Abstract
Objective
To assess the magnitude of disability and its associated factors among patients with schizophrenia in North West Ethiopia in selected hospitals, 2019.
Design
Multicenter hospital-based cross-sectional study.
Setting
Gondar, Felege Hiwot, and Debre Tabor hospitals.
Participants
We recruit 420 participants for interviews using a systematic random sampling technique.
Measurement
We collect the data by face-to-face interview. Disability was measured using the World Health Organization Disability Assessment Scale 2.0. Coded variables were entered into Epi data V.4.4.2 and exported to SPSS V.24 for analysis. Bivariate and multivariate logistic regressions with OR and 95% CI were employed.
Result
A total of 423 participants were interviewed, with a response rate of 99.3%. The magnitude of disability in this study was 41.7 % (95 %CI: 36.9, 46.4). Current use of alcohol (AOR = 2.47,n95CI; 1.36,4.48), being jobless (AOR = 3.27, 95CI; 1.80, 5.93), had negative symptoms (AOR = 13.05,95CI, 7.58,22.45), had 5 and more years of illness (AOR = 2.75,95CI; 1.29,5.86), and had 5 and more years of untreated psychosis (AOR = 3.78,95CI, 1.85,7.75) were predictors of disability.
Conclusion and recommendation
The magnitude of disability in this study was 41.7 %. Avoidance of alcohol usage, early initiation of treatment, creating job opportunities, and giving special emphasis to patients having negative symptoms is recommended.
Keywords: Mental health, Schizophrenia, Disability
Mental health; Schizophrenia; Disability.
1. Introduction
Schizophrenia is a severe, chronic, and disabling mental illness comprising several discrete clinical features with extensive variation between individuals [1], which places a significant burden not only on the individuals but also on their families and society [2]. Currently, it affects approximately 20–24 million people worldwide [3]. In the global burden of disease study, schizophrenia accounted for 1.1% of the total disability-adjusted life year (DALYs) and 2.8% of Years lived with disability (YLDs) [4].
Disability is one of the consequences of schizophrenia that individuals afflicted with it experience. It is highly prevalent across patients themselves, families, communities, and professionals [5]. According to the World Health Organization report, schizophrenia is the world's fourth leading cause of disability [6]. Disability in schizophrenia interferes with self-care and mental illness, medical care, further worsening physical health to produce a vicious cycle of disability [7], and the level of disability is more in chronic and episodic mental disorders [8].
Despite long years of pharmacological and psychosocial interventions, schizophrenia remains one of the leading causes of disability [9, 10] including poor self-care, inability to manage the tasks of daily living, social withdrawal, poor functioning in affinitive roles, and work incapacity [11]. A recent study comparing the functional disability between schizophrenia and bipolar disorder resulted in greater disability in schizophrenia than bipolar Disorder [12, 13].
A previous study analyzed that various aspects of psychosocial disability occur in schizophrenia such as psychopathological symptoms [14], impairments of basic cognition [14], social cognition [15], emotional experience [16], social functioning [17], vocational functioning [18] and quality of life [19, 20].
Particularly social disability is one of the most crippling aspects of functioning in schizophrenic patients because in a patient with schizophrenia there is a range [14] of deficits in emotion processing, including the ability to accurately perceive emotions, to use emotions to facilitate thinking and decision making and to understand and manage emotions in oneself and others [21]. According to research done in low- and middle-income countries, mental disorders account for 25.3% and 33.5% of all years lived with a disability respectively. People living with mental illness usually suffer from educational and income-generation opportunities and poor social networks within their society. Of all disabilities, severe mental illness is associated with the highest rates of unemployment, rating up to 90%. Despite the widespread availability of medications that suppress psychosis and prevent relapse, most patients with chronic mental illnesses such as schizophrenia remain disabled in different functions in the community [22].
Research done in India among schizophrenic patients, 83% of them found with mild to moderate disability [23]. Another comparative study in Southern India showed that patients on antipsychotics had significantly less disability across all domains of disability, which was rating as 40% of the patients with treatment were disabled in contrast to 71% of the patients not receiving treatment [24].
Likewise, a comparatives study of disability in individuals with bipolar affective disorder and schizophrenia in a sub-Saharan African revealed that 24.93% and 27.02% of patients were disabled respectively. The factors associated with this study were: unemployment status and remittance source of income [13].
Disability in schizophrenia is the main public health problem due to its severity, chronic, and disabling nature. Its impact is not limited to the individual but rather it passes down to the whole family and society. Inability to function in everyday settings is responsible for the huge indirect costs of schizophrenia, which may be as much as three times larger than direct treatment costs for psychotic symptoms.
Early treatment with antipsychotics reduces the severity as well as the occurrence of disability. In the Ethiopian context, prevalence studies of disability in schizophrenia are very scarce. It is, therefore, necessary to assess the magnitude and associated factors of disability in a schizophrenic patient.
Thus, the findings of this will help to plan intervention programs for chronic mentally ill patients.
Therefore, this study aimed to assess the magnitude and associated factors of disability among schizophrenic patients at Debretabor, Felegehiwot, and Gondar general hospital attending psychiatry unit, Amhara North West Ethiopia, 2019.
2. Methods
2.1. Study area and period
An institutional-based cross-sectional study was conducted from January 1 to February 15 2019. The study was conducted at Debre tabor, Felegehiwot, and Gondar hospitals which are Far from 666, 563, and 738 km respectively north of the capital city of Ethiopia. Based on the monthly report of the psychiatry unit there are approximately about 100 at Debretabor, 250 at Felegehiwot, and 280 patients at Gondar hospital. In all the three hospitals outpatient, inpatient, and emergency mental health services for adult and childhood psychiatric problems are being given. Moreover, outpatient services for substance use disorder have been given in the hospitals. Specifically, Debre Tabor comprehensive specialized hospital is now in the process to begin a comprehensive substance rehabilitation center in its full capacity.
2.2. Study participants and sampling
The study participants were recruited by using a systematic random sampling technique.
There were 150, 375 and 420 participants who visited Debre tabor, Felege Hiwot and Gondar hospitals per 1 and half month respectively. To select the study subjects from each hospital; the interval size (k) was calculated using the following formula.
where 67, 168 and 188 were the number of participants interviewed in Debre Tabor, Felege Hiwot and Gondar hospital respectively.
Therefore the interval K was 2 that the participants interviewed every 2 for the three hospitals. and the first participant was determined by lottery method. This recruitment process was done on the registration book of the hospital. To avoid the repeated interview of a single subject, their medical registration number were recorded and checked in the subsequent interviews. Participants aged 18 years and above and having no active psychopathology were included in the study during the data collection period. There were a total of 945 schizophrenic patients who had follow up over 1 and half month and participants who were epileptic and intellectually disabled were excluded (Figure 1).
Figure 1.
Showing sampling procedure for magnitude and associated factors of disability among patients with schizophrenia Amhara, North West, Ethiopia, 2019.
2.3. Sample size determination
The sample size was determined by using a single population proportion formula.
Taking into account the following assumption, the proportion of patients with schizophrenia (p) is 0.5%; (as there was no research done in Ethiopia), the margin of error (α) = 0.05; the level of confidence (95%), 1.96 Z (standard normal distribution), and 10% non-response rate. Accordingly, a representative sample was calculated to be 423.
2.4. Study variables
The dependant variable was disability measured by WHO disability assessment scale 2.0. We measured disability as dichotomous variables (yes/No).
Independent variables included Sociodemographic factors (age, sex, marital status, ethnicity, religion, residence, educational, and occupational status), clinical variables (current medication, number of medication, duration illness, duration of untreated psychosis, positive, and negative), and substance-related factors (alcohol consumption, cigarette smoking, khat chewing).
2.5. Data sources and measurement
Data were collected by face-to-face interviews using a semi-structured questionnaire by four trained mental health professional specialists using the Amharic version of the tool for 1 and half month. The questionnaire was designed in English and translated to Amharic and back to English to maintain its consistency. Data collectors were trained on how to interview participants and explain unclear questions and the purpose of the study. Furthermore, they were made aware of ethical principles, such as confidentiality/anonymity/data management, and securing respondents' informed consent for participation.
Disability was measured using WHODAS 2 which has a 36-item self-report measure with Likert response options ranging from 1 ‘None’ to 5 ‘extremely’ for each item, giving a potential scale score range of 36–180, and disability was explained by the sum of WHODAS 2 items scored above mean. We adapted this instrument from a study conducted in rural Ethiopia [1]. It showed a high internal consistency, reliability, and a strong correlation with a disability diagnosis. We conducted a reliability analysis for data that gave an acceptable score (Cronbach's α = 0.73).
Disability: is any restriction or lack (resulting from an impairment) of ability to perform an activity in the manner or within the range considered normal for an individual in his or her socio-cultural setting [2].
Diagnosis of schizophrenia: was made based on diagnostic statistical manual of American psychiatric association-5 (DSM-5) and their diagnosis were taken from the chart based on their medical registration number.
Disability in schizophrenia: The presence of disability in schizophrenia was explained by the sum of WHODAS 2 items scored above mean.
Substance use history: To examine substance use history, respondents were asked: ‘Have you ever used any substance in the last 3 months or in your lifetime?’ and the responses were yes/no [3].
Positive symptoms: The presence of exaggerated ideas, perceptions, or actions that show the person can't tell what's real from what isn't including hallucination, delusion disorganized speech, grossly disorganized or catatonic behavior.
Negative symptoms: refer to an absence or lack of normal mental function involving thinking, behavior, and perception including lack of pleasure, alogia, a volition affective flattening, apathy, poor rapport, lack of spontaneity.
Positive or negative symptoms were examined by verbal report and physical manifestations during the course of interview as well as reports of behavior by primary care workers or families.
Number of medications: To examine the numbers of mediation that participants were taking: Respondents were asked how many medications you are taking? The responses were one/two or more.
Items on Sociodemographic factors: Items on Sociodemographic factors (age, sex, and ethnicity, religion, and marital status, residence, educational and occupational status) were adopted from a variety of literature.
2.6. Data processing and analysis
All collected data were checked for completeness and consistency and entered into Epi-data V.4.4.2 and then exported to SPSS V.24 for analysis. We computed descriptive, bivariate, and multivariate logistic regression analyses to see the frequency distribution and to test the association between independent and dependent variables, respectively. Factors associated with disability were selected during the bivariate analysis with a p < 0.05 for further analysis in the multivariable logistic regression analysis. In the multivariable logistic regression analysis, variables with p < 0.05 at 95% CI with adjusted OR were considered as statistically significant.
2.7. Ethical consideration
Permission was obtained from the Amhara Health Bureau Ethical Committee. We received written informed consent from study participants who could give consent and from the caretakers for those participants who could not have capacity to give consent after expressing the advantage of this research work. .Confidentiality was maintained by omitting personal identifiers.
2.8. Patient and public involvement
In the current study, participants were people who had follow-up at outpatients departments of psychiatry and they were not involved in the study design and recruitment. The results of this study will be disseminated to the Federal Ministry of Health, Amhara Health Bureau, and the three hospitals.
3. Results
A total of 420 respondents participated in this study with a response rate of 99.3%. The majority of the respondents were males 221 (52.6%). Most of the participants were single 222 (52.9%), orthodox followers 369 (87.9%), and Amhara by ethnicity 418 (99.5%). Regarding their occupation, about 1/4th of them were jobless 108 (25.7%) (Table 1).
Table 1.
Sociodemographic characteristics of participants attending Debretabor, Felegehiwot, and Gondar hospitals, North West Ethiopia, 2019 (n = 420).
| Characteristics | Frequency | Percent |
|---|---|---|
| Age | ||
| 18–24 | 115 | 27.3 |
| 25–39 | 209 | 49.8 |
| 40–49+ |
96 |
22.9 |
| Sex | ||
| Male | 221 | 52.6 |
| Female |
199 |
47.4 |
| Marital status | ||
| Single | 222 | 52.9 |
| Married | 126 | 30 |
| Widowed | 16 | 3.8 |
| Divorced |
56 |
13.3 |
| Religion | ||
| Orthodox | 369 | 87.9 |
| Muslim | 49 | 11.7 |
| Protestant |
2 |
0.5 |
| Ethnicity | ||
| Amhara | 418 | 99.5 |
| Tigray |
2 |
0.5 |
| Educational status | ||
| Illiterate | 158 | 37.6 |
| Primary school | 126 | 30 |
| Secondary school | 80 | 19 |
| Diploma | 30 | 7.1 |
| Degree and above |
26 |
6.2 |
| Job status | ||
| Has job | 312 | 74.3 |
| Jobless |
108 |
25.7 |
| Residence | ||
| Urban | 211 | 50.2 |
| Rural | 209 | 49.8 |
3.1. Substance-related factors of the respondents
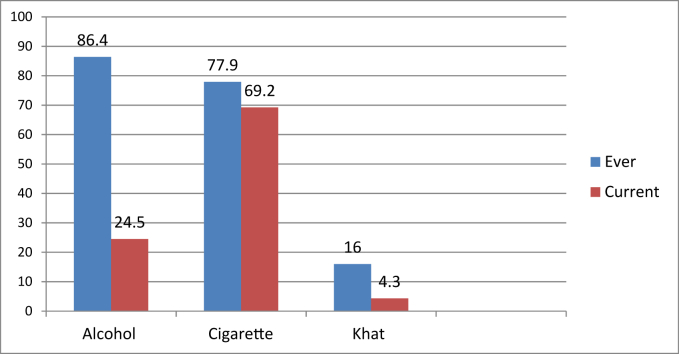
The majority of the respondents had ever use of alcohol and cigarette (Figure 2).
Figure 2.
Substance-related factors of disability among patients with schizophrenia attending outpatient departments in North West, Ethiopia, 2019.
3.2. Clinical factors
The majorities of the respondents were taking medications currently 401 (95.5%) and were taking only one medication 384 (91.4%). Near to half of the participants had positive symptoms 200 (47.6%) and were untreated 215 (51.2%) (Table2).
Table 2.
Clinical factors of the participants attending Debretabor, Felegehiwot and Gondar hospitals, North West Ethiopia, 2019 (n = 420).
| Characteristics | Frequency | Percent | |
|---|---|---|---|
| Negative symptoms | Yes No |
180 240 |
42.9 57.1 |
| Positive symptoms | Yes No |
200 220 |
47.6 52.4 |
| Taking medication currently | Yes No |
401 19 |
95.5 4.5 |
| Number of medications | One medication 2≥ medications |
384 36 |
91.4 8.6 |
| Duration of the illness | <1 year 1–5 years ≥5 |
104 184 132 |
24.8 43.8 31.4 |
| Duration of untreated psychosis | 1–2 years 2–5 years ≥5 years |
91 114 215 |
21.7 27.1 51.2 |
3.3. Magnitude of disability
The magnitude of disability in this study was 41.7% (95 % CI: 36.9, 46.4).
3.4. Factors associated with disability
To determine the association of independent variables with a disability, bivariate, and multivariate binary logistic regression analysis was carried out.
On the bivariate analysis of disability in relation to each explanatory variable: Not taking medication currently, longer duration of the illness, longer duration of untreated psychosis, current use of alcohol, being jobless, had positive and negative symptoms were found to be significant at a P-value <0.05. These factors were entered into multivariable binary logistic regression for further analysis to control confounding effects. In multivariate analysis having current alcohol use, being jobless, having ≥5 years of duration of illness, having untreated psychosis for ≥ 5 years, and having negative symptoms were significantly associated with disability at a p-value less than 0.05.
The odds of being disabled among patients with schizophrenia were 2.47 times higher among respondents who use alcohol as compared with those who didn't use alcohol currently (AOR = 2.47,95CI; 1.36,4.48).
Being jobless was 3.27 times more likely to develop a disability as compared with those respondents who had a job (AOR = 3.27, 95CI; 1.80, 5.93).
The likelihood of developing disability was 2.75 times higher among respondents who had 5 and more years of illness as compared with those respondents who had less than a 1-year duration of illness (AOR = 2.75,95CI; 1.29,5.86).
Those respondents who were not treated for 5 and more years were 3.78 times more likely to develop a disability as compared with those respondents who were not treated for less than two years (AOR = 3.78,95CI, 1.85,7.75). The likelihood of developing disability was 13.05 times higher among respondents who had negative symptoms as compared with those who had no negative symptoms (AOR = 13.05,95 CI, 7.58,22.45) (Table 3).
Table 3.
Factors of disability among participants attending Felegehiwot, Gondar and Debretabor hospitals North West, Ethiopia, 2019 (n = 420).
| variables | Category | Disability Yes No |
COR (95%CI) | AOR (95%CI) |
|---|---|---|---|---|
| Job-status | Has job Jobless | 100 212 75 33 |
1 4.82 (3.00,7.74)∗ |
1 3.27 (1.80,5.93)∗ |
| Current use of alcohol | No Yes |
106 211 69 34 |
1 4.04 (2.52,6.48)∗ |
1 2.47 (1.34.4.45)∗ |
| Positive symptoms | No Yes |
76 144 99 101 |
1 1.86 (1.25,2.75)∗ |
1 1.48 (0.87,2.53) |
| Negative symptoms | No Yes |
42 198 133 47 |
1 13.34 (8.33,21,34)∗ |
1 13.05 (7.58,22.45)∗ |
| current medication | Yes No |
160 241 15 4 |
1 5.65 (1.84,17.33)∗ |
1 1.48 (0.39,5.62) |
| Duration of the illness | <1 year 1–5 years ≥5 years |
32 72 77 107 66 66 |
1 1.62 (0.97,2.69) 2.25 (1.31,3.86)∗ |
1 1.57 (0.79,3,13) 2.75 (1.29,5.86)∗ |
| Duration of untreated psychosis | 1–2 years 2–5 years ≥5 years |
28 63 38 76 109 106 |
1 1.13 (0.62,2.03) 2.31 (1.38,3.89)∗ |
1 1.60 (0.73,3.53) 3.78 (1.85,7.75)∗ |
Key: ∗P < 0.05, model fitness (Hosmer and Lemshow) = 0.172.
4. Discussion
Schizophrenia remains one of the leading causes of disability and a life-shortening illness, caused mainly by poor physical health and its complications. The result is a considerably reduced lifespan that is marred by reduced levels of independence. In this study, the magnitude of disability was 41.7 % (95 %CI: 36.9, 46.4). This finding was in line with the studies conducted in China 41% [4], and other research conducted in China 37 %, 44% in men and women respectively [5], in India 41% [6]. On the other hand, the findings of this study were lower than the previous studies undertaken in India 83% [7], Ranchi Institute of Neuropsychiatry and Allied science Ranchi, 88% [8], Thirthahalli Taluk of Shimoga District, Karnataka 62% [9], in Spain 67.6% [10] and Nigeria 78% [11]. The possible reason could be the instrument, sample size, and cultural difference.
On the contrary, the finding of this research was higher than the studies done in Malaysia 34% [12]. The difference could be the sample size, in this study the sample size was 420 but in the Malaysian study, 128, and in this study, all the respondents were schizophrenic but in the case of Malaysia study the participants were both patients with schizophrenia and mood disorders.
On the independent predictors of disability, current use of alcohol being jobless, had negative symptoms, had 5 and more years of illness, and had 5 and more years of untreated psychosis were predictors of disability.
Specifically, the greater likelihood of disability occurred among those who used alcohol currently as compared with those respondents who did not use alcohol currently, which is similar to other study [9]. The evidence indicates that substance abuse severely complicates schizophrenia by causing relapse, hospitalization, disrupting behavior, creating familial problems, residential instability, decreased functional status, and medication noncompliance [13].
Participants who had negative symptoms were more likely to develop a disability as compared with those respondents who had no negative symptoms. This is due to that the negative symptoms of schizophrenia, including problems with motivation, social withdrawal, diminished affective responsiveness, speech, and movement, contribute more to poor functional outcomes and quality of life for individuals with schizophrenia than do positive symptoms [14]. This was supported by the studies conducted in Turkey, India, Spain, and a result of meta-analysis [15, 16, 17, 18].
Having 5 and more years of illness was significantly associated with disability in this study. The rationale might be, longer duration of psychosis is associated with poor response to antipsychotic treatment, the severity of negative symptoms, and poor functional outcomes [19]. The finding was supported by the studies conducted in Indian studies [8, 9, 20].
The odds of developing disability were 3.78 times higher among respondents who had 5 and more years of untreated psychosis as compared with those respondents who were not treated for less than two years which is similar to the results of other studies [16, 21]. The possible explanation might be there is an association between a longer duration of untreated psychosis and poor outcome in schizophrenia. These studies have been interpreted as providing evidence that untreated psychosis may constitute an "active morbid process" that is "toxic" to the brain which leads to disability [22].
Moreover, being jobless was the strongest predictor of disability as compared with those individuals who had a job which was supported by the study done in Taiwan [23]. Because employment for individuals living with psychiatric disabilities becomes an acceptable norm and expectation, then the barriers of stigma, class bias, and discrimination diminish [24].
4.1. Strength and limitations
The design of the study was cross-sectional; therefore, we were unable to conclude the observed associations may not necessarily any causal direction. This study also missed important factors to be included as factors that greatly affected disability including social support, quality of life, and the type of medication that the patients were taking.
This is the first novel study in this area that tried to show the magnitude of disability in schizophrenic patients.
In this research, a relatively large sample size was included and since it was a face-to-face interview, we were addressing individuals who had a disability for further investigation and intervention.
5. Conclusion
The magnitude of disability in patients with schizophrenia was 41.7 %. This confirmed that schizophrenia has a greater impact on the functionality of the patient. Current use of alcohol, being jobless, had negative symptoms, had 5 and more years of illness, and had 5 and more years of untreated psychosis were factors significantly associated with disability. Therefore we recommend that disability-focused regular screening of the patient with schizophrenia by trained health professionals and timely linkage for better rehabilitation and other mental health services. It is also necessary to emphasize individuals with current use of alcohol, jobless, had negative symptoms, had 5 and more years of illness, and had 5 and more years of untreated psychosis. Furthermore, longitudinal study is recommended by including important factors that have been missed in this study such as social support, quality of life and the type of medication that the patients take.
Declarations
Author contribution statement
Getnet Mihretie Beyene: Conceived and designed the experiments; Performed the experiments.
Getasew Legas, Telake Azale and Mebrat Abera: Analyzed and interpreted the data.
Sintayehu Asnakew: Analyzed and interpreted the data; Wrote the paper.
Funding statement
This work was supported by Debre Tabor University
Data availability statement
Data included in article/supplementary material/referenced in article.
Declaration of interests statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
References
- 1.Habtamu K., Alem A., Medhin G., Fekadu A., Dewey M., Prince M. Validation of the World Health Organization disability assessment schedule in people with severe mental disorders in rural Ethiopia. Health Qual. Life Outcome. 2017;15(1):64. doi: 10.1186/s12955-017-0647-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barbotte E., Guillemin F., Chau N. Prevalence of impairments, disabilities, handicaps, and quality of life in the general population: a review of recent literature. Bull. World Health Organ. 2001;79:1047–1055. [PMC free article] [PubMed] [Google Scholar]
- 3.Humeniuk R., Ali R., Babor T.F., Farrell M., Formigoni M.L., Jittiwutikarn J. Validation of the alcohol, smoking, and substance involvement screening test (ASSIST) Addiction. 2008;103(6):1039–1047. doi: 10.1111/j.1360-0443.2007.02114.x. [DOI] [PubMed] [Google Scholar]
- 4.Liu T., Zhang L., Pang L., Li N., Chen G., Zheng X. Schizophrenia-related disability in China: prevalence, gender, and geographic location. Psychiatr. Serv. 2015;66(3):249–257. doi: 10.1176/appi.ps.201400032. [DOI] [PubMed] [Google Scholar]
- 5.Liu T., Song X., Chen G., Paradis A.D., Zheng X. Prevalence of schizophrenia disability and associated mortality among Chinese men and women. Psychiatr. Res. 2014;220(1-2):181–187. doi: 10.1016/j.psychres.2014.04.042. [DOI] [PubMed] [Google Scholar]
- 6.Ranganathan M., Ezhumalai S., Praharaj S.K. The pattern of disability among persons who availed half-way home-care services for psychosocial rehabilitation. Ind. Psychiatr. J. 2012;21(2):173. doi: 10.4103/0972-6748.119655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shihabuddeen I., Harpreet M., Pinto A. Disability in schizophrenia and bipolar mood disorder at a general hospital psychiatry unit. Delhi Psychiat. J. 2011;14(2):258–261. [Google Scholar]
- 8.Ali A. Disability in schizophrenia and its relationship with the duration of illness and age of onset. Int. J. Psychosoc. Rehabil. 2009;14(2) [Google Scholar]
- 9.Thirthalli J., Venkatesh B.K., Naveen M.N., Venkatasubramanian G., Arunachala U., Kumar K.V.K. Do antipsychotics limit disability in schizophrenia? A naturalistic comparative study in the community. Indian J. Psychiatr. 2010;52(1):37. doi: 10.4103/0019-5545.58893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guilera G., Gómez-Benito J., Pino O., Rojo J.E., Cuesta M.J., Martínez-Arán A. Utility of the World Health Organization disability assessment schedule II in schizophrenia. Schizophr. Res. 2012;138(2-3):240–247. doi: 10.1016/j.schres.2012.03.031. [DOI] [PubMed] [Google Scholar]
- 11.Fakorede O.O., Ogunwale A., Akinhanmi A.O. Disability among patients with schizophrenia: a hospital-based study. Int. J. Soc. Psychiatr. 2020;66(2):179–187. doi: 10.1177/0020764019894608. [DOI] [PubMed] [Google Scholar]
- 12.Rahman M., Indran S. Disability in schizophrenia and mood disorders in a developing country. Soc. Psychiatr. Psychiatr. Epidemiol. 1997;32(7):387–390. doi: 10.1007/BF00788178. [DOI] [PubMed] [Google Scholar]
- 13.Drake R.E., Brunette M.F. Recent Developments in Alcoholism. Springer; 1998. Complications of severe mental illness related to alcohol and drug use disorders; pp. 285–299. [DOI] [PubMed] [Google Scholar]
- 14.Correll C.U., Schooler N.R. Negative symptoms in schizophrenia: a review and clinical guide for recognition, assessment, and treatment. Neuropsychiatric Dis. Treat. 2020;16:519. doi: 10.2147/NDT.S225643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gupta A., Chadda R. Disability in schizophrenia: do short hospitalizations have a role? Int. J. Psychosoc. Rehabil. 2008;13(1) [Google Scholar]
- 16.Alptekin K., Erkoç Ş., Göğüş A.K., Kültür S., Mete L., Üçok A. Disability in schizophrenia: clinical correlates and prediction over 1-year follow-up. Psychiatr. Res. 2005;135(2):103–111. doi: 10.1016/j.psychres.2004.05.027. [DOI] [PubMed] [Google Scholar]
- 17.Eack S.M., Newhill C.E. Psychiatric symptoms and quality of life in schizophrenia: a meta-analysis. Schizophr. Bull. 2007;33(5):1225–1237. doi: 10.1093/schbul/sbl071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Villalta-Gil V., Vilaplana M., Ochoa S., Haro J.M., Dolz M., Usall J. Neurocognitive performance and negative symptoms: are they equal in explaining disability in schizophrenia outpatients? Schizophr. Res. 2006;87(1-3):246–253. doi: 10.1016/j.schres.2006.06.013. [DOI] [PubMed] [Google Scholar]
- 19.Perkins D.O., Gu H., Boteva K., Lieberman J.A. Relationship between duration of untreated psychosis and outcome in first-episode schizophrenia: a critical review and meta-analysis. Am. J. Psychiatr. 2005;162(10):1785–1804. doi: 10.1176/appi.ajp.162.10.1785. [DOI] [PubMed] [Google Scholar]
- 20.Mohan I., Tandon R., Kalra H., Trivedi J. Disability assessment in mental illnesses using Indian disability evaluation assessment scale (IDEAS) Indian J. Med. Res. 2005;121(6):759. [PubMed] [Google Scholar]
- 21.Del Rey-Mejías Á., Fraguas D., Díaz-Caneja C.M., Pina-Camacho L., Castro-Fornieles J., Baeza I. Functional deterioration from the premorbid period to 2 years after the first episode of psychosis in early-onset psychosis. Eur. Child Adolesc. Psychiatr. 2015;24(12):1447–1459. doi: 10.1007/s00787-015-0693-5. [DOI] [PubMed] [Google Scholar]
- 22.Norman R.M., Malla A.K. Duration of untreated psychosis: a critical examination of the concept and its importance. Psychol. Med. 2001;31(3):381–400. doi: 10.1017/s0033291701003488. [DOI] [PubMed] [Google Scholar]
- 23.Chen R., Liou T.-H., Chang K.-H., Yen C.-F., Liao H.-F., Chi W.-C. Assessment of functioning and disability in patients with schizophrenia using the WHO Disability Assessment Schedule 2.0 in a large-scale database. Eur. Arch. Psychiatr. Clin. Neurosci. 2018;268(1):65–75. doi: 10.1007/s00406-017-0834-6. [DOI] [PubMed] [Google Scholar]
- 24.Marrone J., Golowka E. If work makes people with mental illness sick, what do unemployment, poverty, and social isolation cause? Psychiatr. Rehabil. J. 1999;23(2):187. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data included in article/supplementary material/referenced in article.