic seizures. Neurology, 66(11), 1620–1621. 10.1212/01.wnl.0000224953.94807.be [DOI] [PubMed] [Google Scholar]
- Lanzara R., Scipioni M., Conti C. (2019). A clinical-psychological perspective on somatization among immigrants: A systematic review. Frontiers in Psychology, 9, 2792. https://www.frontiersin.org/article/10.3389/fpsyg.2018.02792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieb R., Pfister H., Mastaler M., Wittchen H.-U. (2000). Somatoform syndromes and disordersin a representative population sample of adolescents and young adults: Prevalence, comorbidity and impairments. Acta Psychiatrica Scandinavica, 101(3), 194–208. 10.1034/j.1600-0447.2000.101003194.x [DOI] [PubMed] [Google Scholar]
- Lipowski Z. J. (1988). Somatization: The concept and its clinical application. The American Journal of Psychiatry, 145(11), 1358–1368. 10.1176/ajp.145.11.1358 [DOI] [PubMed] [Google Scholar]
- Looper K. J., Kirmayer L. J. (2004). Perceived stigma in functional somatic syndromes and comparable medical conditions. Journal of Psychosomatic Research, 57(4), 373–378. 10.1016/j.jpsychores.2004.03.005 [DOI] [PubMed] [Google Scholar]
- Malas N., Ortiz-Aguayo R., Giles L., Ibeziako P. (2017). Pediatric somatic symptom disorders. Current Psychiatry Reports, 19(2), 11. 10.1007/s11920-017-0760-3 [DOI] [PubMed] [Google Scholar]
- Mapelli E., Black T., Doan Q. (2015). Trends in pediatric emergency department utilization for mental health-related visits. The Journal of Pediatrics, 167(4), 905–910. 10.1016/j.jpeds.2015.07.004 [DOI] [PubMed] [Google Scholar]
- Mayou R. A, Bass C., Hart G., Tyndel S., Bryant B. (2000). Can clinical assessment of chest pain be made more therapeutic? QJM : Monthly Journal of the Association of Physicians, 93(1460-2725 SB-IM JC-B4V), 805–811. [DOI] [PubMed] [Google Scholar]
- Newlove T., Stanford E., Chapman A., Dhariwal A. (2016). Pediatric somatization: Professional handbook [Internet]. Vancouver, BC. Retrieved from https://www.macpeds.com/documents/PediatricSomatizationProfessionalHandbook_Aug2016.pdf (accessed 11 May 2021)
- Offord D. R., Boyle M. H., Szatmari P., Rae-grant N. I., Links P. S., Cadman D. T., Byles J. A, Crawford J. W., Blum H. M., Byrne C., Thomas H., Woodward C. A. (1987). Ontario child health study: I. Methodology. Archives of General Psychiatry, 44, 832–836. [DOI] [PubMed] [Google Scholar]
- Owens P. L., Hoagwood K., Horowitz S., Leaf P., Poduska J. M., Kellam S. G., Ialongo N. S. (2002). Barriers to children’s mental health services. Journal of the American Academy of Child & Adolescent Psychiatry, 41(6), 731–738. 10.1097/00004583-200206000-00013 [DOI] [PubMed] [Google Scholar]
- PROMIS Cooperative Group. (2013). PROMIS® instrument development and validation scientific standards version 2.0 (Issue May). http://www.nihpromis.org/Documents/PROMISStandards_Vers2.0_Final.pdf?AspxAutoDetectCookieSupport=1
- Ring A., Dowrick C. F., Humphris G. M., Davies J., Salmon P. (2005). The somatising effect of clinical consultation: What patients and doctors say and do not say when patients present medically unexplained physical symptoms. Social Science and Medicine, 61(7), 1505–1515. 10.1016/j.socscimed.2005.03.014 [DOI] [PubMed] [Google Scholar]
- Salmon P., Ring A., Dowrick C. F., Humphris G. M. (2005). What do general practice patients want when they present medically unexplained symptoms, and why do their doctors feel pressurized? Journal of Psychosomatic Research, 59(4), 255–260. 10.1016/j.jpsychores.2005.03.004 [DOI] [PubMed] [Google Scholar]
- Saunders N. R., Gandhi S., Chen S., Vigod S., Fung K., De Souza C., Saab H., Kurdyak P. (2020). Health care use and costs of children, adolescents, and young adults with somatic symptom and related disorders. JAMA Network Open, 3(7), e2011295. 10.1001/jamanetworkopen.2020.11295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sergeant E. (2019). Epitools epidemiological calculators. Ausvet Pty Ltd. [Google Scholar]
- Sills M. R., Bland S. D. S. D. (2002). Summary statistics for pediatric psychiatric visits to US emergency departments, 1993–1999. Pediatrics, 110(4), e40. http://www.ncbi.nlm.nih.gov/pubmed/12359813 [DOI] [PubMed] [Google Scholar]
- Smart A. (2006). A multi-dimensional model of clinical utility. International Journal for Quality in Health Care, 18(5), 377–382. 10.1093/intqhc/mzl034 [DOI] [PubMed] [Google Scholar]
- Solomon P., Gordon B. (1988). Follow-up of Outpatient Referrals From A Psychiatric Emergency Room. Social Work in Health Care, 13(1), 57–67. 10.1300/J010v13n01_05 [DOI] [PubMed] [Google Scholar]
- Stephenson D. T., Price J. R. (2006). Medically unexplained physical symptoms in emergency medicine. Emergency Medicine Journal, 23(8), 595–600. 10.1136/emj.2005.032854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone J., Carson A., Duncan R., Coleman R., Roberts R., Warlow C., Hibberd C., Murray G., Cull R., Pelosi A., Cavanagh J., Matthews K., Goldbeck R., Smyth R., Walker J., MacMahon A. D., Sharpe M. (2009). Symptoms “unexplained by organic disease” in 1144 new neurology out-patients: How often does the diagnosis change at follow-up? Brain, 132(10), 2878–2888. 10.1093/brain/awp220 [DOI] [PubMed] [Google Scholar]
- Tsai C. H. (2010). Factor analysis of the clustering of common somatic symptoms: A preliminary study. BMC Health Services Research, 10(1), 1–8. 10.1186/1472-6963-10-160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Virk P., Vo D. X., Ellis J., Doan Q. (2020). Pediatric somatization in the emergency department: Assessing missed opportunities for early management. CJEM, 22(3), 331–337. 10.1017/cem.2019.477 [DOI] [PubMed] [Google Scholar]
- Woolard R., Cherpitel C., Thompson K. (2011). Brief intervention for emergency department patients with alcohol misuse: Implications for current practice. Alcoholism Treatment Quarterly, 29(2), 146–157. 10.1080/07347324.2011.557978 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-ccp-10.1177_13591045211017619 for The utility of universal screening for somatization in a pediatric emergency department: A prospective evaluation by Punit Virk, Jacob Ellis, Amrit Dhariwal, Andrea Chapman and Quynh Doan in Clinical Child Psychology and Psychiatry


