Abstract
Objectives
The purpose of this study was to examine the biomechanical effects of fixation on range of motion (ROM) in the upper and lower adjacent segments of different lumbar spine segments in a goat spine model.
Methods
Fifteen goat spine specimens (vertebrae T12–S1) were randomly divided into three groups: A (single-segment fixation), B (double-segment fixation), and C (triple-segment fixation). Motion in different directions was tested using a spinal motion simulation test system with five external loading forces. Transverse, forward–backward, and vertical displacement of the upper and lower adjacent segments were measured.
Results
As the external load increased, the upper and lower adjacent segment ROM increased. A significantly greater ROM in group C compared with group A was found when the applied external force was greater than 75 N. The upper adjacent segment showed a significantly greater ROM than the lower adjacent segment ROM within each group.
Conclusions
Adjacent segment ROM increased with an increasing number of fixed lumbar segments. The upper adjacent segment ROM was greater than that of the lower adjacent segments. Adjacent segment stability after lumbar internal fixation worsened with an increasing number of fixed segments.
Keywords: Adjacent segment degeneration, range of motion, biomechanics, fixed segment, lumbar vertebrae, lumbar internal fixation
Introduction
Lumbar internal fixation is the main treatment method for patients with lumbar spondylolisthesis, lumbar spinal stenosis, and lumbar vertebral fractures. However, adjacent segment degeneration (ASD) often occurs after lumbar multisegment fixation,1–3 resulting in unsatisfactory clinical efficacy in long-term follow-up and a high incidence of revision lumbar surgery.4,5
Many potential mechanisms contribute to the occurrence of ASD, but one of most important mechanisms is increased mobility in adjacent segments caused by the rigid and long fixed segments, which leads to ASD.6–8 Stress is concentrated on the adjacent segments, resulting in their increased activity and poor stability.8,9 ASD has also been detexted in patients with an increased number of lumbar internal fixations and fusions.
Because ASD often occurs after lumbar internal fixation, improving the surgical methods and strategies to reduce the incidence of ASD has become a topic of interest to scholars. There are several surgical strategies to prevent ASD, such as hemilaminectomy and total laminectomy, 10 hybrid instrumentation of the lumbar spine, 11 the topping-off technique, 12 semi-rigid stabilization device, 13 dynamic stabilization devices, and other implants. 14 Most lumbar degenerative diseases in middle-aged and older patients involve multisegmental degeneration, and the degree of degeneration from lesions in different segments varied. 15
To reduce the incidence of ASD caused by multisegment fixation, some surgeons recommend selecting the short-segment internal fixation, which solves the problem of lumbar instability, preserves the range of motion (ROM) in the lumbar spine, and conforms to the original physiological activity of the spine. However, surgical treatment of lumbar fractures or degenerative diseases often requires fixation of multiple segments, and even if therapy is limited to single or double segments, various degrees of degeneration in adjacent segments were found during long-term follow-up.
Our previous biomechanical study 16 found that when the number of fixated lumbar segments increased, the ROM and intradiscal pressure of the adjacent segments also increased. The upper adjacent segment or the lower adjacent segment is more prone to degeneration after firm fixation. However, it is still unclear if the superior or inferior segment is more significantly affected after fixation. To the best of our knowledge, this topic has not yet been reported in the current research literature and is worthy of further study.
Humans and goats are not closely related species. However, the goat spine model is considered to have good similarity to the human spine and to be a good biomechanical model to simulate human spinal motion after anatomical and biomechanical analysis. 17 Therefore, the main purpose of this study was to analyze the effects of applying different pressures and mechanical loads in various directions on the ROM in adjacent upper and lower segments in different fixed segments of the goat lumbar spine.
Materials and methods
Materials
Fifteen spine specimens from 1- to 2-year-old goats were selected. 4 After the goats were sacrificed, isolated spine specimens were obtained within 2 hours. All the tested specimens were from vertebra T12 to S1. They were kept moist using wet gauze and were sealed in plastic bags and stored frozen at −20°C until experimentation. The specimens were removed from the −20°C freezer 24 hours before the experiment and allowed to thaw naturally to a room temperature of 22°C to 25°C.
The paravertebral muscles of the goat spine were removed, but the interspinous ligaments, the supraspinous ligaments, the intervertebral discs, and the vertebral bodies were completely preserved. All specimens were radiologically examined to exclude deformed spine specimens. A denture base polymer (Shanghai Beiqiong Tooth Co. Ltd., Shanghai, China) was reconstituted and used to embed the first lumbar vertebra and tail vertebral bodies. Spinal internal fixation equipment (Shanghai Sanyou Medical Co., Ltd., Shanghai, China) included pedicle screws (diameter, 5.0 mm; length, 30 mm), titanium rods (diameter, 5.0 mm; length, 55 mm, 85 mm, and 110 mm), and eight boxes of bone cement (Shanghai Sanyou Medical Co. Ltd.). The biomechanical test system was mainly a spinal motion simulation test system (Shimadzu Corporation, Jiangsu, China) and high definition (HD) cameras (Canon Co. Ltd., Beijing, China; Shenzhen Jinghang Technology Co., Ltd., Shenzhen, China) (Figure 1).
Figure 1.
Main experimental equipment.
Groups and experimental models
The 15 experimental specimens were randomly divided into three groups: A, B, and C. Each group included five specimens, and is described below.
Group A was a single-segment fixation group. Pedicle screws (5.0 mm × 30 mm) were screwed into the bilateral sides of the L4 and L5 vertebral bodies, titanium rods (5.0 mm × 55 mm) were attached, and the nuts were tightened. The upper segment is indicated by A1 while the lower segment is indicated by A2.
Group B was a double-segment fixation group. Pedicle screws (5.0 mm × 30 mm) were inserted bilaterally into the L3, L4, and L5 vertebral bodies, titanium rods (5.0 mm × 85 mm) were placed, and the nuts were tightened. The upper segments are indicated by B1 while the lower segment is indicated by B2.
Group C was a triple-segment fixation group. Pedicle screws (5.0 mm × 30 mm) were inserted into both sides of the vertebral bodies of L2, L3, L4 and L5, titanium rods (5.0 mm × 110 mm) were placed, and the nuts were tightened. The upper segments are indicated by C1 while the lower segment is indicated by C2.
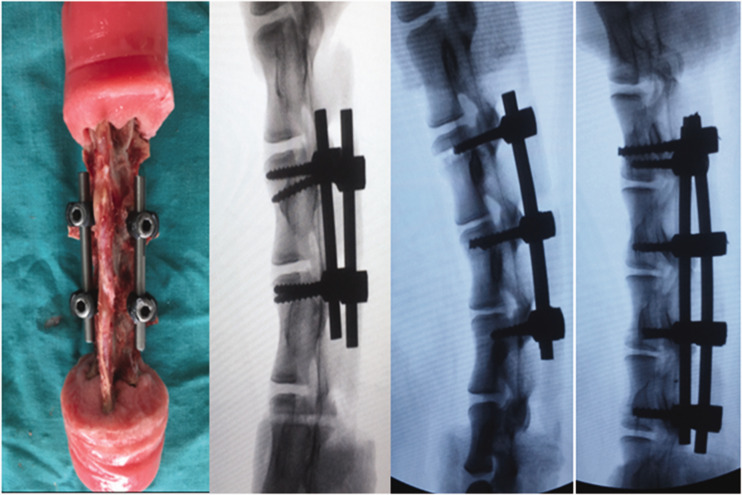
All specimens were subsequently examined using an X-ray to determine whether the lumbar internal fixation implant was in a good position. A representative specimen model and its radiologic image are shown in Figure 2.
Figure 2.
Successful specimen model and its X-ray imaging.
Experimental protocol
After successfully establishing the specimen model, we began to test the ROM of the goat lumbar spine specimens. The force-loading device was produced by Shimadzu (AG-IS-20 model; Shimadzu Analytical China Ltd., Suzhou, China). The torque generation and image detextion device were homemade and calibrated. The force-loading device was a universal testing machine with accurate measurements that were obtained using crosshead displacement measurements. The measurement resolution was 0.001 mm, and the crosshead speed accuracy was ±1%. The accuracy of the pressure sensor (type: SFL-20KNAG) was ±0.5% of the displayed value for tensile pressure measurement, and the accuracy of displacement that was measured using visual methods (depending on the spatial position of each experiment) was up to ±0.01 mm.
The Shimadzu universal testing machine that was used for this experiment was set at a constant loading speed of 35 mm/minute, and the frequency of acquisition was 50 Hz/s. Anterior flexion, posterior extension, and lateral bending were generated by applying a pure torque in the forward, backward, left, and right directions, without axial external load involvement. The top of the device is a fixed disc on which paired force couples were applied with a force arm length of 45 mm, the size of which can be calculated from the force×force arm (45 mm). Three preconditioning steps were performed before each force loading. Preloading was used for flexion and extension of the spine as well as left and right torsion. The magnitude of the preload moment was 20% of the experimental maximum moment.
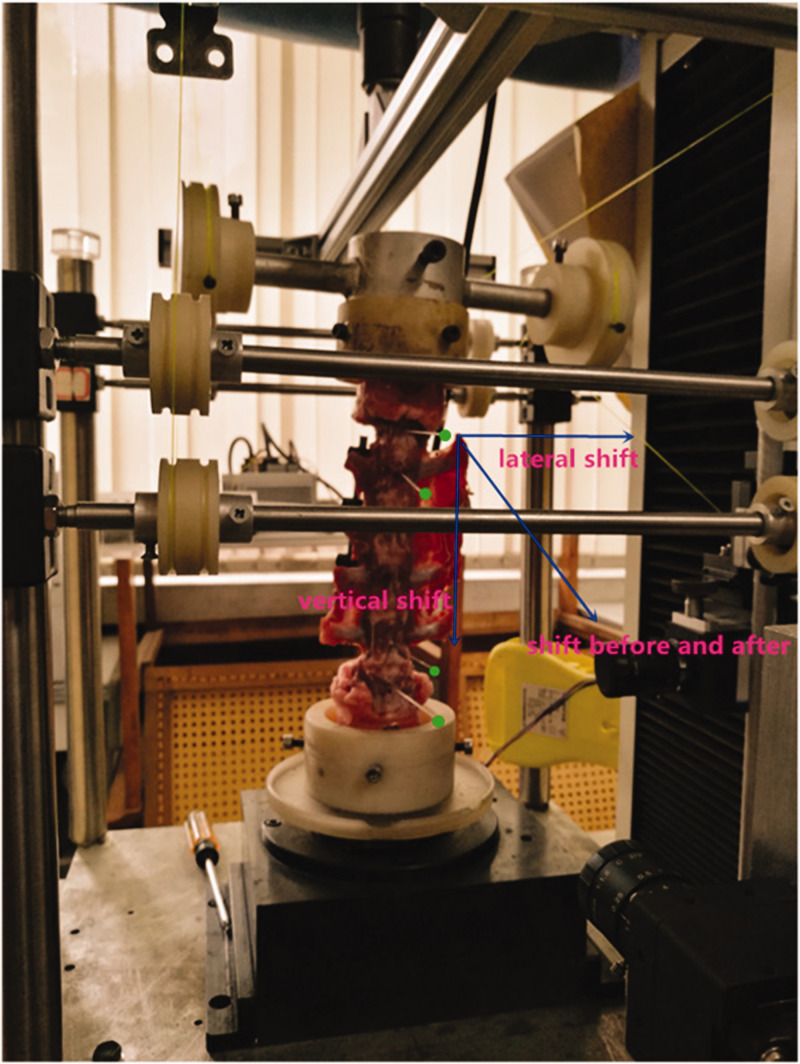
Spinal specimens were tested using anterior flexion, posterior extension, and lateral bending in group A under loading with five axial external forces (45 N, 75 N, 105 N, 135 N, or 165 N). The transverse displacement, forward–backward displacement, and vertical displacement of the upper and lower observation points of the adjacent segments were recorded. The biomechanical tests in Groups B and C were performed using the same method. Figure 3 shows the schematic diagram of the coordinates of the ball movement during the testing process.
Figure 3.
Schematic diagram of the coordinates of the ball movement.
This study was performed under the guidance of the relevant laws and regulations. This animal biomechanics research program was reviewed and approved by the Guangxi Zhuang Autonomous Region People’s Hospital Medical Ethics Committee (approval no. 2016065).
Camera calibration and coordinate conversion
In the experiments involving cameras, the left and right cameras were calibrated independently, and the physical-to-pixel ratio was converted from the physical size of the marker sphere to the pixel size relationship for the current experiments. In this manner, the actual displacement was converted from the displacement that was calculated using the image method. The observed diameter of the sphere was 110 pixels, the physical diameter was 1.45 mm, the physical size of each pixel was 1.45/110, and the pixel-level accuracy was approximately 0.013200 mm.
The relationship in the physical-to-pixel ratio in the current experiment was calculated using the relationship between the physical size of the marker ball (D. 1.35 mm) and the pixel size. The actual displacement of the observation ball was converted using the conversion formula.
During the test, some images were taken from a 45° perspective (left and right viewing angles). For the unification of the final result, according to the three-dimensional coordinate transformation formula, the rotation transformation around the Z axis (vertical direction, which is the Y reverse direction in the acquired image) is as follows:
Its transformation matrix is as follows:
The calibration results were obtained as described below. When the angle (θ) is 45° (clockwise), the diameter of the marker ball is 1.35 mm, and its pixels are 110. After the above matrix formula transformation and calculation, the physical size of each pixel is 1.35 mm/110, from which the displacement of the ball is calculated to be approximately 0.01227 mm.
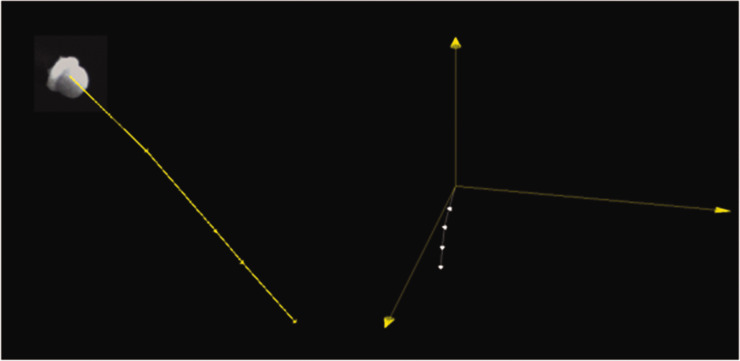
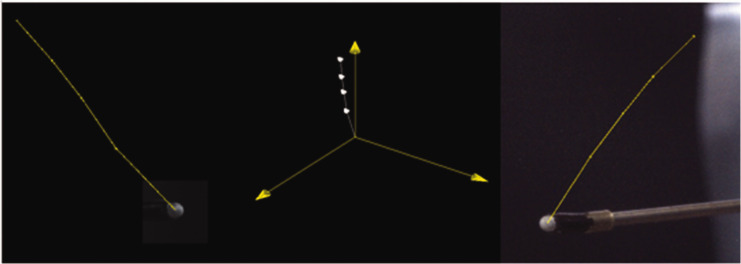
The displacement distance of the points was input into the calculation transformation formula to calculate the forward–backward displacement, transverse displacement, and vertical displacement. Figure 4 shows the plan view of the displacement of the ball, and Figure 5 shows the stereo view of the small ball displacement track.
Figure 4.
Plan view and 3D view of the displacement of the ball.
Figure 5.
Left view of the ball/3D displacement schematic diagram/Right view of the ball.
Statistical methods
SPSS version 18.0 (SPSS Inc., Chicago, IL, USA) was used for the statistical analysis. The displacement data are expressed as the mean ± standard deviation. One-way analysis of variance was used for pairwise comparisons between groups, and a t-test was used to compare the upper and lower points within the group. The test level was set at α=0.05, and P<0.05 was considered to be statistically significant.
Results
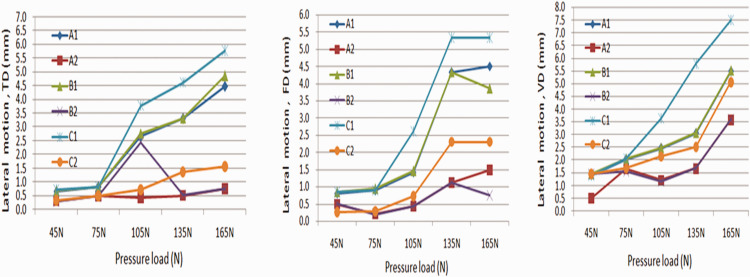
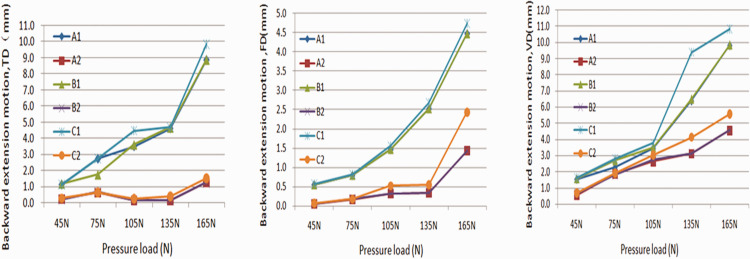
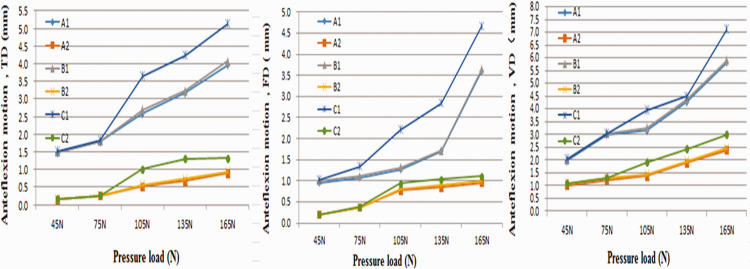
As shown in Figures 6, 7, and 8, as the external load increased, the ROM of the upper and lower adjacent segments increased in all three groups. The ROM includes the lateral motion (Figure 6), backward extension (Figure 7), and anteflexion motion (Figure 8). In all groups, the ROM of the upper adjacent segment was greater than that of the lower adjacent segment for the different directions of movement when the external force was greater than 75 N (P<0.001; Supplementary Tables 1–9).
Figure 6.
Measurement results of transverse displacement, forward?backward displacement, and vertical displacement in lateral motion; A1, B1 and C1 represent the upper adjacent segments; A2, B2 and C2 represent the lower adjacent segments. TD, transverse displacement; FD, forward?backward displacement; VD, vertical displacement.
Figure 7.
Measurement results of transverse displacement, forward?backward displacement, and vertical displacement in backward extension; A1, B1 and C1 represent the upper adjacent segments; A2, B2 and C2 represent the lower adjacent segments.TD, transverse displacement; FD, forward?backward displacement; VD, vertical displacement.
Figure 8.
Measurement results of transverse displacement, forward?backward displacement, and vertical displacement in anteflexion motion; A1, B1 and C1 represent the upper adjacent segments; A2, B2 and C2 represent the lower adjacent segments.TD, transverse displacement; FD, forward?backward displacement; VD, vertical displacement.
When the ROM was compared between groups A and C in different directions of movement, including anterior flexion, posterior extension, and lateral bending, the differences in displacement (transverse displacement, forward–backward displacement, and vertical displacement) of the upper and lower adjacent segments were not statistically significant when the external force was less than or equal to 75 N. However, the displacement representing the ROM was significantly greater in group C compared with group A when the external force was greater than 75 N (P<0.05 for all directions) (Supplementary Tables 1–9).
For lateral motion, significantly greater displacement was found when the upper ends of groups A and C and the lower ends of groups A and C were compared for transverse displacement (P<0.001; Supplementary Table 1), forward and backward displacement (P<0.020; Supplementary Table 2), and vertical displacement (P<0.001; Supplementary Table 3) when forces of 105 N, 135 N, and 165 N were applied. There were no significant differences in the transverse displacement, forward and backward displacement, or vertical displacement movements when forces of 45 N or 75 N were applied.
For backward extension, significant differences were found in the ROM when the upper and lower ends of groups A and C were compared for transverse displacement (P<0.001; Supplementary Table 4), forward and backward displacement (P<0.003; Supplementary Table 5), and vertical displacement (P<0.013; Supplementary Table 6) when forces of 105 N, 135 N, and 165 N were applied. There were no significant differences in the transverse displacement, forward and backward displacement, or vertical displacement movements when forces of 45 N or 75 N were applied.
For anteflexion motion, significant differences were found when the upper and lower ends of groups A and C were compared for transverse displacement (P<0.001; Supplementary Table 7), forward and backward displacement (P<0.003; Supplementary Table 8), and vertical displacement (P<0.007; Supplementary Table 9) when forces of 105 N, 135 N, and 165 N were applied. There were no significant differences in the transverse displacement, forward and backward displacement, or vertical displacement movements when forces of 45 N or 75 N were applied.
The ROM in groups B and C were also compared. The displacement representing the ROM was also significantly greater in group C compared with group B in the upper and lower adjacent segments for lateral motion (Supplementary Table 1), backward extension (Supplementary Table 2), and anteflexion (Supplementary Table 3) motions, including anterior flexion, posterior extension, and lateral bending, when forces of 105 N, 135 N, or 165 N were applied (P<0.05 for most, with some exceptions; see Supplementary Tables 1, 2, and 3). When the force was less than or equal to 75 N, the displacement was not significantly different in the upper or lower adjacent segments.
For lateral motion, when groups B and C were compared, statistically significant differences in the ROM were observed for transverse displacement (P<0.001; Supplementary Table 1), forward and backward displacement (P<0.001; except for the upper end at 135 N, which was not significant; Supplementary Table 2), and vertical displacement (P<0.001; Supplementary Table 3) when forces of 105 N, 135 N, and 165 N were applied. There were no significant differences in the transverse displacement, forward and backward displacement, or vertical displacement movements when forces less than or equal to 75 N were applied.
For backward extension, when groups B and C were compared, statistically significant differences were observed in the ROM for transverse displacement (P<0.001; except for the upper end at 135 N, which was not statistically significant; Supplementary Table 4), forward and backward displacement (P<0.001; Supplementary Table 5), and vertical displacement (P<0.001; except for the upper end at 105 N, which was not statistically significant; Supplementary Table 6) when forces of 105 N, 135 N, and 165 N were applied. There were no significant differences in the transverse displacement, forward and backward displacement, or vertical displacement movements when forces of less than or equal to 75 N were applied.
For anteflexion motion, when groups B and C were compared, statistically significant differences were observed for transverse displacement (P < 0.001; Supplementary Table 7), forward and backward displacement (P < 0.015; Supplementary Table 8), and vertical displacement (P < 0.001; except for the upper end at 135 N, which was not significant; Supplementary Table 9) when forces of 105 N, 135 N, and 165 N were applied. There were no significant differences in the transverse displacement, forward and backward displacement, or vertical displacement movements when forces less than or equal to 75 N were applied.
In group A compared with group B, the differences in the ROM of the upper and lower adjacent segments were not statistically significant in any direction of movement.
Discussion
Main findings
In our study, the ROM of adjacent segments in goat lumbar vertebrae increased with increasing external mechanical load after motions involving lateral bending, anterior flexion, or posterior extension. Compared with single- or double-segment fixation, triple-segment fixation has a more significant negative effect on the activity of adjacent segments. In this experiment, the ROM of the upper adjacent segment was larger than the ROM of the next adjacent segment, and the more fixed segments there were, the greater was the increase in horizontal displacement.
The influence of different fixed lumbar vertebrae segments on adjacent segments
Regardless of whether lateral bending motion, anterior flexion, or posterior extension was performed, the displacement of the upper and lower adjacent segments of the lumbar spine after fixation increased with increasing external mechanical load, but the most significant change in displacement was after three-segment fixation. The main results of this research are consistent with the results that were reported in previous studies.4,6,16
The reason may be that the concentration of stress in adjacent segments after lumbar internal fixation was significant, leading to disc degeneration and symptoms.3,9,18 Some researchers found that following long segmental fixation of the spine, especially after fixation to the fifth lumbar vertebral body or pelvis and loss of lumbosacral mobility, stress was concentrated on the proximal adjacent segment, causing lesions in the proximal junction area. This has even been shown to cause kyphosis or failure of the proximal junction.19,20
In this experiment, the increase in the displacement of the adjacent segments after multisegment fixation under external force loading can also be explained by the stress concentration theory. 21 This means that when one or more spinal segments are fixed, the amount of deformation of the fixed segment will decrease or disappear and can only be transferred to the upper and lower segments. This results in increased displacement, stress concentration, and increased passive motion of these segments, and ultimately, the adjacent segments become unstable.
To the best of our knowledge, there is no biomechanical study that compares the activity of the upper and lower adjacent segments in an animal model. The results of this study show that the number of fixed segments is associated with horizontal displacement and that the ROM of the upper adjacent segments is greater than that of the lower adjacent segments. Our biomechanical research results are consistent with previous research results on proximal degeneration.22,23 Lange et al. 24 performed a biomechanical study that showed that when the L2 to L6 vertebral bodies were fixed, the proximal adjacent segment ROM significantly increased. However, the results from our study are not consistent with actual clinical work. The potential explanations may be that our experiment was performed in vitro, and exercise experiments using isolated specimens under different loading conditions may not completely simulate the physiological movement of the living body. Additionally, goats and humans are not closely related species, and the physiological movement of the goat spine is not identical to the physiological movement of the human spine.
When multiple segments of the lumbar spine are rigidly fixed, the fixed segment loses its mobility and cannot disperse the stress. The physiological stress transmission of the lumbar vertebra will change, and the stress is concentrated on the segments above and below the fixed segment, resulting in poor stability of the adjacent segments. The increased stress on, and increased ROM of, adjacent segments inevitably aggravate the degeneration of the intervertebral discs and the facet joints of adjacent segments.25,26 Therefore, based on previous studies and our experimental results, to prevent the occurrence of ASD, we suggest that lumbar vertebral fracture or lumbar degenerative disease should be fixed in the responsible segment. For stable segments, the original physiological activity of the lumbar spine should be preserved as much as possible. Minimally invasive decompression or short segment fixation should be used as its basic standard procedure.
Limitations of the study
The limitations of this study are described below. First, although there is structural similarity between the goat spine and human spine, the goat spine cannot completely simulate the physiological movement mechanism of the human spine. Second, the isolated lumbar spine specimens that we selected had the paravertebral muscles removed, which may have caused experimental error due to structural integrity damage. Finally, there may have been some experimental errors in data collection and the transformation process during the experiments. Further biomechanical experiments of isolated human spine specimens or animal in vivo biomechanical experiments are needed to detext the effects of different fixed segments of the lumbar spine on the proximal and distal mobility of adjacent segments.
Conclusion
Goat biomechanical experiments show that for the degree of motion in the adjacent lumbar spine segments, the activity of the upper adjacent segments is greater than the activity of the lower adjacent segments. Additionally, the more fixed segments there are, the more obvious is the increase in displacement. The increased ROM in the adjacent segments could accelerate degeneration in adjacent segments, which is likely to be the main factor in ASD after lumbar internal fixation.
Supplemental Material
Supplemental material, sj-pdf-1-imr-10.1177_03000605211020219 for Upper and lower adjacent segment range of motion after fixation of different lumbar spine segments in the goat: an in vitro experiment by Yufu Ou, Zengming Xiao, Jianxun Wei, Hua Jiang and Zhuhai Li in Journal of International Medical Research
Acknowledgment
The authors would like to thank the members of the research group for useful discussions.
Author contributions: Yufu Ou, Zengming Xiao, and Jianxun Wei analyzed and interpreted the data and drafted the manuscript. Hua Jiang and Zhuhai Li acquired the data. Yufu Ou and Zengming Xiao contributed to conception and design of the study. All authors approved the final content of the manuscript.
Declaration of conflicting interest: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: This work was supported by the Guangxi Natural Science Foundation Program (2016GXNSFAA380058 and 2020GXNSFAA297217).
ORCID iD: Zengming Xiao https://orcid.org/0000-0003-3583-9474
Supplemental material: Supplementary material for this article is available online.
References
- 1.Bredow J, Löhrer L, Oppermann J, et al. Pathoanatomic risk factors for instability and adjacent segment disease in lumbar spine: how to use topping off?. Biomed Res Int 2017; 2017: 2964529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Heo Y, Park JH, Seong HY, et al. Symptomatic adjacent segment degeneration at the L3-4 level after fusion surgery at the L4-5 level: evaluation of the risk factors and 10-year incidence. Eur Spine J 2015; 24: 2474–2480. [DOI] [PubMed] [Google Scholar]
- 3.Yamasaki K, Hoshino M, Omori K, et al. Risk factors of adjacent segment disease after transforaminal inter-body fusion for degenerative lumbar disease. Spine (Phila Pa 1976) 2017; 42: E86–E92. [DOI] [PubMed] [Google Scholar]
- 4.Thomas S, Dante M, Max A, et al. Posterolateral and anterior interbody spinal fusion models in the sheep. Clin Orthop Relat Res 2000; 2: 28–37. [DOI] [PubMed] [Google Scholar]
- 5.Kim DK, Lim H, Rim DC, et al. Clinical and radiological comparison of semirigid (WavefleX) and rigid system for the lumbar spine. Korean J Spine 2016; 13: 57–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nagata H, Schendel MJ, Transfeldt EE, et al. The effects of immobilization of long segments of the spine on the adjacent and distal facet force and lumbosacral motion. Spine (Phila Pa 1976) 1993; 18: 2471–2479. [DOI] [PubMed] [Google Scholar]
- 7.Radcliff KE, Kepler CK, Jakoi A, et al. Adjacent segment disease in the lumbar spine following different treatment interventions. Spine J 2013; 13: 1339–1349. [DOI] [PubMed] [Google Scholar]
- 8.Saavedra-Pozo FM, Deusdara RA, Benzel EC. Adjacent segment disease perspective and review of the literature. Ochsner J 2014; 14: 78–83. [PMC free article] [PubMed] [Google Scholar]
- 9.Harrop JS, Youssef JA, Maltenfort M, et al. Lumbar adjacent segment degeneration and disease after arthrodesis and total disc arthroplasty. Spine (Phila Pa 1976) 2008; 33: 1701–1707. [DOI] [PubMed] [Google Scholar]
- 10.Liu H ,Wu W , Li Y, et al. Protextive effects of preserving the posterior complex on the development of adjacent-segment degeneration after lumbar fusion: clinical article. J Neurosurg Spine 2013; 19: 201–206. [DOI] [PubMed] [Google Scholar]
- 11.Hudson WR, Gee JE, Billys JB, et al. Hybrid dynamic stabilization with posterior spinal fusion in the lumbar spine. SAS J 2011; 5: 36–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oikonomidis S, Ashqar G, Kaulhausen T, et al. Clinical experiences with a PEEK-based dynamic instrumentation device in lumbar spinal surgery: 2 years and no more. J Orthop Surg Res 2018; 13: 196–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jain P, Khan MR. Prediction of biomechanical behavior of lumbar vertebrae using a novel semi-rigid stabilization device. Proc Inst Mech Eng H 2019; 233: 849–857. [DOI] [PubMed] [Google Scholar]
- 14.Mu X, Wei J, AJ, et al. The short-term efficacy and safety of artificial total disc replacement for selected patients with lumbar degenerative disc disease compared with anterior lumbar interbody fusion: a systematic review and meta-analysis. PLoS ONE 2018, 13(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu H, Pang Q and, Jiang G. . Medium-term effects of Dynesys dynamic stabilization versus posterior lumbar interbody fusion for treatment of multisegmental lumbar degenerative disease. J Int Med Res 2017; 45: 1562–1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mu X, Li Z, Yin D, et al. Biomechanical effects of fixation of different segments of goat lumbar spine on adjacent segmental motion and intradiscal pressure change. Med Sci Monit 2019; 25: 4885–4891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kumar N, Kukreti S, Ishaque M, et al. Anatomy of deer spine and its comparison to the human spine. Anat Rec 2000; 260: 189–203. [DOI] [PubMed] [Google Scholar]
- 18.Lange T, Schmoelz W, Gosheger G, et al. Is a gradual reduction of stiffness on top of posterior instrumentation possible with a suitable proximal implant? A biomechanical study. Spine J 2017; 17: 1148–1155. [DOI] [PubMed] [Google Scholar]
- 19.Cho KJ, Suk SI, Park SR, et al. Short fusion versus long fusion for degenerative lumbar scoliosis. Eur Spine J 2008; 17: 650–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ignasiak D, Peteler T, Fekete TF, et al. The influence of spinal fusion length on proximal junction biomechanics: a parametric computational study. Eur Spine J 2018; 27: 2262–2271. [DOI] [PubMed] [Google Scholar]
- 21.Shono Y, Kaneda K, Abumi K, et al. Stability of posterior spinal instrumentation and its effects on adjacent motion segments in the lumbosacral spine. Spine (Phila Pa 1976) 1998; 23: 1550–1558. [DOI] [PubMed] [Google Scholar]
- 22.Cammarata M, Aubin CE, Wang X, et al. Biomechanical risk factors for proximal junctional kyphosis: a detailed numerical analysis of surgical instrumentation variables. Spine(Phila Pa 1976) 2014; 39: E500–E507. [DOI] [PubMed] [Google Scholar]
- 23.Hart RA, Prendergast MA, Roberts WG, et al. Proximal junctional acute collapse cranial to multi -level lumbar fusion: a cost analysis of prophylactic vertebral augmentation. Spine J 2008; 8: 875–881. [DOI] [PubMed] [Google Scholar]
- 24.Lange T, Schulte TL, Gosheger G, et al. Effects of multilevel posterior ligament dissection after spinal instrumentation on adjacent segment biomechanics as a potential risk factor for proximal junctional kyphosis: a biomechanical study. BMC Musculoskelet Disord 2018; 19: 57–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Siebert E, Pruss H, Klingebiel R, et al. Lumbar spinal stenosis: syndrome, diagnostics and treatment. Nat Rev Neurol 2009; 5: 392–403. [DOI] [PubMed] [Google Scholar]
- 26.Imagama S, Kawakami N, Matsubara Y, et al. Radiographic adjacent segment degeneration at 5 years after L4/5 posterior lumbar interbody fusion with pedicle screw instrumentation: evaluation by computed tomography and annual screening with magnetic resonance imaging. Clin Spine Surg 2016; 29: E442–E451. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-imr-10.1177_03000605211020219 for Upper and lower adjacent segment range of motion after fixation of different lumbar spine segments in the goat: an in vitro experiment by Yufu Ou, Zengming Xiao, Jianxun Wei, Hua Jiang and Zhuhai Li in Journal of International Medical Research