Abstract
IMPORTANCE
Childhood adversity (CA) is a powerful determinant of long-term physical and mental health that is associated with elevated risk for chronic disease and psychopathology. However, the degree to which CA contributes to mortality as a preventable driver of ill-health and death is unknown.
OBJECTIVE
To estimate the contribution of CA to health behaviors, including smoking and sedentary behavior, as well as the annual mortality attributable to CA in the US through influences on leading causes of death (eg, cardiovascular disease).
EVIDENCE REVIEW
For this systematic review, the PsycINFO and MEDLINE databases were searched on November 15, 2019. The databases were searched for publications from inception (1806 for PsycINFO, 1946 for MEDLINE) to November 15, 2019. Meta-analyses of the associations between CA and morbidity outcomes were included. The population attributable fraction (PAF) was calculated from these associations along with the estimated US prevalence of CA. The PAF was then applied to the number of annual deaths associated with each cause of death to estimate the number of deaths that are attributable to CA. Additionally, the PAF was applied to the incidence of health behaviors to derive the number of cases attributable to CA. Exposure to 1 or more experiences of adversity before the age of 18 years was analyzed, including abuse, neglect, family violence, and economic adversity.
FINDINGS
A total of 19 meta-analyses with 20 654 832 participants were reviewed. Childhood adversity accounted for approximately 439 072 deaths annually in the US, or 15% of the total US mortality in 2019 (2 854 838 deaths), through associations with leading causes of death (including heart disease, cancer, and suicide). In addition, CA was associated with millions of cases of unhealthy behaviors and disease markers, including more than 22 million cases of sexually transmitted infections, 21 million cases of illicit drug use, 19 million cases of elevated inflammation, and more than 10 million cases each of smoking and physical inactivity. The greatest proportion of outcomes attributable to CA were for suicide attempts and sexually transmitted infections, for which adversity accounted for up to 38% and 33%, respectively.
CONCLUSIONS AND RELEVANCE
The results of this systematic review suggest that CA is a leading contributor to morbidity and mortality in the US and may be considered a preventable determinant of mortality. The prevention of CA and the intervention on pathways that link these experiences to elevated disease risk should be considered a critical public health priority.
The published leading causes of death in the US include heart disease, cancer, injuries, and respiratory disease.1 Two seminal studies beginning in the 1990s, however, encouraged consideration of upstream exposures and health behaviors, such as cigarette smoking, as actual determinants of mortality, in addition to proximal causes of death that are routinely administratively reported.2,3 This approach revealed health behaviors including poor diet, physical inactivity, and cigarette smoking as leading preventable contributors to mortality, accounting for approximately 835 000 US deaths annually.2,3 Subsequently, this approach was broadened to consider the extent to which social determinants of health, such as poverty and low educational attainment, additionally contribute to early mortality.4 For example, Galea and colleagues4 estimated that approximately 245 000 annual US deaths are attributable to low levels of education. This recalibration in understanding the determinants of mortality has important implications for the allocation of resources aimed at promoting population health.5 Given that resources are finite, the consideration of upstream, common, and preventable causes of morbidity and mortality has the potential to more effectively prevent negative health outcomes and early mortality.6 Here, we examine the degree to which exposure to childhood adversity (CA) serves as a preventable contributing factor to morbidity and mortality.
Childhood adversity has consistently been identified as a powerful determinant of physical and mental health. Childhood adversity encompasses experiences involving threat (eg, abuse, domestic violence) and deprivation (eg, neglect, parental separation) occurring before adulthood that are likely to require significant adaptation by a child.7 Childhood adversity is common, affecting approximately half of US children, with the majority experiencing multiple types of adversity.8-10 Exposure to adversity is associated with elevated risk for mental disorders, substance use, suicide attempts, and numerous chronic diseases, including heart disease, obesity, cancer, and diabetes.8-13 Experiences of adversity have also been associated with premature mortality.12,14-16
However, the degree to which CA contributes to premature mortality as a preventable driver of illness and death is, to our knowledge, currently unknown. Here, we conduct a novel synthesis of existing evidence to estimate the scope of health burden and preventable mortality attributable to CA. We do so using an approach used in prior work,2-4 by examining associations of CA with leading causes of death (eg, cardiovascular disease and cancer) and with health behaviors including smoking, alcohol use, and sedentary behavior.2,3 This method of estimating attributable deaths was first developed in medicine and public health to highlight that many preventable health behaviors (eg, smoking and physical inactivity) and their consequences (eg, obesity) were leading causes of mortality.2,3 This approach resulted in a paradigm shift away from conceptualizing only disease outcomes as causes of mortality to include health behaviors and social determinants.4 The present study builds on this established approach, incorporating a life-course perspective with a focus on CA as a modifiable driver of mortality.
The framework of attributable deaths has proven to be useful for public health assessment of burden and ideally would affect resource allocation for prevention. Given the stagnation in life expectancy projected to occur in the US over the next decade,17 such research can inform efforts to improve population health by demonstrating the urgency of increasing efforts to both prevent exposure to CA and intervene on the pathways linking these experiences to elevated disease risk.18 The present study was performed to estimate the health burden and annual number of deaths attributable to CA in the US and to highlight the scope of the associations of CA with health that extend to early mortality.
Methods
We estimated the annual mortality and health burden attributable to CA in 5 sequential steps. First, we extracted the magnitude of associations between CA and a range of health outcomes through a systematic review of meta-analyses conducted from database inception to November 15, 2019. Second, we estimated the prevalence of CA from the National Comorbidity Survey Adolescent Supplement—a population-based study of greater than 6500 parent-child dyads in the US.8 Third, these 2 components were used to calculate the population attributable fraction (PAF) for CA and each health outcome. Fourth, the number of annual deaths due to each of the causes of death and the incidence of health behaviors were extracted from national databases. Fifth, we applied the PAF for CA to the total number of deaths for each cause of death and to the incidence of health behaviors to estimate the number of deaths and proportion of health outcomes attributable to CA for each outcome. This study followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline.
Associations Between CA and Health Outcomes
A systematic review was conducted to identify meta-analyses linking CA to a range of health outcomes. Two electronic databases (PsycINFO and MEDLINE) were searched from inception through November 15,2019 (eTable 1 in the Supplement). Studies were extracted based on the following eligibility criteria: study design was a meta-analysis; study included a measure of CA; study reported an odds ratio (OR) or risk ratio (RR) and corresponding 95% CI of CA and an outcome considered to be a cause of death; study was not restricted to a clinical sample in which participants were included based on a medical or psychiatric diagnosis; sample was not restricted to a single sex; and the study was published in the last 10 years (2011 and later).
Outcomes included (1) the published leading causes of death1 (ie, heart disease, cancer, unintentional injuries, chronic lower respiratory disease [CLRD], stroke, Alzheimer disease, diabetes, influenza and pneumonia, kidney disease, and suicide); (2) previously identified upstream causes of death3 (ie, tobacco smoking, poor diet, physical inactivity, alcohol consumption, microbial agents, motor vehicle incidents, toxic agents, firearms, sexually transmitted infections [STIs], and illicit drug use); and (3) prodromal indicators of disease risk associated with elevated mortality risk3 (ie, metabolic syndrome, hypertension, inflammation, low-density lipoprotein cholesterol/lipids, and obesity). We estimated attributable deaths to CA through the published leading causes of death. All other outcomes were used to estimate the number of cases of unhealthy behaviors and disease markers attributable to CA.
A flowchart of the screening process and included meta-analyses are summarized in the eFigure and eTable 2 in the Supplement. No meta-analyses were found linking CA to the following outcomes, which were dropped from our analysis: poor diet, microbial agents, toxic agents, motor vehicle crashes, firearms, Alzheimer disease, influenza and pneumonia, unintentional injuries, hypertension, and low-density lipoprotein cholesterol.
Prevalence of CA
The prevalence of CA was extracted from the National Comorbidity Survey Adolescent Supplement,19 a population-representative survey of children and their caregivers. We selected this survey based on the rigorous population-based sampling methods and high-quality assessments of CA based on both child and caregiver reports. Following the approach outlined by McLaughlin et al,8 we estimated 12 forms of CA: parental death, parental divorce, other parent loss, parent psychopathology, parent substance use, parent criminal behavior, family violence, physical abuse, sexual abuse, emotional abuse, neglect, and economic adversity (eTables 3 and 4 in the Supplement).
Population Attributable Fractions
Odds ratios or RRs were extracted for the association of CA with each outcome from each identified meta-analysis. The ORs or RRs were used to calculate the PAF associated with CA for each health outcome (Table 1). We used the following formula:
where P is the prevalence of the exposure (experiencing 1 or more types of adversity).20,21 We substituted ORs where RRs were not available. The PAF can be interpreted as the proportion of cases of each outcome that would be prevented should the exposure have not occurred.22 For example, the PAF represents the proportion of suicide attempts that would be prevented if exposure to CAs was eradicated, which assumes the associations between exposure and outcome are causal.23 Given the observational nature of virtually all existing data on CA and health outcomes, causality cannot be directly inferred. Unmeasured third variables may contribute to associations of CAs and health outcomes. Furthermore, changing the prevalence of 1 level of adversity exposure may affect prevalence of other adversity experiences, which is a limitation in interpretation of all observational effect estimates. Nonetheless, the PAF is a useful indicator of the degree to which CAs contribute to mortality in the population.
Table 1.
Range and Point Estimates of Odds Ratios and Corresponding PAFs of Unhealthy Behaviors, Disease Markers, and Disease Outcomes Attributable to CA
| Variable | 1 CA |
2 CAs |
3 CAs |
4+ CAs |
||||
|---|---|---|---|---|---|---|---|---|
| OR or RR | PAF | OR or RR | PAF | OR or RR | PAF | OR or RR | PAF | |
| Unhealthy behaviors and disease markers | ||||||||
| Tobacco smoking | ||||||||
| Range (95% CI) | 1.23 to 1.24 (1.04 to 1.46) | 0.052 to 0.054 | 1.43 (1.39 to 1.47) | 0.055 to 0.065 | 1.62 (1.56 to 1.68) | 0.048 to 0.058 | 1.90 to 2.70 (1.81 to 3.11) | 0.082 to 0.144 |
| Point estimate | 1.23 | 0.052 | 1.43 | 0.060 | 1.62 | 0.053 | 2.70 | 0.144 |
| Illicit drug use | ||||||||
| Range (95% CI) | 1.61 to 1.64 (1.48 to 1.83) | 0.128 to 0.133 | 2.44 (2.28 to 2.62) | 0.159 to 0.193 | 2.95 (2.71 to 3.21) | 0.135 to 0.167 | 3.66 to 5.17 (3.27 to 5.96) | 0.208 to 0.292 |
| Point estimate | 1.64 | 0.133 | 2.44 | 0.176 | 2.95 | 0.151 | 5.17 | 0.292 |
| Physical inactivity | ||||||||
| Range (95% CI) | 1.18 (1.03 to 1.35)a | 0.007 to 0.077 | 1.15 (1 to 1.33)a | 0.000 to 0.047 | 1.29 (1.08 to 1.53)a | 0.007 to 0.046 | 0.90 to 1.12 (0.58 to 1.52) | −0.010 to 0.012 |
| Point estimate | 1.18 | 0.041 | 1.15 | 0.022 | 1.29 | 0.026 | 1.12 | 0.012 |
| Harmful alcohol consumption | ||||||||
| Range (95% CI) | 1.44 to 1.46 (1.20 to 1.74) | 0.096 to 0.099 | 1.89 (1.82 to 1.98) | 0.108 to 0.127 | 2.99 (2.80 to 3.20) | 0.141 to 0.167 | 2.00 to 4.31 (1.69 to 4.76) | 0.090 to 0.247 |
| Point estimate | 1.44 | 0.096 | 1.89 | 0.116 | 2.99 | 0.153 | 2.00 | 0.090 |
| STIs | ||||||||
| Range (95% CI) | NA | NA | NA | NA | NA | NA | 5.92 (3.21 to 10.92) | 0.180 to 0.495 |
| Point estimate | NA | NA | NA | NA | NA | NA | 5.92 | 0.328 |
| Obesity | ||||||||
| Range (95% CI) | 1.08 (1.00 to 1.17) | 0.000 to 0.039 | NA | NA | NA | NA | 1.35 to 1.90 | 0.033 to 0.082 |
| Point estimate | 1.08 | 0.019 | NA | NA | NA | NA | 1.62 | 0.058 |
| Inflammationb | ||||||||
| Range (95% CI) | 1.29 to 1.44 (1.16 to 1.66) | 0.145 to 0.204 | NA | NA | NA | NA | NA | NA |
| Point estimate | 1.44 | 0.204 | NA | NA | NA | NA | NA | NA |
| Metabolic syndromec | ||||||||
| Range (95% CI) | NA | NA | 1.26 (1.14 to 1.40) | 0.046 to 0.122 | NA | NA | NA | NA |
| Point estimate | NA | NA | 1.26 | 0.083 | NA | NA | NA | NA |
| Disease outcomes | ||||||||
| Heart disease | ||||||||
| Range (95% CI) | 0.88 to 1.16 (0.69 to 1.29) | −0.030 to 0.037 | 1.60 (1.22 to 2.10)a | 0.032 to 0.140 | 2.48 (2.38 to 2.58)a | 0.112 to 0.126 | 2.07 to 2.30 (1.49 to 3.55) | 0.096 to 0.114 |
| Point estimate | 1.16 | 0.037 | 1.60 | 0.082 | 2.48 | 0.119 | 2.07 | 0.096 |
| Cancer | ||||||||
| Range (95% CI) | 1.10 (0.95 to 1.28) | −0.012 to 0.063 | NA | NA | NA | NA | 2.31 (1.82 to 2.95)c | 0.075 to 0.162 |
| Point estimate | 1.10 | 0.023 | NA | NA | NA | NA | 2.31 | 0.115 |
| CLRD | ||||||||
| Range (95% CI) | 1.29 to 1.46 (1.15 to 1.86) | 0.065 to 0.099 | 1.55 (1.23 to 1.97)a | 0.033 to 0.126 | 2.44 (1.80 to 3.32)a | 0.068 to 0.174 | 2.60 to 3.05 (1.33 to 5.10) | 0.137 to 0.169 |
| Point estimate | 1.29 | 0.065 | 1.55 | 0.075 | 2.44 | 0.116 | 3.05 | 0.169 |
| Suicide | ||||||||
| Range (95% CI) | 1.57 (1.37 to 1.80) | 0.082 to 0.161 | 2.19 (1.88 to 2.55) | 0.115 to 0.187 | 3.43 (2.92 to 4.02) | 0.149 to 0.216 | 7.30 to 37.48 (4.33 to 63.31) | 0.384 to 0.783 |
| Point estimate | 1.57 | 0.120 | 2.19 | 0.150 | 3.43 | 0.181 | 7.30 | 0.384 |
| Diabetes | ||||||||
| Range (95% CI) | 1.02 to 1.11 (0.84 to 1.24) | 0.005 to 0.026 | 0.79 (0.62 to 1.01)a | −0.060 to 0.001 | 1.12 (0.81 to 1.56)a | −0.018 to 0.048 | 0.80 to 1.38 (0.46 to 1.60) | −0.020 to 0.036 |
| Point estimate | 1.11 | 0.026 | .79 | −0.032 | 1.12 | 0.011 | 1.38 | 0.036 |
| Strokea | ||||||||
| Range (95% CI) | 1.01 (0.75 to 1.34) | −0.064 to 0.075 | 1.50 (0.90 to 2.50) | −0.015 to 0.182 | 1.19 (0.76 to 1.87) | −0.022 to 0.073 | 2.00 (0.89 to 4.50) | −0.011 to 0.257 |
| Point estimate | 1.01 | 0.002 | 1.50 | 0.069 | 1.19 | 0.017 | 2.00 | 0.090 |
Abbreviations: CA, childhood adversity; CLRD, chronic lower respiratory disease; NA, not available; OR, odds ratio; PAF, population attributable fraction; RR, risk ratio; STI, sexually transmitted infection (specifically HIV, syphilis, gonorrhea, trichomoniasis, genital herpes, human papillomavirus, sexually transmitted hepatitis B virus).
Estimate based on <5 primary empirical studies.
Exposure is any adversity (≥1 childhood adversity). Outcome specifically elevated C-reactive protein (>3 mg/L in a high-sensitivity C-reactive protein test).
Exposure is ≥2 childhood adversities.
Annual Deaths and the Incidence of Health Behaviors in the US and the Proportion Attributable to CA
Numbers of deaths were extracted from the Centers for Disease Control and Prevention WONDER database for 2019.1 The incidence of unhealthy behaviors and disease markers24-31 was extracted from national databases (Table 2). Deaths were not restricted to a certain age, as meta-analytic estimates for the association between CA and outcomes were of lifetime risk based on a range of ages across the life span.
Table 2.
US Cases of Unhealthy Behaviors and Disease Markers and Annual US Deaths Attributable to CA
| Variable | Cases or deaths, No.a | Cases or deaths due to CA, No.a | ||||
|---|---|---|---|---|---|---|
| 1 CA | 2 CAs | 3 CAs | 4+ CAs | Total | ||
| Unhealthy behaviors and disease markers | ||||||
| Tobacco smoking24 | 34 000 000 | 1 778 620 | 2 034 297 | 1 815 831 | 4 897 886 | 10 526 634 |
| Illicit drug use25 | 28 500 000 | 3 794 730 | 5 006 858 | 4 295 151 | 8 327 722 | 21 424 461 |
| Physical inactivity26 | 107 489 253 | 4 451 242 | 2 334 437 | 2 763 707 | 1 261 980 | 10 811 366 |
| Alcohol consumption27 | 14 400 000 | 1 375 398 | 1 676 005 | 2 207 872 | 1 297 179 | 6 556 454 |
| STIs28 | 67 636 000 | NA | NA | NA | 22 153 578 | 22 153 578 |
| Obesity29 | 107 998 681 | 2 034 512 | NA | NA | 6 245 604 | 8 280 116 |
| Inflammation30b | 95 189 462 | NA | NA | NA | NA | 19 433 038 |
| Metabolic syndrome31c | 112 257 917 | NA | NA | NA | NA | 9 314 335 |
| Disease outcomes | ||||||
| Heart disease | 659 041 | 24 371 | 53 750 | 78 224 | 63 125 | 219 470 |
| Cancer | 599 601 | 14 053 | NA | NA | 68 835 | 82 888 |
| CLRD | 156 979 | 10 215 | 11 816 | 18 187 | 26 484 | 66 702 |
| Suicide | 47 511 | 5717 | 7115 | 8604 | 18 250 | 39 686 |
| Diabetes | 87 647 | 2254 | −2811 | 947 | 3178 | 3568 |
| Stroke | 150 005 | 359 | 10 336 | 2550 | 13 513 | 26 758 |
| Totald | 1 705 874 | 56 969 | 80 206 | 108 512 | 193 385 | 439 072 |
Abbreviations: CA, childhood adversity; CLRD, chronic lower respiratory disease; STI, sexually transmitted infection (specifically HIV, syphilis, gonorrhea, trichomoniasis, genital herpes, human papillomavirus, sexually transmitted hepatitis B virus).
Values for unhealthy behaviors and disease markers represent number of cases; values for disease outcomes represent number of deaths.
Exposure is any adversity (≥1 childhood adversity).
Exposure is ≥2 childhood adversities.
The bottom total row refers only to the causes of death and reflects the number of deaths attributable to each level of exposure to CA.
The PAFs were multiplied by the number of annual deaths and number of cases of health behaviors. The resulting number is interpreted as the number of annual deaths and number of cases via each outcome attributable to CA.
Results
A total of 1858 records were identified through the database search. After removal of duplicates, abstracts were screened for 936 records and 114 records were included in the full-text screening. Ultimately, we identified 19 meta-analyses32-50 with approximately 20 654 832 participants that linked CA with health outcomes of interest across the life span (eFigure in the Supplement). Some meta-analyses reported an overall participant sample size with additional outcomes not included in the current analysis; the reported sample size includes all study participants for these studies. The present analysis includes 7 meta-analyses32-38; an additional 12 are included in supplementary analyses39-50 focused on different types of adversity experiences (eTables 5 and 6 in the Supplement).
Population Attributable Fractions for CA
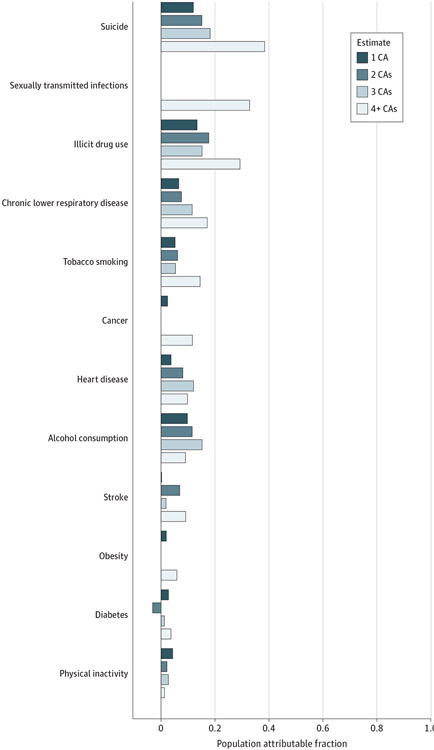
Table 1 reports the ORs extracted from the meta-analyses and resulting PAFs. Where multiple studies provided an association for the same health outcome, we constructed a range of associations and PAFs from all published estimates and extracted the lowest and highest bounds of the 95% CI reported across the included meta-analyses. Where only 1 meta-analytic estimate was available, the point estimate and 95% CI from that meta-analysis is reported in the “range (95% CI)” row in Table 1. Reported as a point estimate is the meta-analytic estimate that reflected the largest number of empirical data sets, which was used to derive the number of cases and deaths for each outcome. The PAF range was calculated using the range of OR estimates; where only one estimate was available (ie, no range), the PAF range was calculated using the 95% CI. Figure 1 shows the PAFs associated with exposure to CA for each health outcome. For the causes of death, the largest PAF was for suicide attempts (PAF for 4+ CAs = 0.384). Experiencing at least 4 CAs was associated with 38% of all suicide attempts. Furthermore, experiencing more than 1 CA accounted for 8% to 17% of CLRD cases (2+ CAs, PAF range, 0.075-0.169), 8% to 12% of all cases of heart disease (2+ CAs, PAF range, 0.082-0.119), and up to 12% of cancer cases (4+ CAs, PAF, 0.115; range, 0.075-0.162).
Figure 1. Population Attributable Fractions of Unhealthy Behaviors, Disease Markers, and Disease Outcomes Attributable to Childhood Adversity.
Population attributable fractions are based on meta-analytic estimates of the associations between different levels of exposure to childhood adversity and each health outcome along with the US prevalence of exposure to childhood adversity. Two outcomes had unique exposures: inflammation (≥1 childhood adversity; population attributable fraction = 0.204) and metabolic syndrome (≥2 childhood adversities; population attributable fraction = 0.083). CA indicates childhood adversity.
For unhealthy behaviors and disease markers, the largest PAF was for STIs (4+ CAs, PAF, 0.328; range, 0.180-0.495), with CA accounting for 33% of all cases. A further 13% to 29% of illicit drug use (1+ CAs, PAF range, 0.133-0.292), 20% of elevated inflammation (4+ CAs, PAF, 0.204; range, 0.145-0.204), 10% to 15% of harmful alcohol consumption (1+ CAs, PAF range, 0.096-0.153), and 5% to 14% of the incidence of smoking (1+ CAs, PAF range, 0.052-0.144) was attributable to CA.
The PAF is sometimes larger for exposure to fewer adverse childhood experiences. This is owing to the fact that the PAF formula includes the prevalence of the exposure; thus, the PAF will also increase when the prevalence of the exposure increases. As shown in eTable 3, the prevalence of 2 adversities is greater than 3 or 4 adversities. When the OR or RR range includes 1 and the PAF range includes 0, this indicates that an included meta-analysis did not find CA to be associated with increased risk of that outcome.
Deaths and Incidence of Unhealthy Behaviors and Disease Markers Attributable to CA
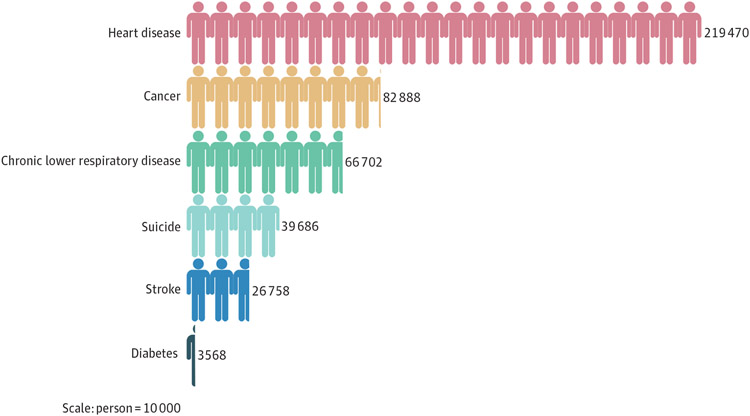
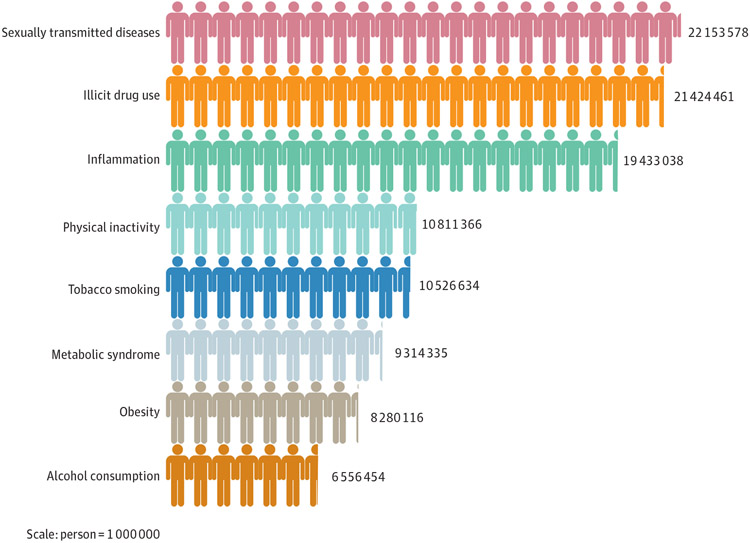
As shown in Table 2, the total number of annual deaths attributable to CA was 439 072 deaths. The greatest number of deaths attributable to CA were for heart disease (219 470), cancer (82 888), and CLRD (66 702). Moreover, CA accounted for 39 686 deaths from suicide in 2019 and 26 758 deaths from stroke (Table 2, Figure 2). In addition, CA was associated with 22153 578 cases of STIs, 21424 461 cases of illicit drug use, 19 433 038 cases of inflammation, 10 526 634 cases of tobacco smoking, and 10 811366 of physical inactivity (Table 2, Figure 3).
Figure 2. Annual US Deaths Attributable to Childhood Adversity.
Annual deaths attributable to childhood adversity are based on meta-analytic estimates of the associations between different levels of exposure to childhood adversity and disease outcomes that are currently the leading causes of mortality in the US.
Figure 3. US Cases of Unhealthy Behaviors and Disease Markers Attributable to Childhood Adversity.
Cases of unhealthy behaviors and disease markers attributable to childhood adversity are based on meta-analytic estimates of the associations between different levels of exposure to childhood adversity and each health outcome.
Discussion
This systematic review found that approximately 439 072 US deaths are annually attributable to CA through associations with the leading causes of death. For perspective, this figure is higher than the total number of US COVID-19 deaths for 2020. The true contribution of CA to mortality is likely much higher, as no published estimates were available on the association of CA with many leading causes of death. In addition, results of the present study reveal that millions of cases of preventable causes of disease and mortality, such as smoking, physical inactivity,2,3 and inflammation are attributableto CA. However, we did not estimate the number of deaths from these factors owing to potential for overlap with deaths attributable to specific disease outcomes (eg, cancer).
The largest numbers of deaths associated with CA were from heart disease, cancer, and CLRD. More than 219 000 deaths from heart disease, 82 000 deaths from cancer, and 66 000 deaths from CLRD were attributed to experiencing CA. Each of these estimates is larger than the total US deaths attributable to influenza and pneumonia, kidney disease, and suicide—3 of the 10 leading causes of death.1 Moreover, CA accounted for up to 38% of all suicide attempts.
The present study was, to our knowledge, the first attempt to examine the degree to which CA contributes to annual mortality, building on previous research that has demonstrated an increased risk of developing a wide range of chronic diseases—including many leading causes of death—as well as elevated risk for early mortality among those exposed to CA.11,12,14,15,51,52 We extended this prior work by additionally examining the contribution of CA to preventable risk factors, such as smoking, sedentary behavior, and alcohol use. Recent work estimating population attributable fractions for CA and health outcomes in England and Wales demonstrated similar estimates to the current study.53 Overall, these results suggest that experiencing CA is a leading preventable factor associated with mortality and should be a target for public health efforts to prevent chronic disease and mortality.
Our findings align with previous research demonstrating that social determinants of health (ie, poverty and low educational attainment), health behaviors (ie, substance use and sedentary behavior), and obesity have a comparable contribution to mortality as the published leading causes of death.2-4 The total estimate of approximately 439 072 deaths annually attributable to experiencing CA was similar to estimates of the number of deaths attributable to racial/ethnic segregation, poverty, and income inequality.4 Current health care spending that disproportionately targets disease outcomes and neglects these social determinants of health may be missing a substantial opportunity to intervene and improve population health.54
These findings give greater urgency to recent efforts to screen for early adversity in pediatric primary care as a way of identifying children at risk for poor health and delivering early interventions.55,56 Considering CA as a preventable contributing factor to early mortality may help to shift action and funding into primary and secondary prevention of adversity. Preventing exposure to CA may be best achieved through policies that provide structural solutions to constraints experienced by families. Affordable childcare, paid parental leave, and a universal basic income are policies that can reduce parental stress and provide support that better enables parents to provide adequate supervision and sensitive and responsive care for their children.57 Home visitation services that provide education and support for families and provide them with available services have been shown to reduce child abuse, neglect, and emergency department visits.58,59 Increasing access to such services is vital, with estimates that suggest these services reach only 3% to 6% of families who could benefit.60,61 Moreover, policy efforts to mitigate the clustering of adversities, such as broadening work requirements for the receipt of economic relief to include substance use and mental health treatment, could reduce the accumulation of adversities by enabling parents to access support and resources critical to promote adaptive child development.62 In addition, evidence-based programs, such as the Safe Environment for Every Kid program—a brief, scalable intervention delivered within pediatric primary care—hold great promise in preventing exposure to CA.63 The Safe Environment for Every Kid program has demonstrated lower rates of childhood maltreatment compared with standard care through training of pediatric primary care physicians to identify and address risk factors for CA in families.55
Our findings also suggest the importance of secondary prevention, that is, the prevention of health consequences among those exposed to adversity. Exposure to CA is associated with altered neurodevelopment64 and changes in physiological regulatory systems, including the autonomic nervous system, hypothalamic-pituitary-adrenal axis, and immune and metabolic systems.65 Accumulating evidence also suggests that exposure to CA accelerates the pace of biological aging.66 This biological embedding of early adversity may contribute to cascading influences on social, emotional, and cognitive development throughout childhood and adolescence67-69 and ultimately culminate in elevated risk for substance use,70,71 psychiatric disorders,10,72,73 and chronic diseases.65,66 However, more research is needed to elucidate the pathways from distinct experiences of adversity; evidence suggests that the type of exposure (ie, deprivation vs threat) has at least partially different associations with development.69 Psychosocial interventions may be able to reverse these biological changes that occur after exposure to CA.74 Moreover, evidence-based psychosocial interventions exist to treat psychopathology in young people exposed to adversity.75,76 Our findings suggest that efforts to increase access to such interventions may be an important public health priority.
Limitations
Several limitations of the current study should be noted. First, most meta-analyses did not restrict their sample to US studies; thus, risk estimates may differ slightly when considering a US-only sample. However, the meta-analyses included in this study reported a majority of samples from North America; thus, substantial differences are unlikely. The prevalence used to calculate the PAFs and the number of annual deaths were restricted to US-only data. Second, the prevalence data was collected between 2001 and 2004 and thus does not reflect any prevalence trends since that time. However, these prevalence estimates were sourced from a population-representative survey of US adolescents and caregivers, thereby reducing bias inherent in other measures of prevalence data, such as retrospective reporting of adversity by adults or a lack of representative sampling methods. Third, ORs were used to approximate the RRs for the PAF formula when RRs were not available, which can inflate the RR when the outcome is common. However, the PAF estimates based on ORs begin to diverge from those based on RRs only when the prevalence of the outcome is greater than 25%77; here, that was relevant only for obesity and physical inactivity. Finally, the estimates in the current study were subject to the inclusion and exclusion criteria of the meta-analyses from which they were derived. Meta-analyses differ somewhat in the specific experiences of CA included, producing some heterogeneity in the specific exposures that contributed to the associations with health outcomes. Future research concerned with producing attributable death estimates for specific adversity experiences (eg, child neglect) could be informed by the synthesis of studies examining that particular exposure.
Conclusions
The results of this systematic review suggest that exposure to CA is a meaningful driver of preventable early mortality, associated with more than 439 000 annual US deaths. These findings suggest the importance of preventing exposure to CA and intervening early among children who have experienced CA in order to prevent disease onset. Determining whether or not evidence-based interventions that are designed to address the mental health consequences of CA can also reduce risk for chronic disease and early mortality is a critical next step for research in this area. This study adds to a growing literature demonstrating that social determinants of health are important to consider as preventable causes of death. By reframing how we think about the causes of death to include upstream drivers of poor health, the finite resources available to address population health may be allocated more effectively.
Supplementary Material
Key Points.
Question
To what degree does childhood adversity contribute to preventable causes of morbidity and mortality in the US?
Findings
In this systematic review including 19 meta-analyses with a total of 20 654 832 participants, exposure to childhood adversity accounted for approximately 439 072 deaths annually across various health outcomes, with the largest contributions to deaths related to heart disease (219 470), cancer (82 888), and chronic lower respiratory disease (66 702). More than 1 in 3 suicide attempts were attributable to childhood adversity.
Meaning
Results of this systematic review suggest that childhood adversity is a major contributing factor to early mortality; reduction of adversity exposure and early intervention on intermediate pathways that contribute to disease outcomes may promote health and longevity at the population level.
Funding/Support:
The current study was funded by grants R01-MH103291, R01-MH106482, and R37-MH119194 from the National Institute of Mental Health (Dr McLaughlin).
Role of the Funder/Sponsor:
The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Conflict of Interest Disclosures: Dr Keyes reported receiving personal fees from National Prescription Opioid Litigation K and testifying as an expert witness in litigation against opioid manufacturers and other defendants outside the submitted work. No other disclosures were reported.
Contributor Information
Lucinda Rachel Grummitt, National Health and Medical Research Council Centre of Research Excellence in PREMISE, The Matilda Centre for Research in Mental Health and Substance Use, The University of Sydney, Sydney, New South Wales, Australia; Mailman School of Public Health, Department of Epidemiology, Columbia University, New York, New York.
Noah T. Kreski, Mailman School of Public Health, Department of Epidemiology, Columbia University, New York, New York.
Stephanie Gyuri Kim, Department of Psychology, Harvard University, Cambridge, Massachusetts.
Jonathan Platt, Mailman School of Public Health, Department of Epidemiology, Columbia University, New York, New York.
Katherine M. Keyes, Mailman School of Public Health, Department of Epidemiology, Columbia University, New York, New York.
Katie A. McLaughlin, Department of Psychology, Harvard University, Cambridge, Massachusetts.
REFERENCES
- 1.Centers for Disease Control and Prevention. National Center for Health Statistics mortality data on CDC WONDER. Accessed April 23, 2020. https://wonder.cdc.gov/mcd.html [Google Scholar]
- 2.McGinnis JM, Foege WH. Actual causes of death in the United States. JAMA. 1993;270(18):2207–2212. doi: 10.1001/jama.1993.03510180077038 [DOI] [PubMed] [Google Scholar]
- 3.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291(10):1238–1245. doi: 10.1001/jama.291.10.1238 [DOI] [PubMed] [Google Scholar]
- 4.Galea S, Tracy M, Hoggatt KJ, Dimaggio C, Karpati A. Estimated deaths attributable to social factors in the United States. Am J Public Health. 2011;101(8):1456–1465. doi: 10.2105/AJPH.2010.300086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Galea S An argument for a consequentialist epidemiology. Am J Epidemiol. 2013;178(8):1185–1191. doi: 10.1093/aje/kwt172 [DOI] [PubMed] [Google Scholar]
- 6.Keyes K, Galea S. What matters most: quantifying an epidemiology of consequence. Ann Epidemiol. 2015;25(5):305–311. doi: 10.1016/j.annepidem.2015.01.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McLaughlin KA, Sheridan MA, Lambert HK. Childhood adversity and neural development: deprivation and threat as distinct dimensions of early experience. Neurosci Biobehav Rev. 2014;47:578–591. doi: 10.1016/j.neubiorev.2014.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McLaughlin KA, Greif Green J, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and first onset of psychiatric disorders in a national sample of US adolescents. Arch Gen Psychiatry. 2012;69(11):1151–1160. doi: 10.1001/archgenpsychiatry.2011.2277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Green JG, McLaughlin KA, Berglund PA, et al. Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: associations with first onset of DSM-IV disorders. Arch Gen Psychiatry. 2010;67(2):113–123. doi: 10.1001/archgenpsychiatry.2009.186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kessler RC, McLaughlin KA, Green JG, et al. Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. Br J Psychiatry. 2010;197(5):378–385. doi: 10.1192/bjp.bp.110.080499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dong M, Giles WH, Felitti VJ, et al. Insights into causal pathways for ischemic heart disease: adverse childhood experiences study. Circulation. 2004;110(13):1761–1766. doi: 10.1161/01.CIR.0000143074.54995.7F [DOI] [PubMed] [Google Scholar]
- 12.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. the Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–258. doi: 10.1016/S0749-3797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- 13.Kalmakis KA, Chandler GE. Health consequences of adverse childhood experiences: a systematic review. J Am Assoc Nurse Pract. 2015;27(8):457–465. doi: 10.1002/2327-6924.12215 [DOI] [PubMed] [Google Scholar]
- 14.Brown DW, Anda RF, Tiemeier H, et al. Adverse childhood experiences and the risk of premature mortality. Am J Prev Med. 2009;37(5):389–396. doi: 10.1016/j.amepre.2009.06.021 [DOI] [PubMed] [Google Scholar]
- 15.Chen E, Turiano NA, Mroczek DK, Miller GE. Association of reports of childhood abuse and all-cause mortality rates in women. JAMA Psychiatry. 2016;73(9):920–927. doi: 10.1001/jamapsychiatry.2016.1786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Puterman E, Weiss J, Hives BA, et al. Predicting mortality from 57 economic, behavioral, social, and psychological factors. Proc Natl Acad Sci U S A. 2020;117(28):16273–16282. doi: 10.1073/pnas.1918455117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kontis V, Bennett JE, Mathers CD, Li G, Foreman K, Ezzati M. Future life expectancy in 35 industrialised countries: projections with a Bayesian model ensemble. Lancet. 2017;389(10076):1323–1335. doi: 10.1016/S0140-6736(16)32381-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McLaughlin KA, DeCross SN, Jovanovic T, Tottenham N. Mechanisms linking childhood adversity with psychopathology: learning as an intervention target. Behav Res Ther. 2019;118:101–109. doi: 10.1016/j.brat.2019.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kessler RC. National comorbidity survey: adolescent supplement (NCS-A), 2001-2004 (ICPSR 28581). Accessed April 2, 2020. https://www.icpsr.umich.edu/web/HMCA/studies/28581 [Google Scholar]
- 20.Kelsey JL, Whittemore AS, Evans AS, Thompson WD. Methods in Observational Epidemiology (Monographs in Epidemiology and Biostatistics). 2nd ed. Oxford University Press; 1996. [Google Scholar]
- 21.Levin ML. The occurrence of lung cancer in man. Acta Unio Int Contra Cancrum. 1953;9(3):531–541. [PubMed] [Google Scholar]
- 22.Northridge ME. Public health methods—attributable risk as a link between causality and public health action. Am J Public Health. 1995;85(9):1202–1204. doi: 10.2105/AJPH.85.9.1202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rockhill B, Newman B, Weinberg C. Use and misuse of population attributable fractions. Am J Public Health. 1998;88(1):15–19. doi: 10.2105/AJPH.88.1.15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. Current cigarette smoking among adults in the United States. Accessed April 24, 2020. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/adult_data/cig_smoking/index.htm [Google Scholar]
- 25.Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results from the 2017 National Survey on Drug Use and Health. US Department of Health and Human Services; 2019. [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention. Table 57. participation in leisure-time aerobic and muscle-strengthening activities that meet the federal 2008 Physical Activity Guidelines for Americans among adults aged 18 and over, by selected characteristics: United States, selected years 1998–2018. National Center for Health Statistics; 2017. [Google Scholar]
- 27.Substance Abuse and Mental Health Services Administration. Results from the 2019 National Survey on Drug Use and Health: detailed tables. US Department of Health and Human Services; 2020. [Google Scholar]
- 28.Kreisel KM, Spicknall IH, Gargano JW, et al. Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2018. Sex Transm Dis. 2021;48(4):208–214. doi: 10.1097/OLQ.0000000000001355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS Data Brief. 2020;(360):1–8. [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey. Accessed April 30, 2020. https://www.cdc.gov/nchs/nhanes/index.htm [Google Scholar]
- 31.Moore JX, Chaudhary N, Akinyemiju T. Metabolic syndrome prevalence by race/ethnicity and sex in the United States, National Health and Nutrition Examination Survey, 1988-2012. Prev Chronic Dis. 2017;14:E24. doi: 10.5888/pcd14.160287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bellis MA, Hughes K, Ford K, Ramos Rodriguez G, Sethi D, Passmore J. Life course health consequences and associated annual costs of adverse childhood experiences across Europe and North America: a systematic review and meta-analysis. Lancet Public Health. 2019;4(10): e517–e528. doi: 10.1016/S2468-2667(19)30145-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Petruccelli K, Davis J, Berman T. Adverse childhood experiences and associated health outcomes: A systematic review and meta-analysis. Child Abuse Negl. 2019;97:104127. doi: 10.1016/j.chiabu.2019.104127 [DOI] [PubMed] [Google Scholar]
- 34.Hughes K, Bellis MA, Hardcastle KA, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health. 2017;2(8):e356–e366. doi: 10.1016/S2468-2667(17)30118-4 [DOI] [PubMed] [Google Scholar]
- 35.Norman RE, Byambaa M, De R, Butchart A, Scott J, Vos T. The long-term health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta-analysis. PLoS Med. 2012;9(11):e1001349. doi: 10.1371/journal.pmed.1001349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jakubowski KP, Cundiff JM, Matthews KA. Cumulative childhood adversity and adult cardiometabolic disease: A meta-analysis. Health Psychol. 2018;37(8):701–715. doi: 10.1037/hea0000637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kuhlman KR, Horn SR, Chiang JJ, Bower JE. Early life adversity exposure and circulating markers of inflammation in children and adolescents: A systematic review and meta-analysis. Brain Behav Immun. 2020;86:30–42. doi: 10.1016/j.bbi.2019.04.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Baumeister D, Akhtar R, Ciufolini S, Pariante CM, Mondelli V. Childhood trauma and adulthood inflammation: a meta-analysis of peripheral C-reactive protein, interleukin-6 and tumour necrosis factor-α. Mol Psychiatry. 2016;21(5):642–649. doi: 10.1038/mp.2015.67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wiss DA, Brewerton TD. Adverse childhood experiences and adult obesity: a systematic review of plausible mechanisms and meta-analysis of cross-sectional studies. Physiol Behav. 2020;223:112964. doi: 10.1016/j.physbeh.2020.112964 [DOI] [PubMed] [Google Scholar]
- 40.Danese A, Tan M. Childhood maltreatment and obesity: systematic review and meta-analysis. Mol Psychiatry. 2014;19(5):544–554. doi: 10.1038/mp.2013.54 [DOI] [PubMed] [Google Scholar]
- 41.Hemmingsson E, Johansson K, Reynisdottir S. Effects of childhood abuse on adult obesity: a systematic review and meta-analysis. Obes Rev. 2014;15(11):882–893. doi: 10.1111/obr.12216 [DOI] [PubMed] [Google Scholar]
- 42.Solmi M, Köhler CA, Stubbs B, et al. Environmental risk factors and nonpharmacological and nonsurgical interventions for obesity: An umbrella review of meta-analyses of cohort studies and randomized controlled trials. Eur J Clin Invest. 2018;48(12):e12982. doi: 10.1111/eci.12982 [DOI] [PubMed] [Google Scholar]
- 43.Wang Y, Wu B, Yang H, Song X. The effect of childhood abuse on the risk of adult obesity. Ann Clin Psychiatry. 2015;27(3):175–184. [PubMed] [Google Scholar]
- 44.Irish L, Kobayashi I, Delahanty DL. Long-term physical health consequences of childhood sexual abuse: a meta-analytic review. J Pediatr Psychol. 2010;35(5):450–461. doi: 10.1093/jpepsy/jsp118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Huang H, Yan P, Shan Z, et al. Adverse childhood experiences and risk of type 2 diabetes: A systematic review and meta-analysis. Metabolism. 2015;64(11):1408–1418. doi: 10.1016/j.metabol.2015.08.019 [DOI] [PubMed] [Google Scholar]
- 46.Angelakis I, Gillespie EL, Panagioti M. Childhood maltreatment and adult suicidality: a comprehensive systematic review with meta-analysis. Psychol Med. 2019;49(7):1057–1078. doi: 10.1017/S0033291718003823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Castellví P, Miranda-Mendizábal A, Parés-Badell O, et al. Exposure to violence, a risk for suicide in youths and young adults. A meta-analysis of longitudinal studies. Acta Psychiatr Scand. 2017;135(3):195–211. doi: 10.1111/acps.12679 [DOI] [PubMed] [Google Scholar]
- 48.Zatti C, Rosa V, Barros A, et al. Childhood trauma and suicide attempt: A meta-analysis of longitudinal studies from the last decade. Psychiatry Res. 2017;256:353–358. doi: 10.1016/j.psychres.2017.06.082 [DOI] [PubMed] [Google Scholar]
- 49.Devries KM, Mak JY, Child JC, et al. Childhood sexual abuse and suicidal behavior: a meta-analysis. Pediatrics. 2014;133(5):e1331–e1344. doi: 10.1542/peds.2013-2166 [DOI] [PubMed] [Google Scholar]
- 50.Ng QX, Yong BZJ, Ho CYX, Lim DY, Yeo W-S. Early life sexual abuse is associated with increased suicide attempts: An update meta-analysis. J Psychiatr Res. 2018;99:129–141. doi: 10.1016/j.jpsychires.2018.02.001 [DOI] [PubMed] [Google Scholar]
- 51.Bellis MA, Hughes K, Leckenby N, Hardcastle KA, Perkins C, Lowey H. Measuring mortality and the burden of adult disease associated with adverse childhood experiences in England: a national survey. J Public Health (Oxf). 2015;37(3):445–454. doi: 10.1093/pubmed/fdu065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Anda RF, Felitti VJ, Bremner JD, et al. The enduring effects of abuse and related adverse experiences in childhood. a convergence of evidence from neurobiology and epidemiology. Eur Arch Psychiatry Clin Neurosci. 2006;256(3):174–186. doi: 10.1007/s00406-005-0624-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hughes K, Ford K, Kadel R, Sharp CA, Bellis MA. Health and financial burden of adverse childhood experiences in England and Wales: a combined primary data study of five surveys. BMJ Open. 2020;10(6):e036374–e036374.doi: 10.1136/bmjopen-2019-036374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Medsafe. 2017 National health expenditures highlights. February 13, 2019. Accessed July 1, 2020. https://www.medsafe.com/blog/compliance-topics/2017-national-health-expenditures-highlights [Google Scholar]
- 55.Dubowitz H, Feigelman S, Lane W, Kim J. Pediatric primary care to help prevent child maltreatment: the Safe Environment for Every Kid (SEEK) Model. Pediatrics. 2009;123(3):858–864. doi: 10.1542/peds.2008-1376 [DOI] [PubMed] [Google Scholar]
- 56.Garner AS, Shonkoff JP; Committee on Psychosocial Aspects of Child and Family Health; Committee on Early Childhood, Adoption, and Dependent Care; Section on Developmental and Behavioral Pediatrics. Early childhood adversity, toxic stress, and the role of the pediatrician: translating developmental science into lifelong health. Pediatrics. 2012;129(1):e224–e231. doi: 10.1542/peds.2011-2662 [DOI] [PubMed] [Google Scholar]
- 57.Daelmans B, Darmstadt GL, Lombardi J, et al. ; Lancet Early Childhood Development Series Steering Committee. Early childhood development: the foundation of sustainable development. Lancet. 2017;389(10064):9–11. doi: 10.1016/S0140-6736(16)31659-2 [DOI] [PubMed] [Google Scholar]
- 58.Olds DL, Eckenrode J, Henderson CR Jr, et al. Long-term effects of home visitation on maternal life course and child abuse and neglect. fifteen-year follow-up of a randomized trial. JAMA. 1997;278(8):637–643. doi: 10.1001/jama.1997.03550080047038 [DOI] [PubMed] [Google Scholar]
- 59.Olds DL, Henderson CR Jr, Chamberlin R, Tatelbaum R. Preventing child abuse and neglect: a randomized trial of nurse home visitation. Pediatrics. 1986;78(1):65–78. [PubMed] [Google Scholar]
- 60.Prevent Child Abuse America. 2020 Federal policy agenda. Accessed August 10, 2020. https://preventchildabuse.org/resources/2020-federal-policy-agenda/ [Google Scholar]
- 61.The Children’s Defense Fund. The state of America’s children 2020. Accessed August 10, 2020. https://www.childrensdefense.org/the-state-of-americas-children-2020/ [Google Scholar]
- 62.Martin M, Erney R, Citrin A, Reeves R. 20 Years of TANF: Opportunities to better support families facing multiple barriers. Accessed June 17, 2021. https://cssp.org/wp-content/uploads/2018/08/TANF-at-20.pdf [Google Scholar]
- 63.Dubowitz H The Safe Environment for Every Kid (SEEK) Model: helping promote children’s health, development, and safety: SEEK offers a practical model for enhancing pediatric primary care. Child Abuse Negl. 2014;38(11):1725–1733. doi: 10.1016/j.chiabu.2014.07.011 [DOI] [PubMed] [Google Scholar]
- 64.McLaughlin KA, Weissman D, Bitrán D. Childhood adversity and neural development: a systematic review. Annu Rev Dev Psychol. 2019;1(1):277–312. doi: 10.1146/annurev-devpsych-121318-084950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Berens AE, Jensen SKG, Nelson CA III. Biological embedding of childhood adversity: from physiological mechanisms to clinical implications. BMC Med. 2017;15(1):135. doi: 10.1186/s12916-017-0895-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Colich NL, Rosen ML, Williams ES, McLaughlin KA. Biological aging in childhood and adolescence following experiences of threat and deprivation: a systematic review and meta-analysis. Psychol Bull. 2020;146(9):721–764. doi: 10.1037/bul0000270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hardcastle K, Bellis MA, Ford K, Hughes K, Garner J, Ramos Rodriguez G. Measuring the relationships between adverse childhood experiences and educational and employment success in England and Wales: findings from a retrospective study. Public Health. 2018;165:106–116. doi: 10.1016/j.puhe.2018.09.014 [DOI] [PubMed] [Google Scholar]
- 68.Jimenez ME, Wade R Jr, Lin Y, Morrow LM, Reichman NE. Adverse experiences in early childhood and kindergarten outcomes. Pediatrics. 2016;137(2):e20151839. doi: 10.1542/peds.2015-1839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Miller AB, Sheridan MA, Hanson JL, et al. Dimensions of deprivation and threat, psychopathology, and potential mediators: a multi-year longitudinal analysis. J Abnorm Psychol. 2018;127(2):160–170. doi: 10.1037/abn0000331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Andersen SL, Teicher MH. Desperately driven and no brakes: developmental stress exposure and subsequent risk for substance abuse. Neurosci Biobehav Rev. 2009;33(4):516–524. doi: 10.1016/j.neubiorev.2008.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Edalati H, Krank MD. Childhood maltreatment and development of substance use disorders: a review and a model of cognitive pathways. Trauma Violence Abuse. 2016;17(5):454–467. doi: 10.1177/1524838015584370 [DOI] [PubMed] [Google Scholar]
- 72.Keyes KM, Eaton NR, Krueger RF, et al. Childhood maltreatment and the structure of common psychiatric disorders. Br J Psychiatry. 2012;200(2):107–115. doi: 10.1192/bjp.bp.111.093062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Edwards VJ, Holden GW, Felitti VJ, Anda RF. Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: results from the adverse childhood experiences study. Am J Psychiatry. 2003;160(8):1453–1460. doi: 10.1176/appi.ajp.160.8.1453 [DOI] [PubMed] [Google Scholar]
- 74.Purewal Boparai SK, Au V, Koita K, et al. Ameliorating the biological impacts of childhood adversity: a review of intervention programs. Child Abuse Negl. 2018;81:82–105. doi: 10.1016/j.chiabu.2018.04.014 [DOI] [PubMed] [Google Scholar]
- 75.Berkowitz SJ, Stover CS, Marans SR. The child and family traumatic stress intervention: secondary prevention for youth at risk of developing PTSD. J Child Psychol Psychiatry. 2011;52(6):676–685. doi: 10.1111/j.1469-7610.2010.02321.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Cohen JA, Mannarino AP, Murray LK, Igelman R. Psychosocial interventions for maltreated and violence-exposed children. J Soc Issues. 2006;62(4):737–766. doi: 10.1111/j.1540-4560.2006.00485.x [DOI] [Google Scholar]
- 77.Shrier I, Pang M. Confounding, effect modification, and the odds ratio: common misinterpretations. J Clin Epidemiol. 2015;68(4): 470–474. doi: 10.1016/j.jclinepi.2014.12.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.