Abstract
Introduction
Population health (PH) is an important component of medical school education and is required for physicians to practice effectively. Identifying the number of medical schools teaching population health and the individual curricular components could lead to a better understanding of the current status of population health implementation into medical education.
Materials and Methods
Between February and March 2019, medical schools in the USA were surveyed about the structure and content of their population health curriculum. Differences were analyzed by school funding and class size.
Results
Respondents were gathered from 28 (68%) public and 13 (32%) private schools; 27 (66%) schools having fewer than 150 students and 14 (34%) having greater than or equal to 150. Thirty-two schools (78%) had a structured PH curriculum. Seven (22%) only had a dedicated preclinical module and 33 (83%) had a longitudinal curriculum throughout multiple years of school. Many programs utilized flipped classroom models (n = 19, 46%); however, only 8 (20%) utilized standardized patients. Health disparities (100%), community health initiatives (88%), and preventative health guidelines (88%) are among the most commonly taught subjects. Quality improvement was taught by 34 of 41 programs (83%), but only sixteen (39%) schools required students to complete a quality improvement project.
Discussion
Differences in population health curricula were found between school size and funding. As evidenced by this study, most medical schools recognize the importance of population health by including it in their curriculum and a majority are incorporating the subject longitudinally into multiple years of school.
Keywords: Population health, Longitudinal curriculum, Medical education, Quality improvement, Medical school integration
Introduction
Population health (PH) contains critically important concepts for physicians to learn, as the field of medicine faces complex challenges at the national and community-based level. Encompassing a wide variety of topics, population health includes biostatistics and epidemiology, health disparities, private and public health insurance, preventative health guidelines, medical coding and billing, patient safety, quality improvement (QI), and medical malpractice. Proficiency in these subjects allows physicians to effectively communicate and treat patients. On a larger scale, physicians can influence patient-centered care by advocating for effective health policy and creating health care initiatives. However, most of this knowledge is gained through years of experience in practice, and rarely do physicians gain exposure during residency and medical school [1, 2]. Historically, these subjects have proven difficult to incorporate into an already “overcrowded” medical curriculum that is attempting to keep pace with the continuously growing field of basic sciences and clinical sciences [3, 4].
An increasing societal expectation is that physicians will be more knowledgeable about population-based issues and will make prevention a large priority [5]. The Liaison Committee on Medical Education (LCME) has made changes that reflect these growing expectations by adding PH curricular requirements into the standards for medical school accreditation [6]. The Association of American Medical Colleges (AAMC) and Centers for Disease Control (CDC) created a formal relationship through a cooperative agreement to address this topic, developing the Regional Medicine-Public Health Education Centers (RMPHECs) Initiative. Schools were awarded grants to become RMPHECs by partnering with a local and/or state health agency to improve public health and population health for their medical students [7]. Despite the urgent need, medical educators continue to struggle finding the time and resources to integrate this material into curricula, and this emerging issue is being addressed by deans of medical education throughout the nation [8–10]. Challenges include finding qualified faculty, institutional support, making changes in the current curriculum, and identifying appropriate student evaluation [6].
Medical education has been evolving, and the structure of many schools currently focuses on earlier clinical experiences, emphasis on interprofessional education opportunities, and case-based learning [11]. A recent survey by the AAMC found that 84.3% of allopathic medical schools are planning a curriculum change or the change has been implemented within the past 3 years [12]. Limited data exists that compares PH content and teaching methods between US institutions. With the rapidly changing landscape of medical education, we sought to identify how population health is currently taught in accredited allopathic medical schools in the USA, and whether breadth of PH content varies by matriculation size or sources of funding between private and public institutions.
Materials and Methods
Design
We used a cross-sectional survey methodology to obtain data about the current status of PH topics in medical school curricula at allopathic medical schools in the USA.
Participants and Setting
A total of 150 allopathic medical schools identified by the AAMC were contacted via email and asked to complete a web-based questionnaire [13]. Medical schools located in Puerto Rico and Canada were not included. The primary contact was the Associate Dean of Medical Education and the secondary point of contact was the Assistant Dean of Medical Education or the designated Educational Support Technologist. The Associate Dean was encouraged to complete the study or forward the email to a designated appointee. Email addresses were acquired through institutional websites. All survey data were collected between February 1 and March 31, 2019.
Survey Development
The survey consisted of multiple choice, multiple answer, and free-text responses. The variables were aimed at identifying core components of medical schools’ PH curriculum. Population health was defined in the survey as preventive health, evidence-based medicine, public and private insurance, social determinants of health, patient safety and health care delivery, and quality improvement. While epidemiology and biostatistics relate to PH, these topics were not included as they are universally required for United States Medical Licensing Examination (USMLE) Step 1 and Step 2 test preparation. Demographic data were self-reported by respondents regarding program matriculation size and source of school funding, whether private or public. Survey questions focused on the structure of PH in the curricula, how that material was taught (whether it was dedicated to a module or integrated throughout the curriculum), and during what years of medical school it was taught (preclinical, clinical, or both). Additional components included methods of teaching, assessment methods, faculty information, and the PH concepts covered. Schools were also asked if QI is a required project for students and to provide specific details about their project requirements.
Data Collection and Analysis
This study was exempted by the Institutional Review Board at the University of Kansas Medical Center as it was categorized as an institutional research that does not involve human subjects. Study data were collected and managed using REDCap electronic data capture tools hosted at the University of Kansas Medical Center [14, 15]. Each school was given 8 days to respond and a reminder message was sent on the seventh day. Only one response was collected from each institution. All responses were kept confidential and de-identified from the name of respondent and institution. All responses were included in the analysis. Differences between public and private institutions as well as class sizes (less than or greater than or equal to 150 students) were examined using Fisher’s exact test or Pearson’s chi-squared test as appropriate. Statistical analyses were conducted using SPSS software version 25.0 (IBM SPSS Statistics, Armonk, NY). Statistical significance was achieved with a p value < 0.05 and p values were two-sided.
Results
School Characteristics
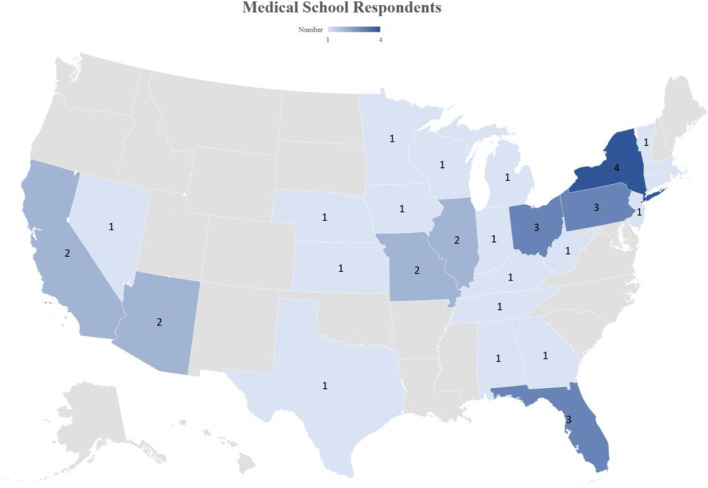
Responses were received from 41 out of 150 surveyed US allopathic medical schools (27%). Characteristics of responding medical schools can be found in Table 1. A geographical heat map representing the location of the responding schools can be found in Fig. 1. The most commonly reported class size was 99–149 students (n = 18 schools, 44%), closely aligning with the reported mean of 143 students from the American Medical Association (AMA) [13]. Twenty-eight programs which responded reported being a public institution (68%), and 13 (32%) reported they were a private institution. Twenty-seven (66%) programs had fewer than 150 students while 14 (34%) had greater than or equal to 150.
Table 1.
Characteristics of responding medical school programs
| Number of schools | Percentage | |
|---|---|---|
| Medical schools | ||
| Public | 28 | 68% |
| Private | 13 | 32% |
| Total | 41 | 100% |
| School size (number of students per class) | ||
| 0–49 | 1 | 2% |
| 50–99 | 8 | 20% |
| 99–149 | 18 | 44% |
| 150–199 | 8 | 20% |
| 200–249 | 5 | 12% |
| 250–299 | 0 | 0% |
| > 300 | 1 | 2% |
Fig. 1.
Heat map of medical school respondents in the USA
Population Health Curriculum
Thirty-two schools (78%) reported having a structured PH curriculum in place, with no significant difference between school funding (n = 21, 75% public versus n = 11, 85% private, p = 0.69) and class size (n = 22, 81% < 150 versus n = 10, 71% ≥ 150, p = 0.69). Of the 32 schools with a structured curriculum, seven (22%) reported having a dedicated PH module. All seven of these schools taught their module during the preclinical years. Most medical schools (33/41; 83%) reported their PH curriculum to be integrated longitudinally throughout multiple years of school. Among schools with integrated material, 10 (30%) reported teaching PH content during only preclinical course years, while the remaining 23 (70%) teach the content during all years of medical school. No program reported teaching this material specifically during the clinical years only. One school stated they do not teach PH topics to the entire class. Four programs indicated that they teach most material within a defined course but try to reemphasize PH as a content thread through the rest of the curriculum. When surveyed about the faculty members responsible for the PH curriculum, 29 (71%) reporting having 1–5 faculty members teaching PH content, while 4 (10%) use 6–10, and 7 (17%) have content taught by 11+ faculty members. No significant difference was found when comparing curricular involvement with 1–5 faculty versus ≥ 6 between class sizes under 150 (74.1% 1–5 faculty, 25.9% ≥ 6 faculty) and over 150 (71.4% 1–5 faculty, 28.6% ≥ 6 faculty) (p = 0.856). Twenty-six programs (63%) have the option for students to take PH as an elective course, and no statistical difference was associated with school funding (n = 17, 61% public versus n = 9, 69% private, p = 0.734) or class size (n = 15, 56% < 150 versus n = 11, 79% ≥ 150, p = 0.147).
Approaches to Population Health
Several differences were found in methods of teaching PH by funding source and class size, although not all reached statistical significance (Table 2). One school commented they teach through a service-learning project. Another school noted a scholarly concentration program that was recently implemented with help from their School of Public Health. This voluntary program includes additional didactic courses, along with the design and completion of a community public health program, to help students obtain a certificate or master’s degree in Public Health. Programs were surveyed about different methods used to assess their students’ competency in PH (Table 2). Individual responses about assessment methods included community service project, completion in problem-based and team-based learning activities, poster project, patient navigation logs with PH-focused questions, journal club participation, and group proposals/presentations for PH projects. Schools were asked to explain the different concepts covered in their PH curriculum (Table 3). One program stated their medical law and malpractice is taught in conjunction with faculty from their school of law. Two programs additionally reported teaching medical ethics in their PH curriculum and one school reported teaching Lean Six Sigma process improvement.
Table 2.
Representation of teaching methods utilized in PH education and competency methods used to assess PH education
| Total | Public | Private | p value | < 150 students | ≥ 150 students | p value | |
|---|---|---|---|---|---|---|---|
| Number of schools (%) | 41 (100) | 28 (100) | 13 (100) | 27 (100) | 14 (100) | ||
| Teaching methods | |||||||
| Small-group exercises | 38 (93) | 26 (93) | 12 (92) | 1.00* | 24 (89) | 14 (100) | .539* |
| Large-group didactics | 35 (85) | 23 (82) | 12 (92) | .645* | 22 (81) | 13 (93) | .645* |
| Standardized patients | 8 (20) | 7 (25) | 1 (8) | .398* | 8 (30) | 0 (0) | .035* |
| Project/presentation-based | 29 (71) | 17 (61) | 12 (92) | .064* | 19 (70) | 10 (71) | 1.00* |
| Self-study assignments | 23 (56) | 17 (61) | 6 (46) | .382 | 19 (70) | 4 (29) | .011 |
| Flipped classroom model | 19 (46) | 13 (46) | 6 (46) | .987 | 12 (44) | 7 (50) | .735 |
| Online lectures or modules | 17 (41) | 14 (50) | 3 (23) | .103 | 11 (41) | 6 (43) | .896 |
| Assessment methods | |||||||
| Multiple choice exam | 30 (73) | 21 (75) | 9 (69) | .719* | 19 (70) | 11 (79) | .719* |
| Essay questions | 16 (39) | 9 (32) | 7 (54) | .185 | 11 (41) | 5 (36) | .754 |
| Written report | 13 (32) | 9 (32) | 4 (31) | 1.00* | 8 (30) | 5 (36) | .734* |
| Oral report | 11 (27) | 7 (25) | 4 (31) | .719* | 3 (11) | 8 (57) | .003* |
| PowerPoint presentation | 8 (20) | 5 (18) | 3 (23) | .692* | 6 (22) | 2 (14) | .692* |
All p values determined to be statistically significant (< .05) are denoted in italic font. Differences were examined using Fisher’s exact test or Pearson’s chi-squared test as appropriate. Fisher’s exact test is denoted with an asterisk
Table 3.
Representation of concepts taught in PH curriculum
| Total | Public | Private | p value | < 150 students | ≥ 150 students | p value | |
|---|---|---|---|---|---|---|---|
| Number of schools (%) | 41 (100) | 28 (100) | 13 (100) | 27 (100) | 14 (100) | ||
| Concepts taught | |||||||
| Community health initiatives | 36 (88) | 24 (86) | 12 (92) | 1.00* | 25 (93) | 11 (79) | .317* |
| Preventative health guidelines | 36 (88) | 24 (86) | 12 (92) | 1.00* | 25 (93) | 11 (79) | .317* |
| Assessment of medical research & literature | 33 (80) | 23 (82) | 10 (77) | .692* | 21 (78) | 12 (86) | .692* |
| Public and private insurance | 32 (78) | 21 (75) | 11 (85) | .692* | 20 (74) | 12 (86) | .692* |
| Global health | 22 (54) | 12 (43) | 10 (77) | .042 | 16 (59) | 6 (43) | .318 |
| Business of medicine | 16 (39) | 10 (36) | 6 (46) | .524 | 11 (41) | 5 (36) | .754 |
| Health disparities | 41 (100) | 28 (100) | 13 (100) | 1.00* | 27 (100) | 14 (100) | 1.00* |
| Patient safety & medical error | 36 (88) | 24 (86) | 12 (92) | 1.00* | 23 (85) | 13 (93) | .645* |
| Health care delivery | 37 (90) | 24 (86) | 13 (100) | .288* | 25 (93) | 12 (86) | .596* |
| Medical law & malpractice | 22 (54) | 13 (46) | 9 (69) | .173 | 13 (48) | 9 (64) | .326 |
| Quality improvement | 34 (83) | 21 (75) | 13 (100) | .077* | 21 (78) | 13 (93) | .389* |
All p values determined to be statistically significant (< .05) are denoted in italic font. Differences were examined using Fisher’s exact test or Pearson’s chi-squared test as appropriate. Fisher’s exact test is denoted with an asterisk
Quality Improvement
Quality improvement was reported to be covered in the PH curriculum by 34 of 41 programs (83%). Sixteen (39%) programs require students to complete a QI project in their PH curriculum. A strong trend was shown for private schools covering QI in their PH curriculum more often than public schools (n = 13, 100% versus n = 21, 75%, p = 0.077), but no difference was observed in schools requiring students to complete a QI project in PH (n = 6, 46% private versus n = 10, 36% public, p = 0.524). No statistically significant difference between class sizes was observed for covering QI in the curriculum or requiring a QI project.
Three schools implemented a required QI project during clinical primary care rotations. One of these programs has students join ongoing projects with their ambulatory clinic attendings and another uses the third-year ambulatory rotation for students to complete a QI project they have been preparing for through the preclinical longitudinal PH curriculum. Another program teaches the concepts of a QI project but starts with a simple idea of a self-improvement project. Students choose something they would like to improve, such as increasing sleep and exercise, and they are required to perform a formal project that tracks the impact of two different interventions. With a more formal approach, a different university requires students to complete a QI project with a minimum of two Plan-Do-Study-Act (PDSA) cycles in their clinics. Two schools require students to identify a systems issue encountered during their clerkship rotations that is negatively impacting patient care or safety and then brainstorm potential solutions. One of these schools additionally commented that the top two solutions are voted on and presented in a team-based learning environment, with some students who choose to move forward with completing the planned project. In addition to learning the models to develop improvement projects and developing their own projects, some schools require students to assess other published QI projects and their impact. Additionally, one program also requires fourth year students to complete Institute for Healthcare Improvement (IHI) learning modules before residency.
Discussion
This study provides unique insight into population health curricula at medical schools around the country and helps identify the shift in medical education to expand curricula beyond the basic sciences and clinical care. As evidenced by respondents of this study, PH was included in most curricula for allopathic medical schools and these programs chose an integrated model taught throughout multiple years of school. The PH concepts being taught included major areas where physicians are directly involved with patient care and have potential for influential change. Quality improvement was frequently included in the education curriculum for medical students and this survey gathered details regarding heterogenous project requirements that exist between schools. Matriculation size and source of school funding did show variances between the teaching and assessment methods and the topics taught.
PH encompasses a wide array of subject matter that plays a direct role in the well-being of patients and the community. This study demonstrated significant advances that most programs (32/41; 78%) are educating future physicians in these areas, and hopefully this number continues to reach 100%. Integration has become a key component of medical education reform. Basic science learning is reinforced with early clinical exposure and placed in the context of professional practice [16]. Many of the schools surveyed reinforced this theory by responding that their PH content has been integrated longitudinally and throughout all four years of medical school. There are several benefits that come with an integration model, specifically relating to PH. These topics may be introduced more quickly, not require large blocks of time, require less faculty effort, and might demonstrate relevance more easily [6, 17]. A minority indicated their content is taught only during the preclinical years, and a common criticism of this approach is that students will not see the relevance applied to practice [16]. With clinical experience, they may be able to apply learned concepts more appropriately and have an increased understanding of their clinical application [4].
Alternative approaches to traditional lectures have been successfully utilized in medical education including the flipped classroom model [18–20] and problem-based learning (PBL) [21, 22]. This study found moderate use of these non-traditional exercises; however, only 20% (8/41) of schools are currently utilizing standardized patient encounters. Standardized patients typically prepare students with real-life scenarios, forcing them to face difficult patient situations with recorded feedback from trained faculty. Studies have shown benefits in smoking cessation counseling [23] and disclosing medical errors to patients [24]. PH scenarios could include identifying a reportable disease and initiating the report to health agencies or requiring accurate completion of a death examination and fulfillment of a death certificate [6]. Many medical schools commented on continued involvement with their public health professions program to integrate learning content across specialties. Consulting services have been created at some institutions in which the public health and population health experts “round” with medical teams to encourage the discussion of population health and prevention topics that are relevant to the patients on the ward team’s service [25].
Programs successfully reported teaching quintessential topics, such as the benefit of preventative health, community health engagement, detailed knowledge of medical insurance, and identifying social determinants of health. Areas that were less frequently taught and require future attention include global health, learning the business of medicine (i.e., in relation to sustaining an independent physician practice or medical billing), and medical malpractice. An emerging topic in PH not specifically reported in this study that requires future attention is the implementation of climate change into medical education [26, 27] and lesbian, gay, bisexual, and transgender–related content [28, 29]. Quality improvement serves as the means to systematically improve the way care is delivered to patients, by defining processes with characteristics that can be measured, analyzed, improved, and controlled. Most programs in this study reported teaching QI; however, only 39% (16/41) required project completion. Apart from working alongside local/state health agencies and politicians, QI may serve as the largest impetus to improve patient care on a population level for physicians. The Accreditation Council for Graduate Medical Education (ACGME) requires programs to educate residents in QI [30], but the heavy burden of clinical responsibilities creates a major barrier, and there is often limited time for this learning experience, let alone a finished project [31]. Early QI education in medical school would allow time for effective learning, appropriate project development, and students to potentially develop a passion for QI [32] that could be continued in the future.
One limitation of this study is that responses were not received from all allopathic medical schools. The limited sample size (27%) makes it difficult to extrapolate conclusions when such a large portion of medical schools did not respond. However, groups were well-balanced between public and private schools and between class sizes, which does allow for accurate comparisons between groups. Responses by members in the department of medical education may have introduced bias between individuals with different levels of job experience. This study focused on quantitative discrete responses with limited open-ended questions, and future studies could include one-on-one interviews or focus groups with faculty members to provide qualitative information. Population health can be a difficult subject to define; however, we suspect most experienced medical educators are familiar with these terms [5]. This study primarily focused on curricular components of PH, but additional study about perception from current students and efficacy from graduated students that are in practice would be important.
Conclusion
Expectations are growing for physicians to employ population health management, and our study reflects that medical school curricula are adapting to this need. While many schools are teaching PH, clearly the topics and curricular requirements vary widely. A potential approach to educating students in PH would be a standardized PH curriculum that has clear objectives and requirements with defined assessment methods. This may prove to be challenging but could be more effective. Medical schools may benefit from diversifying educational content by mirroring current events in culture, politics, and the economy, while continuously using innovative teaching methods to increase student engagement. There is population health content implemented in a variety of ways into medical education giving encouragement that future physicians will possess the tools necessary to handle the complexities of our growing health care system.
Acknowledgments
We would like to acknowledge the following individuals for help with this groundwork article: Giulia Bonaminio, PhD; Luke Barnard, MD; Aubrie Finlay, MD; Joe Thelen, MD; Alex Visk, MD; Christina Magnifico, MLS; Catherine Satterwhite, PhD, MSPH, MPH; Edward Ellerbeck, MD, MPH.
Data Availability
Data from this study can be made available by reasonable request.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
This study was exempted by the Institutional Review Board at the University of Kansas Medical Center as it was categorized as an institutional research that does not involve human subjects.
Code Availability
Not applicable.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Agrawal JR, Huebner J, Hedgecock J, Sehgal AR, Jung P, Simon SR. Medical students’ knowledge of the U.S. health care system and their preferences for curricular change: a national survey. Acad Med. 2005;80(5):484–488. doi: 10.1097/00001888-200505000-00017. [DOI] [PubMed] [Google Scholar]
- 2.King BF, Kindig RC, Noah WH, Tuteur PG. Internal medicine chief residents suggest need to improve health care delivery and public policy education. Internal Medicine Center to Advance Research and Education. Internist. 1990;31(7):suppl 3–suppl15. [PubMed] [Google Scholar]
- 3.Ruis AR, Golden RN. The schism between medical and public health education: a historical perspective. Acad Med. 2008;83(12):1153–1157. doi: 10.1097/ACM.0b013e31818c6583. [DOI] [PubMed] [Google Scholar]
- 4.Finkel ML. Integrating the public health component into the medical school curriculum. Public Health Rep. 2012;127(2):145–146. doi: 10.1177/003335491212700201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gourevitch MN. Population health and the academic medical center: the time is right. Acad Med. 2014;89(4):544–549. doi: 10.1097/acm.0000000000000171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mahoney JF, Fox MD, Chheda SG. Overcoming challenges to integrating public and population health into medical curricula. Am J Prev Med. 2011;41(4 Suppl 3):S170–S175. doi: 10.1016/j.amepre.2011.06.025. [DOI] [PubMed] [Google Scholar]
- 7.Maeshiro R. Responding to the challenge: population health education for physicians. Acad Med. 2008;83(4):319–320. doi: 10.1097/ACM.0b013e318166ae9f. [DOI] [PubMed] [Google Scholar]
- 8.Sachdeva AK. Faculty development and support needed to integrate the learning of prevention in the curricula of medical schools. Acad Med. 2000;75(7):S35–S42. doi: 10.1097/00001888-200007001-00006. [DOI] [PubMed] [Google Scholar]
- 9.Contemporary issues in medicine-medical informatics and population health: report II of the Medical School Objectives Project. Acad Med. 1999;74(2):130–41. [PubMed]
- 10.Maeshiro R, Koo D, Keck CW. Integration of public health into medical education: an introduction to the supplement. Am J Prev Med. 2011;41(4 Suppl 3):S145–S148. doi: 10.1016/j.amepre.2011.07.010. [DOI] [PubMed] [Google Scholar]
- 11.Rasouli T. How medical education is changing. In: Policy Priorities to Improve the Nation’s Health. Association of American Medical Colleges. 2016. https://www.aamc.org/advocacy-policy/priorities. Accessed 15 Nov 2019.
- 12.Curriculum change in US medical schools: implementation of change in 2017-2018. In: Curriculum Reports. Association of American Medical Colleges. 2018. https://www.aamc.org/data-reports/curriculum-reports/interactive-data/curriculum-change-us-medical-schools. Accessed 20 Nov 2019.
- 13.U.S. Medical School Applications and Matriculants by School, State of Legal Residence, and Sex, 2018-2019. In: 2019 FACTS: Applicants and Matriculants Data. Association of American Medical Colleges. 2018. https://www.aamc.org/data-reports/students-residents/interactive-data/2019-facts-applicants-and-matriculants-data. Accessed 20 Dec 2019.
- 14.Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;103208:103208. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Quintero GA, Vergel J, Arredondo M, Ariza MC, Gomez P, Pinzon-Barrios AM. Integrated medical curriculum: advantages and disadvantages. J Med Educ Curric Dev. 2016;3:JMECD.S18920. doi: 10.4137/jmecd.S18920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brill JR, Chheda SG, Rusch RB, Seibert CS. A mapping process for identifying and enhancing public health education in required medical student clerkships. Am J Prev Med. 2011;41(4 Suppl 3):S304–S305. doi: 10.1016/j.amepre.2011.06.008. [DOI] [PubMed] [Google Scholar]
- 18.Liebert CA, Mazer L, Bereknyei Merrell S, Lin DT, Lau JN. Student perceptions of a simulation-based flipped classroom for the surgery clerkship: a mixed-methods study. Surgery. 2016;160(3):591–598. doi: 10.1016/j.surg.2016.03.034. [DOI] [PubMed] [Google Scholar]
- 19.Morgan H, McLean K, Chapman C, Fitzgerald J, Yousuf A, Hammoud M. The flipped classroom for medical students. Clin Teach. 2015;12(3):155–160. doi: 10.1111/tct.12328. [DOI] [PubMed] [Google Scholar]
- 20.Lew EK. Creating a contemporary clerkship curriculum: the flipped classroom model in emergency medicine. Int J Emerg Med. 2016;9(1):25. doi: 10.1186/s12245-016-0123-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Neville AJ. Problem-based learning and medical education forty years on. A review of its effects on knowledge and clinical performance. Med Princ Pract. 2009;18(1):1–9. doi: 10.1159/000163038. [DOI] [PubMed] [Google Scholar]
- 22.Koh GC-H, Khoo HE, Wong ML, Koh D. The effects of problem-based learning during medical school on physician competency: a systematic review. Can Med Assoc J. 2008;178(1):34–41. doi: 10.1503/cmaj.070565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Herold R, Schiekirka S, Brown J, Bobak A, McEwen A, Raupach T. Structured smoking cessation training for medical students: a prospective study. Nicotine Tob Res. 2016;18(12):2209–2215. doi: 10.1093/ntr/ntw191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Raper SE, Resnick AS, Morris JB. Simulated disclosure of a medical error by residents: development of a course in specific communication skills. J Surg Educ. 2014;71(6):e116–e126. doi: 10.1016/j.jsurg.2014.06.020. [DOI] [PubMed] [Google Scholar]
- 25.Maeshiro R. Public health practice and academic medicine: promising partnerships regional medicine public health education centers--two cycles. J Public Health Manag Pract. 2006;12(5):493–495. doi: 10.1097/00124784-200609000-00018. [DOI] [PubMed] [Google Scholar]
- 26.Wellbery C, Sheffield P, Timmireddy K, Sarfaty M, Teherani A, Fallar R. It’s time for medical schools to introduce climate change into their curricula. Acad Med. 2018;93(12):1774–1777. doi: 10.1097/acm.0000000000002368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Maxwell J, Blashki G. Teaching about climate change in medical education: an opportunity. J Pub Health Res. 2016;5(1):673. doi: 10.4081/jphr.2016.673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Obedin-Maliver J, Goldsmith ES, Stewart L, White W, Tran E, Brenman S, Wells M, Fetterman DM, Garcia G, Lunn MR. Lesbian, gay, bisexual, and transgender-related content in undergraduate medical education. JAMA. 2011;306(9):971–977. doi: 10.1001/jama.2011.1255. [DOI] [PubMed] [Google Scholar]
- 29.Eckstein MA, Newsome CC, Borrego ME, Burnett A, Wittstrom K, Conklin JR. A cross-sectional survey evaluating transgender-related care education in United States pharmacy school curricula. Curr Pharm Teach Learn. 2019;11(8):782–792. doi: 10.1016/j.cptl.2019.04.005. [DOI] [PubMed] [Google Scholar]
- 30.Massagli TL, Zumsteg JM, Osorio MB. Quality improvement education in residency training: a review. Am J Phys Med Rehabil. 2018;97(9):673–678. doi: 10.1097/phm.0000000000000947. [DOI] [PubMed] [Google Scholar]
- 31.Jones AC, Shipman SA, Ogrinc G. Republished: Key characteristics of successful quality improvement curricula in physician education: a realist review. Postgrad Med J. 2015;91(1072):102–113. doi: 10.1136/postgradmedj-2014-002846rep. [DOI] [PubMed] [Google Scholar]
- 32.Abdel MM. Quality Improvement in Medical Education: Implications for Curriculum Change. Acad Med. 2017;92(4):431–432. doi: 10.1097/acm.0000000000001600. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data from this study can be made available by reasonable request.