Abstract
Objectives:
Post-operative pain is a form of acute pain following surgical intervention. And it is due to skin incision, tissue dissection, manipulation, and traction during the surgical procedure. The magnitude may reach up to 85.5% globally. Age, gender, duration of surgery, and length of skin incision were the common factors for post-operative pain. This study aims to assess the magnitude and associated factors of post-operative pain among surgical patients.
Methods:
Institutional-based cross-sectional study design was used. The study was conducted on a total of 159 surgical patients aged 8 years and above. The data were collected using chart review and recording the status of post-operative pain by the result of the Numeric Rating Scale at 1, 6, 12, 24, and 72 h of the post-operative period. Descriptive statistics, bivariate, and multivariable logistic regression were used. An adjusted odds ratio with a 95% confidence interval was used to determine the association. A p-value of less than 0.05 was used to declare statistical significance.
Results:
The majority (58.5%) of the study participants were females. The percentage of moderate to severe post-operative pain (Numeric Rating Scale: 4 and above) was between 37.7% within 1 h and 76.7% at 6 h of post-operative period. On multivariable logistic regression being female gender, preoperative pain and large skin incision were significantly associated with post-operative pain.
Conclusions:
Post-operative pain is still high which needs the attention of health professionals working on surgical patients and considering factors associated with post-operative pain.
Keywords: Associated factor, Ethiopia, post-operative pain
Introduction
Post-operative pain (POP) is a form of acute pain following surgical intervention. And it is due to skin incision, tissue dissection, manipulation, and traction during the surgical procedure. It is also one of the complications of surgery and anesthesia intervention. Despite improved understanding of pain mechanisms, increased awareness of the prevalence of postsurgical pain, advances in pain-management styles, and other measures aimed at improving pain-related outcomes in recent decades, inadequately managed POP continues to be a widespread, unresolved health-care problem and it reaches 85%.1 And in different hours of the post-operative period at 30 min much higher and reduced in 24 h and 48 h of operation.2
There are identified factors for POP like the presence of preoperative pain, preoperative anxiety, type of surgery, and also younger age also associated with the presence of acute POP.3 Access to analgesic drugs and health professionals’ knowledge on POP also had an impact on POP.4
Inadequate management of POP leads to prolong the time of recovery and also decrease the quality of surgical patients’ life in the post-operative period.5 POP assessment tool and pain-management protocol were distributed in Hospitals but still, POP was an unmet problem so it needs intervention to improve the pain management. This study aimed to assess the magnitude of POP as well as the associated factors of POP among surgical patients.
Method and materials
An institutional-based cross-sectional study was conducted at Debre Tabor compressive specialized Hospital. Debre Tabor is a town located in the South Gondar Zone of the Amhara Region of Ethiopia which is 667 km far away from Addis Ababa, the capital city of Ethiopia. Debre Tabor General Hospital is one of the eight governmental Hospitals in the zone and under the Administration of the Amhara Health Bureau. The Hospitals provide medical, surgical, and diagnostic services for patients from Debre Tabor town and other woredas catchment populations. Debre Tabor compressive specialized hospital provides surgical service for about 2880 patients per year (yearly report of the hospital). This hospital has a protocol of POP assessment and management and is documented on the surgical patient chart. The pain assessment is done for the surgical patient every 4 h for the first 72 h of the surgical patient. Based on the pain assessment and request of the patient they took analgesia. The choice of analgesia and dose of the drugs depend on the patients’ age, weight, and also the preference of the professional. The researcher and data collector had no role in analgesia drug selection and dose only record the POP status of the patients based on the record on the chart. The Numeric Rating Scale (NRS) is a valid pain intensity assessment tool and used to rate a patient his or her pain from 0 to 10 with the understanding that 0 is equal to no pain and 10 equal to the worst possible pain. NRS is reliable in a rural population irrespective of literacy6 status and used for age 8 and above years of surgical patients in this hospital and the pain assessment scale was recorded on each surgical patient chart. POP was managed based on the professionals’ decision and availability of analgesics drugs in the hospital, but there was a guideline that patients who had NRS more than 4 value should be got analgesics. A study was conducted from September 2018 to November 2018. In this study, we used a convenient sampling technique and we include all surgical Patients’ charts with the age of 8 years and above, and ASA class, I and II during the study period were included.
The questioner prepared by reviewing different literature to include all important variables and we had done a pretest before the actual data collection at another nearby hospital also we perform Cronbach’s alpha test which was more than 70%. The data were collected from the surgical patient chart and recorded their data from the chart including pain assessment and pain management. Surgical patient charts without complete POP assessment status and pain-management data were excluded from the study. After getting ethical approval from Debre Tabor University’s ethical Review committee and the approval number was R/P/586/2018, permission was obtained from Debre Tabor general hospital. The data were collected from all surgical patients during the study period after taking written informed consent from each patient surgical patient at or after 72 h of their post-operative period. During the surgery, patients use analgesia techniques based on the assigned anesthetist at the operation room, and their post-operative pain management at post-anesthesia care unit (PACU) and their respective ward depend on the decision of the assigned professionals (mostly nurses). Trained data collectors reviewed the patient chart, and record their POP status at 1, 6, 12, 24, and 72 h of the post-operative period.
Statistical analysis
Data were entered into EPI info version 7.1 then transferred to SPSS version 21 computer program for cleaning and analysis purposes. Descriptive statistics were summarized by tables and figures. Logistic regression is used for the analysis technique to see the association of the independent variable and dependent variable. Variable with a p-value of 0.25 at bivariate analysis entered into multivariate analysis and p-value less than 0.05 in multivariate analysis was used to declare statistical significance.
Operational definitions
Post-operative pain: It is pain after the operation until 72 h of the post-operative period. In this study, a patient who has an NRS of 4 and above is classified as having pain.
Numeric rating scale (NRS): A type of pain assessment tool and scale from 0 to 10 (0 = no pain and 10 = worst pain) and instruct the patient to locate their pain status and commonly used for patients above 8 years. Based on NRS pain is categorized into mild pain (0–3), moderate (4–6) pain, and severe pain (7 and above).
Size of skin incision: It is a break of skin continuity to access the specified pathologic organ or actual site of surgery and which is measured externally in centimeter. In this study, we classified incision size less than 10 cm as small and more than 10 cm as large skin incision.
Results
A total of 159 operated patients have analyzed in this study and the majority of the participants were female 58.5% and orthodox Christian followers with 93.7%. Majority of the participants (156) within the normal range of body mass index (BMI; 18.5–24.5) and the remaining3 patients their BMI less than 18.5. And all are Amhara in ethnicity (Table 1). The majority of the procedures were done under General Anesthesia (Table 2). Most of the surgical patients did not have preoperative pain (52.2%; Table 3). None of the patients took peripheral nerve block, skin infiltration, strong opioid, and epidural analgesia for their POP rather based on their pain complain and assigned professionals they took diclofenac and tramadol. The majority (112/159) of the site of surgery were intra abdominal (Figure 1). From the type of analgesia technique, all post-operative patients took diclofenac and 123 patients took additional tramadol analgesics on their post-operative period and recorded on their chart. The time of analgesia given was dependent on the request of the patient and the professional decision.
Table 1.
Socio-demographic characteristics of the study participant at DTGH from September to December 2018.
| Variables | Frequency (N = 159) | Percentage (%) |
|---|---|---|
| Male | 66 | 41.5 |
| Female | 93 | 58.5 |
| Age | ||
| 8–14 | 12 | 7.5 |
| 15–29 | 63 | 39.6 |
| 30–59 | 65 | 40.9 |
| 60 and above | 19 | 11.9 |
| Educational status | ||
| Unable to read and write | 60 | 37.7 |
| Read and write | 49 | 30.8 |
| College | 33 | 20.8 |
| Above college | 17 | 10.7 |
| Occupation | ||
| Student | 24 | 15.1 |
| Merchants | 10 | 6.3 |
| Farmers | 74 | 46.5 |
| House wife | 26 | 16.4 |
| Civil servant | 21 | 13.2 |
| Others | 4 | 2.5 |
DTGH: Debre Tabor General Hospital.
Table 2.
Perioperative characteristics of the study participants at DTGH from September to December 2018.
| Variables | Frequency (N = 159) | Percentage (%) |
|---|---|---|
| Preoperative anxiety | ||
| Yes | 78 | 49.5 |
| No | 81 | 50.5 |
| Preoperative pain | ||
| Yes | 76 | 47.8 |
| No | 83 | 52.2 |
| Type of anesthesia given | ||
| GA | 88 | 55.3 |
| RA | 71 | 44.7 |
| Length of skin incision in cm | ||
| Less than 5 cm | 31 | 19.5 |
| 5 to less than 10 cm | 89 | 56 |
| 10 cm and above | 39 | 24.5 |
| Duration of surgery in minute | ||
| Less than 30 min | 17 | 10.7 |
| 30 to less than 60 min | 76 | 47.8 |
| 60 to less than 120 min | 52 | 32.7 |
| 120 min and above | 14 | 8.8 |
DTGH: Debre Tabor General Hospital; GA: General Anesthesia; RA: Regional Anesthesia.
Table 3.
Distribution of post-operative pain with patient characteristics of the study participants at DTGH from September to December 2018.
| Variables | NRS (0–3) | NRS (4 and above) | |
|---|---|---|---|
| Sex | Male | 23 | 43 |
| Female | 14 | 79 | |
| Age | Less than 60 | 31 | 109 |
| 60 and above | 6 | 13 | |
| BMI | Less than 18.5 | 0 | 3 |
| 18.5–24.5 | 37 | 119 | |
| I | 19 | 61 | |
| ASA | II | 18 | 61 |
| Preoperative pain | Yes | 22 | 54 |
| No | 15 | 68 | |
| Yes | 21 | 57 | |
| Preoperative anxiety | No | 16 | 65 |
| Type of anesthesia | GA | 20 | 68 |
| RA | 18 | 53 | |
| Site of incision | Abdominal | 25 | 83 |
| other sites | 12 | 39 | |
| Length of incision | Less than 10 cm | 34 | 90 |
| 10 cm above | 3 | 32 | |
| Duration of surgery | Less than 2 h | 35 | 109 |
| 2 h and above | 3 | 12 |
ASA: American Society of Anesthesiology; BMI: body mass index; DTGH: Debre Tabor General Hospital; GA: General Anesthesia; NRS: numeric rating scale; RA: Regional Anesthesia.
Figure 1.
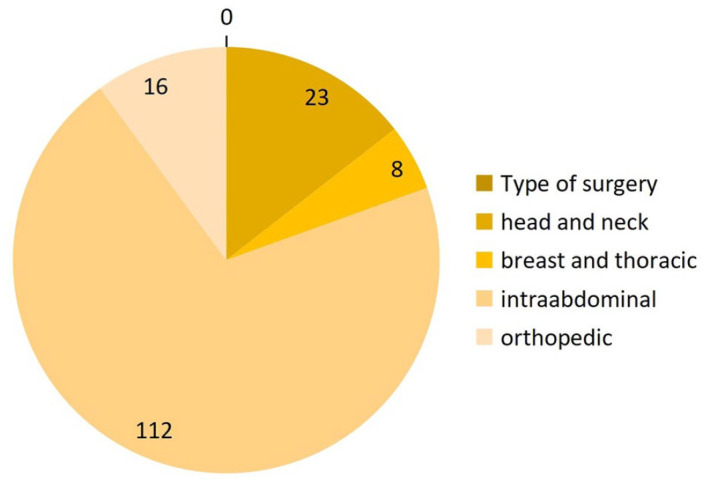
Pie chart showing distribution type of surgery among the study participants during the study period at DTGH September to December 2018.
Post-operative pain assessment
The POP of surgical patients was assessed using a NRS on the post-operative period by attending professional on the time of post-operative period at PACU and surgical ward at 1, 6, 12, 24, and 72 h of the post-operative period and recorded on their chart. In this study, the data collector records the status of pain based on the patient chart record. Patients who had a report of NRS scores 4 and above within 72 h of the post-operative period were considered as having POP. A Patient may have pain once or more times within 72 h of the post-operative period. A large number of patients scored moderate to severe pain at 6 h of their post-operative period (76.7%) whereas a small number of patients scored pain at PACU within 1 h of the post-operative period (37.7%). Generally, the magnitude of post-operative pain was found to be between 37.7% and 76.7% in their post-operative period (Table 4).
Table 4.
Percentage of moderate to severe post-operative pain using NRS in the study participant at DTGH from September to December 2018.
| Pain scale with NRS | At 1 h of POP number (%) | At 6 h of POP | At 12 h POP | At 24 h of POP | At 72 h of POP |
|---|---|---|---|---|---|
| 0 | 39 (24.5) | 15 (9.4) | 22 (13.8) | 20 (12.6) | 20 (12.6) |
| 1–3 | 60 (37.7) | 22 (13.8) | 38 (23.9) | 47 (29.6) | 74 (46.5) |
| 4–6 | 58 (36.5) | 118 (74.2) | 93 (58.5) | 86 (54.1) | 63 (39.6) |
| 7 and above | 2 (1.3) | 4 (2.7) | 6 (3.8) | 6 (3.8) | 2 (1.2) |
ASA: American Society of Anesthesiology; DTGH: Debre Tabor General Hospital; NRS: numeric rating scale; POP: post-operative pain.
On multivariable logistic regression, female gender, having preoperative pain and large skin incision (AOR = 4.57, 95% CI = 1.761–11.89; AOR = 4.592, 95% CI = 1.637–12.884; AOR = 6.108, 95% CI = 1.448–25.778), respectively, associated with POP (Table 5).
Table 5.
Association of factors with post-operative pain at 6 h of the post-operative period in the study participants at DTGH from September to December 2018.
| Variables | Moderate to severe pain | p-value | OR | 95% CI | |
|---|---|---|---|---|---|
| Sex | Male | 43 | 0.002 | 4.57 | 1.761–11.89 |
| Female | 78 | ||||
| ASA | I | 63 | 0.063 | 0.385 | 0.141–1.053 |
| II | 58 | ||||
| Preoperative pain | Yes | 53 | 0.004 | 4.592 | 1.637–12.884 |
| No | 68 | ||||
| Length of incision | <10 cm | 85 | |||
| ⩾10 cm | 36 | 0.014 | 6.108 | 1.448–25.778 | |
| Site of incision | Abdominal | 84 | |||
| Other | 37 | 0.81 | 2.423 | 0.897–6.547 |
CI: confidence interval; DTGH: Debre Tabor General Hospital; OR: odds ratio.
Discussion
In this study, a total of 159 surgical patients participated. The percentage of moderate to severe POP was found to be between 37.7% and 76.7% in their post-operative period within 72 h of operation. The maximum number of patients having pain was at 6 h of the post-operative period, while the minimum was within 1 h of the post-operative period. Even if there are guidelines POP management, development of new technology, availability of potent drugs, the professional numbers as well as variety are increased to manage patients. Still, patients are suffering from pain during post-operative period.
The finding of this study is in line with Arissara Iamaroon et al. who reported the incidence of POP as 75% within 24 h of the post-operative period.7
However, Tania casino et al. and other study showed that less POP incidence with our result.8,9 The differences were due to the timing of the pain assessment and the study area.
In this study, female gender was significantly associated with POP. In agreement with our finding, other studies also showed that the female gender had high pain magnitude and severity than the male.10,11 The pain modulatory effect of sex hormone and pain sensitivity differences among gender was considered as a reason for high pain magnitude among females. But the current finding was not consistent with the finding of casino T et al. which showed that there was no statistically significant difference among gender in pain magnitude as well as pain severity.9
The other factor for POP was a large skin incision. This study was comparable with other studies which showed that large skin incision was associated with the development of severe POP and analgesic consumption also high in patients with large skin incision.12,13 But other studies did not find any association between length of skin incision and POP magnitude.14 This difference might be due to the lack of controlling perioperative pain management and the type of surgery in this study.
In this study, another factor for POP was the presence of preoperative pain. In line with this finding, other studies also concluded that preoperative pain was a significant predictive factor for POP.15,16 Increased pain sensitivity and central sensitization as well as other factors considered as a reason for POP. Patients who underwent surgery with spinal anesthesia were showed less pain score at 1 h of post-operative period than patients are done under general anesthesia but in multivariable analysis’ it was not significant at 6 h of the post-operative period. The reason could be the analgesic effect of spinal anesthesia may last longer than the surgical duration which helps the patient for post-operative pain control.
Conclusion and recommendation: The percentage of moderate to severe POPs is still high which needs the attention of health professionals working on surgical patients by considering factors associated with POP. Other studies like cohort and clinical trial studies were recommended to get better evidence on this topic.
Limitation of the study: This is a single-center study and used a small sample size without randomization, so it is impossible to generalize the result for all post-operative patients. We did not use sample size calculation simply, we collect all surgical patients and it has its limitation. This study also did not control the co-founders due to the study design. The other limitation was the pain-management history and used analgesic dose had not studied which may affect POP.
Supplemental Material
Supplemental material, sj-pdf-1-smo-10.1177_20503121211014730 for The magnitude and associated factors of post-operative pain at Debre Tabor compressive specialized hospital, Debre Tabor Ethiopia, 2018 by Abebe Tiruneh, Tadese Tamire and Simegnew Kibret in SAGE Open Medicine
Acknowledgments
The authors want to also thank Debre Tabor University for giving us ethical clearance during data collection, and the Authorities of Debre Tabor Compressive specialized Hospital for their permission to do the research.
Footnotes
Author contributions: All authors contribute from topic selection, proposal writing, analysis, and manuscript writing.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: This study was ethically approved by Debre Tabor University Ethical review committee and the approval number was R/P/586/2018.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written Informed consent was taken from each study subjects and their parents in the case of pediatrics age less than 18 years old.
ORCID iDs: Abebe Tiruneh  https://orcid.org/0000-0003-4154-3207
https://orcid.org/0000-0003-4154-3207
Tadese Tamire  https://orcid.org/0000-0001-6851-5359
https://orcid.org/0000-0001-6851-5359
Supplemental material: Supplemental material for this article is available online.
References
- 1. Admassu WS, Hailekiros AG, Abdissa ZD. Severity and risk factors of post-operative pain in University of Gondar Hospital, Northeast Ethiopia. J Anesth Clin Res 2016; 7(10): 1–7. [Google Scholar]
- 2. Mwaka G, Thikra S, Mung’ayi V. The prevalence of postoperative pain in the first 48 hours following day surgery at a tertiary hospital in Nairobi. Afr Health Sci 2013; 13(3): 768–776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ip HYV, Abrishami A, Peng PWH, et al. Predictors of postoperative pain and analgesic consumption: a qualitative systematic review. Anesthesiology 2009; 111(3): 657–677. [DOI] [PubMed] [Google Scholar]
- 4. Wurjine TH, Nigussie BG. Knowledge, attitudes and practices of nurses regarding to post-operative pain management at hospitals of Arsi zone, Southeast Ethiopia, 2018. MOJ Womens Heal 2018; 7(5): 130–135. [Google Scholar]
- 5. Manworren RCB, Gordon DB, Montgomery R. CE: managing postoperative pain. Am J Nurs 2018; 118(1): 36–43. [DOI] [PubMed] [Google Scholar]
- 6. Mudgalkar N, Bele SD, Valsangkar S, et al. Utility of numerical and visual analog scales for evaluating the post-operative pain in rural patients. Indian J Anaesth 2012; 56(6): 553–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Iamaroon A, Tangwiwat S, Nivatpumin P, et al. Risk factors for moderate to severe pain during the first 24 hours after laparoscopic bariatric surgery while receiving intravenous patient-controlled analgesia. Anesthesiol Res Pract 2019; 2019: 6593736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rungwattanakit P, Sondtiruk T, Nimmannit A, et al. Perioperative factors associated with severe pain in post-anesthesia care unit after thoracolumbar spine surgery: a retrospective case-control study. Asian Spine J 2019; 13(3): 441–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cursino T, Couceiro DM, Valença MM, et al. Prevalência e Influência do Sexo, Idade e Tipo de Operação na Dor Pós-Operatória [Prevalence and influence of gender, age, and type of surgery on postoperative pain]. Brazilian J Anesthesiol 2009; 59(3): 314–320. [DOI] [PubMed] [Google Scholar]
- 10. Edgley C, Hogg M, De Silva A, et al. Severe acute pain and persistent post-surgical pain in orthopaedic trauma patients: a cohort study. Br J Anaesth 2019; 123(3): 350–359. [DOI] [PubMed] [Google Scholar]
- 11. Singh JA, Gabriel S, Lewallen D. The impact of gender, age, and preoperative pain severity on pain after TKA. Clin Orthop Relat Res 2008; 466(11): 2717–2723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kim KT, Kim YB. Comparison between open procedure and tubular retractor assisted procedure for cervical radiculopathy: results of a randomized controlled study. J Korean Med Sci 2009; 24(4): 649–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Madureira FAV, Manso JEF, Madureira Fo D, et al. Randomized clinical study for assessment of incision characteristics and pain associated with LESS versus laparoscopic cholecystectomy. Surg Endosc 2013; 27(3): 1009–1015. [DOI] [PubMed] [Google Scholar]
- 14. Beirer M, Postl L, Crönlein M, et al. Does a minimal invasive approach reduce anterior chest wall numbness and postoperative pain in plate fixation of clavicle fractures? BMC Musculoskelet Disord 2015; 16: 128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gramke HF, De Rijke JM, Van Kleef M, et al. Predictive factors of postoperative pain after day-case surgery. Clin J Pain 2009; 25(6): 455–460. [DOI] [PubMed] [Google Scholar]
- 16. Hartwig M, Allvin R, Bäckström R, et al. Factors associated with increased experience of postoperative pain after laparoscopic gastric bypass surgery. Obes Surg 2017; 27(7): 1854–1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-smo-10.1177_20503121211014730 for The magnitude and associated factors of post-operative pain at Debre Tabor compressive specialized hospital, Debre Tabor Ethiopia, 2018 by Abebe Tiruneh, Tadese Tamire and Simegnew Kibret in SAGE Open Medicine


