Abstract
Hypothesis/Background
Treatment options for the biceps brachii tendon include tenotomy, arthroscopic tenodesis, and open tenodesis. Few studies to date have compared all treatment options in the context of a rotator cuff repair.
Methods
A retrospective review of 100 patients who underwent arthroscopic supraspinatus repair between 2013 and 2018 with a minimum of one-year follow-up was performed. Patients were separated into the following 4 groups: (1) 57 had isolated supraspinatus repair with no biceps tendon surgery (SSP); (2) 16 had supraspinatus repair and biceps tenotomy; (3) 18 had supraspinatus repair and arthroscopic biceps tenodesis; (4) 9 had supraspinatus repair and an open biceps tenodesis (SSP + OT). The primary outcome was operative time. The secondary outcomes were cost analysis, complications, patient-reported outcome measures, range of motion, and strength testing.
Results
The operative time for the SSP + OT group was significantly longer than that of the SSP group (P < .05) but was not significantly longer than that of the other groups. The cost for the SSP group was significantly less than the cost for the SSP + OT and supraspinatus repair and arthroscopic biceps tenodesis groups (P < .05 for both), whereas the cost for the supraspinatus repair and biceps tenotomy group was significantly less than the cost for the SSP + OT group (P < .05). There were no significant differences between groups for complications, all patient-reported outcome measues, all range of motion, and all strength parameters.
Discussion/Conclusion
Operative time is the longest in open biceps tenodesis and is significantly longer than that of isolated supraspinatus repair. No significant differences in operative times or costs were identified in patients undergoing arthroscopic vs. open biceps tenodesis. All patients, irrespective of the type of biceps tendon procedure, had excellent clinical and functional outcomes at least one year after surgery. There was no difference in clinical or functional outcomes, or complications, among the 4 groups.
Keywords: Biceps tendon, Tenodesis, Arthroscopic, Subpectoral, Open, Outcomes
The long head of the biceps brachii tendon (LHB) is a common source of pain, especially with concomitant rotator cuff tears.2,11 Prior studies have demonstrated the incidence of LHB pathology in the setting of rotator cuff tears to be 16%-75%.3,6,16 In isolation, LHB lesions can be treated nonoperatively with rest, nonsteroidal anti-inflammatory medications, and physical therapy. However, when combined with rotator cuff pathology necessitating surgical repair, many surgeons consider addressing the LHB during concomitant rotator cuff repair. A recent retrospective review demonstrated improved patient-reported outcome scores at one year postoperative in those patients undergoing biceps tendon surgery and rotator cuff repair compared with isolated rotator cuff repair.17 Various surgical treatment options exist for LHB pathology, including tenotomy, arthroscopic tenodesis, and open tenodesis.
A recent article looking at isolated LHB lesions demonstrated both arthroscopic and open biceps tenodesis have excellent clinical and functional outcomes in a short-term follow-up.18 A randomized control trial demonstrated no significant differences in clinical outcomes between biceps tenotomy and tenodesis; however, this study included isolated LHB procedures and those with concurrent rotator cuff repairs.9 When combined with arthroscopic rotator cuff repair, arthroscopic tenodesis was shown to have greater operative time than tenotomy.19 Few studies to date, however, have compared all treatment options in the context of a rotator cuff repair.
The purpose of this study was to compare all LHB treatment options (tenotomy, arthroscopic tenodesis, and open tenodesis) in the context of a rotator cuff repair, specifically comparing operative time, cost, complications, patient-reported outcomes, and strength. The hypothesis was open biceps tenodesis would have comparable outcomes as other techniques but a significantly longer operative time and a higher complication profile.
Materials and methods
A retrospective chart review of all patients who underwent a primary rotator cuff repair by 2 fellowship-trained orthopedic sports medicine surgeons between 2013 and 2018 was performed. Inclusion criteria were defined as patients >30 years of age, an isolated supraspinatus tear, primary surgical repair of the tear, and a minimum of one-year follow-up data. Exclusion criteria included prior rotator cuff repair, prior infection to the ipsilateral shoulder, concomitant tears of the infraspinatus or subscapularis, and a follow-up less than one year. A waiver of consent was granted by the Institutional Review Board at the University of Pittsburgh.
Patients were separated into 4 groups based on biceps tendon treatment: isolated supraspinatus repair with no biceps tendon surgery (SSP group), supraspinatus repair and biceps tenotomy (SSP + tenotomy group), supraspinatus repair and arthroscopic biceps tenodesis (SSP + AT group), and supraspinatus repair and open subpectoral biceps tenodesis (SSP + OT group). Biceps tendon surgery was performed when the patient had significant bicipital groove pain on clinical examination, or there was intraoperative evidence for pathology including tenosynovitis, tearing, biceps tendon subluxation, or degenerative superior labrum anterior to posterior tear; when these findings were absent, no biceps tendon surgery was performed.
The primary outcome was operative time. Operative time was calculated from the documented incision time to final closure, which was recorded for each patient in the intraoperative records in the electronic medical record. The secondary outcomes of interest included cost analysis, complications, patient-reported outcome measures, range of motion (ROM), and strength. For the cost analysis, recent studies have reported the mean operative room cost to be $60 per minute,8,13,14 whereas implant costs are approximately $600 for the arthroscopic and open biceps tenodesis procedures. For this analysis, a complication was any infection, postoperative bicipital groove pain, revision biceps tendon surgery, and biceps tenodesis failure that occurred in the postoperative period till the most recent follow-up. For patient-reported outcome measures, the visual analog pain scale and the subjective shoulder value were measured at the final follow-up. ROM and strength consisting of the manual muscle testing scale were assessed at the final follow-up for forward flexion, external rotation, and internal rotation. ROM and strength testing were performed by the 2 operative surgeons. Demographic variables including body mass index, sex, and medical comorbidities including neurologic disease, diabetes, alcohol use, hypercholesterolemia, and tobacco use were also assessed.
To compare groups, a Kruskal-Wallis test followed by the post hoc Mann-Whitney Utest was used for continuous, nonparametric data. For categorical data, chi-square and Fisher exact tests were used. A Bonferroni correction was used for all secondary tests. A post hoc power analysis was performed for the primary outcome of surgical time for each pair-wise comparison between groups. Effect sizes of 0.56, 0.76, 1.71, 0.28, 1.11, and 0.52 resulted in a calculated power of 0.48, 0.77, 0.99, 0.12, 0.70, and 0.22 for comparison between SSP and SSP + tenotomy; between SSP and SSP + AT; SSP and SSP + OT; between SSP + tenotomy and SSP + AT; between SSP + tenotomy and SSP + OT; and between SSP + AT and SSP + OT, respectively. All statistical analyses were performed by an individual not involved with data collection or processing using SPSS, version 26 (IBM, Armonk, NY, USA). Statistical significance was set at P < .05.
Results
A total of 748 patients were reviewed; of which, 100 patients met the inclusion criteria and were included in the analysis. Of the patients excluded, 516 patients had less-than-one-year follow-up data, whereas 216 patients had concomitant infraspinatus and/or subscapularis tears. There were 57 patients in the SSP group, 16 patients in the SSP + tenotomy group, 18 patients in the SSP + AT group, and 9 patients in the SSP + OT group. There were no differences in demographic variables including body mass index, sex, and medical comorbidities between the 4 treatment groups (Table I).
Table I.
Demographic data for each bicep procedure groups.
| Factor | SSP | SSP + tenotomy | SSP + AT | SSP + OT | P value |
|---|---|---|---|---|---|
| BMI (kg/m2) | 29.9 ± 6.1 | 34.1 ± 11.0 | 26.8 ± 4.7 | 28.0 ± 3.1 | .116 |
| Sex (Male/Female) | 21/36 | 5/11 | 10/8 | 6/3 | .173 |
| Neurologic disease | 6/57 (11%) | 3/16 (19%) | 2/18 (11%) | 0/9 (0%) | .588 |
| Diabetes | 6/57 (11%) | 4/16 (25%) | 1/18 (6%) | 1/9 (11%) | .354 |
| Alcohol use | 29/57 (51%) | 5/16 (31%) | 10/18 (56%) | 6/9 (67%) | .548 |
| Hypercholesterolemia | 14/53 (26%) | 8/16 (50%) | 2/17 (12%) | 2/9 (22%) | .102 |
| Tobacco use | 8/56 (14%) | 4/16 (25%) | 4/18 (22%) | 0/9 (0%) | .358 |
BMI, body mass index.
Data reported as n/total (%) or mean ± standard deviation unless otherwise specified.
No statistically significant differences were found.
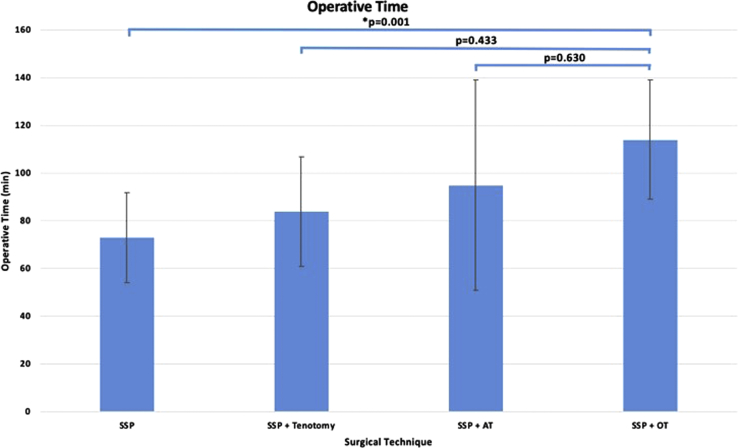
There was a statistically significant difference in operative time among groups, with the SSP + OT group having the longest operative time at 114 minutes, followed by the SSP + AT group at 94 minutes, then the SSP + tenotomy group at 84 minutes, and finally, the SSP group at 73 minutes (P < .05, Table II). When comparing among individual groups, the operative time for the SSP + OT group was significantly longer than for the SSP group (P < .05, Fig. 1) but was not significantly longer than that of the other groups (P > .05, Fig. 1).
Table II.
One-year follow-up data.
| Outcome datapoint | SSP | SSP + tenotomy | SSP + AT | SSP + OT | P value |
|---|---|---|---|---|---|
| Operative time (min) n = 92 | 73 ± 19 | 84 ± 23 | 94 ± 44 | 114 ± 25 | .00 |
| Complications (%) n = 100 | 9.0 | 1.0 | 2.0 | 1.0 | .90 |
| VAS n = 81 | 2.0 ± 2.6 | 2.5 ± 3.3 | 1.5 ± 2.2 | 0.3 ± 0.7 | .26 |
| SSV (%) n = 68 | 85 ± 15 | 89 ± 10 | 77 ± 18 | 92 ± 8 | .22 |
| ROM FF (deg) n = 98 | 161 ± 12 | 162 ± 10 | 155 ± 31 | 158 ± 8 | .68 |
| ROM ER (deg) n = 98 | 51 ± 8 | 55 ± 10 | 49 ± 9 | 53 ± 9 | .35 |
| ROM IR (level) (%) n = 91 | .13 | ||||
| T1-T12 | 80.8 | 81.4 | 66.7 | 66.7 | |
| L1-L5 | 7.1 | 12.6 | 27.8 | 22.2 | |
| Sacrum | 1.8 | 11.4 | 0 | 0 | |
| Unknown | 10.3 | 6 | 5.5 | 11.1 | |
| Strength FF (MMT, %) | .55 | ||||
| n = 93 | |||||
| 4/5 | 13.2 | 6.7 | 18.8 | 11.8 | |
| 5/5 | 86.8 | 93.3 | 81.3 | 88.2 | |
| Strength ER (MMT, %) | .90 | ||||
| n = 91 | |||||
| 4/5 | 7.7 | 6.7 | 12.5 | 0 | |
| 5/5 | 92.3 | 93.3 | 87.5 | 100 | |
| Strength IR (MMT, %) | .24 | ||||
| n = 81 | |||||
| 4/5 | 2.2 | 7.7 | 12.5 | 0 | |
| 5/5 | 97.8 | 92.3 | 87.5 | 100 |
AT, arthroscopic biceps tenodesis; deg, degrees; ER, external rotation; FF, forward flexion; IR, internal rotation; L, lumbar; min, minutes; MMT, manual muscle test; n, number of patients; OT, open biceps tenodesis; ROM, range of motion; SSP, supraspinatus repair; SSV, subjective shoulder value; T, thoracic; VAS, visual analog pain scale.
Significance set at P value < .05 (bold).
Figure 1.
Comparison of operative time by surgical technique. There was a statistically significant difference in the operative time among groups. When comparing among individual groups, the operative time was significantly longer for the SSP + OT group than for the SSP group. Error bars represent standard deviation. AT, arthroscopic biceps tenodesis; OT, open subpectoral biceps tenodesis; min, minutes; SSP, supraspinatus repair. Corrected P values for multiple comparisons are indicated between groups. Significance set at P < .05 (∗).
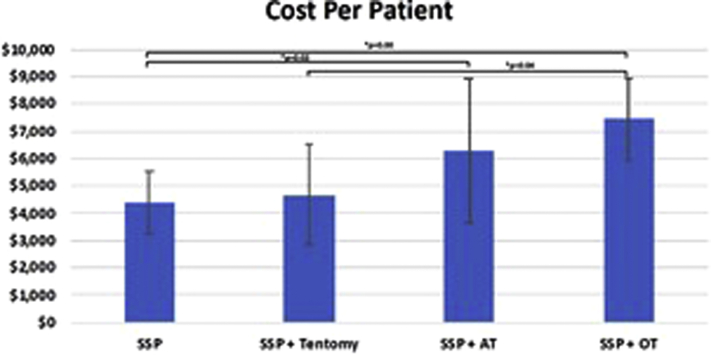
There was a statistically significant difference in cost among groups (P < .05, Table III). When comparing among individual groups, the cost for the SSP group was significantly less than the cost for the SSP + OT and SSP + AT groups (P < .05 for both), whereas the cost for the SSP + tenotomy group was significantly less than the cost for the SSP + OT group (P < .05) (Fig. 2).
Table III.
Cost analysis of the 4 groups.
| Group | N | Mean | SD |
|---|---|---|---|
| SSP | 53 | $4397 | $1120 |
| SSP + tenotomy | 15 | $4684 | $1848 |
| SSP + AT | 16 | $6274 | $2666 |
| SSP + OT | 9 | $7427 | $1515 |
| Total | 93 | $5059 | $1915 |
AT, arthroscopic biceps tenodesis; N, number of patients; OT, open biceps tenodesis; SD, standard deviation; SSP, supraspinatus repair; $, American dollars.
Figure 2.
Comparison of cost analysis by surgical technique. There was a statistically significant difference in costs among groups. When comparing among individual groups, the cost for the SSP group was significantly less than the cost for the SSP + OT and SSP + AT groups. In addition, the SSP + OT group was significantly more expensive than the SSP + tenotomy group; however, there was no significant difference in costs between the SSP + AT and SSP + tenotomy groups or between the SSP + AT and SSP + OT groups. Error bars represent standard deviation. AT, arthroscopic biceps tenodesis; OT, open subpectoral biceps tenodesis; SSP, supraspinatus repair. Corrected P values for multiple comparisons are indicated between groups. Significance set at P < .05 (∗).
The rate of complications did not significantly differ between groups (P = .90, Table II). The list of complications can be found in Table IV. There was no significant difference in visual analog pain scale or subjective shoulder value scores, ROM or strength with forward flexion, external rotation, or internal rotation among groups (P > .05, Table II).
Table IV.
Complications among the 4 groups.
| Complications | SSP | SSP + tenotomy | SSP + AT | SSP + OT | P value |
|---|---|---|---|---|---|
| Bicipital groove pain (n = 62) | 5/35 (14) | 1/10 (10) | 1/10 (10) | 0/7 (0) | .92 |
| Revision biceps tenodesis (n = 94) | 3/53 (6) | 0/15 (0) | 0/17 (0) | 0/9 (0) | 1.00 |
| Infection requiring washout (n = 100) | 0/57 (0) | 0/16 (0) | 0/18 (0) | 1/9 (11) | .90 |
| Manipulation under anesthesia (n = 100) | 3/57 (9) | 0/16 (0) | 1/18 (6) | 0/9 (0) | 1.00 |
| Total (n = 100) | 9/57 (16) | 1/16 (6) | 2/18 (11) | 1/9 (11) | .90 |
AT, arthroscopic biceps tenodesis; N, number of patients; OT, open biceps tenodesis; SD, standard deviation; SSP, supraspinatus repair.
Data reported as n/total (%).
Significance set at P value < .05.
Discussion
The main finding of this study was operative time was the longest in patients undergoing supraspinatus repair with concurrent open biceps tenodesis, followed by concurrent arthroscopic tenodesis, then concurrent tenotomy group, and finally supraspinatus repair alone. The surgical costs for patients undergoing concurrent open tenodesis were significantly more expensive than those for the concurrent tenotomy group; however, there was no significant difference in costs between the concurrent arthroscopic tenodesis and concurrent tenotomy groups or between the concurrent arthroscopic and open tenodesis groups. All patients, irrespective of the type of biceps tendon procedure, had excellent clinical and functional outcomes at least one year after surgery. There was no difference in clinical or functional outcomes, or complications, among the 4 groups.
This study found that the operative time was significantly longer for the SSP + OT group than for the SSP group, but no significant difference was identified in operative times between the other groups. Recent literature reports mixed results when discussing operative times in biceps surgery with concomitant rotator cuff repair; however, these studies do not compare arthroscopic and open biceps tenodesis. A recent prospective randomized trial reported the surgical time was approximately 10 minutes higher in the arthroscopic tenodesis group than that in the tenotomy group.19 Another prospective cohort study found similar surgical times between arthroscopic tenodesis and tenotomy.5 MacDonald et al9 conducted a prospective randomized control trial comparing tenodesis and tenotomy. The authors included isolated LHB pathology, LHB pathology with repairable rotator cuff tears, and LHB pathology with irreparable rotator cuff tears. Arthroscopic and open tenodesis methods were used; however, the results were combined into the tenodesis group and not differentiated. The authors found similar operative times between the 2 groups.9 The results from the present study demonstrated longer operative times for open tenodesis with simultaneous supraspinatus repair than supraspinatus repair alone, but interestingly, there was no statistically significant difference among the 3 biceps tendon procedures, including arthroscopic vs. open biceps tenodesis.
The difference in operative times between the groups, although not statistically significant, could have clinical and monetary implications. A recent descriptive epidemiologic study found a 15-minute increase in the operative time after arthroscopic rotator cuff repair was associated with an increased risk of short-term complications, including anemia requiring transfusion, venous thromboembolism, surgical site infection, and hospital stay duration.1 The present study found the SSP group had a mean operative time of 73 minutes, whereas the SSP + tenotomy group had 84 minutes, the SSP + AT group had 94 minutes, and the SSP + OT group had 114 minutes. The difference in time between the 4 groups could impact complications, even though this study found no significant difference in postoperative complications. In addition, this study found a significant difference in costs among the groups. When comparing individual groups, the SSP + OT group was significantly more expensive than the SSP + tenotomy group with a mean cost difference of approximately $2800. Although not statistically significant, the SSP + OT group was $1200 more expensive than the SSP + AT group, whereas the SSP + AT group was $1400 more expensive than the SSP + tenotomy group. These findings can help guide surgeons in decision-making, especially for medical circumstances in which surgical time may need to be limited.
The results of this study demonstrated no difference in clinical or functional outcomes among patients undergoing isolated supraspinatus repair, arthroscopic biceps tenodesis with simultaneous rotator cuff repair, open biceps tenodesis with simultaneous rotator cuff repair, and biceps tenotomy with simultaneous rotator cuff repair. Previous studies have evaluated outcome differences with tenotomy vs. tenodesis in the setting of rotator cuff tears5,9,10,17,19; however, no study has specifically compared all treatment options. A recent retrospective review found no difference in one-year outcomes between patients undergoing tenotomy and tenodesis in the setting of rotator cuff repair; however, the authors demonstrated greater improvement in outcomes for those patients undergoing biceps surgery vs. patients undergoing rotator cuff repair without biceps surgery.17 Another retrospective review reported decreased abduction strength in patients undergoing tenotomy with simultaneous rotator cuff repair as compared with patients undergoing tenodesis with simultaneous rotator cuff repair.10 Two recent prospective studies demonstrated equivalent outcome measures and strength at 2 years between patients undergoing tenodesis and tenotomy with concurrent rotator cuff repair but reported increased Popeye’s deformity in the tenotomy group.5,12 A prospective, randomized control trial reported equivalent outcome measures and pain scores between patients undergoing tenodesis and tenotomy; however, the authors included isolated LHB pathology and patients with concurrent rotator cuff tears.9 Various systematic reviews have found no significant functional differences between patients undergoing tenodesis and tenotomy in the setting of rotator cuff repair,4,7,15 which is in agreement with the findings in this study. There was no difference in the complication rates among the groups, which did not support our initial hypothesis. However, a significant number of patients undergoing rotator cuff repair without biceps surgery reported postoperative bicipital groove pain. Although no significant conclusions can be drawn from these findings, future studies are warranted to investigate the role in biceps surgery in all patients undergoing rotator cuff repair. Our findings suggest that the type of surgery to address biceps pathology during rotator cuff repair may be chosen based on surgeon preference and comfort level in addition to the individual clinical scenario with no effect on the rate of complications.
The strengths of the study include the comparison of all treatment types for LHB pathology in the setting of rotator cuff repair with isolated rotator cuff repair, which eliminates potential confounding variables present in many studies previously reported in the literature. In addition, all patients had isolated supraspinatus tears without concurrent subscapularis tears. This study, however, is not without limitations. This study is a retrospective review with a small number of patients; this was secondary to following strict inclusion criteria, and therefore, recruiting a larger number of patients may require a multicenter study. Further prospective studies with larger numbers may be warranted to further evaluate operative times and outcomes.
Conclusion
The operative time is the longest in open biceps tenodesis and is significantly longer than that in isolated supraspinatus repair. No significant differences in operative times or costs were identified in patients undergoing arthroscopic vs. open biceps tenodesis. All patients, irrespective of the type of biceps tendon procedure, had excellent clinical and functional outcomes at least one year after surgery. There was no difference in clinical or functional outcomes, or complications, among the 4 groups. These findings can help guide surgical decision-making when approaching LHB tendon pathology in the setting of rotator cuff tears. In addition, these findings may deter a surgeon from performing a biceps tendon procedure on all patients during rotator cuff repair, irrespective of biceps tendon pathology, as surgical timing and costs are increased. Each surgery should be individualized to the patient and the comfort level of the surgeon, with the knowledge that biceps tendon surgery is an excellent option for patients with significant biceps pathology.
Disclaimers:
Funding: No funding was disclosed by the author(s).
Conflicts of interest: Albert Lin is a paid consultant for Arthrex and Wright Medical. The other authors, their immediate family, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
A waiver of consent for this study was granted by the Institutional Review Board at the University of Pittsburgh.
References
- 1.Agarwalla A., Gowd A.K., Yao K., Bohl D.D., Amin N.H., Verma N.N. A 15-minute incremental increase in operative duration is associated with an additional risk of complications within 30 days after arthroscopic rotator cuff repair. Orthopaedic J Sports Med. 2019;7 doi: 10.1177/2325967119860752. 2325967119860752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Boileau P., Baqué F., Valerio L., Ahrens P., Chuinard C., Trojani C. Isolated arthroscopic biceps tenotomy or tenodesis improves symptoms in patients with massive irreparable rotator cuff tears. JBJS. 2007;89:747–757. doi: 10.2106/JBJS.E.01097. [DOI] [PubMed] [Google Scholar]
- 3.Chen C.-H., Hsu K.-Y., Chen W.-J., Shih C.-H. Incidence and severity of biceps long-head tendon lesion in patients with complete rotator cuff tears. J Trauma Acute Care Surg. 2005;58:1189–1193. doi: 10.1097/01.TA.0000170052.84544.34. [DOI] [PubMed] [Google Scholar]
- 4.Hsu A.R., Ghodadra N.S., Provencher C.M.T., Lewis P.B., Bach B.R. Biceps tenotomy versus tenodesis: a review of clinical outcomes and biomechanical results. J Shoulder Elbow Surg. 2011;20:326–332. doi: 10.1016/j.jse.2010.08.019. [DOI] [PubMed] [Google Scholar]
- 5.Koh K.H., Ahn J.H., Kim S.M., Yoo J.C. Treatment of biceps tendon lesions in the setting of rotator cuff tears: prospective cohort study of tenotomy versus tenodesis. Am J Sports Med. 2010;38:1584–1590. doi: 10.1177/0363546510364053. [DOI] [PubMed] [Google Scholar]
- 6.Lafosse L., Reiland Y., Baier G.P., Toussaint B., Jost B. Anterior and posterior instability of the long head of the biceps tendon in rotator cuff tears: a new classification based on arthroscopic observations. Arthrosc J Arthroscopic Relat Surg. 2007;23:73–80. doi: 10.1016/j.arthro.2006.08.025. [DOI] [PubMed] [Google Scholar]
- 7.Leroux T., Chahal J., Wasserstein D., Verma N.N., Romeo A.A. A systematic review and meta-analysis comparing clinical outcomes after concurrent rotator cuff repair and long head biceps tenodesis or tenotomy. Sports health. 2015;7:303–307. doi: 10.1177/1941738114539627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Macario A. What does one minute of operating room time cost? J Clin Anesth. 2010;4:233–236. doi: 10.1016/j.jclinane.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 9.MacDonald P., Verhulst F., McRae S., Old J., Stranges G., Dubberley J. Biceps tenodesis versus tenotomy in the treatment of lesions of the long head of the biceps tendon in patients undergoing arthroscopic shoulder surgery: a prospective Double-Blinded randomized Controlled trial. Am J Sports Med. 2020 doi: 10.1177/0363546520912212. [DOI] [PubMed] [Google Scholar]
- 10.Meraner D., Sternberg C., Vega J., Hahne J., Kleine M., Leuzinger J. Arthroscopic tenodesis versus tenotomy of the long head of biceps tendon in simultaneous rotator cuff repair. Arch orthopaedic Trauma Surg. 2016;136:101–106. doi: 10.1007/s00402-015-2343-2. [DOI] [PubMed] [Google Scholar]
- 11.Murthi A.M., Vosburgh C.L., Neviaser T.J. The incidence of pathologic changes of the long head of the biceps tendon. J Shoulder Elbow Surg. 2000;9:382–385. doi: 10.1067/mse.2000.108386. [DOI] [PubMed] [Google Scholar]
- 12.Oh J.H., Lee Y.H., Kim S.H., Park J.S., Seo H.J., Kim W. Comparison of treatments for superior labrum–biceps complex lesions with concomitant rotator cuff repair: a prospective, randomized, comparative analysis of debridement, biceps tenotomy, and biceps tenodesis. Arthrosc J Arthroscopic Relat Surg. 2016;32:958–967. doi: 10.1016/j.arthro.2015.11.036. [DOI] [PubMed] [Google Scholar]
- 13.Raft J., Millet F., Meistelman C. Example of cost calculations for an operating room and a post-anaesthesia care unit. Anaesth Crit Care Pain Med. 2015;34:211–215. doi: 10.1016/j.accpm.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 14.Shippert R.D. A study of time-dependent operating room fees and how to save $100 000 by using time-saving products. Am J Cosmet Surg. 2005;22:25–34. doi: 10.1177/074880680502200104. [DOI] [Google Scholar]
- 15.Slenker N.R., Lawson K., Ciccotti M.G., Dodson C.C., Cohen S.B. Biceps tenotomy versus tenodesis: clinical outcomes. Arthrosc J Arthroscopic Relat Surg. 2012;28:576–582. doi: 10.1016/j.arthro.2011.10.017. [DOI] [PubMed] [Google Scholar]
- 16.Walch G., Nové-Josserand L., Boileau P., Levigne C. Subluxations and dislocations of the tendon of the long head of the biceps. J Shoulder Elbow Surg. 1998;7:100–108. doi: 10.1016/s1058-2746(98)90218-x. [DOI] [PubMed] [Google Scholar]
- 17.Watson S.T., Robbins C.B., Bedi A., Carpenter J.E., Gagnier J.J., Miller B.S. Comparison of outcomes 1 year after rotator cuff repair with and without concomitant biceps surgery. Arthrosc J Arthroscopic Relat Surg. 2017;33:1928–1936. doi: 10.1016/j.arthro.2017.05.009. [DOI] [PubMed] [Google Scholar]
- 18.Werner B.C., Evans C.L., Holzgrefe R.E., Tuman J.M., Hart J.M., Carson E.W. Arthroscopic suprapectoral and open subpectoral biceps tenodesis: a comparison of minimum 2-year clinical outcomes. Am J Sports Med. 2014;42:2583–2590. doi: 10.1177/0363546514547226. [DOI] [PubMed] [Google Scholar]
- 19.Zhang Q., Zhou J., Cheng B. Tenotomy or tenodesis for long head biceps lesions in shoulders with reparable rotator cuff tears: a prospective randomised trial. Knee Surg Sports Traumatol Arthrosc. 2015;23:464–469. doi: 10.1007/s00167-013-2587-8. [DOI] [PubMed] [Google Scholar]