Abstract
Objective
To implement a collaborative statewide antibiotic stewardship initiative in both the ambulatory and inpatient settings.
Methods
Five participating Delaware health systems each convened internal team(s) to translate the vision set forth by the eBrightHealth LLC Choosing Wisely Work Group into clinical action through process improvement efforts at their institutions. The teams focused on implementing antibiotic time-outs, and on improving antibiotic prescribing for upper respiratory infections in ambulatory settings. The learning network utilized an “all teach, all learn” methodology via monthly conference calls and quarterly face-to-face meetings.
Results
All inpatient teams implemented antibiotic time-outs for at least 1 unit. Other interventions included commitment posters; submitting antibiotic utilization data nationally; provider/patient surveys; local stewardship champions; and provider prescribing data feedback. Barriers to implementation included competing priorities, lack of reliable utilization data, and suboptimal provider engagement. Overall antibiotic utilization decreased by 9%, compared to the pre-intervention period.
Conclusions
This initiative has demonstrated the value of multidisciplinary teams, from varying healthcare systems, coming together to work on a single project. While each team’s interventions and specific goals differed slightly, all teams implemented new initiatives to promote appropriate use of antibiotics.
Policy Implications
Antibiotic stewardship is a national priority. Acute care hospitals are required to have antibiotic stewardship programs; similar programs are proposed for ambulatory settings.
Introduction
In 2016, five Delaware hospital systems (Bayhealth, Beebe Healthcare, Christiana Care Health System, Nanticoke Health Services and Nemours/Alfred I. duPont Hospital for Children) developed a statewide strategic alliance named eBrightHealth LLC. The goals of eBrightHealth LLC are to increase access to health care services, to improve the quality and affordability of care, and to offer all Delawareans an even brighter health care future through collaboration and innovation. The alliance builds on the foundation and strengths of the statewide eBrightHealth Accountable Care Organization (ACO), which includes approximately 300 primary care and 900 specialist providers who are working together to deliver high quality care at a lower cost for traditional Medicare beneficiaries across the region. The network includes both employed and affiliated providers. The partners included in eBrightHealth LLC differ slightly from those of eBrightHealth ACO (see Figure 1).
Figure 1.

Health system partners participating in eBrightHealth LLC Strategic Alliance, and eBright Health Accountable Care Organization (ACO).
One of the early innovations eBrightHealth LLC (hereafter referred to as eBH) chose to focus on was to implement recommendations from the national Choosing Wisely campaign to avoid wasteful or unnecessary medical tests, treatments and procedures, thus promoting better care and higher efficiencies. More than 80 professional societies and other partners have submitted lists with recommendations for tests and procedures “whose necessity should be questioned or discussed.”1 The eBH Choosing Wisely Work Group decided to pursue antibiotic stewardship as its initial focus, given that antibiotic recommendations represented more than 30 items on the Choosing Wisely lists, across multiple primary care and specialty societies. Concurrently, the Work Group learned that others in the state were focusing on this topic and invited them to be collaborative partners in this state-wide effort. They included Quality Insights, the Quality Innovation Network-Quality Improvement Organization (QIN-QIO) for Delaware, New Jersey, Pennsylvania, West Virginia and Louisiana, who had been awarded a contract from the Centers for Medicare and Medicaid Services (CMS) to work on improving antibiotic stewardship best practices among all providers within the represented states; and the Delaware Division of Public Health (DPH), who had received grant funding to support antibiotic stewardship efforts in the state.
Antibiotic stewardship refers to programs, policies and actions designed to optimize treatment of infections while reducing adverse events associated with antibiotic use.2 More than half of all hospitalized patients receive at least one antibiotic during their stay,3 and enough antibiotics are dispensed from outpatient pharmacies in the U.S. each year for five out of every six people to receive one antibiotic prescription.4–6 While antibiotics have transformed the practice of medicine, approximately 30-50% of all antibiotics prescribed in the U.S. are either unnecessary or inappropriate.7 Based on available data, Delaware appears to have higher than average antibiotic prescribing practices. In 2016, 929 antibiotic prescriptions per 1000 population were dispensed by community and mail-order pharmacies in Delaware, above the national average of 836 per 1000 population.5 These represent prescriptions filled at the time of hospital discharge, as well as those prescribed in the context of outpatient visits or via telephone consultation. The Centers for Disease Control and Prevention (CDC) has published what they consider to be Core Elements of hospital antibiotic stewardship programs8 (Table 1); similar documents have also been published for long term care settings10 and ambulatory care.9 As of 2016, 75% of Delaware hospitals reported meeting all seven hospital core elements, greater than the national average of 64%.11 However, the goal is to achieve 100% by 2020. Most hospital antibiotic stewardship programs, including all of those in Delaware prior to the eBH Choosing Wisely initiative, have focused primarily on inpatient utilization; however, more than 60% of all antibiotic expenditures in humans in the U.S. are related to care received in outpatient settings.12
Table 1. Core Elements of Hospital and Outpatient Antibiotic Stewardship programs, proposed by the Centers for Disease Control and Prevention (CDC).
| Core Elements of Hospital Antibiotic Stewardship Programs8 | Core Elements of Outpatient Antibiotic Stewardship9 |
|---|---|
| 1. Leadership Commitment: Dedicating necessary human, financial and information technology resources. | Commitment: Demonstrate dedication to and accountability for optimizing antibiotic prescribing and patient safety. |
| 2. Accountability: Appointing a single leader responsible for program outcomes. | Action: Implement at least one policy or practice to improve antibiotic prescribing, assess whether it is working, and modify as needed |
| 3. Drug Expertise: Appointing a single pharmacist leader responsible for working to improve antibiotic use. | Tracking and reporting: Monitor antibiotic prescribing practices and offer regular feedback to clinicians, or have clinicians assess their own antibiotic prescribing practices themselves. |
| 4. Action: Implementing at least one recommended action. | Education and expertise: Provide educational resources to clinicians and patients on antibiotic prescribing, and ensure access to needed expertise on optimizing antibiotic prescribing. |
| 5. Tracking: Monitoring antibiotic prescribing and resistance patterns | |
| 6. Reporting: Regular reporting information on antibiotic use and resistance to doctors, nurses and relevant staff. | |
| 7. Education: Educating clinicians about resistance and optimal prescribing. |
Based upon this information, the Work Group’s initial focus was to implement a collaborative statewide antibiotic stewardship initiative in both inpatient and ambulatory settings. To facilitate this effort, the Work Group decided to initially narrow the focus to treatment of upper respiratory infections (URI) in the ambulatory setting, and the implementation of an “antibiotic time-out” after 48-72 hours of antibiotics. The intention of an antibiotic time-out is to encourage data review, enhance documentation, and provide clarity amongst multiple caregivers. Improved documentation and clarity allows for increased knowledge about the patient and disease state, facilitating antibiotic de-escalation or discontinuation if appropriate, efficient and smooth transitions in care, and appropriate discharge planning. Upper respiratory conditions were chosen as the initial target because they are commonly caused by viruses (including the common cold, viral sore throats, and bronchitis) and thus do not require antibiotics, or do so only under specific circumstances (such as some sinus and ear infections).4
Methods
The Collaborative Statewide Antibiotic Learning Network
The eBH Choosing Wisely Work Group developed the infrastructure to lead and support a collaborative statewide learning network. They brought together both national and other statewide organizations with an interest in promoting antibiotic stewardship (e.g., American Board of Internal Medicine [ABIM] Foundation, the Delaware Health Information Network [DHIN], DPH, CareLink-CareNow, and Quality Insights); thereby enabling the coordination of efforts and messages to both the provider community and the broader communities in Delaware. In addition to the eBH organizations, other Delaware health systems that are not members of eBH were invited to participate in this learning network.
Each participating health system was asked to convene an internal team to translate the vision set forth by the Work Group into clinical action through process improvement efforts at their institutions. The benefit of participation for each team was the collaborative environment that enabled learning from one another, and teaching one another (“all teach, all learn”). This was accomplished primarily through monthly facilitated teleconference calls with all institutional team leads. Additionally, there were quarterly face-to-face meetings for all team members. These meetings were structured with a plenary speaker and breakout sessions where the attendees were taught process improvement skills, and had facilitated discussions on implementation tactics that included direct application of the day’s learning to their individual projects. The project initially kicked off with a face-to-face meeting in August 2017, and concluded in August 2018; however, each institution has continued their internal work groups, and collaboration has continued via teleconference and in-person meetings, supported by the Healthcare-associated Infections Advisory Committee under DPH.
Throughout this initiative, Quality Insights distributed resources to all participating providers (including not only the eBH Choosing Wisely teams, but also urgent care centers, physician practices, and community pharmacies throughout Delaware) and met one-on-one with providers to review the CDC Core Elements and provide guidance on strategies to implement them. Additionally, Quality Insights created provider-specific antibiotic prescribing reports using Medicare claims data for participating providers. Lastly, they developed patient-focused educational videos and handouts supporting appropriate antibiotic use. In addition, the teams reviewed and selected resources from CDC’s “Be Antibiotics Aware”13 and the ABIM Foundation’s Choosing Wisely® campaigns.1
Structure and Activities of Individual Teams
The five participating hospitals convened six stewardship teams (Christiana Care created separate inpatient- and outpatient-focused teams). Of these six teams, most (n=4) included an infectious diseases (ID)-trained pharmacist, and three included ID-trained physicians. All teams comprised of both pharmacist and physician representatives, who included specialists such as hospital medicine and primary care. Infection Preventionists were also common members (n=4); other individuals included nurses and Quality/Safety representatives.
Prior to the initiation of the eBH Choosing Wisely project, all participating hospitals had inpatient stewardship teams already working on various initiatives (Figure 2). These initiatives included restricting certain antibiotics to specific providers, retrospective audit and feedback, requiring an indication for antibiotic prescriptions, making changes within the electronic medical record (EMR) to facilitate stewardship goals, guidelines development, and patient and provider education. One team had signed up to participate in the Agency for Healthcare Research and Quality (AHRQ) Safety Program for Improving Antibiotic Use.14,15 During the eBH Choosing Wisely project, many of these previous initiatives were either maintained or newly introduced at other hospitals. Additionally, new stewardship interventions were initiated (Figure 2). All inpatient teams implemented an antibiotic time-out at 48-72 hours, a main goal of the project. Other interventions included developing and posting commitment posters, an evidence-based practice in which the provider(s) pledge to use antibiotics appropriately and these pledges are posted in exam rooms or other areas visible to patients;16 submitting antibiotic utilization data to CDC for benchmarking; surveying providers and/or patients; identifying stewardship champions at the clinic or unit level; and providing prescribing data feedback to providers.
Figure 2.
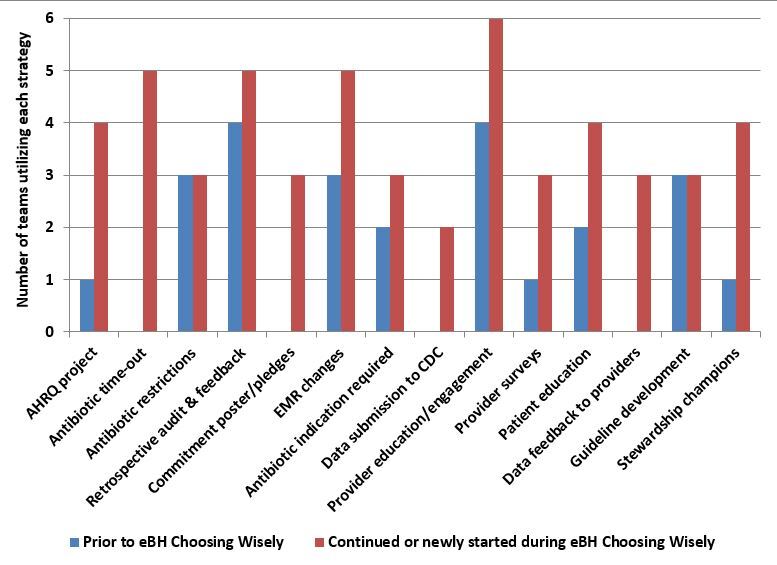
Antibiotic stewardship interventions in place prior to the eBrightHealth Choosing Wisely initiative (blue bars), and either continued or initiated during the project (red bars).
Legend: AHRQ, Agency for Healthcare Quality and Research; eBH, eBrightHealth LLC Strategic Alliance; CDC, Centers for Disease Control and Prevention; EMR, electronic medical record.
It was well-recognized by all participants that patient education was an important part of this initiative, as real or perceived demand for antibiotics is considered a primary driver of inappropriate antibiotic prescriptions.17–19 Teams reported that prior to the project, patient education included handouts (n=2), posters in waiting rooms (n=3), and education embedded into the EMR that was available for nursing to distribute to patients (n=3). Additional methods that were utilized during the project included updating an external website (n=1), creating videos (n=2), and creating phone messages for patients while waiting on hold (n=1). In addition, more programs added handouts, posters and other signage, and EMR-based education.
Individual Program Vignettes
Bayhealth
Bayhealth’s inpatient goal was to implement an antibiotic time-out to reduce antibiotic patient days by 10% in one year, and to improve patient outcomes including Clostridium difficile, readmission, and excess length of stay. This effort included participating in the AHRQ program in the intensive care unit (ICU). A dedicated pharmacist was assigned to complete the time-out for 10 patients per month, hoping that selecting a single pharmacist would increase rapport with the ICU intensivist team. The team also implemented a best practice alert in the EMR for a 72-hour antibiotic time-out for all inpatients receiving piperacillin/tazobactam or ceftriaxone. This time-out would alert only the attending hospitalist. The outpatient initiative’s goal was to reduce the number of outpatient antibiotic prescriptions for the treatment of URI (sinusitis, acute bronchitis, otitis media, and pharyngitis) by 10% over one year. Efforts toward this goal included displaying patient education posters in the emergency department (ED) fast-track rooms and patient bathrooms. Provider education targeted internal medicine and other primary care physicians via letters and staff meetings about decreasing antibiotic use for URI.
Beebe Healthcare
The Beebe team’s overarching goal was to develop and sustain a culture of optimal antimicrobial use throughout the health system. The team recruited ID and hospitalist provider champions, trained pharmacists via certification through the Society of Infectious Diseases Pharmacists (SIDP),20 and identified the medical-surgical ICU – as the area with greatest opportunity – to participate in the AHRQ Safety Program for Improving Antibiotic Use. The team used adaptive training via TeamSTEPPS,21 clinical education via monthly webinars, and standardized real-time reviews of antibiotic use employing the AHRQ four moments of antibiotic decision making.14 Quality Insights webinars were made available to hospital and outpatient providers, and Choosing Wisely commitment posters were placed strategically in both hospital and outpatient settings. The team implemented an EMR tool to submit antibiotic use and antibiotic resistance to the CDC, and conducted data analysis and timely feedback for specific antibiotics (e.g., mainly focusing on broad spectrum carbapenem usage, specifically ertapenem). The team conducted C. difficile deep dives for all hospital onset cases, as well as 1:1 meetings when opportunities for provider feedback and education were identified.
Christiana Care Health System– Ambulatory
The ambulatory team chose two key areas of focus: the health system’s five urgent care centers, known as medical aid units (MAUs), and primary care practices. Within the MAUs, the lead physician served as a stewardship champion. After on-site education by the stewardship team to MAU providers, the lead physician performed manual chart audits in order to review antibiotic prescribing, and gave the MAU providers feedback via email or in-person meetings. Antibiotic utilization data became available in February 2018, and from this point forward emails were distributed monthly to all MAU providers with their antibiotic prescribing rates, allowing for peer-to-peer comparison.
For the system’s 14 primary care practices, similar efforts were made to emphasize the importance of using antibiotics appropriately. Unfortunately antibiotic utilization data was not available for these practices, so efforts focused on provider engagement and education and patient education. The team distributed needs assessment surveys to all primary care providers, nurses, and medical assistants to gain a better understanding of the groups’ baseline knowledge. The survey identified barriers to appropriate antibiotic prescribing that included lack of access to educational materials. Therefore, the team made educational resources more readily available within the practices. Posters and pamphlets that were developed by CDC and Choosing Wisely were made available in the practices’ ordering system, and the task force developed a commitment letter that was posted in all exam rooms. Additional patient education efforts included developing a patient-focused external website, a phone recording that patients will hear when calling to request a sick visit appointment, in-person provider education at monthly clinic meetings at all sites, provider quizzes, creating a new sinusitis guideline, and identifying an office stewardship champion at each site.
Christiana Care Health System – Inpatient
The primary goal of the inpatient team was the incorporation of an antibiotic time-out into the rounding process with a focus on the 5D’s of stewardship – discernment, drug, dose, de-escalation and duration of therapy. The team completed a pilot in the fall of 2017 with the help of medical residents, who completed a separate antibiotic time-out note for 29 patients over a period of two weeks. While the process was not overly time-consuming or difficult, the lack of ability to force this function created limitations. The team also had the opportunity to participate in the AHRQ Safety Program for Improving Antibiotic Use, choosing a geriatric medicine unit and surgical/trauma ICU to participate. The project started with engaging key stakeholders including pharmacy, nursing, physician extenders, residents and physicians on each unit; sharing antibiotic utilization; and exploring opportunities for improvement. The geriatric unit focused on ceftriaxone use and the management of asymptomatic bacteriuria, while the surgical ICU focused on linezolid use.
Nanticoke Health Services
Nanticoke formed outpatient and inpatient Antibiotic Stewardship Committees, which worked with their EMR to develop reports so that meaningful data could be collected. The team distributed education to all staff regarding antimicrobial stewardship, and provided face-to-face education to ED clinicians by pharmacy and physician leaders. The Infection Preventionist also provided face-to-face education at several community events. The team is currently testing a 72-hour antibiotic time-out for four frequently used antibiotics in the inpatient population.
Nemours/A.I. duPont Hospital for Children
The Nemours team focused on two areas of antimicrobial stewardship: development and implementation of clinical pathways for ambulatory care practices including primary care, emergency department and urgent care; and development of an inpatient unit-specific antimicrobial stewardship initiative via the AHRQ Safety Program for Improving Antibiotic Use. For the clinical pathways, a multidisciplinary team was established and identified common diagnoses with the greatest potential for practice variation (i.e. acute respiratory tract infection). The team measured baseline data on antimicrobial prescribing and diagnostic test utilization for these diagnoses, and developed evidence-based clinical pathways. Ultimately the team developed and implemented 4 clinical pathways (streptococcus pharyngitis, URI, acute bacterial sinusitis and influenza) during the one-year period. The team leveraged the EMR to provide clinical support consistent with recommendations of the clinical pathways (best practice alerts, order sets, preference lists, express lanes), and engaged front line clinicians via in-person training and open communication regarding feedback or concerns about the pathway. Lastly, they developed individualized physician performance dashboards.
For the AHRQ program, the team identified the pediatric ICU (PICU) as the unit with the highest patient acuity and highest utilization of broad-spectrum antibiotics. The unit-specific initiative included identifying unit physician champions, with whom biweekly meetings were held to perform prospective review of patients’ antimicrobial therapy and identify opportunities for improvement. With the champions, the team reviewed at least ten patients per month, after which they developed and implemented a formal process for antibiotic time-outs, in collaboration with the PICU attending physicians and PICU pharmacy clinical specialist. The pharmacist and clinical team assessed a standardized set of questions on antibiotic indications, route, and duration during patient rounds, and the pharmacist documented the assessment and decision in a progress note. All patients receiving antimicrobials for greater than 48 hours were included for assessment.
Utilization Data
Given the disparate EMRs utilized by the participating hospitals, we did not attempt to pool utilization data for this project. However, Quality Insights, through a contract funded by CMS, provided pooled outpatient utilization data for Medicare beneficiaries, using Medicare Part D claims and national drug codes to calculate the total number of antibiotic prescriptions, divided by the total member months for beneficiaries with pharmacy benefits for the same time period. Available data included the first quarter of 2016 (2016Q1) through the second quarter of 2018 (2018Q2). We calculated overall utilization, as well as utilization of broad-spectrum (defined as agents effective against both Gram positive and Gram negative bacteria), and narrow-spectrum (defined as agents effective against specific families of bacteria) antibiotics. Because the initiative began in August 2017, we compared the pre-intervention one-year period (2016Q3-2017Q2) to the intervention period (2017Q3-2018Q2), and calculated rate ratios.
Results
The teams reported many lessons learned as well as barriers to implementation of the project (see Table 2). Examining the Medicare Part D fee for service antibiotic claims, 142,148 antibiotic prescriptions were filled during the baseline year (2016 Q3-2017 Q2), for an average of 1.19 prescriptions per member per year. This decreased slightly during the intervention year (2017 Q3-2018 Q2) to 132,736 prescriptions or 1.07 antibiotics per member per year. Clear seasonality was evident, with higher utilization during quarter 1 (January-March) of each year (see Figure 3). Overall, outpatient antibiotic utilization decreased by 9% between the baseline and implementation years (see Figure 4). In both years, broad-spectrum antibiotics made up approximately two-thirds of all antibiotics prescribed (69.7% during baseline; 69.4% during intervention). Utilization of broad-spectrum antibiotics decreased to a greater extent than did that of narrow-spectrum agents (see Figure 4).
Table 2. Lessons Learned and Barriers reported by the six Choosing Wisely Antibiotic Stewardship teams.
| Lessons Learned | Barriers to Implementation |
|---|---|
| • Importance of multidisciplinary team approach, including providers, pharmacists and nurses • Critical to have clinical champions within each practice setting • Participating in national study (AHRQ project) provided additional momentum and interest • Important to identify one or two small efforts to focus on (e.g., specific drug and/or specific disease state) • Importance of communication with all necessary parties/people impacted by changes • Doing snowflake model at beginning with well thought out planning • Need to have dedicated time allocated for calls and face-to-face meetings for all members of the team • Need representation from different practice areas in pathway development as workflows vary by practice and by site • Need uniform way to disseminate information to the front-line clinicians • Need forum to obtain and respond to feedback • Leadership support key for driving improvement throughout multiple practice settings • Analytics don't have to be complex in order to be effective • Vary methods for engaging providers, nursing, pharmacy, patients and families - different approaches may work for each |
• Data issues: o Access to all antibiotic prescribing data o Development of accurate data dashboards o Developing a consistent way to have oversight over development of EHR changes o AHRQ data imperfect for specific units types/ formularies o Delays in implementing EHR changes • Engaging patients and other community members – population can be difficult to reach • Physician engagement • Competing priorities in primary care and among inpatient teams • Marketing delays • Insurance prior-authorization requirements vary between different states • Needs for discretionary time by team members – challenging to schedule meetings for a large team of busy clinicians |
Figure 3.
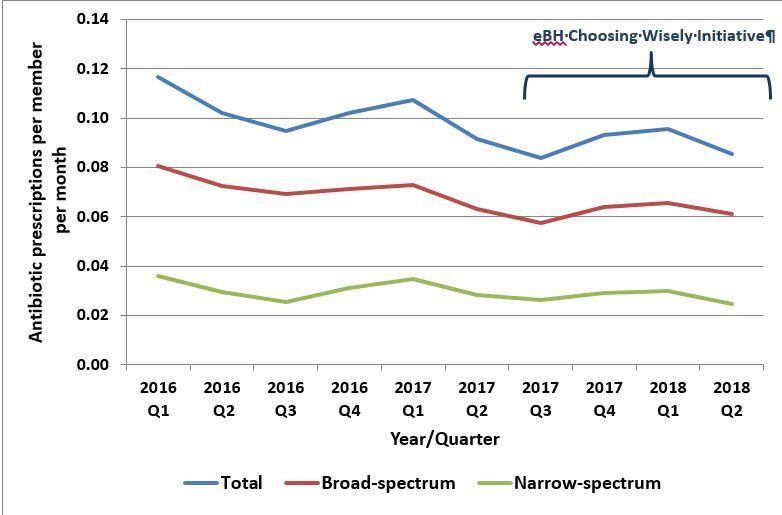
Outpatient antibiotic utilization among Delaware Medicare Part D beneficiaries, 2016 quarter 1 through 2018 quarter 2, based on claims data.
Figure 4.
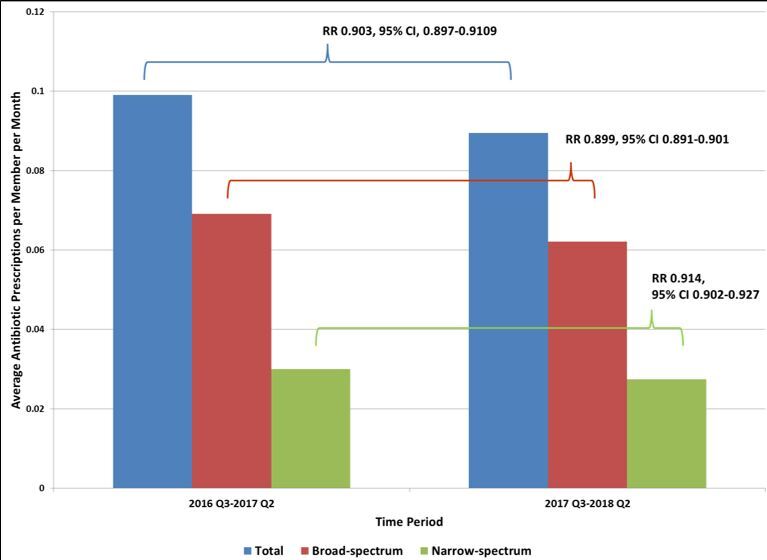
Outpatient antibiotic utilization among Delaware Medicare Part D beneficiaries, comparing eBH pre-intervention (2016 Q3-2017 Q2) to intervention (2017 Q3-2018 Q2) periods.
Legend: eBH, eBrightHealth LLC Strategic Alliance. Green bar demonstrates duration of eBH Choosing Wisely antibiotic stewardship project.
Legend: CI, confidence interval; eBH, eBrightHealth LLC Strategic Alliance; RR, rate ratio.
Discussion
The eBH Choosing Wisely antibiotic stewardship initiative has demonstrated the value of multiple individuals and teams, with multidisciplinary backgrounds and from widely varying health care systems, coming together to work on a single project. While each team’s interventions and specific goals differed slightly based on their unique clinical situation and patient populations, all teams were able to move forward toward their goal and implement new interventions to promote appropriate use of antibiotics. The “all teach, all learn” method of collaboration provides a framework for not only learning from others but also disseminating similar messaging to health care consumers. While many patients (and parents) are aware of the downsides of antibiotic use,22,23 hearing a similar message from providers across the health care continuum is essential for successful reduction of unnecessary antimicrobial use. Our results demonstrated a modest decline in outpatient antibiotic utilization among Medicare beneficiaries that was consistent with an overall downward trend. This is not unexpected given the relatively small number of providers impacted by this work over the one year duration of the project; the teams continue to work to further spread their interventions, and anticipate greater impact. Impact on other populations, including pediatrics and younger adults, is not known.
The importance of antibiotic stewardship cannot be overstated. Antibiotics are unique among medications in that their use, appropriate or otherwise, affects not only the individual taking the medication, but also the community around them. While life-saving when needed, extensive research has demonstrated their overuse, which can include using antibiotics for diagnoses that are either not infectious in nature, or caused by viruses; using unnecessarily broad-spectrum agents; and prescribing unnecessarily long courses of antibiotics, when shorter courses are equally effective. Such overuse contributes to worsening antibiotic resistance, thereby making true infections increasingly difficult and expensive to treat. It is the primary driver of increasing rates of C. difficile infections, both within hospitals as well as the community, and is a major cause of significant allergic reactions and other adverse drug events.4
Antimicrobial stewardship programs have been recommended for all hospitals since 2014, and since 2016 have been required by CMS as a condition of participation for hospitals and nursing homes.24 In early 2019 the Joint Commission proposed a new requirement for antimicrobial stewardship in ambulatory health care.25 To support these efforts, the CDC has published a series of documents describing the Core Elements required for effective stewardship programs.8,9 Primary among these elements is the leadership commitment necessary not only to state that this work is a priority, but also to dedicate sufficient human and other resources necessary to complete this challenging task. The eBH Choosing Wisely framework was able to garner such leadership support from each health system, and foster accountability from all the teams via designating team leads and facilitating regular meetings. Additionally, eBH was able to convene other organizations to participate in the these efforts, which not only served to facilitate the integration of their expertise and insight into team projects, but also to minimize the potential for redundant work being commissioned within our community.
Having teams comprised of multidisciplinary health care professionals allowed the efforts to benefit from the multifaceted expertise that contributed to all teams implementing multiple interventions. While education of both providers and patients regarding stewardship principles is necessary, it is also recognized that education alone is not sufficient to create lasting changes. Developing the ability to track and report reliable data is crucial for long-term improvement and sustainment of antimicrobial stewardship, but remains elusive and is probably the greatest barrier reported by all the teams; however, despite limited resources to make major changes in this arena during the one-year time span of this project, the teams were able to make progress in acquiring data. We are hopeful that additional data resources will be available in the near future.
The collaborative work described in this paper demonstrates the statewide progress that can be accomplished and the many efforts required to successfully implement such a multi-institution, multi-disciplinary project. The Choosing Wisely Work Group has since initiated similar collaborations around imaging for low back pain and end-of-life care. Creating a statewide group to focus, align and collaborate on issues such as these, which demonstrate wide practice variability, will improve the health of all Delawareans while promoting safety, efficiency, and access to quality care.
Acknowledgements:
The authors would like to acknowledge and thank the following people, without whose contributions this project would not have been possible:
ABIM Foundation: Kelly Rand, Program Manager, Choosing Wisely® campaign
Bayhealth: Eric J. Gloss, DO, MMM; Kelly Gardner, BSN, RN, CIC; Holly Helmick, MSN, RN, CNOR, CIC
Beebe Healthcare: Michael J. Fraundorder, PharmD; Michael Salvatore, MD
Christiana Care Health System: Tony Bianchetta, MD; Mary Ann Faralli, EdD, MSN, MBA, RN, CCRN-K; Harold P. Kramer, MD; Helenann Mccloskey, MSN, RN
Nanticoke: Robert C. Ferber, MD
Nemours/A.I. duPont Hospital for Children: Craig Shapiro, MD; Karen Ravin, MD; Sara Slovin, MD; Elysha Pifko, MD; Yamara Coutinho-Sledge, MD; Karina Chara; Leigh Gage, RN; Jennifer Cooper, RN
Footnotes
Disclosures:
The analyses upon which this publication is based were performed under Contract Number HHSM-500-2014-QIN003I, funded by the Centers for Medicare & Medicaid Services, an agency of the U.S. Department of Health and Human Services. The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government. The authors assume full responsibility for the accuracy and completeness of the ideas presented.
All authors report no conflicts of interest related to this work.
References
- 1.ABIM Foundation. Choosing Wisely: promoting conversations between patients and clinicians. http://www.choosingwisely.org/. Accessed January 30, 2019.
- 2.Society for Healthcare Epidemiology of America, Infectious Diseases Society of America, Pediatric Infectious Diseases Society. Policy Statement on Antimicrobial Stewardship.; 2012. https://www.shea-online.org/index.php/policy/positions-statements/288-policy-statement-on-antimicrobial-stewardship-by-the-society-for-healthcare-epidemiology-of-america-shea-the-infectious-diseases-society-of-america [DOI] [PubMed]
- 3.Baggs, J., Fridkin, S. K., Pollack, L. A., Srinivasan, A., & Jernigan, J. A. (2016, November 1). Estimating national trends in inpatient antibiotic use among US hospitals from 2006 to 2012. JAMA Internal Medicine, 176(11), 1639–1648. 10.1001/jamainternmed.2016.5651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention (CDC). Antibiotic Use in the United States, 2017: Progress and Opportunities. Atlanta, GA; 2017. https://www.cdc.gov/antibiotic-use/stewardship-report/pdf/stewardship-report.pdf
- 5.Centers for Disease Control and Prevention (CDC). Outpatient Antibiotic Prescriptions - United States, 2016. https://www.cdc.gov/antibiotic-use/community/programs-measurement/state-local-activities/outpatient-antibiotic-prescriptions-US-2016.html. Accessed February 4, 2019.
- 6.Centers for Disease Control and Prevention (CDC). Viewing outpatient antibiotic use data. https://gis.cdc.gov/grasp/PSA/AUMapView.html. Accessed January 30, 2019.
- 7.Fleming-Dutra, K. E., Hersh, A. L., Shapiro, D. J., Bartoces, M., Enns, E. A., File, T. M., Jr., et al. Hicks, L. A. (2016, May 3). Prevalence of inappropriate antibiotic prescriptions among US ambulatory care visits, 2010-2011. JAMA, 315(17), 1864–1873. 10.1001/jama.2016.4151 [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention (CDC). Core Elements of Hospital Antibiotic Stewardship Programs. Atlanta, GA; 2014. http://www.cdc.gov/getsmart/healthcare/%0Aimplementation/core-elements.html [DOI] [PMC free article] [PubMed]
- 9.Sanchez, G. V., Fleming-Dutra, K. E., Roberts, R. M., & Hicks, L. A. (2016, November 11). Core elements of outpatient antibiotic stewardship. MMWR Recomm Rep, 65(6), 1–12. 10.15585/mmwr.rr6506a1 [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. The Core Elements of Antibiotic Stewardship for Nursing Homes. Atlanta, GA; 2015. https://www.cdc.gov/longtermcare/pdfs/core-elements-antibiotic-stewardship.pdf
- 11.Centers for Disease Control and Prevention (CDC). Percentage of Hospitals Meeting all 7 Core Elements of Hospital Antibiotic Stewardship Program by State, 2016. https://www.cdc.gov/antibiotic-use/community/images/materials/2016-Percentages-B.jpg. Accessed January 30, 2019.
- 12.Suda, K. J., Hicks, L. A., Roberts, R. M., Hunkler, R. J., & Danziger, L. H. (2013, March). A national evaluation of antibiotic expenditures by healthcare setting in the United States, 2009. The Journal of Antimicrobial Chemotherapy, 68(3), 715–718. 10.1093/jac/dks445 [DOI] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention (CDC). Be Antibiotics Aware: Smart Use, Best Care. https://www.cdc.gov/features/antibioticuse/index.html. Accessed February 4, 2019.
- 14.Tamma, P. D., Miller, M. A., & Cosgrove, S. E. (2019, January 15). Rethinking how antibiotics are prescribed: Incorporating the 4 moments of antibiotic decision making into clinical practice. JAMA, 321(2), 139–140. 10.1001/jama.2018.19509 [DOI] [PubMed] [Google Scholar]
- 15.Agency for Healthcare Research and Quality. AHRQ Safety Program for Improving Antibiotic Use. https://safetyprogram4antibioticstewardship.org/page/AHRQ-Safety-Program-for-Improving-Antibiotic-Use. Accessed January 30, 2019.
- 16.Meeker, D., Knight, T. K., Friedberg, M. W., Linder, J. A., Goldstein, N. J., Fox, C. R., et al. Doctor, J. N. (2014, March). Nudging guideline-concordant antibiotic prescribing: A randomized clinical trial. JAMA Internal Medicine, 174(3), 425–431. 10.1001/jamainternmed.2013.14191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Szymczak, J. E., Feemster, K. A., Zaoutis, T. E., & Gerber, J. S. (2014, October). Pediatrician perceptions of an outpatient antimicrobial stewardship intervention. Infection Control and Hospital Epidemiology, 35(Suppl 3), S69–S78. 10.1086/677826 [DOI] [PubMed] [Google Scholar]
- 18.McKay, R., Mah, A., Law, M. R., McGrail, K., & Patrick, D. M. (2016, June 20). Systematic review of factors associated with antibiotic prescribing for respiratory tract infections. Antimicrobial Agents and Chemotherapy, 60(7), 4106–4118. 10.1128/AAC.00209-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mangione-Smith, R., McGlynn, E. A., Elliott, M. N., Krogstad, P., & Brook, R. H. (1999, April). The relationship between perceived parental expectations and pediatrician antimicrobial prescribing behavior. Pediatrics, 103(4), 711–718. Retrieved from http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med4&NEWS=N&AN=10103291 10.1542/peds.103.4.711 [DOI] [PubMed] [Google Scholar]
- 20.Society of Infectious Diseases Pharmacists (SIDP). Antimicrobial Stewardship Certificate Programs. https://sidp.org/Stewardship-Certificate. Accessed January 30, 2019.
- 21.Agency for Healthcare Research and Quality. TeamSTEPPSTM Guide to Action: Creating a Safety Net for Your Healthcare Organization.; 2006. AHRQ Publication No. 06-0020-4.
- 22.Szymczak, J. E., Klieger, S. B., Miller, M., Fiks, A. G., & Gerber, J. S. (2018, December 3). What parents think about the risks and benefits of antibiotics for their child’s acute respiratory tract infection. Journal of the Pediatric Infectious Diseases Society, 7(4), 303–309. 10.1093/jpids/pix073 [DOI] [PubMed] [Google Scholar]
- 23.Ancillotti, M., Eriksson, S., Veldwijk, J., Nihlén Fahlquist, J., Andersson, D. I., & Godskesen, T. (2018, October 3). Public awareness and individual responsibility needed for judicious use of antibiotics: A qualitative study of public beliefs and perceptions. BMC Public Health, 18(1), 1153. 10.1186/s12889-018-6047-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.The Joint Commission. Approved: New Antimicrobial Stewardship Standard. 2016;36(7):1-8. https://www.jointcommission.org/assets/1/6/New_Antimicrobial_Stewardship_Standard.pdf [PubMed]
- 25.The Joint Commission. Proposed New Requirement at MM.09.01.03 – Antimicrobial Stewardship – Ambulatory Health Care. https://www.jointcommission.org/antimicrobial_stewardship_–_ambulatory_health_care_ahc/. Accessed February 1, 2019.


