Résumé
Position du problème
L’épidémie de Covid-19 du printemps 2020 a fortement affecté le système de soins. Le confinement et les risques d'exposition au coronavirus ont incité les patients à modifier leur recours aux soins. L'objectif était de partager un retour d'expérience sur la mise en place d'un dispositif de surveillance en temps réel de l'activité des médecins libéraux de la région Provence-Alpes-Côte d'Azur, et de l’évolution des remboursements de médicaments prescrits aux assurés du régime général pour le diabète, pour des troubles de la santé mentale et pour certains vaccins.
Méthodes
Les données ont été extraites à partir des bases régionales de l'Assurance maladie pour les années 2019 et 2020. Elles ont permis de construire des indicateurs en date de soins pour le régime général stricto sensu, calculés de façon hebdomadaire, à partir de la semaine 2.
Résultats
On constate une chute d'activité des médecins libéraux lors du confinement (-23 % pour les médecins généralistes ; -46 % pour les spécialistes), suivie d'un quasi retour à la normale par la suite. Dans le même temps, les téléconsultations ont connu un véritable essor : elles ont constitué 30 % des actes des médecins libéraux au plus fort de la crise. Le début du confinement a été marqué par un pic d'approvisionnement en médicaments, tandis que la vaccination a fortement diminué (-39 % concernant le vaccin contre la rougeole, les oreillons et la rubéole chez les enfants de moins de 5 ans ; -54 % pour le vaccin contre les papillomavirus humains chez les filles de 10-14 ans).
Conclusion
L’épidémie de Covid-19 risque d'entraîner d'autres conséquences sanitaires que celles directement imputables à la Covid-19 elle-même. Le renoncement aux soins pourrait causer des retards de soins fortement préjudiciables aux individus et à la collectivité. Ces questions inquiètent les autorités publiques, qui mettent en place des actions visant à inciter les patients à se soigner sans tarder. Mais la crise liée à la Covid-19 a aussi créé des opportunités, telles que le déploiement de la téléconsultation et de la téléexpertise. Bien que partiels, les indicateurs mis en œuvre peuvent permettre aux décideurs publics d’être réactifs et de mettre en place certaines actions afin de répondre aux besoins de santé des populations.
Mots clés en français: Covid-19, Recours aux soins, Soins de ville, Médecins, Médicaments, Vaccination, Santé publique
Abstract
Background
The spring 2020 COVID-19 epidemic severely impacted France's healthcare system. The associated lockdown (17 March- 11 May 2020) and the risk of exposure to SARS-CoV-2 led patients to change their use of healthcare. This article presents the development and implementation of a real-time system to monitor i) private doctors’ activity in South-eastern France, and ii) changes in prescription of drugs for people with diabetes, mental health disorders and for certain vaccines from Mars 2020 to October 2020.
Methods
Data extracted from the regional healthcare insurance databases for 2019 and 2020 were used to construct indicators of healthcare use. They were calculated on a weekly basis, starting from week 2 2020 and compared for the same period between 2019 and 2020.
Results
Private doctors’ activity decreased during the spring 2020 lockdown (by 23 % for general practitioners and 46 % for specialists), followed by an almost complete return to normal after it ended until week 41. Over the same period, a huge increase in teleconsultations was observed, accounting for 30 % of private doctors’ consultations at the height of the crisis. The start of the lockdown was marked by a peak in drug prescriptions, while vaccinations declined sharply (by 39 % for the measles, mumps and rubella (MMR) vaccine in children under 5 years old, and by 54 % for human papillomavirus vaccine in girls aged 10-14 years old).
Conclusion
The ongoing COVID-19 epidemic may lead to health consequences other than those directly attributable to the disease itself. Specifically, lockdowns and foregoing healthcare could be very harmful at the individual and population levels. The latter issue is a concern for French public authorities, which have implemented actions aimed at encouraging patients to immediately seek treatment. However, the COVID-19 crisis has also created opportunities, such as the roll-out of teleconsultation and tele-expertise. The indicators described here as part of the monitoring system can help public decision-makers to become more responsive and to implement tailored actions to better meet the general population's healthcare needs.
Keywords: COVID-19, Healthcare use, Private healthcare, Doctors, Drugs, Vaccination, Public health
1. Introduction
In spring 2020, the coronavirus disease (COVID-19) epidemic severely impacted France's healthcare system, with contrasting effects on community and hospital settings. Some hospital services had to deal with a large influx of patients - most of whom were admitted for COVID-19 - while in community settings, general practitioners, specialists, and other healthcare professionals saw their practices being deserted by patients, with a resulting decrease and/or modification of their professional activity [1], [2]. The reasons why patients limited their use of healthcare were i) the country's first lockdown in spring 2020, and ii) the risks of exposure to the disease. Between March 16 and April 12, 2020, the number of consultations with general practitioners decreased by a factor of over fifteen [3]. This is why the Ministry of Social Affairs and Health issued a general guidelines sheet [4] at the beginning of April 2020, and encouraged people who required essential non-COVID-19-related care to contact their doctor so as not to unduly delay treatment, as postponing it could be harmful [5]. One study suggests that, during the lockdown, the number of heart attacks in the Paris area was twice that for the same period in previous years. The authors provided several hypotheses for this, including saturation of the overall healthcare system and the fact that medical monitoring of patients was sometimes interrupted during the lockdown period [6].
The deployment of teleconsultation (i.e., access to remote medical consultations by video) improved the continuity of care, especially for patients with chronic diseases. In order to support this deployment, the conditions for implementing and managing teleconsultation were simplified and extended over the full official nationwide health emergency period (March 23 to July 10, 2020). Specifically, as an exception to normal practice, telephone-based consultations were authorized for people diagnosed with or suspected of having COVID-19, people with official Long-Term Illness (Affection de Longue Durée (ALD)) status (a special status for which healthcare costs are completely covered by the National Health Insurance System for a specific list of illnesses), people over the age of 70, people living in areas without internet coverage, and pregnant women [7]. Between March and April 2020, the National Health Insurance System counted 5.5 million teleconsultations, 30 times more than the number between February and March 2020 [8]. Between March 23 and July 10, pharmacists were also temporarily authorized to dispense treatments to patients with renewable prescriptions that had expired (Public Health Emergency Decree, March 23, 2020).
In this exceptional health crisis context, it was essential to objectify, monitor, and quantify the changes in the use of non-hospital care, in order to both anticipate the possible consequences of these changes on public health, and to study how private doctors adapted to this situation by modifying their activities and by appropriating new tools, in particular teleconsultation. Obtaining this information in real time was critical in order to ensure that health authorities could respond quickly and tailor their response and associated interventions as closely as possible to this dynamic situation.
In order to have indicators which could be used to monitor changes in the levels and types of community healthcare use during the crisis, a real-time monitoring system was set up and implemented at the beginning of the country's first lockdown and continues today, in order to respond, among other things, to concerns about the risk of saturation of the non-hospital healthcare system, but also to concerns over patients possibly foregoing or delaying their use of healthcare. More specifically, this real-time system monitors 1) the activity (i.e., physical and remote consultations) of general practitioners and private specialists in the Provence-Alpes-Côte d'Azur region, and 2) the evolution of reimbursements for drugs prescribed to persons with diabetes, mental health disorders and certain vaccines, who live in the South-east and are covered under the National Health Insurance's General Scheme1 .
This article presents the development of the monitoring system and its results from week 2 to week 41, 2020. Apart from discussing the system in terms of public health (i.e., quantifying the general public's waiving of community healthcare use, associated risks with waiving and delaying treatment, and the use of new consultation methods), we also identify its strengths and limitations. Finally, we discuss the prospects for its future use both in crisis and non-crisis contexts.
2. Materials and Methods
2.1. Data source
Data were extracted from the Health Insurance Information System regional database (Erasme : Extraction, research and analyses for a medico-economic monitoring) for the years 2019 and 2020. Only data for insured people covered under the National Health Insurance's General Scheme were used in the tool, in order to ensure that comparisons of indicators could be made over time. More specifically, data on the other health insurance schemes (covering teachers, officials, self-employed workers, etc.) were excluded. The General Scheme covers more than 85 % of the population in the South-east [9].
In order to study the behaviours of insured persons over time, data were extracted for the date on which care was provided (date of private doctor consultation, and date that prescribed drugs were dispensed).
2.1.1. Activity of private doctors
For this dimension, the population comprised private doctors practicing in the Provence-Alpes-Côte d'Azur region, who provided care to persons covered under the General health insurance scheme. In 2020, the South-east had 5,230 private general practitioners and 6,120 private specialists [10].
2.1.2. Drug reimbursement data
For this dimension, the population comprised people covered by the General health insurance scheme affiliated to one of the six health insurance local offices (CPAM) in the South-east at the time of data extraction (3rd quarter 2020).
For each therapeutic class of drugs studied, the data extracted included all reimbursements for drugs dispensed in community pharmacies, irrespective of the type of prescribing physician (private, or hospital-based). Medicines dispensed in hospitals or nursing homes with an internal pharmacy were not taken into account in the monitoring system because this information is not available in the databases used.
The choice of which drugs/vaccines to study was primarily based on the major COVID-19-related public health issues which France faced in the spring of 2020, the associated lockdown and subsequent end of lockdown. More specifically these issues concerned i) the management of chronic pathologies (e.g., reimbursements for diabetes drugs were selected as a tracer indicator), mental health (e.g., monitoring reimbursements for psychotropic drugs), and prevention (e.g., reimbursements for vaccines). The selection of specific therapeutic classes was based on previous work on these themes [11], [12], on algorithms used in the mapping of pathologies which were developed by the National Health Insurance Fund (Caisse nationale d'Assurance Maladie (Cnam)) [13], and on a national study dedicated to drug use during the pandemic [14].
2.2. Indicators
The indicators selected as part of the development of the monitoring system were calculated weekly, from week 2 to week 41 (end date of available data for the current article) for 2020, and for the same period in 2019, in order to be able to make comparisons.
2.2.1. Indicators for private doctors’ activity
The indicators were based on the number of medical consultations performed :
-
-
For general practitioners : the number of office-based consultations, home visits, and teleconsultations.
-
-
For specialists : the number of office-based consultations and teleconsultations. We detailed data according to eight medical specialties (cardiology, endocrinology, gynaecology, nephrology, neurology, paediatrics, pneumology and psychiatry) in order to refine certain results.
The identification of consultations for patients with chronic conditions (ALD, see above) made it possible to focus on the monitoring of a particularly vulnerable population when contaminated by SARS-CoV-2, or when not provided prompt care for their chronic illness.
In addition to these weekly measurements, which provided ‘cyclical’ information by measuring the change of healthcare use from one week to the next (e.g., week N of 2020 compared with week N-1 of 2020), cumulative measures (number of consultations since week 2 of 2020) provided more ‘structural’ information by providing a ‘smoothed’ evolution over the entire period.
2.2.2. Drug reimbursement indicators
The indicators selected for this theme were :
-
-
Drug dispensing : number of insured persons with at least one reimbursement for each of the following drugs : insulin, oral antidiabetic drugs, antidepressants, anxiolytics/hypnotics, or neuroleptics ;
-
-
Vaccination : number of insured persons with at least one reimbursement for i) a pentavalent or hexavalent vaccine in children under one year old, ii) vaccination against measles and rubella or MMR vaccination in children under five years of age, and finally, iii) vaccination against the human papillomavirus (HPV) in girls aged 10 to 14 years.
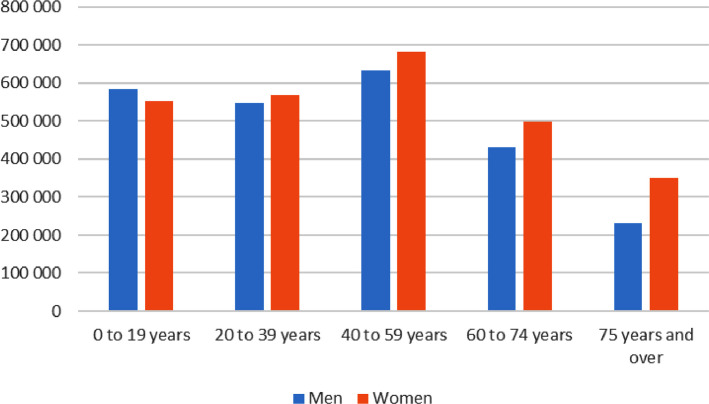
We stratified some of these indicators according to sex and age to refine certain results. Figure 1 shows the distribution of the regional population by sex and age in 2020.
Fig. 1.
Distribution of the population of the Provence-Alpes-Côte d´Azur region by sex and age in 2020
Source : INSEE
3. Results2
A sharp drop in private doctors’ activity during the spring 2020 lockdown, followed by an almost full return to normality
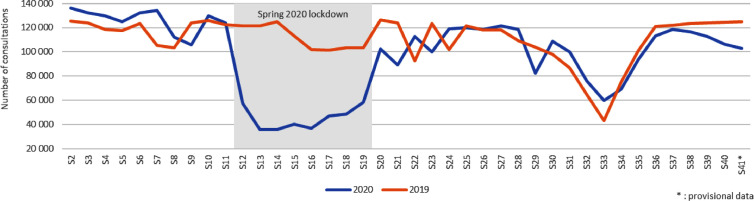
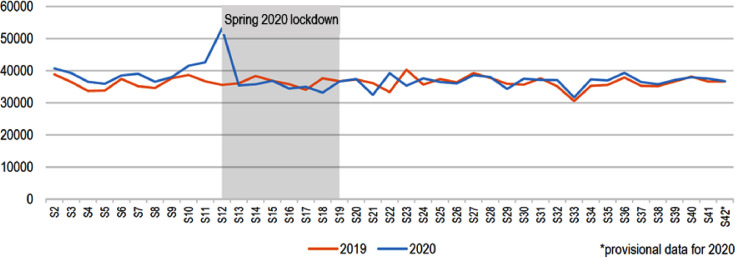
Table 1 summarizes the evolution of private doctors’ activity in the South-east at various pivotal moments in spring 2020 (before, during and after the first lockdown) compared with the same periods in the previous year. According to the data extracted from the local health insurance databases, general practitioner activity - measured by the number of medical consultations (office-based and home visits), fell by 23 % during the lockdown (week 12 to week 19) compared with the same period in 2019. Specialists’ activity fell by 46 % over this same period (Figure 2 ). The decrease in the number of consultations was especially high from the first week of the lockdown (week 12) : -23 % compared to the previous week for general practitioners, and -50 % for specialists (Figure 2).
Table 1.
Evolution in healthcare use in the Provence-Alpes-Côte d´Azur region between 2019 and 2020
| w10 (before 1st lockdown 2020) | w12 (beginning of 1st lockdown 2020) | w19 (end of 1st lockdown 2020) | w23 (1 month after 1st lockdown 2020) | w31 (3 months 1st lockdown 2020) | |
|---|---|---|---|---|---|
| Number of consultations - general practitioners | +7,3 % | -22,0 % | -32,3 % | -23,1 % | +4,0 % |
| Number of teleconsultations – general practitioners | x 78 | x 1172 | x 1103 | x 480 | x 157 |
| Number of consultations - specialists | +2,9 % | -52,8 % | -43,3 % | -18,9 % | +15,0 % |
| Number of teleconsultations - specialists | x 78 | x 2640 | x 1160 | x 279 | x 157 |
| Number of insured persons reimbursed for oral antidiabetic drugs | +7,0 % | +47,9 % | -0,6 % | -12,8 % | -1,4 % |
| Number of insured females aged girls 10-14 years old reimbursed for HPV vaccine | +7,5 % | -53,3 % | -20,8 % | -7,2 % | +25,3 % |
Reading : The number of consultations by general practitioners during week 10 (W10 - before the first lockdown) increased by 7.3 % between 2019 and 2020. Teleconsultations multiplied by a factor of 78 during week 10 of 2020, compared with the same week in 2019.
Source : Erasme (Extraction, research and analyses for a medico-economic monitoring) database (part of the Health Insurance Information system (SIAM)) - Data for date of care for persons insured under the General Health Insurance Regime.
Fig. 2.
Weekly change in the number of consultations in private specialist doctors’ offices in the Provence-Alpes-Côte d´Azur region in 2019 and 2020
From week 22 (i.e., three weeks after the end of the lockdown) onward, private doctors’ activity was close to that in 2019 : for example, for week 35, the extracted data indicated 290,000 general practitioner consultations in 2020, compared with 295,000 in 2019 (Figure 3 ). For specialists, the respective numbers were 90,000 and 100,000.
Fig. 3.
Weekly change in the total number of consulations (office-based + home visits + teleconsultations) by private general practitioners in the Provence-Alpes-Côte d´Azur region in 2019 and 2020
The more ‘structural’ approach (see above), which looked at cumulative activity over the first eight months of the year (weeks 2 to 35), complemented these results3 . More specifically, from week 2 of 2020, the overall decrease in general practitioner activity was measured at 2.7 % compared with the same period (weeks 2 to 35) in 2019. This is explained by the much higher activity in the first two months of 2020 (weeks 2 to 8) compared with 2019, and the almost full return to normal activity after the spring lockdown ended which largely offset the drop in activity during the lockdown. For specialists, activity fell more sharply over the first eight months of 2020, because of the larger decrease in their consultations during the lockdown. The percentage decrease varied greatly depending on the speciality, with only a slight dip for pneumology (-1.6 %), psychiatry (-1.8 %) and gynaecology (-3.6 %), but almost 20 % for cardiology and paediatrics. Other specialties recorded an increase in their activity from the beginning of 2020 (i.e., week 2) compared with 2019 : + 2.5 % for neurology, + 5.4 % for endocrinology, + 13.3 % for nephrology.
The rise of teleconsultation during the lockdown slowed down considerably after the end of the spring 2020 lockdown, but restarted
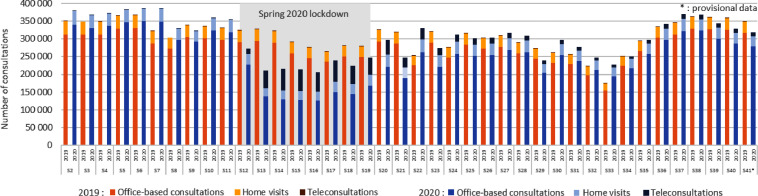
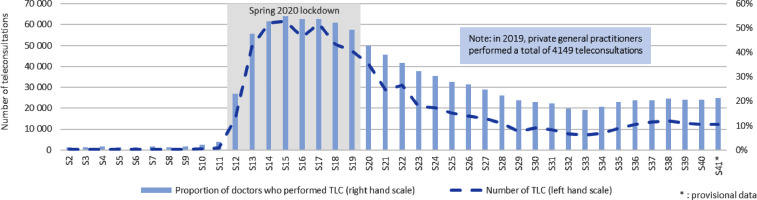
During the spring 2020 lockdown, and in particular during the peak of the first wave of the epidemic (week 15), approximately 55 % of general practitioners (Figure 4 ), and over 40 % of private specialists used teleconsultation at least once. Teleconsultations represented nearly 30 % of general practitioner consultations, and a third of specialist consultations in week 15.
Fig. 4.
Weekly change in the number of teleconsultations (TLC) and the proportion of private general practitioners who performed TLC in the Provence-Alpes-Côte d´Azur region in 2020
After the end of the lockdown, teleconsultation sharply decreased, although the number of such consultations was still higher than for the same period in 2019. From week 28 (July 6, 2020), fewer than one in five general practitioners (Figure 4) and one in fifteen specialists used teleconsultation. More specifically, teleconsultations only accounted for approximately 4 % of general practitioners’ and specialists’ consultations. This sharp decrease in teleconsultations continued until wwwk 33 (August 10, 2020), after which the number increased slightly over the following weeks (Figure 4), with their proportion of total activity of doctors increasing slightly over the last few weeks of the period covered in this article (i.e., weeks 34 to 41).
Special attention given to patients with chronic diseases
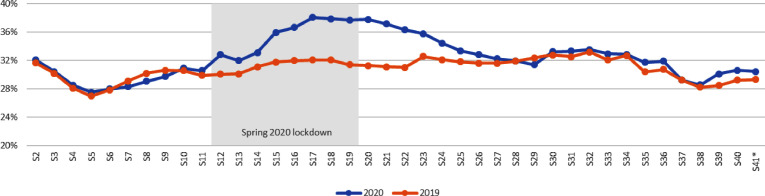
During the lockdown, the percentage of private doctors’ consultations with patients with chronic conditions (ALD, see above) was greater than that observed in 2019 for the same period. More specifically, for general practitioners, in week 11 this share was 30 % in both 2020 and 2019, increasing from week 12 onward (i.e., beginning of lockdown) to reach 38 % in week 17 (Figure 5 ) versus 32 % for the same week in 2019. It then returned to the 2019 level from week 27 onward (i.e., eight weeks after the end of the lockdown). A similar dynamic was observed for specialists, with a bell-shaped curve corresponding exactly to the lockdown period : from 21 % ALD-related consultations in week 11, to 28 % in week 12, to over 30 % in weeks 13 to 17, and finally back to 22 % in week 20 (end of lockdown week). Therefore, the number of ALD-related consultations and their share in the total activity of private physicians increased in 2020 compared with 2019, indicating greater vigilance of frail people suffering from chronic diseasesby these professionals.
Fig. 5.
Weekly change in the proportion of consultations for patients with ALD status in the total number of consultations performed by general practitioners in the Provence-Alpes-Côte d´Azur region in 2019 and 2020
A peak in personal stocking-up of drugs at the start of the lockdown
A sharp increase in drug reimbursements was observed for the week before and the week after the lockdown started (weeks 11 and 12) for diabetes drugs (insulin and oral antidiabetic drugs - Figure 6 ) and drugs for mental health symptoms and/or disorders (anxiolytics, antidepressants and hypnotics). From week 14, the numbers of people reimbursed for these drugs returned to levels similar to those of 2019, until the end of the observation period.
Fig. 6.
Weekly change in the number of insured persons who had at least one reimbursement for oral diabetes medication in the Provence-Alpes-Côte d´Azur region in 2019 and 2020
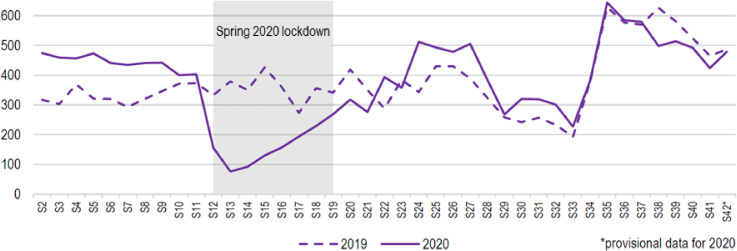
A large drop in vaccinations during the lockdown
The analyses showed a very large decrease in the administration of the studied vaccinations during the lockdownbetween weeks 12 and 19 compared with the same period in 2019, specifically 5 % for pentavalent and hexavalent vaccines in children under one year of age (i.e., approximately 900 unvaccinated children), 39 % for the MMR vaccine in children under five years of age (i.e., approximately 4,100 children), and 54 % for the human papillomavirus vaccine in girls aged between 10 and 14 years old (i.e., approximately 1,500 girls) (Figure 7 ).
Fig. 7.
Weekly trend in the number of insured females aged 10 to 14 who received at least one reimbursement for a human papillomavirus (HPV) vaccine in the Provence-Alpes-Côte d´Azur region in 2019 and 2020
From week 14, these figures gradually increased and by mid-June (week 24) they were similar to 2019 figures. No ‘catch-up’ phenomenon was observed for the drop in weeks 12 or 13.
4. Discussion
This article describes the development and implementation of a real-time monitoring system for healthcare use in South-eastern France in 2020 which is still in use today. The system objectively characterizes the impact that the COVID-19 pandemic has on healthcare use in order to allow the health authorities to act quickly in a ‘cyclical’ situation that can vary greatly from one week to the next.
With regard to the period covered by this article, in addition to the fear of negative consequences of the pandemic on the health of people with chronic diseases (such as hypertension, diabetes, certain cancers or cardiac pathologies) who did not receive necessary regular monitoring [15] despite the deployment of telemedicine, one might have expected that consultations for these illnesses would have been postponed until after the spring 2020 lockdown ended, leading to a peak of activity in general medicine, and more generally, non-hospital based healthcare. However, this was not in case, as a matter of fact, the monitoring system highlighted greater vigilance by private doctors towards these populations during the lockdown.
No catch-up in private doctors’ activity after the strong negative impact of the lockdown
Our results show a sharp drop in the activity of private doctors during the eight weeks of France's spring 2020 lockdown. No ‘catch-up’ in activity was observed after the lockdown ended ; rather, activity returned to normal, and was comparable with 2019 levels. These variations in the South-east were also observed elsewhere, for example in North-western France [16], where general practitioner consultations with patients who had chronic illnesses decreased by 41 % in patients aged under 15 years old, and 19 % in those aged 15 and over, compared with the same period the previous year.
Similarly, a survey conducted between April 9 and 21, 2020 on physicians participating in the fourth French observation panel for the practices and conditions of practice in general medicine during the lockdown [1] confirmed a decrease in general practitioners’ activity : the decrease in their average working time was estimated at between 13 and 24 % for those practicing in the week preceding the survey. Follow-up and prescription refill consultations for patients with chronic disease saw the greatest decrease, with a drop of more than 50 % for 6 out of 10 physicians, and less than 50 % for 3 out of 10. Although automatic renewal of prescriptions in pharmacies may partly explain this finding, the same argument cannot be applied for other types of consultation (paediatric follow-ups, request for healthcare following chronic disease complications, pregnancy follow-up, etc.), whose frequency should not have decreased a priori.
In the first week after the lockdown ended (week 20, 2020), the above mentioned survey in the North-west [16] found that general practitioner activity was relatively close to that observed the week before the lockdown started (week 11) for people aged 65 years and over, but not for younger populations. Likewise, another survey on general practitioners participating in the fourth observation panel, but this time for the post-lockdown period, showed a certain level of ‘catch-up’ for chronic disease-related consultations, more frequent requests mental health-related care compared to the pre-lockdown period, and less frequent paediatric follow-up than usual [17].
In terms of patients, various surveys have also characterized their healthcare-seeking behaviours. More specifically, between 28 and 38 % of adults interviewed in France in April 2020 had reduced their number of medical consultations [18], [19]. Results varied depending on the type of pathology. For one in ten chronically ill patients, fear related to COVID-19 was an especially large obstacle to having non-hospital based consultations. Similar results were found in a Belgian survey [20], where one in five people interviewed had foregone consulting their general practitioner during that country's first lockdown. Moreover, 90 % of the persons interviewed were not able to go through with a medical examination which had been scheduled before the COVID-19 crisis started. Furthermore, among those with chronic illness, nearly 23 % said that foregoing care during the lockdown had led to a ‘quite severe’ or ‘very severe’ deterioration in their health.
These findings were also found internationally : a study covering six countries (Australia, New Zealand, Canada, the Netherlands, the United Kingdom, and the United States) [21] highlighted that doctors had been on the front line during the pandemic, and that primary care for non-COVID-19 related issues had declined. Lockdowns in these countries had drastically reduced access to healthcare, which was only partially offset by telemedicine. Effectively, the priority given to COVID-19 excluded care for other pathologies.
According to a more detailed study looking only at the United States, primary care declined by 21.4 % in the second quarter of 2020 compared with the previous two years. The drop in private health professionals’ practices was 50 %, partly offset by an increase in teleconsultation. However, strong geographic disparities were observed [22]. Despite a slight rebound in activity following the spring 2020 lockdown in the USA, the postponement of consultations because of the epidemic generated “cumulative deficits” both in terms of patient care and doctors’ income [23]. These deficits were boosted by the continued decrease in the use of primary care which has been observed for several years in the country [24]. Three possible hypotheses have been put forward to explain this decrease : less patient ability, need or desire to seek care ; changes in primary care practices (more frequent teamwork, remote care) ; substitution/transfer of primary physical consultations with/to alternative offers, such as specialist consultations, specialized clinic-based care, and telemedicine.
Teleconsultation deployment and associated limitations
To fight against disruption of the care pathway caused by the COIVD-19 health crisis and associated lockdown in France, specific measures were quickly put in place, including automatic prescription renewal and teleconsultation. The considerable rise in teleconsultation observed in our results has also been confirmed by other data sources. In the general practitioner panel mentioned above, 75 % of doctors reported using teleconsultation, whether for diagnosis or for monitoring patients with COVID-19 [25]. By comparison, between October 2018 and April 2019, 86 % of general practitioners declared that they had never used teleconsultation or tele-expertise since these tools’ implementation in France in June 2018. At the national level, figures published by the National Health Insurance System [26] report massive use of teleconsultation : at the height of the pandemic's first wave in France in April 2020, more than 4.5 million teleconsultations were reimbursed by the healthcare system. For June and August 2020, these figures were 1.9 million and 650,000, respectively. Over 60,000 doctors used teleconsultation, especially general practitioners. Given that telephone consultations were exceptionally the status of teleconsultations during France's public health emergency, it is difficult to count the exact number of doctors who actually used online video-based platforms. Nevertheless, this indicator shows the responsiveness and adaptability of private doctors to guarantee follow-up for their patients, as well as the feasibility of remote follow-up within certain limits (see below). In an epidemic context, this type of care made it possible to facilitate access to care throughout all of France, particularly for the follow-up of patients with chronic pathologies, the elderly and the vulnerable [27]. Moreover, teleconsultation won the public's support. In a survey of the French general population, 5 % of those interviewed declared having used teleconsultation during the lockdown, 9 out of 10 had been satisfied with it, and the majority believed they would continue to use it after the lockdown ended [19].
However, the use of teleconsultation led to certain difficulties for general practitioners : more than half of those who used it believed that face-to-face clinical examinations are often or always essential. Slightly less than half had often or systematically encountered technical problems [25]. In fact, results from the monitoring system show that after the spring 2020 lockdown ended, teleconsultation gradually decreased in the South-east, reaching quite a low level. Nevertheless, this level was still higher than the pre-lockdown level. The end of reimbursement for telephone consultations on July 10 (as they were no longer considered teleconsultations), 2020 probably contributed in part to this decrease4 .
Again, these findings reflect international literature. In the United States, telemedicine expanded very rapidly shortly after the start of the epidemic for both COVID-19 and non-COVID-19 health problems [28], and although its use made it possible to provide care while limiting the risk of contamination linked to the spread of the virus [29], it also had limitations. A qualitative study conducted in California [30] showed that doctors appreciated the fact that telemedicine offers new opportunities to improve the quality of care provided. However, they also pointed to changes in their interactions with patients. While several of these changes were positive, it remained to be seen whether others (such as lack of physical examination and contact) could negatively impact patient-practitioner communication and patients’ propensity to disclose their concerns, two dimensions which could affect the care provided to them, and consequently their health.
The impact of the COVID-19 health crisis on drug consumption
With regard to the consumption of drugs, the results from the monitoring system were comparable with those of the ANSM [31], with a peak in personal stocking-up on drugs at the start of the first lockdown in France, followed by a return to normality for drugs for chronic pathologies, such as anti-diabetic and psychotropic drugs. The initial peak could be linked to the phenomenon of stocking-up, observed at the start of the lockdown for essential products (food, hygiene products and drugs) for fear of running out of vital resources, and to the uncertainty at the start of the lockdown containment about future access and supply.
Despite the marked psychological impact of the COVID-19 pandemic and the associated lockdown described in several studies [32], [33], [34], [35], [36], [37], [38], [39], apart from the peak stocking-up at the start the lockdown, the monitoring system's results did not show any increase in the dispensing of psychotropic drugs. More specifically, the dynamic observed was similar to that seen for antidiabetic drugs : a peak in stocking-up followed by a return to normal levels. Nevertheless, several parameters suggest that these results need to be interpreted with some caution. First, because of the structure of the National Health Insurance System's databases used in our monitoring system, only private doctors’ activities and the dispensing of drugs (even if the drug was prescribed by hospital-based doctors) could be monitored. The results therefore do not include drug consumption by hospitalized patients [40].
Second, the data extracted and analysed related to the dispensing of treatments by pharmacists, and not to actual consumption by patients. No drug dispensing does not therefore necessarily mean drugs were not consumed, as may be the case for example with hypnotics and anxiolytics. More specifically, patients may have consumed more without buying more, using old stock, or drugs prescribed to other family members’, friends, etc. Furthermore, the data used did not distinguish between new treatment initiation and continuation of an old treatment. Finally, anxiety and depressive disorders do not necessarily require first-line drug prescription. The survey of physicians participating in the fourth panel to observe practices and conditions of practice in general medicine in the first week post-lockdown [17] noted more frequent requests for mental health care. A recent report from the Ministry of Social Affairs and Health reports on lessons learned from the health crisis in the mental health and psychiatry sector, which highlighted the huge mobilization, responsiveness and inventiveness of care providers in order to adapt to this unprecedented situation [41].
The impact of the COVID-19 health crisis on vaccinations
In terms of the vaccinations studied here, the monitoring system's results are comparable with those of the French National Agency for the Safety of Medicines [31]. Specifically, the reduction in general practitioners’ consultations had an impact on prevention activity, in particular vaccination. In North-western France, a sharp drop in general medicine consultations was also observed for children under 15 years of age during the entire period of the first lockdown [16].
In our monitoring system, decreases were observed for compulsory vaccinations for children under 2 years old (the percentage decrease depending on the vaccine). A larger decrease was observed for HPV in adolescents. During the lockdown, French paediatric societies recommended i) maintaining consultations for children aged 1 month, ii) maintaining compulsory vaccine consultations for all children under 2 years old (2, 4, 5, 11, 12, 16 months) [42], [43], [44], and iii) postponing consultations for vaccination in persons over 2 years of age. These recommendations seem to have been followed better for pentavalent or hexavalent vaccinations in children under 1 year old (2, 4 and 11 months), but less well for vaccinations against measles and rubella (1st MMR dose : 12 months – 2nd dose : 16 months). Foregoing or postponing vaccination seems to have concerned children between 1 and 2 years old more than those under 1 year old.
After the lockdown ended, the HPV and measles and rubella vaccinations returned to the 2019 levels from week 23 onward. The fact that these vaccinations returned to a similar but not higher level than 2019, suggests that catch-up of the vaccines missed during the lockdown could not or could only partially be performed. This finding should encourage public authorities and the appropriate agencies to disseminate targeted messages to ensure catch-up with the vaccination schedule. It is essential to monitor vaccination coverage and the epidemic risks that may result from its temporary decline. Moreover, along with the focus and resources given to contact-tracing since the end of summer 2020 [45], maintaining adequate surveillance of other COVID-19-related risks is also essential.
Limitations
In addition to the points mentioned above on the measurement of drug consumption, other limitations should be taken into consideration when interpreting the results presented here. The monitoring system only extracted data for persons covered under the general health insurance scheme (i.e., over 85 % of the entire population in South-eastern France), in order to be able to make comparisons of indicators between 2019 and 2020. The observed phenomena may therefore have been overestimated or underestimated if healthcare use care by persons insured under other schemes was significantly different. However, results at the national level seem to point in the same direction as those observed in our monitoring system for the South-east. Moreover, it is important to point out that all of the results presented in this article were provisional. They were dependent on health professionals transmitting consultation data to the National Health Insurance System, and varied from week to week, only stabilizing over time. Nevertheless, they enabled us to see emerging trends quickly, and to measure them more accurately with some hindsight.
It would have been interesting to be able to stratify these indicators according to the specific characteristics of the people insured and of private doctors (sex, age, place of practice, etc.). However, the primary objective of the monitoring system is to be reactive, and in order not to overburden the health system's personnel who already very busy on contact-tracing, this work has not yet been carried out. It could be done in the future, in order to distinguish factors which encourage the use of healthcare in times of crisis from those which do not, as well as markers of inequalities, and to draw lessons for other potential crisis situations.
5. Conclusion and perspectives
The COVID-19 pandemic risks creating other consequences for public health than those directly attributable to the disease itself. Many hospital and non-hospital based doctors did not see their usual patients return for consultation, with many not going to hospitals or doctors’ waiting rooms for fear of being infected [46]. What has been the impact of all this on the management of, for example, cancer [36,47,48] or psychiatric care [49], [50] ? Is foregoing care likely to continue in the future, and lead to delays in care which are detrimental to the health of individuals and the general public [20] ?
The long-term effects of the crisis are particularly worrying [51] : will patients, especially those with chronic pathologies, have to bear adverse and costly consequences due to delayed treatment ? What will be the financial impact on healthcare providers’ incomes ? These questions are a concern for France's public authorities, and consequently they are actively implementing actions aimed at encouraging patients to seek treatment without delay. Example of these are the recommendations issued by the High Authority of Health (Haute Autorité de Santé (HAS)) for the post-lockdown follow-up of chronically ill patients [52], the setting up of a ‘assessment and vigilance’ consultationfor people at risk promoted by the representatives of National Health Insurance System [53], and information campaigns and incentives to go and see one's doctor quickly [54].
However, the COVID-19 crisis has also created opportunities. As data from the National Health Insurance System demonstrate, telehealth has shown its usefulness during this health crisis and is now indispensable, as it has become integrated into doctors’ professional practice. This dynamic should continue in the coming months, in particular thanks to negotiations with doctors on their contracts, aiming to accelerate the deployment of teleconsultation and tele-expertise under conditions ensuing quality in contexts where these tools are very obviously needed [26].
In the United Kingdom, new working methods emerged based on a collective and multidisciplinary approach [55], which are similar to the Professional and Territorial Health Communities (CommunautésProfessionnellesTerritoriales de Santé (CPTS)) in France [56]. By seeking to bring together the experiences and initiatives of primary care carried out internationally, authors in another study concluded : 1) that primary care played a key role in the management of the COVID-19 pandemic, thanks to the fact that it promptly adapted to an unprecedented situation ; 2) that it was necessary to strengthen primary care, by allocating adequate equipment, training and funding [57].
Although partial, the indicators we implemented in our real-time monitoring system enabled and still enable local public decision-makers to be responsive and to implement specific actions to meet the health needs of the French general population. Thanks to the rapid establishment of the indicator dashboards, the Health Regional Agency was immediately able to closely monitor the impact of the epidemic on non-hospital based medicine. The monitoring system made it possible very early on to objectify not only the size of the decrease in private doctors’ consultations activity - which had been indicated in feedback from actors on the ground - but also the rapid rise in teleconsultation. Furthermore, it reassured decision-makers that drug prescriptions for chronically ill patients were being maintained, and provided prompt warning of a decrease in vaccinations, especially for paediatric vaccines.
The Health Regional Agency and the Health Insurance System were therefore able to quickly launch communication actions with healthcare professionals, patients and vulnerable populations, to alert them to the importance of continuing to monitor chronic pathologies, pregnancies, vaccinations and of maintaining cancer screening. These dashboards were also useful in the context of regular exchanges, set up to monitor the crisis, with healthcare professionals and their representatives (Healthcare Professionals'Regional Unions(Unions régionales des professionnels de santé (URPS), etc.).
Furthermore, they made it possible to enrich discussions, complement analysis of feedback from field actors, and create a shared understanding of the spring 2020 lockdown and post-lockdown contexts. They constituted tools for dialogue which were accepted and recognized by healthcare professionals. Finally, following the results of the analyses presented here, the regional Health Insurance System set up two working groups, one on ‘mental health’ and the other on ‘vaccination’, in order to carry out reflection on the actions to be implemented and the populations to target.
In order to be made available to all stakeholders, these indicators will be integrated into the online system SirséPACA (www.sirsepaca.org), and updated regularly to monitor the development of private doctors’ activity and patients’ use of healthcare in the South-east of France. In addition, other indicators are being studied, especially concerning cancer screening. Finally, it is planned to integrate elements which will make it possible to measure social inequalities in access to non-hospital-based care in times of health crises.
Conflict of interest
No conflict of interest
Footnotes
The French version of this article has been published in the issue for June 2021 : Volume 69, Issue 3, June 2021, Pages 105-115.
France's National Health Insurance System - which includes several different schemes - provides full or partial reimbursement for health expenditures to all persons living in the country.
These results are updated and are available online in dashboards accessible on the site : http : //www.orspaca.org/covid19/tableaux-bord-covid19
The results presented in this article are provisional. They are based on the transmission of consultation information by health professionals to Health Insurance, and therefore varied from week to week. They stabilized over time : for example, at the time of data extraction presented in this article (week 43, 2020), the breakdown of consultations performed for week 8 was much more complete than that for week 34.
The reimbursement of telephone-based consultations was subsequently reinstated (through a derogation) on October 17, 2020, when a new public health emergency was announced.
References
- 1.Monziols M, Chaput H, Verger P, Scronias D, Ventelou B, et al. Comment les médecins généralistes ont-ils exercé leur activité pendant le confinement lié au Covid-19 ? Drees Études & Résultats. 2020:1150. [Google Scholar]
- 2.Assurance Maladie. Communiqué des dépenses. Les remboursements de soins du Régime Général à fin mai 2020.
- 3.Andolfatto D, Labbé D. Covid-19 : Une défaite française. Rev Politique et Parlementaire. 2020 halshs-02882877. [Google Scholar]
- 4.Ministère des solidarités et de la santé . 2020. Prise en charge hors Covid-19. [Google Scholar]
- 5.Santé Publique France . 2020. Covid-19 et continuité des soins. Continuer de se soigner, un impératif de santé publique. [Google Scholar]
- 6.Marijon E, Karam N, Jost D, Perrot D, Frattini B, Derkenne C, et al. Out-of-hospital cardiac arrest during the Covid-19 pandemic in Paris, France: a population-based, observational study. Lancet Public Health. 2020;5:437–443. doi: 10.1016/S2468-2667(20)30117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ministère des solidarités et de la santé. Covid-19: Le ministre des solidarités et de la santé autorise la téléconsultation par téléphone, pour les patients dépourvus de moyens de connexion en vidéo, 2020.
- 8.Assurance Maladie. Améliorer la qualité du système de santé et maîtriser les dépenses. Propositions de l’Assurance Maladie pour. 2021 [Google Scholar]
- 9.Direction de la Sécurité sociale . 2018. Les chiffres clés de la Sécurité sociale. [Google Scholar]
- 10.Système d'information régional en santé Provence-Alpes-Côte d'Azur : SIRSéPACA (www.sirsepaca.org)
- 11.Verger P, Cortaredona S, Tournier M, Rey D, Bendiane MK, Peretti-Watel P, et al. Psychotropic drug dispensing in people with and without cancer in France. J Cancer Surviv. 2017;11:92–101. doi: 10.1007/s11764-016-0569-9. [DOI] [PubMed] [Google Scholar]
- 12.Verger P, Fressard L, Cortaredona S, Lévy-Bruhl D, Loulergue P, Galtier F, et al. Trends in seasonal influenza vaccine coverage of target groups in France, 2006/07 to 2015/16: Impact of recommendations and 2009 influenza A (H1N1) pandemic. Euro Surveill. 2018;23 doi: 10.2807/1560-7917.ES.2018.23.48.1700801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Assurance Maladie . 2020. Méthodologie médicale de la cartographie des pathologies et des dépenses, version G7 (années 2012 à 2018) [Google Scholar]
- 14.ANSM. Covid-19 : usage des médicaments de ville en France. Rapport 4 : point de situation au 13 septembre 2020.
- 15.Mauro V, Lorenzo M, Paolo C, Sergio H. Treat all Covid-19 positive patients, but do not forget those negative with chronic diseases. Intern Emerg Med. 2020;1 doi: 10.1007/s11739-020-02395-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Observatoire régional de la santé Pays de la Loire . 2020. Recours au médecin généraliste pendant le confinement en Pays de la Loire. Épidémio Covid-19: comprendre et agir #4. [Google Scholar]
- 17.Monziols M, Chaput H, Verger P, Scronias D, Ventelou B, Barlet M, et al. Après le confinement, les médecins généralistes ne reviennent que progressivement à uneactivité normale. Drees Études & Résultats. 2020:1160. [Google Scholar]
- 18.AMGEN - Ipsos. Enquête sur l'accès aux soins et aux traitements des malades chroniques en période de confinement, 2020.
- 19.Arcane Research & EHESP . 2020. Covid-19 et confinement. Comportements, attitudes et impact sur la vie des Français. [Google Scholar]
- 20.Université Catholique de Louvain . 2020. Coronavirus : 1 personne sur 2 renonce durablement aux soins de santé. [Google Scholar]
- 21.Huston P, Campbell J, Russell G, Goodyear-Smith F., Phillips RL, van Weel C, et al. COVID-19 and primary care in six countries. BJGP Open. 2020;27(4(4)) doi: 10.3399/bjgpopen20X101128. bjgpopen20X101128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alexander GC, Tajanlangit M, Heyward J, Mansour O, Qato DM, Stafford RS. Use and Content of Primary Care Office-Based vs Telemedicine Care Visits During the COVID-19 Pandemic in the US. JAMA Netw Open. 2020;3(10) doi: 10.1001/jamanetworkopen.2020.21476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mehrotra A, Chernew M, Linetsky D, Hatch H, Cutler D. The impact of the COVID-19 pandemic on outpatient visits: practices are adapting to the new normal. The Commonwealth Fund. 2020;25 [Google Scholar]
- 24.Ganguli I, Lee TH, Mehrotra A. Evidence and implications behind a national decline in primary care visits. Journal of General Internal Medicine. 2019;34(10):2260–2263. doi: 10.1007/s11606-019-05104-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Monziols M, Chaput H, Verger P, Scronias D, Ventelou B, Barlet M, et al. Trois médecins généralistes sur quatre ont mis en place la téléconsultation depuis le début de l’épidémie de Covid-19. Drees Études & Résultats. 2020:1162. [Google Scholar]
- 26.Assurance Maladie. Téléconsultation, une pratique qui s'installe dans la durée. Communiqué de presse du 16 septembre 2020.
- 27.Genoud-Prachex T, Perrenoud MP, Guevara AB, Moser C, Bieler-Aeschlimann M, Rouaud O, et al. Télé-neuropsychologie, patients âgés et Covid-19. Rev Neuropsychol. 2020;12:178–180. [Google Scholar]
- 28.Mann DM, Chen J, Chunara R, Testa PA, Nov O. COVID-19 transforms health care through telemedicine: evidence from the field. Journal of the American Medical Informatics Association. 2020;27(7):1132–1135. doi: 10.1093/jamia/ocaa072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hollander JE, Carr BG. Telemedicine for COVID-19. New England Journal of Medicine. 2020;382(18):1679–1681. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 30.Gomez T, Anaya YB, Shih KJ, Tarn DM. A qualitative study of primary care physicians’ experiences with telemedicine during COVID-19. The Journal of the American Board of Family Medicine. 2021;34(Supplement):S61–S70. doi: 10.3122/jabfm.2021.S1.200517. [DOI] [PubMed] [Google Scholar]
- 31.ANSM . 2020. Usage des médicaments de ville en France durant l’épidémie de Covid-19 – point de situation après 5 semaines de confinement (jusqu’au 19 avril 2020) Étudepharmaco-épidémiologique à partir des données de remboursement du SNDS. [Google Scholar]
- 32.Aga SS, Khan MA, Nissar SS, Banday MZ. Évaluation de la santé mentale et des diverses stratégies d’adaptation dans la population générale vivant sous l’emprise de la Covid à travers le monde : une étude transversale. Ethics Med Public Health. 2020:15. [Google Scholar]
- 33.Allé M, Berna F, Vidailhet P, Giersch A, Mengin AC. Le confinement peut-il favoriser l’émergence de symptômes traumatiques ou psychotiques ? Rev Neuropsychol. 2020;12:196–203. [Google Scholar]
- 34.Bantman P. Quelles conséquences du Covid-19 sur notre vie psychique ? Métamorphose et transformations liées au coronavirus. L’information Psychiatrique. 2020;96:317–319. [Google Scholar]
- 35.Beck F, Léger D, Fressard L, Peretti-Watel P, Verger P, Group Coconel. Covid-19 health crisis and lockdown associated with high level of sleep complaints and hypnotic uptake at the population level. J Sleep Res. 2020:e13119. doi: 10.1111/jsr.13119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Giffard B, Joly F. Impact psychologique de l’épidémie de Covid-19 et du confinement chez des patients pris en charge pour un cancer. Rev Neuropsychol. 2020;12:193–195. [Google Scholar]
- 37.Leboyer M, Pelissolo A. Les conséquences psychiatriques du Covid-19 sont devant nous…. AnnalesMédico-Psychologiques. 2020;178:669–671. doi: 10.1016/j.amp.2020.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mengin A, Allé M, Rolling J, Ligier F, Schroder C, Lalanne L, et al. Conséquences psychopathologiques du confinement. L’encéphale. 2020;46:S43–S52. doi: 10.1016/j.encep.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Peretti-Watel P, Alleaume C, Léger D, Beck F, Verger P, Group Coconel. Anxiety, depression and sleep problems: a second wave of Covid-19. General Psychiatry. 2020;33 doi: 10.1136/gpsych-2020-100299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Villani P, Morciano C, Ambrosi P, Brondino-Riquier R, Bertault-Peres P. Prescription et consommation des médicaments hypnotiques et anxiolytiques dans les services de médecine des hôpitaux sud du CHU de Marseille. Thérapie (Paris) 2001;56:11–14. [PubMed] [Google Scholar]
- 41.Ministère des solidarités et de la santé. Rapport d'analyse des retours d'expériences de la crise Covid-19 dans le secteur de la santé mentale et de la psychiatrie, 2020.
- 42.Infovac France . 2020. Bulletin supplémentaire mars 2020. Consultation dans les cabinets médicaux recevant des enfants en période de pandémie Covid-19. [Google Scholar]
- 43.Infovac France . 2020. Bulletin supplémentaire mars 2020. Coronavirus : message à destination des familles. [Google Scholar]
- 44.Propositions de l'ensemble des sociétés savantes et organisations professionnellesr eprésentatives de la pédiatrie sur les consultations à maintenir durant la pandémie Covid-19, 2020.
- 45.Assurance Maladie. Point de situation sur le contact tracing alors que l’épidémie à Covid-19 s'accélère. Communiqué de presse du 13 octobre 2020.
- 46.Hanslik T, Flahault A. Prévention de la Covid-19 après le confinement : pour un retour rapide « à la vie d'avant ». Rev Med Interne. 2020;41:358. doi: 10.1016/j.revmed.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Héquet D, Rodrigues M, Tardivon A, Langer A, Dahan M, Rouzier M, et al. Impact de l’épidémie de Covid-19 sur les demandes de prise en charge initiale pour cancer du sein. Bull Cancer. 2020;107:620–622. doi: 10.1016/j.bulcan.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.van de Haar J, Hoes LR, Coles CE, Seamon K, Fröhling S, Jäger D, et al. Caring for patients with cancer in the COVID-19 era. Nat Med. 2020;26(5):665–671. doi: 10.1038/s41591-020-0874-8. [DOI] [PubMed] [Google Scholar]
- 49.Bocher R, Jansen C, Gayet P, Gorwood P, Laprévote V. Réactivité et pérennité des soins psychiatriques en France à l’épreuve du Covid-19. L’encéphale. 2020;46:S81–S84. doi: 10.1016/j.encep.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chevance A, Gourion D, Hoertel N, Llorca PM, Thomas P, Bocher R, et al. Assurer les soins aux patients souffrant de troubles psychiques en France pendant l’épidémie à SARS-CoV-2. L'encéphale. 2020;46:S3–S13. doi: 10.1016/j.encep.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chatterji P, Li Y. Effects of the COVID-19 Pandemic on Outpatient Providers in the US (No. w27173) National Bureau of Economic Research. 2020 [Google Scholar]
- 52.Haute Autorité de Santé . 2020. Réponses rapides dans le cadre du Covid-19. Accompagner les patients ayant une maladie chronique et/ou à risque de forme grave de Covid-19 dans la levée du confinement. [Google Scholar]
- 53.Ministère des Solidarités et de la Santé . 2020. Lancement de la consultation médicale « bilan et vigilance » pour les personnes à risque de forme grave de Covid-19 ou souffrant d’une affection de longue durée. [Google Scholar]
- 54.Azaïs B. #revoirsonmédecin : la campagne nationale lancée pour inciter les patients chroniques à consulter, site PourquoiDocteur, 11 juin 2020.
- 55.Gray R, Sanders C. A reflection on the impact of COVID-19 on primary care in the United Kingdom. J Interprof Care. 2020;34(5):672–678. doi: 10.1080/13561820.2020.1823948. [DOI] [PubMed] [Google Scholar]
- 56.Rist S, Rogez R. Les CPTS : de l’ambition politique à la réalité territoriale. Les Tribunes de la santé. 2020;63(1):51–55. doi: 10.3917/seve1.063.0051. [DOI] [Google Scholar]
- 57.Rawaf S, Allen LN, Stigler FL, Kringos D, Quezada Yamamoto H, van Weel C, et al. Lessons on the COVID-19 pandemic, for and by primary care professionals worldwide. Eur J Gen Pract. 2020;26(1):129–133. doi: 10.1080/13814788.2020.1820479. [DOI] [PMC free article] [PubMed] [Google Scholar]