Abstract
Since the outbreak of Covid-19 in December, 2019, scientists worldwide have been committed to developing COVID-19 vaccines. Only when most people have immunity to SARS-CoV-2, COVID-19 can reduce even wholly overcome. So far, nine kinds of COVID-19 vaccines have passed the phase III clinical trials and have approved for use. At the same time, adverse reactions after COVID-19 vaccination have also reported. This paper focuses on the adverse effects of thrombosis and thrombocytopenia caused by the COVID-19 vaccine, especially the adenovirus-vector vaccine from AstraZeneca and Pfizer, and discusses its mechanism and possible countermeasures.
Keywords: COVID-19, SARS-CoV-2, adenovirus-vectored vaccine, adverse effect, thrombocytopenia, thrombosis
COVID-19 Vaccine Types and Preparation Methods
COVID-19 Vaccine Types
The following nine vaccines have completed phase III clinical trials and have approved by the World Health Organization (WHO). The effectiveness of the various vaccines and other relevant information shows in Table 1.
Table 1.
Types of COVID-19 vaccine.
| Name | Company | Types | Efficacy (%) | Storage condition (°C) | Capacity (billion) |
|---|---|---|---|---|---|
| BNT162b2 | Prizer(US)&BioNTech(GER) | mRNA | 95.00 | −70 | 1.07 |
| mRNA-1273 | Moderna(US) | mRNA | 94.50 | −20 | 0.5-1 |
| CoronaVac | Sinovac Biotech(CHN) | Inactivated viruses | 91.25 | 2-8 | 0.206 |
| BBIBP-CorV | Beijing Institute of Biological Products(CHN) | Inactivated viruses | 86.00 | 2-8 | 1.12 |
| Sputnik V | Gamaleya(Russia) | adenovirus vector | 92.00 | 2-8 | 1.2 |
| AZD1222 | Asrazeneca(UK)&Oxford | adenovirus vector (ChAdOx1) | 70.40 | 2-8 | 2.1 |
| NVX-CoV2373 | Novavax(US) | mRNA | 89.30 60.10 |
2-8 | 2 |
| Ad26.COV2.s | Johnson & Johnson(US) | adenovirus vector(Ad26.COV2.s) | 66.90 | 2-8 | 1 |
| ConvideciaTM | CanSino Bio(CHN) | adenovirus vector(Ad5-nCoV) | 65.28 | 2-8 | 0.1-0.2 |
COVID-19 Vaccine Preparation Methods
Currently, there are three types of COVID-19 vaccine approved worldwide: inactivated vaccine, adenovirus-vector vaccine and nucleic acid vaccine. 11
The inactivated COVID-19 vaccine made from native SARS-Cov-2, which is heated or chemically treated to make its replication defective, thus maintaining the immunogenicity of the SARS-Cov-2 but without causing pathogenicity.
The adenovirus-vector COVID-19 vaccine is to insert part of the gene sequence of SARS-Cov-2 into the adenovirus, in order to construct a fusion type of the two viruses so that it has the infectivity of adenovirus and expresses the antigenicity of SARS-Cov-2.
The mRNA COVID-19 vaccine consists of a nucleoside-modified mRNA encoding SARS-Cov-2, packaged in lipid nanoparticles to reduce RNA degradation and improve translation efficiency.
Adverse Effects of COVID-19 Vaccine
The results of clinical trials on the safety and effectiveness of COVID-19 vaccines have reported one after another. Under the premise of fully affirming the immune protection of the COVID-19 vaccine, the adverse effects cannot ignored.
The most common symptoms after COVID-19 vaccination are fatigue, headache, muscle pain, chills and pain at the injection site, which described in the safety evaluation reports of COVID-19 vaccines such as Pfizer and Moderna and other vaccines.9,12
Scholars conducted a descriptive analysis of the WHO global individual case safety report database VigiBase, reporting the arterial and venous thrombosis adverse effects of COVID-19 vaccination. The thrombosis adverse reactions mainly occurred after vaccination with Pfizer, AstraZeneca and Moderna these adenovirus-vector mRNA vaccines. 13
To Discuss the Mechanism of Adenovirus-Vectored Vaccine Inducing Thrombocytopenia and Thrombosis
Thrombosis and Thrombocytopenia After AstraZeneca's COVID-19 Vaccination
The incidence of thrombotic events per million people after COVID-19 vaccination was 0.21 [95% CI:0.19-0.22]. For VTE (venous thrombus embolism) and ATE (arterial thrombus embolism), there were, respectively, 0.075 [95% CI: 0.07-0.08] and 0.13 [95% CI: 0.12-0.14]. 13
On March 19, 2021, the European Medicines Agency (EMA) disclosed to the public two deaths after AstraZeneca's COVID-19 vaccination. 14 A 49-year-old woman died of severe coagulopathy dysfunction and a 35-year-old woman died of pulmonary embolism. It found that patients with cerebral thrombosis after AstraZeneca's vaccination has the characteristic that they appeared decreased platelet count. On April 10, two simultaneous studies, published in the New England Journal of Medicine (NEJ), discussed symptoms of thrombosis and thrombocytopenia following AstraZeneca's COVID-19 vaccination, and for the first time reported on the underlying mechanism.15,16
Vaccine-Induced Immune Thrombotic Thrombocytopenia
It has confirmed that COVID-19 is associated with a prethrombotic phenotype characterized by coagulation dysfunction and endothelial dysfunction.17-21 In the NEJ reports, all 11 patients in the initial analysis had moderate to severe thrombocytopenia and abnormal thrombosis, especially cerebral venous thrombosis and visceral venous thrombosis. In addition, five patients also had disseminated intravascular coagulation (DIC), with the significantly higher D-dimer level and one or more of the INR (international standardized ratio) of PT (prothrombin time) or fibrinogen level abnormal.15,16
When evaluating the serological characteristics of the four initial patients by the platelet activation assay, found that platelet factor 4 (PF4) significantly enhanced the response and platelet activation. All reactions were blocked by monoclonal antibody and immunoglobulin, indicating that platelet activation occurs through platelet Fcγ receptors. The PF4–heparin ELISA tests of these patients were positive. Most samples (19 out of 24) inhibited by LMWH (low molecular weight heparin). Almost all models (22 out of 24) activated by adding PF4 and inhibiting by high doses of heparin.
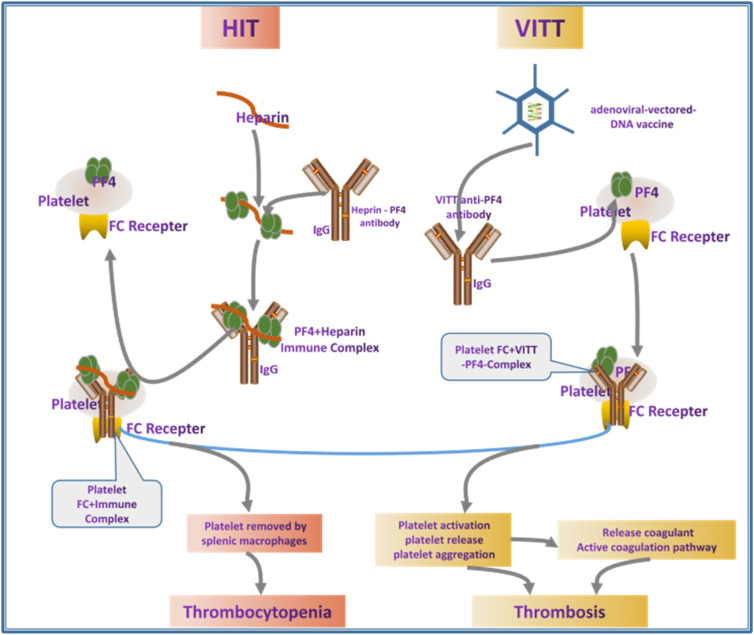
This increased PF4 antibody level mediated thrombocytopenia and thrombosis is similar to the heparin-induced thrombocytopenia (HIT). HIT is an immune complication of heparin therapy caused by PF4 and heparin complex antibodies.22,23 PF4/heparin antibody binds and activates FcγRIIA on platelets and monocytes and mediates HIT and thrombosis. 24
It is precise because the clinical manifestations of thrombocytopenia and thrombosis after adenovirus-vectored COVID-19 vaccination and the production of peculiar auto anti-PF4 antibodies are very similar to HIT. This syndrome is named vaccine-induced immune thrombotic thrombocytopenia (VITT).25,26
VITT is related to the anti-PF4 platelet-activating antibody, patients with VITT occur thrombocytopenia and thrombosis without heparin exposure.27,28 Studies have shown that VITT anti-PF4 antibodies had a stronger binding reaction than HIT antibodies to the PF4 and PF4/heparin complexes, which collect the PF4 tetramers to cluster and form immune complexes, thereby causing the FCγRIIA dependent platelet activation. Adverse reactions after adenoviral-vectored vaccination include microvascular damage, micro-bleeding and thrombosis, which are the result of released platelet activation and PF4-directed autoimmunity of VITT antibody.29,30
HIT and VITT mechanism shows in Figure 1.
Figure 1.
HIT and VITT mechanism schematic. Abbreviations: HIT, heparin-induced thrombocytopenia; VITT, vaccine-induced immune thrombotic thrombocytopenia.
Adenovirus Vectors are Associated with Platelets
According to the proposed model, any adenovirus-vectored-DNA vaccine could drive autoimmune VITT in susceptible individuals. Electrochemical DNA–PF4 interactions and PF4–heparin interactions, but at different locations, represent the common denominator in HIT and VITT related autoimmune-mediated thrombosis.
It has confirmed that some adenoviruses can use coxsackie and adenovirus receptor (CAR) to bind to platelets.31,32 The replication-deficient recombinant chimpanzee ChAdOx1 vector, which is the main component of the Asrazeneca AZD1222 vaccine, uses CAR.33,34 However, Johnson & Johnson's Ad26.COV2.S vaccine does not use CAR as the primary entry receptor. 35 If thrombocytopenia and thrombosis occur after Johnson & Johnson's vaccination, or have target PF4–heparin antibody response, considered that related to the adenovirus vector.
How to Prevent and Treat Thrombocytopenia and Thrombosis Caused by Adenovirus-Vector COVID-19 Vaccine?
Although researchers have not yet been able to confirm what component of the COVID-19 vaccine, caused this rare thrombocytopenia and thrombosis symptom, the following suggestions still have some reference value:
If the patient has venous or arterial thrombosis in unusual parts (brain, abdomen) within 5 to 20 days after COVID-19 vaccination, or accompanied thrombocytopenia, it indicates vaccination adverse reactions.
For patients who have not been exposed to heparin recently but have thrombosis or thrombocytopenia, the PF4–heparin antibody can be detected. This is indicative for the determination of thrombocytopenia or anti-pf4 antibody-related thrombosis after COVID-19 vaccination.
Given that VITT has the same laboratory findings and clinical manifestations as HIT, the use of unfraction heparin (UFH) or LMWH and, or platelet transfusion therapy may lead to disease progression, 36 In contrast, non-heparin anticoagulants and intravenous immunogloblin (IVIG) therapy are often associated with rehabilitation.
Conclusion
Overall, adverse events associated with adenovirus-vectored COVID-19 vaccination was less than 1 in 1 million. The European Medicines Agency has determined that AstraZeneca's COVID-19 vaccine is effective and recommended, thrombosis should list as an “extremely rare” side effect. 14 The agency also stated that there is a “possible link” between AstraZeneca's vaccine and thrombosis, but the existing data are not yet sufficient to confirm specific risk factors. The overall benefits of this vaccine outweigh the disadvantages.
According to current research results, we have known that the adenovirus-vector vaccine activates platelets and produce PF4 antibodies, but only a subset of sensitized patients progress to life-threatening complications of thrombocytopenia and thrombosis,22-24 the reasons and mechanisms need to be further explored.
Footnotes
Compliance with ethics guidelines: This article does not contain any studies with human or animal subjects performed.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
ORCID iD: Haimei MA https://orcid.org/0000-0002-2715-7732
References
- 1.Polack FP, Thomas SJ, Kitchin Net al. C4591001 Clinical Trial Group. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383(27):2603-2615. Epub 2020 Dec 10. PMID: 33301246; PMCID: PMC7745181. doi: 10.1056/NEJMoa2034577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baden LR, El Sahly HM, Essink Bet al. COVE Study Group. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2021;384(5):403-416. Epub 2020 Dec 30. PMID: 33378609; PMCID: PMC7787219. doi: 10.1056/NEJMoa2035389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Turkey declared Sinovac's new coronavirus vaccine effective, http://www.saglik.gov.tr/, 2020 Dec 25.
- 4.Doroftei B, Ciobica A, Ilie OD, Maftei R, Ilea C. Mini-review discussing the reliability and efficiency of COVID-19 vaccines. Diagnostics (Basel). 2021;11(4):579. PMID: 33804914; PMCID: PMC8063839. doi: 10.3390/diagnostics11040579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bucci E, Andreev K, Björkman Aet al. Safety and efficacy of the Russian COVID-19 vaccine: more information needed. Lancet. 2020;396(10256):e53. Epub 2020 Sep 21. PMID: 32971041; PMCID: PMC7503114. doi: 10.1016/S0140-6736(20)31960-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Knoll MD, Wonodi C. Oxford-AstraZeneca COVID-19 vaccine efficacy. Lancet. 2021;397(10269):72-74. Epub 2020 Dec 8. PMID: 33306990; PMCID: PMC7832220. doi: 10.1016/S0140-6736(20)32623-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. https://ir.novavax.com/news-releases/news-release-details/novavax-covid-19-vaccine-demonstrates-893-efficacy-uk-phase-3.
- 8.Shinde V, Bhikha S, Hoosain Zet al. 2019nCoV-501 Study Group. Efficacy of NVX-CoV2373 covid-19 vaccine against the B.1.351 variant. N Engl J Med. 2021;384(20):1899-1909. Epub ahead of print. PMID: 33951374; PMCID: PMC8091623. doi: 10.1056/NEJMoa2103055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sadoff J, Gray G, Vandebosch Aet al. ENSEMBLE Study Group. Safety and efficacy of single-dose Ad26.COV2.S vaccine against covid-19. N Engl J Med. 2021;384:2187–2201. doi: 10.1056/NEJMoa2101544. Epub ahead of print. PMID: 33882225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhu FC, Guan XH, Li YHet al. Immunogenicity and safety of a recombinant adenovirus type-5-vectored COVID-19 vaccine in healthy adults aged 18 years or older: a randomised, double-blind, placebo-controlled, phase 2 trial. Lancet. 2020;396(10249):479-488. Epub 2020 Jul 20. PMID: 32702299; PMCID: PMC7836858. doi: 10.1016/S0140-6736(20)31605-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chung YH, Beiss V, Fiering SN, Steinmetz NF. COVID-19 Vaccine frontrunners and their nanotechnology design. ACS Nano. 2020;14(10):12522-12537. Epub 2020 Oct 9. PMID: 33034449; PMCID: PMC7553041. doi: 10.1021/acsnano.0c07197 [DOI] [PubMed] [Google Scholar]
- 12.Oliver SE, Gargano JW, Marin Met al. The advisory committee on immunization practices’ interim recommendation for use of Pfizer-BioNTech COVID-19 vaccine - United States, December 2020. MMWR Morb Mortal Wkly Rep. 2020;69(50):1922-1924. PMID: 33332292; PMCID: PMC7745957. doi: 10.15585/mmwr.mm6950e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smadja DM, Yue Q-Y, Chocron R, et al. Vaccination against COVID-19: insight from arterial and venous thrombosis occurrence using data from VigiBase. Eur Respir J. 2021; in press. doi: 10.1183/13993003.00956-2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. https://www.ema.europa.eu/en/news/covid-19-vaccine-astrazeneca-benefits-still-outweigh-risks-despite-possible-link-rare-blood-clots.
- 15.Schultz NH, Sørvoll IH, Michelsen AEet al. Thrombosis and thrombocytopenia after ChAdOx1 nCoV-19 vaccination. N Engl J Med. 2021;384:2124–2130. doi: 10.1056/NEJMoa2104882. Epub ahead of print. PMID: 33835768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Greinacher A, Thiele T, Warkentin TE, Weisser K, Kyrle PA, Eichinger S. Thrombotic thrombocytopenia after ChAdOx1 nCov-19 vaccination. N Engl J Med. 2021:NEJMoa2104840. doi: 10.1056/NEJMoa2104840. Epub ahead of print. PMID: 33835769; PMCID: PMC8095372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Philippe A, Chocron R, Gendron N, et al. Circulating Von Willebrand factor and high molecular weight multimers as markers of endothelial injury predict COVID-19 in-hospital mortality. Angiogenesis. 2021;24(3):505–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jevnikar M, Sanchez O, Chocron R, et al. Prevalence of pulmonary embolism in patients with COVID 19 at the time of hospital admission. Eur Respir J. 2021;58(1):2100116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huertas A, Montani D, Savale L, et al. Endothelial cell dysfunction: a major player in SARS-CoV-2 infection (COVID-19)? Eur Respir J. 2020;56(1): 2001634. doi: 10.1183/13993003.01634-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chocron R, Galand V, Cellier J, et al. Anticoagulation prior to hospitalization is a potential protective factor for COVID-19: insight from a French multicenter cohort study. J Am Heart Assoc. 2021:e018288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Haimei MA. Pathogenesis and treatment strategies of COVID-19-related hypercoagulant and thrombotic complications. Clin Appl Thromb Hemost. 2020;26:1076029620944497. PMID: 32722927; PMCID: PMC7391437. doi: 10.1177/1076029620944497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Arepally GM. Heparin-induced thrombocytopenia. Blood. 2017;129(21):2864-2872. Epub 2017 Apr 17. PMID: 28416511; PMCID: PMC5445568. doi: 10.1182/blood-2016-11-709873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oldenburg J, Klamroth R, Langer Fet al. Diagnosis and management of vaccine-related thrombosis following AstraZeneca COVID-19 vaccination: guidance statement from the GTH. Hamostaseologie. 2021;41(3):184–189. doi: 10.1055/a-1469-7481. Epub ahead of print. Erratum in: Hamostaseologie. 2021 May 12: PMID: 33822348. [DOI] [PubMed] [Google Scholar]
- 24.Wines BD, Tan CW, Duncan Eet al. Dimeric FcγR ectodomains detect pathogenic anti-platelet factor 4-heparin antibodies in heparin-induced thromobocytopenia. J Thromb Haemost. 2018;16(12):2520-2525. Epub 2018 Nov 20. PMID: 30269432; PMCID: PMC6635755. doi: 10.1111/jth.14306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aleem A, Nadeem AJ. Coronavirus (COVID-19) vaccine-induced immune thrombotic thrombocytopenia (VITT). StatPearls. 2021. StatPearls Publishing; 2021 Jan–. PMID: 34033367. [PubMed] [Google Scholar]
- 26.Cines DB, Bussel JB. SARS-CoV-2 vaccine-induced immune thrombotic thrombocytopenia. N Engl J Med. 2021;384(23):2254-2256. Epub 2021 Apr 16. Erratum in: N Engl J Med. 2021 Jun 10;384(23):e92. PMID: 33861524; PMCID: PMC8063912. doi: 10.1056/NEJMe2106315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huynh A, Kelton JG, Arnold DM, Daka M, Nazy I. Antibody epitopes in vaccine-induced immune thromboticthrombocytopenia. Nature. 2021;596:565–569. doi: 10.1038/s41586-021-03744-4. Epub ahead of print. PMID: 34233346. [DOI] [PubMed] [Google Scholar]
- 28.McGonagle D, De Marco G, Bridgewood C. Mechanisms of immunothrombosis in vaccine-induced thrombotic thrombocytopenia (VITT) compared to natural SARS-CoV-2 infection. J Autoimmun. 2021;121:102662. Epub 2021 May 19. PMID: 34051613; PMCID: PMC8133385. doi: 10.1016/j.jaut.2021.102662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Makris M, Pavord S, Lester W, Scully M, Hunt B. Vaccine-induced immune thrombocytopenia and thrombosis (VITT). Res Pract Thromb Haemost. 2021;5:e12529. doi: 10.1002/rth2.12529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Franchini M, Liumbruno GM, Pezzo M. COVID-19 vaccine-associated immune thrombosis and thrombocytopenia (VITT): diagnostic and therapeutic recommendations for a new syndrome. Eur J Haematol. 2021;00:1-8. doi: 10.1111/ejh.13665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rzymski P, Perek B, Flisiak R. Thrombotic thrombocytopenia after COVID-19 vaccination: in search of the underlying mechanism. Vaccines (Basel). 2021;9(6):559. PMID: 34071883. doi: 10.3390/vaccines9060559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gupalo E, Buriachkovskaia L, Othman M. Human platelets express CAR with localization at the sites of intercellular interaction. Virol J. 2011;8:456. PMID: 21962080; PMCID: PMC3192782. doi: 10.1186/1743-422X-8-456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dicks MD, Spencer AJ, Coughlan Let al. et al. Differential immunogenicity between HAdV-5 and chimpanzee adenovirus vector ChAdOx1 is independent of fiber and penton RGD loop sequences in mice. Sci Rep. 2015;5:16756. PMID: 26576856; PMCID: PMC4649739. doi: 10.1038/srep16756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li H, Rhee EG, Masek-Hammerman K, Teigler JE, Abbink P, Barouch DH. Adenovirus serotype 26 utilizes CD46 as a primary cellular receptor and only transiently activates T lymphocytes following vaccination of rhesus monkeys. J Virol. 2012;86(19):10862-5. Epub 2012 Jul 18. PMID: 22811531; PMCID: PMC3457266. doi: 10.1128/JVI.00928-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Muir KL, Kallam A, Koepsell SA, Gundabolu K. Thrombotic thrombocytopenia after Ad26.COV2.S vaccination. N Engl J Med. 2021;384(20):1964-1965. Epub 2021 Apr 14. PMID: 33852795; PMCID: PMC8063883. doi: 10.1056/NEJMc2105869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Arepally GM, Ortel TL. Vaccine-induced immune thrombotic thrombocytopenia (VITT): what we know and don't know. Blood. 2021:blood.2021012152. doi: 10.1182/blood.2021012152. Epub ahead of print. PMID: 34061166; PMCID: PMC8172307. [DOI] [PMC free article] [PubMed] [Google Scholar]